Abstract
Background:
The objective of this study is to compare the clinical, functional, and radiological outcomes of using bone-filled Polymethylmethacrylate (PMMA) implant as an inexpensive alternative to Polyetheretherketone (PEEK) cage and Autologous bone graft (ABG) fusion after anterior cervical discectomy (ACD) for the treatment of single level cervical disc disease.
Methods:
60 patients were prospectively randomized according to the material used for fusion after ACD into: 1) PMMA implant; 2) ABG; and 3) PEEK implant. The clinical outcomes were evaluated using Visual Analogue Scale (VAS), whereas the functional outcomes were evaluated using Odom's criteria. Radiological evaluations were also conducted using radiography and Computerized tomography (CT) scans and considered the following factors; bony fusion, cervical stability and disc space height (DSH) changes. The post- operative outcomes were evaluated at the following intervals; 2 weeks, 3 and 6 months.
Results:
The clinical outcomes demonstrated insignificant difference among the three treated groups throughout their follow up period. ABG group showed significant lower satisfactory functional outcomes (68.1%) compared to PMMA and PEEK groups (85% and 88.9%, respectively) at the 2-week post operative evaluation, but the ABG group showed closer functional outcomes to the PMMA and PEEK groups at the 3 and 6-month post operative evaluations. Despite the inferior bony fusion rates of the PMMA group (30%) compared to ABG group (86.3%) and PEEK group (77.7%) at the 6-month post operative evaluation, the clinical and functional outcomes were comparable.
Conclusions:
Bone-filled PMMA implant is a reliable treatment option; despite its inferior fusion rate at the 6-month postoperative evaluation, it still provides acceptable segmental stability, satisfactory clinical and functional outcomes that are comparable to ABG and PEEK grafting procedures.
Keywords: Cervical, Fusion, Polymethylmethacrylate, Polyetheretherketone, Autograft
Introduction
The concept of cervical inter-body fusion after ACD for treating cervical disc diseases developed progressively over the past 50 years in Cloward, Dereymaker, and Smith and Robinson studies using iliac crest bone graft. The basic idea was to stabilize the operated segment long enough to allow new bone growth, maintaining disc height, and avoiding the collapse of the graft until fusion occurred.1,2,3
The ideal fusion substrate remains a controversial issue. Autologous bone graft (ABG) was used in the original descriptions of fusion procedures for the cervical spine, and is still the standard and the most widely used fusion substrate. One important disadvantage associated with ABG is discomfort at the iliac crest; the site at which bone graft is harvested.4
Cervical cage was introduced in cervical spine surgery as an alternative method to ABG for stabilization after anterior cervical discectomy. Numerous types of cages were developed including: titanium, carbon fiber, and Polyetheretherketone (PEEK) cages.
Polyetheretherketone (PEEK) is a non-absorbable biopolymer that demonstrated absence of cytotoxicity and mutagenicity in vitro studies.5 This material is also biocompatible, radiolucent, and has modulus of elasticity similar to that of the bone.6 The principal advantage associated with using PEEK cages is the reduction of donor site morbidity, since it can provide immediate load –bearing support to the anterior column.7 However, cervical cages are significantly expensive, which can substantially increase the cost of the surgery.
In 1968, Grote introduced Polymethylmethacrylate (PMMA) as a quick and simple method to maintain the inter-vertebral distance after ACD8, even though it doesn’t achieve satisfactory bony fusion.9 Whether or not osseous fusion is an important condition for a good long-term outcome after cervical disc surgery is still open for debate.10 Another concern is the effect of exothermic reaction during polymerization of PMMA on neural and/or bone structures.11,12
In the present study, the PMMA was fashioned as hollow cylindrical strut filled with bone chips obtained from subchondral bone and osteophytes curettage. The objective is to get the strength of the PMMA material and the bioactivity of the bone chips in order to initiate bone fusion. The PMMA implant is adjusted after proper size determination, and is prepared before placement in the disc space to avoid exothermic reaction to neural or/and bony structures.
The objective of this study is to compare the short-term (6 months) clinical, functional, and radiological outcomes of using bone-filled PMMA implant as an inexpensive alternative to PEEK cage and ABG fusion after ACD for the treatment of single level cervical disc disease.
Material and methods
Study Design
A consecutive series of patients with compressive radiculopathy secondary to single level cervical disc disease were prospectively randomized into three treatment groups according to the material used for reconstruction of the disc space after ACD. These three groups included: 1) bone- filled PMMA implant; 2) autologous bone graft; and 3) PEEK cervical cage.
Patients who fulfilled the inclusion criteria were informed about the study, and were assigned to one of the three treatment groups. Preoperatively, patients were informed about the result of the selection, and about the proposed treatment. Each patient agreed to the randomization, and provided written consent to the operation. The clinical and radiological data were collected before surgery and after surgery. The post- operative outcomes were evaluated at the following intervals; 2 weeks, 3 and 6 months.
Patient selection
This prospective study was conducted on 60 consecutive patients with pure radicular symptoms. The inclusion criteria required less than 1 year of symptomatic compressive radiculopathy due to single level cervical disc herniation between C3 and C7, confirmed by Magnetic Resonance Imaging (MRI), and clinical findings. Patients with evidence of significant myelopathy, cervical instability, whiplash injury, systemic infection, active malignancy, symptomatic degenerative disc disease with two or more cervical segments, psychiatric disturbance, previous cervical surgery, drug abuse, prolonged steroid therapy, ossification of the posterior longitudinal ligament (OPLL) and rheumatoid disease were excluded from the study.
Clinical evaluation
Preoperatively, The study forms of all the patients were completed, which included: questions regarding work and daily function; complete medical history; physical and neurological examinations. A Visual Analogue Scale (VAS) score was used to estimate the severity of their complaints by asking the patients to quantify their symptoms; neck pain, radicular pain, and neurological deficits (VAS score of 0 mm represents no complaint; VAS score of 100 mm represents the highest level of severity possible).13
Surgical technique
Patients underwent surgery in the supine position after induction of general anesthesia. Surgical procedures were performed using the Smith–Robinson antero-lateral approach via a right-sided skin incision. Anterior cervical microdiscectomy and resection of osteophytes were accomplished in all the studied cases. The posterior longitudinal ligament was excised thoroughly to ensure adequate neural decompression with exposure of the dura mater and origin of the nerve roots bilaterally. Gentle decortication of the middle of the endplates was performed using a curette. Special care was taken not to weaken the endplates in order to prevent the graft or the implant from settling into the vertebral body.
Autologous bone Graft group (ABG)
In the ABG group, a tricortical iliac crest bone graft was harvested using a standard osteotome technique. The tricortical bone graft was adjusted to fit into the slightly distracted disc space, and countersunk into position.
Cervical cage group (PEEK)
The cage is a radio-transparent, trapezoidal-shaped with hollow inner space, and slightly wedged implant, made from a polymer matrix of Polyetheretherketone. An optimal PEEK cage size was selected following completion of discectomy and endplate preparation. The inner cavity of the PEEK cage was filled with bone chips obtained from curettage of subchondral bone and osteophytes. The PEEK cage was impacted into disc space for fusion after adequate distraction with the use of Caspar distractor.
Bone-filled Polymethylmethacrylate group (PMMA)
A round, hollow, cylindrical strut was fashioned from PMMA. The PMMA powder sachet and phial of solvent must be transferred under aseptic conditions to sterile working surface in the operating theatre. The powder sachet was opened and poured over the liquid. Once the powder is mixed with the liquid, the mixture must be left to rest. A sterile plastic syringe (10-12 ml) was sharply divided into cylinders according to the needed height of the disc space. After an adequate amount of resting time has passed, the cement was collected from the bowl and was handled until the cement seized to adhere to the gloves. During this phase, the cement was inserted into the previously prepared appropriate plastic cylinders. Then PMMA mixture was penetrated centrally, using a metal rod to make a central hollow cavity. After few minutes, the PMMA material became harder, and the wall of the plastic cylinder was peeled from the PMMA implant.
The height of the PMMA implant was determined by the pre-operative images and intra-operative measurements of the disc space while in mild distraction. The anterior-posterior surface of the PMMA implant was trimmed to provide a few millimeters of distance between the most posterior part of the fully recessed implant and the spinal cord. The width of the PMMA implant was determined to be smaller than the right-left width of the disc space. The PMMA implant ranged between 12-15 mm in outer diameter and 5-8 mm in the inner diameter to provide the maximum contact surface area between the bone chips filling the PMMA implant and decorticated endplates. (Fig. 1)
Figure 1.

Photograph of the PMMA implant.
Postoperatively, all patients were instructed to wear a hard cervical collar during the first 6 weeks. Complications and morbidity, such as dysphagia, hoarseness of voice, postoperative hematoma, or donor site pain were monitored.
Assessment of the outcome
Post-operative clinical, functional and radiological outcomes were evaluated after 2 weeks, 3 months, and 6 months. No patient was lost during the follow up period.
The clinical outcomes included; evaluation of the post-operative cervical and radicular pain, and neurological status improvement based on the VAS score. The recovery rate was calculated for each patient according to the following equation:
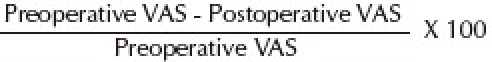
Then, the mean of recovery rates of cervical pain, radicular pain and neurological deficits of each group were estimated after 2 weeks, 3 months and 6 months.
Functional outcomes were assessed by evaluating work capacity according to Odom's Criteria.14 An excellent outcome was achieved in patients without complaints referable to cervical disc disease and who were able to perform their daily routines without impairment; a good outcome was achieved when intermittent cervical disc related discomfort, that did not significantly interfere with work, occurred; a fair outcome was achieved when subjective improvement coupled with limited physical activity occurred; and a poor outcome was achieved when improvement was absent or the patient's condition worsened when compared to his/her preoperative status .
Questionnaires were updated during each visit; additionally patients were encouraged to express their perceptions of surgery outcomes.
Radiological evaluations included; fusion criteria, stability of the operated segment, position of the implant and disc space height changes. Fusion was identified by the following: the absence of motion on flexion-extension lateral plain radiography; the absence of radiolucent gap between the implant or the graft and the host vertebral endplates; and the presence of continuous, bridging, osseous trabeculation at the graft host vertebral endplate junction. The evaluation was performed using conventional plain radiographs, and reconstructed CT scans of the cervical spine at 3 and 6 months. Each operative segment was considered stable if there was no segmental movement on lateral flexion-extension views, at the 6-month post operative evaluation. Post-operative disc space height (DSH) changes were evaluated at 3 and 6 months and compared to the early post-operative disc space height at the 2ed week. Graft/Implant subsidence (migration into the superior and/or inferior vertebral body >2 mm) and extrusion (slipped out >2 mm) were analyzed in this study as well.
Statistical Analysis
The two-tailed Fisher exact test and the Kruskal–Wallis nonparametric analysis of variance test including the Dunn multiple comparison test were conducted to evaluate the intergroup demographic equivalence and to examine the intergroup differences in outcomes. Statistical significance was set at p < 0.05.
Results
Differences in patients’ characteristics
Sixty patients participated in the study. There were 34 men, and 26 women, with ages ranging between 28 and 68 years (mean of patients’ age was 46.7years), the frequency of the 40-50 age group was the highest (24 cases). The duration of the complaints experienced by most patients included in the present study ranged between 3 to 6 months (34cases). Smokers’ distribution was insignificant among the three studied groups; no heavy smokers were found in the studied cases.
Surgery related variables
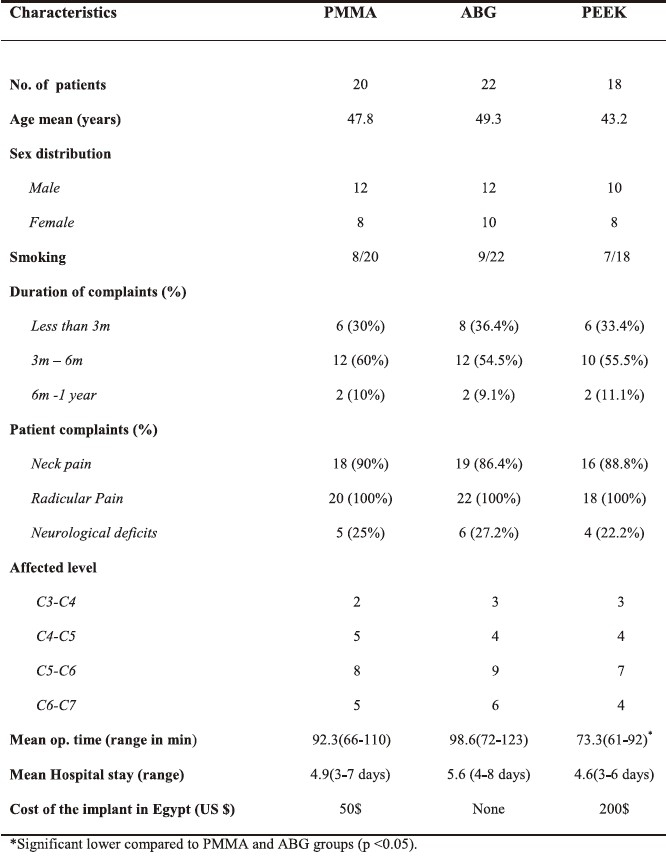
The PEEK cage treatment group demonstrated the shortest mean operating time (73.3 min.) which was significantly shorter time than the PMMA, and ABG treatment groups (mean 92.3min. and 98.6min., respectively; p < 0.05). The mean post-operative hospital stay of ABG group was relatively longer (mean 5.6 days) to the PMMA and PEEK groups (mean 4.9 days and 4.6 days, respectively), but without significant difference among the three treated groups .The cost of PMMA pack was approximately 50 US dollars, and was less expensive than the PEEK cervical cage, which was approximately 200 US dollars. (Table 1)
Table 1.
Characteristics of the studied patients
Post-operative outcomes
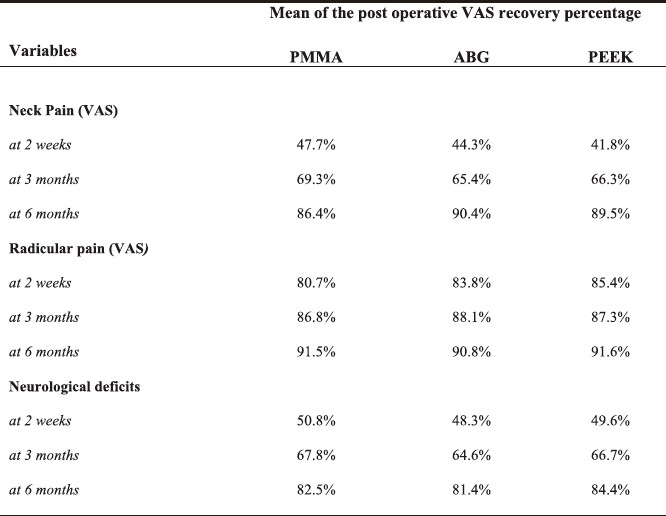
During the clinical follow up period, the mean difference of post-operative clinical outcomes recovery rates regarding neck pain, radicular pain, and neurological deficits was not significantly different among the three treated groups (Table 2).
Table 2.
Post operative clinical outcomes according to VAS recovery percentage
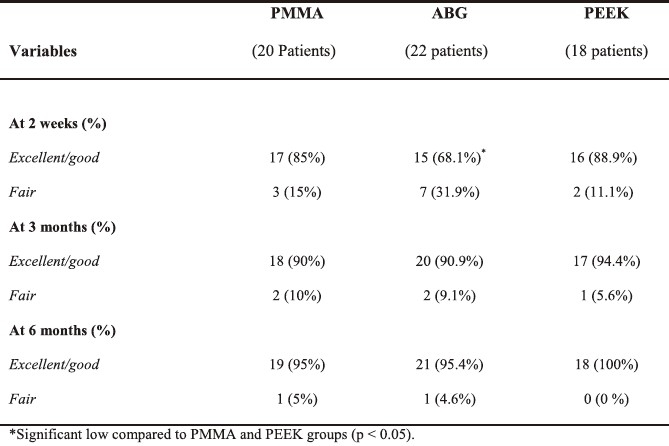
Satisfactory functional outcomes according to Odom's criteria (excellent and good) of the ABG cases were significantly lower (68.1%) than in PMMA and PEEK cases (85% and 88.9%, respectively; p< 0.05) at the 2-week evaluation. However, this was no longer significant by the 3-month follow up, there was a trend of improved functional outcomes for the ABG group according to Odom's criteria, and it became closer to those of the PMMA and PEEK groups, with no statistically significant differences among the three groups at 3 and 6 months. Functional outcomes which were rated as poor were not encountered in the present study (Table 3).
Table 3.
Post operative functional outcomes according to Odom's criteria
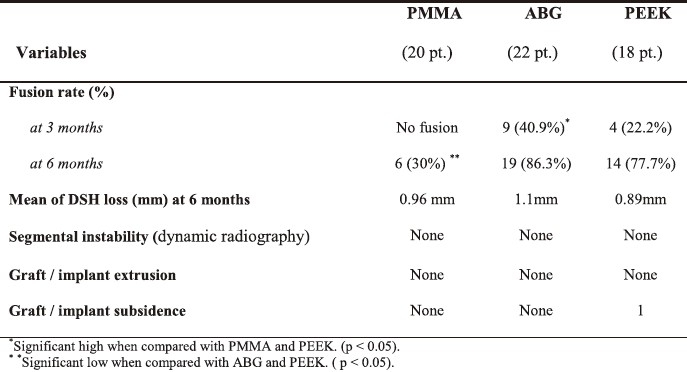
The ABG group recorded a statistically significant higher fusion rate (40.9%) compared to the PMMA and PEEK groups 3 months following surgery (No fusion and 22.2%, respectively). However, after six months of follow up, the difference between the improved fusions rates in the PEEK group (77.7%) and the ABG group (86.3%) was no longer significant (Fig.2). Late evidence of apparent starting osseous fusion of the PMMA group was demonstrated in only six cases (30%) six months following surgery based on the CT scan findings (Fig.3).
Figure 2.
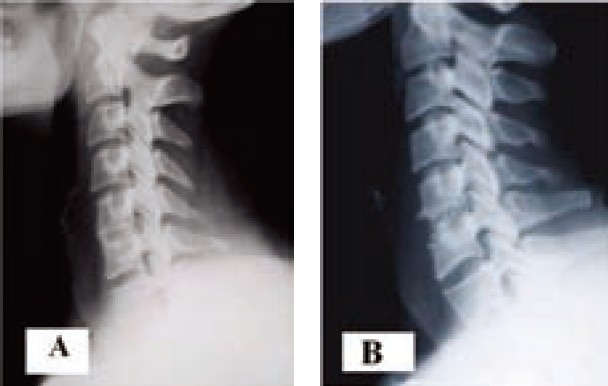
Post operative (6 months) plain radiographs lateral views of cervical spine demonstrate bony fusion after ACD of C5-C6 using ABG (A) and PEEK cage (B).
Figure 3.
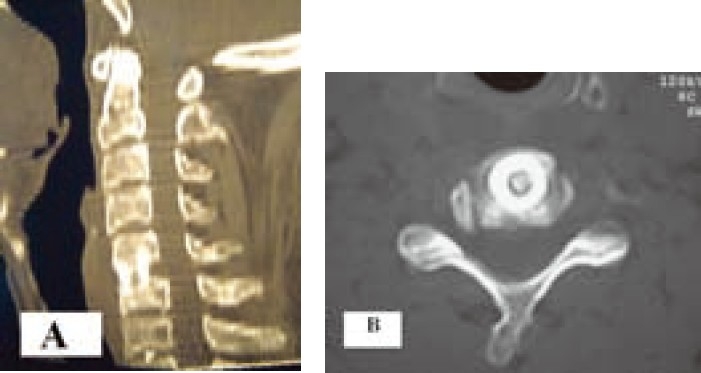
Post operative (6 months) reconstructed CT scan; sagittal (A) and axial (B) views; demonstrate starting bony fusion of the bone-filled PMMA implant after ACD of C5-C6.
Radiological analysis showed good stabilization in all of the studied cases; including the non-fused cases of the PMMA group through out their follow up period, as no mobility was found in flexion-extension radiography of the cervical spine. (Fig.4). The changes of the disc space height were evaluated after three, and six months postoperatively, there were no significant differences regarding disc space height changes that occurred in patients belonging to the three studied groups when compared to the early postoperative disc space height 2-weeks post operatively. Subsidence was demonstrated in one case from the PEEK group 3 months following surgery. However, the degree of subsidence was unchanged at the 6-month evaluation, indicating no progression of subsidence over time (Fig.5). No graft or implant extrusion was encountered in the present study. (Table 4)
Figure 4.

Post operative (6 months) plain lateral radiographs (dynamic views); flexion (A) and extension (B) demonstrate good stability of the incompletely fused bone-filled PMMA implant after ACD of C5-6.
Figure 5.

Plain lateral radiograph demonstrates cervical cage (PEEK) subsidence of C5-C6 level after 6 months.
Table 4.
Post operative radiological outcomes
Surgery –related complications:
No serious surgical or neurological complications occurred in the studied cases. Dysphagia was the most common postoperative complication (16 cases) followed by voice hoarseness (6 cases). However, the Dysphagia and voice hoarseness were mild and only lasted for a few days. Pain at the donor site was found in 14 cases (63.6%) of the ABG group. The pain persisted for more than 2 weeks and then subsided gradually until it completely disappeared by the second month following the surgery.
Discussion
Since the introduction of different grafting strategies after ACD, osseous fusion has been a matter of debate. Fusion can be achieved by autologous bone graft, and cervical cage interposition; which has been introduced as an alternative to ABG to avoid donor site complications, but it substantially added cost.15 The PMMA spacer is used to treat cervical disc disease in many centers, and is found to be a quick, simple and less expensive method to maintain the inter-body distance after cervical discectomy. However, it has been widely criticized due to the resulting reduced osseous fusion with vertebral bodies.16
In the present study, the use of bone – filled PMMA implant for treatment of cervical disc disease achieved earlier bone fusion six months following surgery in 30% of the cases. In contrast, using PMMA spacer alone required much more time for the bone fusion to develop.17,18
The fusion rate was much lower in the PMMA group than the PEEK group; despite both implants having the same structure (cage shaped), similar fusion material (curetted bone chips and osteophytes) albeit different implant material.
As described in Wolff's law, bone grows in response to applied stress and is resorbed if a mechanical stimulus is lacking. The PEEK cage is a semicrystalline polyaromatic linear polymer that provides a good combination of strength, stiffness, toughness, and environmental resistance. The elastic modulus of the cage is close to that of the bone which helps to deleterious influence on cell attachment and growth.19
Polymethylmethacrylate (PMMA) does not attach to bone. After its implantation, a fibrous cement-bone interface is formed. In ACD with PMMA, the radiolucent zone around Polymethylmethacrylate was shown to consist of a similar layer of fibrous tissue.20
Also, bone cannot invade Polymethylmethacrylate. After ACD with Polymethylmethacrylate (PMMA), bone union has to develop by ossification around the PMMA, which clearly takes more time than if bone is being used.21
In the present study, the PMMA was fashioned as hollow cylindrical strut filled with bone chips obtained from subchondral bone and osteophytes curettage. The benefits are getting the strength of the PMMA material and the bioactivity of the bone chips to initiate the bone fusion.
The fusion through the PMMA implant is difficult to be shown through usual radiological techniques but signs of osseous consolidation can be detected around the PMMA implant. Furthermore, it may be assessed from the long term stability, absence of bone rarefaction around the PMMA implant, CT reconstruction and no recurrence of the symptoms.
Wilke, et al., performed an in vitro study of the stabilizing effect and subsidence tendency of cervical fusion cages and bone cement during cyclic loading. In lateral bending, flexion and axial rotation, the PEEK cage promoted the greatest stability followed by PMMA cages. After 700 loading cycles, height loss was 0.7 mm with PEEK cage, and 0.5mm with bone cement cage. They concluded that cages have the potential to stabilize as effectively as bone cement.22
Furderer, et al., compared subsidence of differently designed cervical inter-body fusion cages; end plate abrasion was found to result in increased subsidence, which may explain the occurrence of subsidence of the PEEK cage in the present study. Therefore, it is imperative that cortical bone of the endplate be carefully decorticated during the preparation of the implant bed.23
After 6 months, satisfactory results regarding disc space height changes were observed through the cases of the three studied groups when compared to early postoperative disc space height (two weeks).
In the present study, despite poor segmental fusion of the PMMA group (30%) when compared to ABG group (86.3%) and PEEK group (77.7%), the clinical outcomes according to the mean of percentage of VAS recovery in the PMMA treatment group were comparable to those of the ABG and PEEK groups. This may be attributed to the fact that a similar surgical technique (ACD) was used as well as adequate neural decom-pression in all studied cases; this usually results in satisfactory outcomes. Based on the results of this study, the segmental fusion rate of PMMA is expected to increase with longer follow-up periods because segmental stability was obtained in all cases at the 6-month follow up evaluation.
The functional outcome classification by Odom has been widely used by a number of investigators. After two weeks, 85% of the PMMA cases and 88.9% of the PEEK cases had satisfactory functional outcome (excellent-good), which were statistically significantly higher than in ABG cases (68.1%). This was mainly due to donor site discomfort of the ABG group cases. After 6 months, there was a tendency for a better functional outcome in the ABG cases (95.4%) and became closer to those of the PMMA (95%) and PEEK (100%) cases, with no statistically significant differences among them. There were a few cases that showed fair results; they constituted 5% of the PMMA cases, 4.6% of ABG cases. None of the studied cases experienced poor a functional outcome as defined earlier.
Van den Bent et al., reported excellent and good functional outcomes (successful surgery) in 70 % of 42 cases who has PMMA inter-body fusion after 2 years of follow up. 17 Also, Hamburger et al, reported satisfactory functional outcomes in 77.5% of 249 cases of PMMA inter-body fusion after a follow up period of 12 years.18 Both studies included patients with myelopathy associated with chronic neurological deficits which likely explains why their reported functional outcome results were lower than those reported in the present study. The shorter pre-operative duration of symp-toms and adequate surgical neural decom-pression in properly selected patients appear to be the most important prognostic factors that could result in satisfactory clinical and functional outcomes.
Conclusions
Fusion rates at 6 months with bone- filled PMMA implant were inferior to ABG and PEEK cage. However, bone- filled PMMA still achieved acceptable segmental stability, satisfactory short term clinical and functional outcomes equivalent to ABG and PEEK cage grafting procedures.
Bone-filled PMMA implant is a safe and reliable treatment option after ACD providing;
No donor site harvesting complications.
Inexpensive spacer material compared to PEEK cage.
Easiness of preparation during surgical procedure.
No risk of exothermic injury to neural structures as it is adjusted before placement in the disc space.
The progress of segmental fusion of the bone-filled PMMA implants needs to be studied on a larger series and for a longer follow-up period.
Abbreviations list
ABG = autologous bone graft
ACD= Anterior cervical discectomy
CT= Computerized tomography
DSH= Disc space height
MRI= Magnetic resonance Imaging
OPLL= Ossified posterior longitudinal ligament
PEEK= Polyetheretherketone
PMMA = Polymethylmethacrylate
VAS =visual analog scale
References
- 1.Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 1958;15:602–17. doi: 10.3171/jns.1958.15.6.0602. [DOI] [PubMed] [Google Scholar]
- 2.Dereymaker A, Mulier J. La Fusionverte’brale par voie ventral dans la discopathie cervical. Rev Neurol. 1958;99:597–616. [PubMed] [Google Scholar]
- 3.Smith GW, Robinson RA. Anterolateral cervical disc removal and interbody fusion for cervical disc syndrome. Bull John Hopkins Hosp. 1955;96:223–24. [Google Scholar]
- 4.Cockin J. Autologous bone graft: Complications at the donor site. J. Bone Joins. Surg., (Br.) 1997;53-B:153–59. [Google Scholar]
- 5.Katzer A, Marquardt H, Westendorf J. Polyetheretherketone-cytotoxicity and mutagenicity in vitro. Biomaterials. 2002;23(8):1749–59. doi: 10.1016/s0142-9612(01)00300-3. [DOI] [PubMed] [Google Scholar]
- 6.Toth JM, Wang M, Estes BT, Scifert JL, et al. Polyetheretherketone as a biomaterial for spinal applications. Biomaterials. 2006;27(3):324–34. doi: 10.1016/j.biomaterials.2005.07.011. [DOI] [PubMed] [Google Scholar]
- 7.Brooke NS, Rorke AW, King AT. Preliminary experience of carbon fiber cage prosthesis for treatment of cervical spine disorders. Br J Neurosurg. 1997;11:221–7. doi: 10.1080/02688699746285. [DOI] [PubMed] [Google Scholar]
- 8.Grote W, Bettage W, Rullenweber Indikationen, Technik und Ergebnisse zervikaler fusionen. Mels Med Mitt. 1968;42:119–32. [Google Scholar]
- 9.Cantu RC. Anterior spinal fusion using methyl methacrylate (Acrylic) Int Surg. 1974;59:110–1. [PubMed] [Google Scholar]
- 10.Sonntag VK, Klara P. Controversy in spine care. Is fusion necessary after anterior cervical discectomy? Spine. 1996;21:1111–3. doi: 10.1097/00007632-199605010-00025. [DOI] [PubMed] [Google Scholar]
- 11.Roosen k, Grote w, Bettag W. Komplikationen zervikaler ventraler fusions operationen. Neurochirurgia. 1975;18:1–11. doi: 10.1055/s-0028-1090422. [DOI] [PubMed] [Google Scholar]
- 12.Roosen K, Grote W, Liesegang J, Linke V. Epidural temperature changes during anterior cervical interbody fusion with Polymethyl-methacrylate. Adv Neurosurg. 1987;5:373–5. [Google Scholar]
- 13.Scott J, Huskisson EC. Graphic representation of pain. Pain. 1976;2:175–84. [PubMed] [Google Scholar]
- 14.Odom GL, Finney W, Woodhall B. Cervical disk lesions. JAMA. 1958;166:23–8. doi: 10.1001/jama.1958.02990010025006. [DOI] [PubMed] [Google Scholar]
- 15.Mastronardi L, Ducati A, Ferrante L. Anterior cervical fusion with Polyetheretherketone (PEEK) cages in the treatment of degenerative disc disease. Acta Neurochir (Wien) 2006;148:307–12. doi: 10.1007/s00701-005-0657-5. [DOI] [PubMed] [Google Scholar]
- 16.Whitehill R, Barry JC. The evolution of stability in cervical spine constructs using either autogenous bone graft or methyl-methacrylate cement. Spine. 1995;10:32–41. doi: 10.1097/00007632-198501000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Van den Bent MJ, Oosting J, Wouda EJ, et al. Anterior cervical discectomy with or without fusion with Acrylate. A randomized trial. Spine. 1996;21:834–40. doi: 10.1097/00007632-199604010-00011. [DOI] [PubMed] [Google Scholar]
- 18.Hamburger C, festenberg VF, Uhl E. Ventral discectomy with PMMA inter-body Fusion of cervical disc disease: long term results in 249 patients. Spine. 2001;21:249–55. doi: 10.1097/00007632-200102010-00009. [DOI] [PubMed] [Google Scholar]
- 19.Cho D, Liau W, Lee W, et al. Preliminary experience using a Polyetheretherketone (PEEK) cage in the treatment of cervical disc disease. Neurosurgy on line. 2002;51(6):1343–55. [PubMed] [Google Scholar]
- 20.Horowitz SM, Doty SB, Lane JM, Burstein AH. Studies of the mechanism by which the mechanical failure of polymethylmethacrylate leads to bone resorption. K Bone Joint Surg. 1993;75A:802–13. doi: 10.2106/00004623-199306000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Clark CR, Whitehill R. Two views of the use of methylmethacrylate for stabilization of the cervical spine. Orthopedics. 1989;12:589–96. doi: 10.3928/0147-7447-19890401-14. [DOI] [PubMed] [Google Scholar]
- 22.Wilke HJ, Kettler a, Claes L. Stabilizing effect and Sintering tendency of three different cages and bone cement for fusion for cervical vertebral segment. Orthopade. 2002;31:472–80. doi: 10.1007/s00132-001-0288-3. [DOI] [PubMed] [Google Scholar]
- 23.Fruderer S, Schollhuber F, Rompe JD. Effect of design and implantation technique on risk of progressive sintering of various cervical vertebrae cages. Orthopde. 2002;31:466–71. doi: 10.1007/s00132-001-0289-2. [DOI] [PubMed] [Google Scholar]


