Abstract
Background
The neuroanatomic basis of affective processing deficits in Huntington disease is insufficiently understood. We investigated whether Huntington disease–related deficits in emotion recognition and experience are associated with specific changes in grey matter volume.
Method
We assessed grey matter volume in symptomatic patients with Huntington disease and healthy controls using voxel-based morphometry, and we correlated regional grey matter volume with participants’ affective ratings.
Results
We enrolled 18 patients with Huntington disease and 18 healthy controls in our study. Patients with Huntington disease showed normal affective experience but impaired recognition of negative emotions (disgust, anger, sadness). The patients perceived the emotions as less intense and made more classification errors than controls. These deficits were correlated with regional atrophy in emotion-relevant areas (insula, orbitofrontal cortex) and in memory-relevant areas (dorsolateral prefrontal cortex, hippocampus).
Limitations
Our study was limited by the small sample size and the resulting modest statistical power relative to the number of tests.
Conclusion
Our study sheds new light on the importance of a cognitive–affective brain circuit involved in the affect recognition impairment in patients with Huntington disease.
Introduction
Huntington disease is a progressive neurodegenerative disorder that is caused by a gene mutation on chromosome 4 (locus 4p16.3). The core symptom consists of involuntary hyperkinetic movements in the arms, legs, neck, trunk and face (chorea). The onset of these motor abnormalities, which commonly become noticeable in mid-adulthood, is used as a criterion of clinical manifestation of this disorder.1 However, before the occurrence of motor symptoms, deficits in cognitive and affective processing have been observed in gene carriers.2,3
Impairments in cognitive performance concern functions such as attention, memory and visuo-spatial processing.4 These dysfunctions are already present in individuals who carry the gene mutation but display no overt motor symptoms.2 Evidence from functional neuroimaging suggests that in the presymptomatic stage of the disease, afflicted individuals show altered activation of prefrontal areas, such as the dorsolateral prefrontal cortex (DLPFC) and the orbitofrontal cortex (OFC), during working memory tasks and motor sequence learning.5,6 The localized functional changes occur before neuronal loss can be detected in these regions.6 Over the course of the disorder, the cognitive abilities decline into dementia for most patients and can be clearly related to (sub)cortical atrophy.7,8
Deficits in affective processing have also been described to precede motor dysfunction in patients with Huntington disease.3 An outstanding problem refers to emotion recognition deficits. When gene carriers are asked to label emotional facial expressions, they make more categorization errors than healthy controls. In some studies presymptomatic individuals with Huntington disease displayed a general impairment in facial emotion recognition,9 whereas in others a specific deficit in disgust identification has been described.3,10,11
Similar inconsistent findings have been reported for symptomatic patients with Huntington disease. Most investigations did not detect disproportionally impaired disgust recognition in patients with Huntington disease.12–15 In these studies, several negative emotions (fear, anger, disgust, sadness) were not accurately classified by the patients. On the other hand, some investigations on manifest Huntington disease detected a more pronounced deficit in disgust recognition compared with other negative emotions.16,17
These deficits have been related to the specific atrophy pattern of Huntington disease, which in the beginning primarily targets the basal ganglia (striatum). The importance of striatal recruitment for disgust recognition has been highlighted by several functional neuroimaging studies.18,19 More recent morphometric studies, however, point to the important role of the basal ganglia for the identification of different emotions, such as surprise, disgust and anger.14
Furthermore, the insula has been repeatedly implicated in the processing of facial disgust in healthy individuals18 and in presymptomatic patients with Huntington disease.3,20 As for the striatum, the role of the insula as a specific disgust processor has been questioned, and it has been put forward that this structure is crucial for the recognition and experience of different basic emotions.21
The main purpose of this voxel-based morphometry (VBM) study was to investigate whether impairments in the recognition of specific facial emotions are linked with specific changes in grey matter volume in symptomatic patients with Huntington disease. Moreover, we looked at the association between the experiences of basic emotions and localized grey matter atrophy. Up until now the neurostructural basis of affective experience has not been studied in patients with Huntington disease. There is only 1 related study that showed that patients with Huntington disease classified fewer affective scenes as disgusting than healthy controls.22
In the present investigation, we presented the participants (symptomatic patients with Huntington disease and healthy controls) with affective scenes that have been proven to elicit disgust, fear and happiness, as indicated by subjective ratings and involvement of the insula, amygdala and OFC in healthy individuals21,23 and psychiatric patients.24 Additionally, the participants viewed emotional facial expressions depicting happiness, fear, sadness, anger, disgust and surprise and a neutral affective state. For the 2 tasks, facial emotion recognition and emotion experience, we used a new paradigm in which the participants were asked to judge the intensity of the displayed affect in the faces and the elicited affect in themselves by the scenes for 6 basic emotions (fear, anger, disgust, sadness, surprise and happiness). With this approach, deviant affective processing can be described in more detail and can be quantified (e.g., the extent and type of emotion misclassification). All previous investigations used a forced-choice answering mode that only allowed the researchers to determine that an error in affect recognition had been made; however, it remained unclear which other emotions had been perceived instead of the target emotion.
In this study, we tested the specific hypotheses that patients would rate negative facial emotions (anger, disgust, sadness and fear) as less intense and make more classification errors than healthy controls. We furthermore hypothesized that a set of different regions of interest (ROIs; basal ganglia regions, prefrontal regions, amygdala, insula, hippocampus) might show atrophy in patients with Huntington disease relative to healthy controls, as these regions have been repeatedly identified to be involved in affective processing and memory. The regional grey matter volume was correlated with the intensity of recognized and experienced emotions and with the classification accuracy. Moreover, for the patient sample we related atrophy in the ROIs to different indicators of symptom severity (e.g., degree of motor disturbance, functional capacity, symptom duration, CAG repeats).
Methods
Participants
We recruited symptomatic patients with Huntington disease and healthy controls matched for age and sex for participation in this study. Patients with genetically confirmed Huntington disease were recruited from the Medical University of Graz. They were included in this study when motor symptoms allowed the handling of a response box for the affective ratings. We obtained written informed consent from each participant. This study was carried out in accordance with the Declaration of Helsinki and was approved by the ethics committee of the Medical University of Graz.
Questionnaires
The participants were assessed on the following tests. The Test for Early Detection of Dementia (TFDD)28 allows the detection of early signs of cognitive impairment. The scores of this scale range between 0 and 50. A score below 35 indicates a tentative dementia diagnosis and therefore was considered an exclusion criterion. With insufficient comprehension of instructions, no valid and reliable assessment of emotion recognition and experience can be achieved. The Cronbach α of the TFDD is 0.88.
The Unified Huntington Disease Rating Scale (UHDRS)1 is a standardized clinical rating instrument for the assessment of motor, cognitive and behavioural symptoms and functional capacity in patients with Huntington disease. The UHDRS motor scale ranges from 0 to 124, with higher scores indicating motor impairment. Eye movements, motor control, rigidity, bradykinesia, dystonia, chorea and gait are assessed. The UHDRS Functional Assessment Scale consists of 25 questions referring to the performance of daily life activities (e.g., “Can the subject operate an automobile safely and independently”), ranging from 0 to 25. Using the UHDRS Independence Scale, the current level of a patient’s independence is estimated between 0% and 100% (a higher score indicates better function). The UHDRS Functional Capacity Scale consists of 5 items assessing engagement in occupation, capacity to handle financial affairs, capacity to manage domestic responsibilities, capacity to perform activities of daily living and the type of residential care provided. Scores range from 0 to 13, with higher scores indicating better functioning and greater independence. The Cronbach α of the UHDRS is 0.95.
The Beck Depression Inventory (BDI; German version)25 consists of 21 items rated on 4-point scales. A sum score of 18 or higher shows clinical relevance. The Cronbach α of the BDI is 0.88.
The Questionnaire for the Assessment of Disgust Sensitivity (QADS)26 measures disgust propensity and describes 37 situations that have to be judged on 5-point scales with regard to the experienced disgust (e.g., “You are just about to drink a glass of milk as you notice that it is spoiled”). A rating of 0 means “not disgusting” and a rating of 4 means “very disgusting.” The Cronbach α of the QADS is 0.90.
The trait scale of the State-Trait Anxiety Inventory (STAI)27 measures the frequency of anxious feelings on 4-point scales (e.g., “I am happy,” or “I feel like crying”). The Cronbach α of the STAI is 0.88.
Stimuli and design
All participants viewed 42 pictures (6 in each category) with emotional facial expressions depicting happiness, fear, sadness, anger, disgust, surprise and a neutral affective state from the Karolinska set.29 Half of the models were women, and half were men. Participants also viewed 24 affective scenes (6 in each category) for the elicitation of happiness, fear, disgust and an affectively neutral state. The scenes were taken from the International Affective Picture System (IAPS).30 Disgust-inducing pictures were developed by Schienle and colleagues.21 Since the IAPS does not include pictures that reliably induce anger, sadness and surprise, these categories were omitted.
Each picture was presented once on a computer screen (15-inch diameter) for a maximum of 15 seconds. The participants could terminate the presentation early by pressing a button on a 3-button device that was developed for the experiment. Then, we asked the participants to rate the picture on a 9-point scale within 15 seconds. After the rating of a picture, the next picture was presented without any delay. For each affective scene, participants rated how intensely they had experienced the 6 basic emotions (e.g., “Please indicate how intensely you experienced disgust while viewing the picture:” 1 = very little, 9 = very intense). For each facial expression, participants rated how intensely the depicted person experienced the 6 basic emotions (e.g., “Please indicate how intensely the depicted person experienced disgust:” 1 = very little, 9 = very intense).
We computed the following performance measures for each participant:
emotion recognition intensity, which is the rated intensity of the displayed target emotion in a facial expression (e.g., the participant recognized disgust intensity in a facial disgust expression);
emotion experience intensity, which is the rated intensity of the experienced target emotion elicited by an affective scene (e.g., the participant experienced disgust intensity owing to a disgust-eliciting scene); and
classification accuracy of emotion recognition, which is the difference between the perceived intensity of a target emotion and the mean intensity of all nontarget emotions for a specific facial expression (e.g., classification accuracy of disgust recognition for a disgust expression = disgust intensity minus mean intensity [anger, fear, sadness, happiness, surprise]).
As both patients and controls had no problems with regard to the classification accuracy of emotion experience, this variable was not further considered in the analysis.
The study was conducted within the course of 1 day. In the morning, each participant underwent the first experiment (either emotion recognition or experience). After a break, each participant filled out the questionnaire set. In the afternoon, they underwent the second experiment. Since the emotion recognition experiment contains more stimuli (42) than the emotion experience experiment (24), the former was conducted in 2 parts with a break in between. Pretests had indicated that the rating of 42 stimuli was too exhausting for the patients. The maximum duration of the total experiment (recognition and experience) was 115.5 minutes.
To avoid position effects, the order of the 2 picture tasks (recognition v. experience), of the pictures and of the basic emotions to rate were randomized.
Image acquisition
We acquired T1-weighted anatomic scans using a 3-T Siemens Tim Trio system by means of a 3-dimensional magnetization-prepared rapid-acquisition gradient echo (3D-MPRAGE) sequence (0.8 × 0.8 × 2 mm; 104 transverse slices, repetition time 1300 ms, echo time 2.69 ms, inversion time 900 ms, flip angle 9°, overall duration 4:48 min) using a 12-channel head coil.
Voxel-based morphometry analysis
We analyzed brain imaging data using SPM8 (Statistical Parametric Mapping; Wellcome Trust Centre for Neuroimaging), including the VBM8 toolbox (revision 343, http://dbm.neuro.uni-jena.de/vbm) for VBM31 to gain voxel-wise comparisons of grey matter volume. Individual anatomic scans were partitioned into grey matter, white matter and cerebrospinal fluid (CSF) segments. An optimized blockwise nonlocal means denoising filter,32 a Hidden Markov Random Field approach,33 partial volume estimates34 and normalization to Montreal Neurological Institute (MNI) space by high-dimensional warping (DARTEL)35 with a standard template included in the VBM8 toolbox were used for preprocessing (final resolution 1.5 × 1.5 × 1.5 mm). To preserve brain volume and correct for individual head sizes already in the preprocessing steps of the data, we applied Jacobian modulation to tissue class segments for nonlinear normalization only. Finally, segments were smoothed by a Gaussian kernel (10-mm full-width at half-maximum).
Afterwards, we carried out statistical analyses using random-effects models. A 2-sample Student t test was computed to assess volume differences between patients and controls (comparisons: patients > controls and controls > patients). For group comparisons, we considered age and sex as covariates. Furthermore, to assess correlation of tissue class volume with self-report data, regression analyses were carried out using the following predictors: symptom duration (months), UHDRS motor score, UHDRS functional assessment score, UHDRS independence score, emotion recognition intensity, emotion experience intensity and classification accuracy of emotion recognition. In all analyses, we considered age and sex as covariates. The number of CAG triplets was highly correlated with age in our sample (r = −0.86, p < 0.001) and was therefore not further considered as a predictor or covariate in regression analyses.
For all random-effects analyses, modulated grey matter images were thresholded by a mask created from the grey matter a priori template included in the SPM8 distribution (threshold > 0.2). For exploratory analyses, statistical parametric maps were thresholded at p < 0.05, family wise error–corrected. For ROI analyses, SPMs were initially thresholded at an uncorrected p < 0.005. Peaks for voxel intensity tests of ROI analyses are reported if significant (p < 0.05, family wise error–corrected, small volume correction). Masks for ROI analyses were created for the amygdala, insula, OFC (all orbital parts of the frontal cortex), DLPFC, basal ganglia (caudate nucleus, putamen, pallidum) and hippocampus based on the parcellation by Tzourio-Mazoyer and colleagues36 and were created with the WFU Pickatlas.37
Results
Participants
The Huntington disease sample comprised 18 patients (8 women and 10 men) with a mean age of 51.9 (standard deviation [SD] 10.4) years. The study also included 18 controls (8 women and 10 men) with a mean age of 49.2 (SD 10.3) years. The demographic and clinical characteristics of participants are presented in Table 1.
Table 1.
Sample characteristics of patients with Huntington disease and healthy controls enrolled in a voxel-based morphometry study of emotion recognition and experience
| Group; mean (SD) [range]* | ||
|---|---|---|
| Characteristic | Huntington disease, n = 18 | Control, n = 18 |
| Sex, male:female | 10:8 | 10:8 |
| Age, yr | 51.9 (10.4) [32–63] | 49.2 (10.3) [34–64] |
| TFDD score | 38.2 (4.3) | 46.3 (2.3) |
| QADS score | 2.24 (0.92) | 1.98 (0.61) |
| STAI score | 36.10 (8.4) | 34.3 (8.3) |
| BDI score | 6.61 (6.89) | 4.50 (4.21) |
| CAG repeat length | 45.1 (2.8) [41–54] | NA |
| Symptom duration, mo | 47.9 (30.0) [6–109] | NA |
| UHDRS | ||
| Motor | 31 (17.9) | NA |
| Independence | 81.7 (16.2) | NA |
| Functional assessment | 20.1 (5.0) | NA |
| Total functional capacity | 9.6 (3.4) | NA |
BDI = Beck Depression Inventory;25 NA = not applicable; QADS = Questionnaire for the Assessment of Disgust Sensitivity;26 SD = standard deviation; STAI = State-Trait Anxiety Inventory;27 TFDD = Test for Early Detection of Dementia;28 UHDRS = Unified Huntington Disease Rating Scale.1
Unless otherwise indicated.
Neuropsychologic and affective tests
The UHDRS scales indicated mild-to-moderate symptom severity in patients with Huntington disease (Table 1). We observed a significant group difference for the TFDD (dementia screening), with patients scoring worse than controls (t34 = −7.04, p < 0.001).
Patients and controls obtained comparable scores for disgust proneness (QADS), trait anxiety (STAI) and depression (BDI; all p > 0.28; Table 1).
We calculated 1-sided Student t tests to examine our specific hypotheses that patients would score lower with respect to recognition intensity and classification accuracy of all negative emotions. To account for multiple comparisons, we used the method of Benjamini and Hochberg.38 In the facial emotion recognition task, patients gave reduced intensity ratings for displayed anger (t25.9 = 3.15, p = 0.002), disgust (t34 = 2.05, p = 0.024), sadness (t34 = 2.05, p = 0.025) and fear (t27.5 = 2.01, p = 0.027). The groups did not differ in the recognition of the positive emotions happiness (t26.7 = 1.41, p = 0.17) and surprise (t26.7 = 1.76, p = 0.09). Classification accuracy of emotion recognition was lower in patients for sadness (t34 = 5.50, p < 0.001), anger (t34 = 3.17, p = 0.002) and disgust (t34 = 2.46, p = 0.009), whereas no group differences occurred for fear and surprise (all p > 0.23). The patients showed better classification accuracy for happiness recognition than controls (t34 = 2.33, p = 0.026).
In the emotion experience experiment, groups gave comparable intensity ratings for experienced disgust, fear and happiness (all p > 0.22; Table 2).
Table 2.
Affective ratings of patients with Huntington disease and healthy controls enrolled in a voxel-based morphometry study of emotion recognition and experience
| Group; mean (SD) | ||
|---|---|---|
| Emotional affect | Huntington disease, n = 18 | Controls, n = 18 |
| Recognition (intensity) | ||
| Disgust | 5.61 (2.44) | 7.04 (1.67) |
| Anger | 5.45 (2.20) | 7.31 (1.17) |
| Fear | 5.11 (2.00) | 6.21 (1.18) |
| Sadness | 5.30 (2.27) | 6.57 (1.37) |
| Happiness | 7.81 (1.22) | 8.27 (0.68) |
| Surprise | 6.72 (2.16) | 7.75 (1.21) |
| Recognition (classification accuracy)* | ||
| Disgust | 1.51 (1.86) | 3.24 (2.34) |
| Anger | 1.85 (2.30) | 4.26 (2.27) |
| Fear | 1.19 (1.78) | 1.88 (1.59) |
| Sadness | 1.83 (2.46) | 5.62 (1.58) |
| Happiness | 5.33 (1.70) | 3.73 (2.36) |
| Surprise | 3.71 (2.54) | 4.65 (2.09) |
| Experience (intensity)† | ||
| Disgust | 6.28 (2.33) | 6.20 (1.19) |
| Fear | 6.41 (2.11) | 7.02 (1.36) |
| Happiness | 7.51 (1.89) | 7.50 (1.00) |
SD = standard deviation.
Classification accuracy is the difference between target emotion intensity and mean intensity of nontarget emotions.
Emotion intensity: 1 = weak; 9 = strong.
Imaging data
Groups differed in total grey matter volume (t34 = 5.33, p < 0.001; Mp = 472 mL; Mc = 568 mL), white matter volume (t34 = 2.71, p = 0.010; Mp = 554 mL; Mc = 610 mL) and CSF volume (t34 = 6.20, p < 0.001; Mp = 315 mL; Mc = 240 mL), indicating total grey and white matter volume decreases and CSF increases in patients compared with controls. The groups did not differ with respect to total intracranial volume (grey matter + white matter + CSF; Mp = 1341 mL; Mc = 1417 mL; t34 = 1.86; p = 0.07).
The “controls > patients” contrast showed significant exploratory effects (all p < 0.05, family wise error–corrected) for the bilateral amygdala (left: t = 6.50, MNI x, y, z = −24, −1, −14; right: t = 9.46, MNI x, y, z = 28, 0, −12), the bilateral basal ganglia (including the caudate nucleus, putamen and globus pallidus; left: t = 16.71, MNI x, y, z = −9, 15, 6; right: t = 17.58, MNI x, y, z = 12, 16, 3), the bilateral DLPFC (left: t = 5.55, MNI x, y, z = −27, 44, 16; right: t = 5.56, MNI x, y, z = 21, −4, 54), the right hippocampus (t = 8.74, MNI x, y, z = 32, −7, −14), the bilateral insula (left: t = 8.16, MNI x, y, z = −45, −13, 3; right: t = 7.01, MNI x, y, z = 27, 20, −9) and the left OFC (t = 6.96, MNI x, y, z = −16, 17, −12).
Grey matter volume reduction and emotion recognition and experience
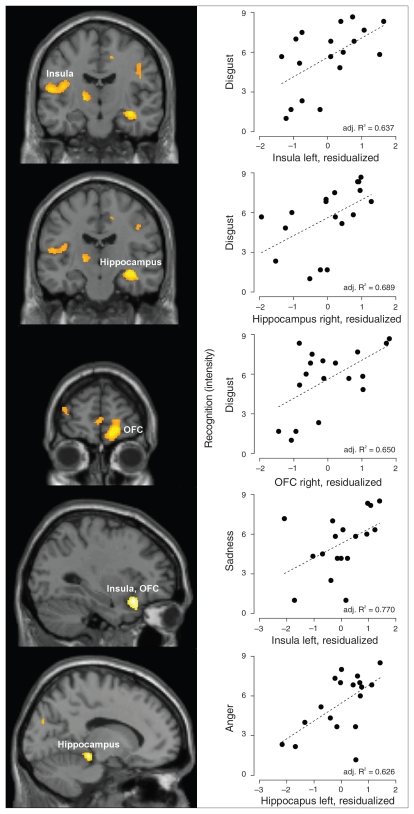
In patients, reduced emotion recognition intensity for disgust was associated with lower grey matter volume in the insula, the OFC and the hippocampus. The extent of classification accuracy for disgust correlated negatively with the grey matter volume in the hippocampus, amygdala and DLPFC. Diminished intensity ratings for expressed anger and happiness were associated with reduced grey matter volume in the hippocampus. Emotion recognition intensity for sadness correlated negatively with the grey matter volume in the insula and the OFC, whereas lower intensity of surprise went along with lower volume in the DLPFC and hippocampus. Lower classification accuracy for recognized surprise was associated with reduced grey matter volume in the amygdala.
We observed an association between grey matter volume and emotion experience intensity for fear and disgust involving the hippocampus and the DLPFC (Table 3, Fig. 1).
Table 3.
Location of maxima for regions with loss of grey matter volume associated with impaired emotion recognition and emotion experience in patients with Huntington disease
| Impaired emotion recognition; brain region | Side | MNI coordinate | t | p value* | ||
|---|---|---|---|---|---|---|
| x | y | z | ||||
| Emotion recognition | ||||||
| Disgust recognition/intensity | ||||||
| Hippocampus | L | −36 | −30 | −11 | 4.70 | 0.016 |
| Hippocampus | R | 36 | −16 | −12 | 5.69 | 0.004 |
| Insula | L | −40 | −13 | 15 | 4.68 | 0.030 |
| Insula | R | 40 | −7 | 22 | 4.35 | 0.046 |
| OFC | R | 16 | 58 | −9 | 5.58 | 0.025 |
| Disgust recognition/classification accuracy | ||||||
| Amygdala | L | −21 | −9 | −17 | 3.09 | 0.048 |
| DLPFC | L | −44 | 36 | 28 | 6.95 | 0.006 |
| Hippocampus | R | 40 | −18 | −17 | 5.22 | 0.007 |
| Anger recognition/intensity | ||||||
| Hippocampus | L | −14 | −28 | −11 | 3.85 | 0.05 |
| Sadness recognition/intensity | ||||||
| Insula | L | −30 | 20 | −20 | 5.51 | 0.009 |
| OFC | L | −32 | 21 | −21 | 5.68 | 0.020 |
| Surprise recognition/intensity | ||||||
| DLPFC | L | −16 | −4 | 78 | 5.31 | 0.045 |
| Hippocampus | L | −18 | −30 | −8 | 4.19 | 0.032 |
| Hippocampus | R | 22 | −28 | −8 | 4.04 | 0.040 |
| Surprise recognition/classification accuracy | ||||||
| Amygdala | L | −27 | −3 | −12 | 3.04 | 0.049 |
| Happiness recognition/intensity | ||||||
| Caudate | L | −8 | 0 | 13 | 4.13 | 0.033 |
| Hippocampus | R | 33 | −28 | −11 | 4.25 | 0.029 |
| Emotion experience | ||||||
| Fear experience/intensity | ||||||
| Hippocampus | L | −30 | −25 | −9 | 4.18 | 0.032 |
| Hippocampus | R | 30 | −18 | −12 | 6.60 | 0.001 |
| Disgust experience/intensity | ||||||
| DLPFC | L | −12 | 45 | 30 | 5.79 | 0.025 |
| Hippocampus | L | −12 | −39 | 10 | 4.42 | 0.023 |
| Hippocampus | R | 14 | −39 | 10 | 4.52 | 0.021 |
DLPFC = dorsolateral prefrontal cortex; L = left; MNI = Montreal Neurological Institute; OFC = orbitofrontal cortex; R = right.
Family wise error–corrected.
Fig. 1.
Correlations between grey matter volume reduction in regions of interest and lowered intensity ratings for displayed facial affect in symptomatic patients with Huntington disease. OFC = orbitofrontal cortex.
In the control group, correlations between grey matter volume and rated emotion recognition intensity and classification accuracy did not reach significance for any ROI.
Grey matter volume and symptom severity
Whereas different indicators of symptom severity (symptom duration, UHDRS motor score) showed no association with grey matter volume, the UHDRS functionality subscales (functional assessment, independence, total functional capacity delete) were good predictors of neuronal loss in ROIs. The independence score and the functional capacity score correlated negatively with grey matter volume in the amygdala and DLPFC. The total functional assessment score showed a negative association with grey matter volume in the amygdala and basal ganglia structures (putamen, caudate nucleus), the hippocampus and the DLPFC (Table 4).
Table 4.
Location of maxima for regions with loss of grey matter volume correlated with decreased functionality scores of the UHDRS
| UHDRS subscale; brain region | Side | MNI coordinate | t | p value* | ||
|---|---|---|---|---|---|---|
| x | y | z | ||||
| Independence | ||||||
| Amygdala | L | −22 | −9 | −12 | 3.58 | 0.024 |
| DLPFC | L | −26 | 51 | 21 | 5.50 | 0.038 |
| DLPFC | R | 26 | 45 | 22 | 7.34 | 0.004 |
| Functional assessment | ||||||
| Amygdala | L | −27 | −9 | −12 | 3.78 | 0.018 |
| Caudate | L | −12 | 14 | −12 | 4.00 | 0.043 |
| DLPFC | L | −22 | 68 | 10 | 6.23 | 0.015 |
| DLPFC | R | 27 | 46 | 24 | 6.79 | 0.008 |
| Hippocampus | L | −28 | −10 | −12 | 3.97 | 0.046 |
| Putamen | L | −27 | −1 | 10 | 4.54 | 0.020 |
| Putamen | R | 27 | −9 | 12 | 4.22 | 0.033 |
| Total functional capacity | ||||||
| Amygdala | L | −30 | 5 | −18 | 3.61 | 0.022 |
| DLPFC | R | 18 | 66 | 25 | 6.36 | 0.013 |
DLPFC = dorsolateral prefrontal cortex; L = left; MNI = Montreal Neurological Institute; R = right; UHDRS = Unified Huntington Disease Rating Scale.1
Family wise error–corrected.
Discussion
This VBM study focused on the neuroanatomy of affect recognition and experience in symptomatic patients with Huntington disease. Relative to healthy controls, the patients gave significantly lower intensity ratings for facial expressions of disgust, sadness, fear and anger. Thus, all negative emotions were affected, whereas the recognition of the positive emotions happiness and surprise was similar in both groups. This finding is in line with most previous reports on presymptomatic and symptomatic patients with Huntington disease, in which the afflicted individuals showed recognition impairments for at least 2 negative emotions and no specific disgust recognition deficit.9,12–15
Besides the decrease in negative emotion recognition intensity, the patients showed lowered classification accuracy for sadness, anger and disgust. For these negative emotions, they gave higher intensity ratings for nontarget emotions. This reflects uncertainty in affect identification, which was comparably poor for these 3 emotions. Yet, the accuracy for happiness recognition was higher among patients with Huntington disease than controls. Thus, the patients were not characterized by a response set with a general tendency to choose nontarget emotions in their affective ratings.
The reduced negative emotion recognition intensity was associated with reduced grey matter volumes in ROIs. Patients’ lowered intensity estimates for facial disgust were related to lower grey matter volume in the insula, OFC and hippocampus. At first glance, this finding might be interpreted as a link between the ability to recognize disgust and a region that has been previously characterized as a specific neural processor of this emotion, namely the insula.18,19 However, in the clinical group, grey matter volume in the insula was also associated with sadness identification. Insular-orbitofrontal grey matter reduction correlated with poor recognition of this emotion. Thus, a selective role of the insula in disgust identification could not be identified in our study. Rather, our data point to a more general role of both brain regions for affective processing, such as a central representation of arousal or negative affectivity (insula) and valence assignment to emotive stimuli or response modulation (OFC).3,19,21
Across different emotions, lower intensity ratings for displayed facial affect were associated with reduced grey matter volume in the hippocampus (disgust, anger, surprise, happiness). Moreover, lower grey matter volumes in the DLPFC were implicated in recognition deficits (lowered intensity and accuracy of emotion recognition) for disgust and surprise. These correlations may be the result of the specific demand of the rating task. Subsequent to the presentation of each picture, the participants had to judge the intensities of 6 basic emotions. This task requires that a mental representation of the picture has to be kept in working memory (DLPFC) and is compared with the episodic representation of the emotional significance of this stimulus (hippocampus). Thus, it seems logical that memory-related brain structures can influence affective ratings.39 This interpretation is, however, not sufficient to explain the difference in recognition performance between positive and negative emotions and associated brain atrophy. As the rating procedure was identical for all emotion categories, attentional and memory demands were also comparable.
Besides the memory-related functions of the DLPFC, a more specific role in affective processing for this ROI has also been suggested: it has been put forward that the DLPFC is relevant for responses to aversive and especially to socially relevant stimuli.40 The social relevance of negative facial expressions needs no further elaboration. They signal to interrupt or change ongoing behaviour. Findings of previous studies already have demonstrated that communication and psychosocial well-being are strongly affected in patients with Huntington disease.41,42
Finally, grey matter volume in the DLPFC was associated with all UHDRS subscales with the exception of the motor scale. Impairments in daily life performance (e.g., no engagement in occupation, lowered capacity to handle financial affairs) went along with reduced grey matter volume in the DLPFC. This finding supports the interpretation of a primarily cognitive DLPFC function that modulates other processes (emotional and nonemotional). A similar interpretation can be given for the observed amygdala effect. Reduced grey matter volume in the amygdala was associated with greater functional impairment (UHDRS) and lower classification accuracy (disgust, surprise) in patients with Huntington disease relative to controls. As the amygdala is crucial for the normal facilitation of attention for emotional stimuli and associated memory encoding, amygdalar atrophy will interfere with these functions.39
It has to be stressed that all patients with Huntington disease were nondepressed and nondemented, which implies that their overall cognitive–emotional impairment had been judged as not clinically relevant. Nonetheless, early changes in DLPFC (amygdala, hippocampus) function and structure might be important for the understanding of early symptoms of Huntington disease.6
In contrast to affect recognition, emotion experience showed no changes in patients with Huntington disease. Patients and controls gave comparable affective ratings for scenes eliciting disgust, fear and happiness. Moreover, they reported similar habitual affective reactivity (e.g., disgust proneness, trait anxiety). To our knowledge, our VBM study is the first to identify dissociation between deficits in emotion recognition and emotion experience for symptomatic patients with Huntington disease. The reason that experience was not (yet) affected in the patient group might be related to the fact that emotional feeling is a more basal process than recognition. For example, fear-relevant scenes pose a direct threat to the viewer, whereas facial expressions of fear indicate indirect threat. The decoding of socially relevant facial information might be less automated than the elicitation of feelings. Moreover, the differentiation of negative facial expressions with similar features (e.g., anger v. disgust) is of great social relevance, as both expressions imply different behaviours in the receiver (submission or aggression v. withdrawal). Consequently, our data suggest the development of new supplementary symptom management strategies for patients with Huntington disease with mild and moderate clinical symptoms (e.g., emotion or empathy training programs or the teaching of alternative strategies for the decoding of negative emotion cues).
The only distinct feature in patients with Huntington disease in our study concerned a correlation between reduced grey matter volume in the DLPFC and hippocampus and reduced experienced intensity of disgust and fear. This grey matter volume effect is most likely not directly related to emotional processing but reflects the influence of cognitive impairment on affective reactivity.
Limitations
As a limitation of our study, we have to mention the small sample size and the resulting modest statistical power relative to the number of tests. Moreover, the restriction of affect recognition deficits to negative emotions, as displayed by patients with Huntington disease, might not only be a consequence of an affective dysfunction but also of variations in task difficulty. It is generally accepted that happiness and surprise are emotions that are easy to categorize, whereas the correct labelling of certain negative facial emotions with similar features (e.g., disgust and anger) is more difficult.12,14
In the future, a direct investigation of the interaction of cognitive–affective processes seems promising. Such a focus might also help us understand the contradicting findings of our investigation and a previous VBM study on affect recognition in patients with Huntington disease.14 Here, problems in negative affect recognition were assessed by means of a forced-choice paradigm (with smaller attention–memory demands) and predominantly involved striatal structures. However, in the natural environment, facial emotional signals are often displayed very briefly and thus have to be kept in memory to guide one’s behaviour adequately. Thus, we believe that our design has a high ecologic validity.
Conclusion
Altogether, patients with Huntington disease showed clear impairment in negative emotion recognition intensity and accuracy, which was associated with changes in grey matter volume in emotion-relevant (insula, OFC) and memory-or attention-related structures (DLPFC, hippocampus). Therefore, our study sheds new light on the importance of cognitive processes on affect recognition in patients with Huntington disease.
Acknowledgements
This study was supported by the Austrian Science Fund (FWF), project number P20779-B02.
Footnotes
Competing interests: See above for Drs. Ille, Schäfer and Schienle and Mr. Scharmüller. None declared for Drs. Enzinger, Schöggl and Kapfhammer.
Contributors: Dr. Schienle designed the study. Drs. Ille, Schöggl and Kapfhammer and Mr. Scharmüller acquired the data, which Drs. Ille, Schäfer, Enzinger and Schienle and Mr. Scharmüller analyzed. Dr. Schienle wrote the article, which all authors reviewed and approved for publication.
References
- 1.Huntington Study Group. Unified Huntington’s Disease Rating Scale: reliability and consistency. Mov Disord. 1996;11:136–42. doi: 10.1002/mds.870110204. [DOI] [PubMed] [Google Scholar]
- 2.Nehl C, Ready RE, Hamilton J, et al. Effects of depression on working memory in presymptomatic Huntington’s disease. J Neuropsychiatry Clin Neurosci. 2001;13:342–6. doi: 10.1176/jnp.13.3.342. [DOI] [PubMed] [Google Scholar]
- 3.Hennenlotter A, Schroeder U, Erhard P, et al. Neural correlates associated with impaired disgust processing in pre-symptomatic Huntington’s disease. Brain. 2004;127:1446–53. doi: 10.1093/brain/awh165. [DOI] [PubMed] [Google Scholar]
- 4.Zakzanis KK. The subcortical dementia of Huntington’s disease. J Clin Exp Neuropsychol. 1998;20:565–78. doi: 10.1076/jcen.20.4.565.1468. [DOI] [PubMed] [Google Scholar]
- 5.Feigin A, Ghilardi MF, Huang C, et al. Preclinical Huntington’s disease: compensatory brain responses during learning. Ann Neurol. 2006;59:53–9. doi: 10.1002/ana.20684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wolf RC, Vasic N, Schönfeldt-Locuona C, et al. Dorsolateral pre-frontal cortex dysfunction in presymptomatic Huntington’s disease: evidence from event-related fMRI. Brain. 2007;130:2845–57. doi: 10.1093/brain/awm210. [DOI] [PubMed] [Google Scholar]
- 7.Douaud G, Gaura V, Ribeiro MJ, et al. Distribution of grey matter atrophy in Huntington’s disease patients: a combined ROI-based and voxel-based morphometric study. Neuroimage. 2006;32:1562–75. doi: 10.1016/j.neuroimage.2006.05.057. [DOI] [PubMed] [Google Scholar]
- 8.Hobbs NZ, Henley SM, Ridgway GR, et al. The progression of regional atrophy in premanifest and early Huntington’s disease: a longitudinal voxel-based morphometry study. J Neurol Neurosurg Psychiatry. 2010;81:756–63. doi: 10.1136/jnnp.2009.190702. [DOI] [PubMed] [Google Scholar]
- 9.Johnson SA, Stout JC, Solomon AC, et al. Beyond disgust: impaired recognition of negative emotions prior to diagnosis in Huntington’s disease. Brain. 2007;130:1732–44. doi: 10.1093/brain/awm107. [DOI] [PubMed] [Google Scholar]
- 10.Gray JM, Young AW, Barker WA, et al. Impaired recognition of disgust in Huntington’s disease gene carriers. Brain. 1997;120:2029–38. doi: 10.1093/brain/120.11.2029. [DOI] [PubMed] [Google Scholar]
- 11.Sprengelmeyer R, Schroeder U, Young AW, et al. Disgust in pre-clinical Huntington’s disease: a longitudinal study. Neuropsychologia. 2006;44:518–33. doi: 10.1016/j.neuropsychologia.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 12.Milders M, Crawford JR, Lamb A, et al. Differential deficits in expression recognition in gene-carriers and patients with Huntington’s disease. Neuropsychologia. 2003;41:1484–92. doi: 10.1016/s0028-3932(03)00079-4. [DOI] [PubMed] [Google Scholar]
- 13.Montagne B, Kessels RP, Kammers MP, et al. Perception of emotional facial expressions at different intensities in early-symptomatic Huntington’s disease. Eur Neurol. 2006;55:151–4. doi: 10.1159/000093215. [DOI] [PubMed] [Google Scholar]
- 14.Henley SM, Wild EJ, Hobbs NZ, et al. Defective emotion recognition in early HD is neuropsychologically and anatomically generic. Neuropsychologia. 2008;46:2152–60. doi: 10.1016/j.neuropsychologia.2008.02.025. [DOI] [PubMed] [Google Scholar]
- 15.Snowden JS, Austin NA, Sembi S, et al. Emotion recognition in Huntington’s disease and frontotemporal dementia. Neuropsychologia. 2008;46:2638–49. doi: 10.1016/j.neuropsychologia.2008.04.018. [DOI] [PubMed] [Google Scholar]
- 16.Sprengelmeyer R, Young AW, Calder AJ, et al. Loss of disgust. Perception of faces and emotions in Huntington’s disease. Brain. 1996;119:1647–65. doi: 10.1093/brain/119.5.1647. [DOI] [PubMed] [Google Scholar]
- 17.Wang K, Hoosain R, Yang RM, et al. Impairment of recognition of disgust in Chinese with Huntington’s or Wilson’s disease. Neuropsychologia. 2003;41:527–37. doi: 10.1016/s0028-3932(02)00171-9. [DOI] [PubMed] [Google Scholar]
- 18.Phillips ML, Young AW, Senior C, et al. A specific neural substrate for perceiving facial expressions of disgust. Nature. 1997;389:495–8. doi: 10.1038/39051. [DOI] [PubMed] [Google Scholar]
- 19.Sprengelmeyer R, Rausch M, Eysel UT, et al. Neural structures associated with recognition of facial expressions of basic emotions. Proc Biol Sci. 1998;265:1927–31. doi: 10.1098/rspb.1998.0522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kipps CM, Duggins AJ, McCusker EA, et al. Disgust and happiness recognition correlate with anteroventral insula and amygdala volume respectively in preclinical Huntington’s disease. J Cogn Neurosci. 2007;19:1206–17. doi: 10.1162/jocn.2007.19.7.1206. [DOI] [PubMed] [Google Scholar]
- 21.Schienle A, Stark R, Walter B, et al. The insula is not specifically involved in disgust processing: an fMRI study. Neuroreport. 2002;13:2023–6. doi: 10.1097/00001756-200211150-00006. [DOI] [PubMed] [Google Scholar]
- 22.Hayes CJ, Stevenson RJ, Coltheart M. Disgust and Huntington’s disease. Neuropsychologia. 2007;45:1135–51. doi: 10.1016/j.neuropsychologia.2006.10.015. [DOI] [PubMed] [Google Scholar]
- 23.Schäfer A, Schienle A, Vaitl D. Emotion-related brain activation depends upon stimulus type and design. Int J Psychophysiol. 2005;57:53–9. doi: 10.1016/j.ijpsycho.2005.01.011. [DOI] [PubMed] [Google Scholar]
- 24.Schienle A, Walter B, Schaefer A, et al. Neural responses of OCD patients towards disorder-relevant, generally disgust-inducing and fear-inducing pictures. Int J Psychophysiol. 2005;57:69–77. doi: 10.1016/j.ijpsycho.2004.12.013. [DOI] [PubMed] [Google Scholar]
- 25.Hautzinger M, Bailer M, Worall H, et al. Beck Depression Inventory [German version] Bern (Germany): Huber; 1994. [Google Scholar]
- 26.Schienle A, Stark R, Walter B, et al. The insula is not specifically involved in disgust processing: an fMRI study. Neuroreport. 2002;13:2023–6. doi: 10.1097/00001756-200211150-00006. [DOI] [PubMed] [Google Scholar]
- 27.Laux L, Glanzmann P, Spielberger CD. State Trait Angstinventar (STAI) Weinheim (Germany): Beltz Testgesellschaft; 1981. [Google Scholar]
- 28.Ihl R, Grass-Kapanke B, Lahrem P, et al. Development and validation of a test for early diagnosis of dementia with differentiation from depression (TFDD) Fortschr Neurol Psychiatr. 2000;68:413–22. doi: 10.1055/s-2000-11799. [DOI] [PubMed] [Google Scholar]
- 29.Lundquist D, Flykt A, Öhman A. The Karolinska Directed Emotional Faces. Stockholm (Sweden): Department of Clinical Neuroscience, Psychology section, Karolinska Institutet; 1998. [Google Scholar]
- 30.Lang PJ, Bradley M, Cuthbert B. International Affective Picture System. Gainsville (FL): Center for Research in Psychophysiology, University of Florida; 2001. [Google Scholar]
- 31.Ashburner J, Friston K. Voxel-based morphometry — the methods. Neuroimage. 2000;11:805–21. doi: 10.1006/nimg.2000.0582. [DOI] [PubMed] [Google Scholar]
- 32.Coupe P, Yger P, Prima S, et al. An optimized blockwise nonlocal means denoising filter for 3-D magnetic resonance images. IEEE Trans Med Imaging. 2008;27:425–41. doi: 10.1109/TMI.2007.906087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rajapakse JC, Giedd JN, Rapoport JL. Statistical approach to segmentation of single-channel cerebral MR images. IEEE Trans Med Imaging. 1997;16:176–86. doi: 10.1109/42.563663. [DOI] [PubMed] [Google Scholar]
- 34.Tohka J, Zijdenbos A, Evans A. Fast and robust parameter estimation for statistical partial volume models in brain MRI. Neuroimage. 2004;23:84–97. doi: 10.1016/j.neuroimage.2004.05.007. [DOI] [PubMed] [Google Scholar]
- 35.Ashburner J. A fast diffeomorphic image registration algorithm. Neuroimage. 2007;38:95–113. doi: 10.1016/j.neuroimage.2007.07.007. [DOI] [PubMed] [Google Scholar]
- 36.Tzourio-Mazoyer N, Landeau B, Papathanassiou D, et al. Automated anatomical labeling of activations in SPM using a macroscopic anatomical parcellation of the MNI MRI single-subject brain. Neuroimage. 2002;15:273–89. doi: 10.1006/nimg.2001.0978. [DOI] [PubMed] [Google Scholar]
- 37.Maldjian JA, Laurienti PJ, Burdette JB, et al. An automated method for 355 neuroanatomic and cytoarchitectonic atlas-based interrogation of fMRI data sets. 356. Neuroimage. 2003;19:1233–9. doi: 10.1016/s1053-8119(03)00169-1. [DOI] [PubMed] [Google Scholar]
- 38.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Statist Soc B. 1995;57:289–300. [Google Scholar]
- 39.Phelps EA. Human emotion and memory: interactions of the amygdala and hippocampal complex. Curr Opin Neurobiol. 2004;14:198–202. doi: 10.1016/j.conb.2004.03.015. [DOI] [PubMed] [Google Scholar]
- 40.Moll J, de Oliveira-Souza R. Moral judgements, emotions and the utilitarian brain. Trends Cogn Sci. 2007;11:319–21. doi: 10.1016/j.tics.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 41.Helder DI, Kaptein AA, van Kempen GM, et al. Impact of Huntington’s disease on quality of life. Mov Disord. 2001;16:325–30. doi: 10.1002/mds.1056. [DOI] [PubMed] [Google Scholar]
- 42.Hartelius L, Jonsson M, Rickeberg A, et al. Communication and Huntington’s disease: qualitative interviews and focus groups with persons with Huntington’s disease, family members, and carers. Int J Lang Commun Disord. 2010;45:381–93. doi: 10.3109/13682820903105145. [DOI] [PubMed] [Google Scholar]