Abstract
Little is known about intracerebral hemorrhage (ICH) patients who undergo chronic life sustaining procedures. We sought to explore variation in treatment, Medicare payments and mortality among elderly ICH patients who received feeding tube, tracheostomy or neither chronic life sustaining procedure. Medicare Provider Analysis and Review (MedPAR) files from 2004 linked to Center for Medicaid and Medicare Services (CMS) denominator files through January 2005 were analyzed. Patients over 65 with primary diagnosis of ICH based on discharge codes (ICD-9-CM 431) were divided into those who underwent tracheostomy, feeding tube placement but not tracheostomy, or neither procedure. Thirty-day and one-year survival were estimated with Kaplan-Meier methods. Among the 32,210 patients, 6% underwent feeding tube placement while 2.5% underwent tracheostomy. Compared to patients who did not undergo a chronic life sustaining procedure, those who underwent tracheostomy had longer length of stay (median 25 vs. 4 days, p<0.01) and greater Medicare spending (median $81,479 vs. $6,008, p<0.01) during their initial hospitalization. Among patients who did not undergo a chronic life sustaining procedure 30-day and 1-year cumulative mortality risks were 47% and 59%. Among patients who underwent feeding tube placement, 30-day and 1-year cumulative mortality risks were 21% and 53% and, for those who underwent tracheostomy, 19% and 65%, respectively (p<0.01, log rank test across the three groups). One-year mortality among elderly ICH patients is high even among patients who receive chronic life sustaining procedures. Medicare payments for patients who undergo tracheostomy are substantial. More information about functional outcomes is needed.
Keywords: Intracerebral Hemorrhage, survivors, aging, mortality, payment, procedures
Over 70,000 cases of intracerebral hemorrhage (ICH) occur annually in the United States, of which approximately half occur in individuals over the age of 65.1, 2 The incidence of ICH increases exponentially with age.3 Over the last decade, hospital admissions for ICH have increased by almost 20%, in part, due to the aging of the population.4, 5
Recent studies have raised the concern that ICH predictive models may be flawed due to confounding by withdrawal of support and early do-not-resuscitate (DNR) orders.6-8 After controlling for demographic and clinical variables, one of the strongest predictors of ICH mortality is limitation in medical care. For this reason, the recent American Heart Association guidelines recommend aggressive full care early after ICH onset and postponement of new DNR orders until at least the second full day of hospitalization.9 However, little is known about patients who undergo aggressive full care which often results in feeding tube or tracheostomy placement. Likewise, little is known about medium and long-term outcomes of these patients since most ICH predictive models have traditionally focused on mortality 30 days from the initial event. 10, 11
We present a national-level perspective of acute care patterns and survival of elderly ICH patients who underwent a chronic life sustaining procedure--feeding tube and/or tracheostomy placement. In particular, we sought to describe the variation in acute hospitalizations, Medicare payments and one-year mortality following ICH admission as a function of whether or not these procedures were performed. These data provide an essential foundation for policy-makers, families and physicians who make decisions about how to manage this growing and understudied disease.
Methods
Data Source
Patient-level data from Centers for Medicare & Medicaid Services (CMS) Medicare Provider Analysis and Review (MedPAR) files were obtained from October 2003 through September 2004. The MedPAR files contain patient level hospitalization data including demographics, primary and secondary discharge diagnosis codes, procedure codes, discharge location and Medicare payment data for all fee-for-service Medicare beneficiaries. We linked MedPAR data to CMS Denominator files using unique patient identifiers to allow us to determine the long-term mortality of individuals through January 1, 2005.
Study Population
Patients over age 65 who were hospitalized with a primary diagnosis of ICH, defined as International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM) code 431,were included in this study.12-14 ICD 9-CM code 430 (subarachnoid hemorrhage) and ICD 9-CM code 432 (other and unspecified intracranial hemorrhage) were excluded. The analysis was limited to the index hospitalization for ICH. To account for acute transfers to higher level of care hospitals, the second hospital admission was used if the patient had two hospital admissions on the same day or separated by one day.
Feeding tube placement was identified by ICD-9-CM procedure codes: 43.11, 43.19, 44.32 and tracheostomy placement was identified by Diagnosis Related Group (DRG) code 483.15-17 We used the Quan implementation of the Charlson index to assess the co-morbidity burden.18 However, we removed the codes of hemiplegia and cerebrovascular disease because of likely poor reliability in the context of a known ICH. 19 Coma was idenfified by ICD-9-CM 780.01 and 780.09. To better understand the acute care provided to elderly ICH patients during their hospitalization, we explored other procedures specific to ICH including mechanical ventilation (96.70, 96.71, 96.72 or tracheostomy DRG), craniotomy (1.39, 1.24, 1.59, 1.31) and ventriculostomy (2.2, 2.39).20 Discharge location data were obtained from the MedPAR discharge destination field.21
Statistical Analysis
For all analyses, the patients were divided into 3 groups based on their receipt of a chronic life sustaining procedure: 1) patients who did not undergo chronic life sustaining procedures; 2) patients who underwent feeding tube placement; 3) patients who underwent tracheostomy with or without feeding tube placement. Preliminary analyses showed that patients who received a feeding tube and tracheostomy had outcomes that more closely resembled patients who received only a tracheostomy as compared to patients who received only a feeding tube. Additionally, there was no statistically significant difference between patients who received a tracheostomy and patients who received both a feeding tube and tracheostomy with respect to age, gender and Charlson stroke co-morbidity index (see Supplementary Appendix). For these reasons, patients who received a feeding tube and tracheostomy were combined with patients who received only a tracheostomy.
Two sets of bivariate comparisons were made.22 Patients who underwent no chronic life sustaining procedures were compared to patients who underwent feeding tube placement and patients who underwent no chronic life sustaining procedures were compared to patients who underwent a tracheostomy. This approach was chosen to highlight differences between patients who did not undergo a chronic life sustaining procedure and those who underwent either tracheostomy or feeding tube placement rather than to explore differences between the three groups of patients. Categorical variables including gender, race/ethnicity, Charlson stroke co-morbidity index, acute care procedures and discharge location were analyzed using x2 tests. Age, length of stay, and total Medicare payments for the acute hospitalization were evaluated using Wilcoxon rank sum.
We used Kaplan-Meier methods and log rank testing to perform a survival analysis of all-cause mortality through 1 year, stratified by presence of chronic life sustaining procedure. Patients who did not undergo a chronic life sustaining procedure are likely a mixed population of those with mild ICH where these procedures were not indicated and patients with severe ICH who required but did not undergo chronic life sustaining treatment. Therefore, a second survival analysis was performed restricted to patients who were discharged alive in an attempt to remove patients who had required but did not receive chronic life sustaining treatments. Survival time in days was from the date of the index ICH hospitalization to the date of death. Patients who were still alive were censored at one year after admission or at the end of the study period (January 1, 2005), whichever came first. All statistical tests were 2-tailed and the probability of Type 1 error was set at 0.05. Stata software version 11 (StataCorp, College Station, Texas) was used for all analysis. This study was approved by the University of Michigan Institutional Review Board.
Results
The study population included 32,210 Medicare patients admitted for ICH during fiscal year 2004. One patient was excluded for invalid Medicare payment data. Six percent of patients (n=2,076) underwent feeding tube placement, 2.5% (n= 812) received a tracheostomy while the remaining 91% (n=29,322) did not undergo chronic life sustaining procedures. Compared with patients who did not undergo a chronic life sustaining procedure, patients who received a tracheostomy were younger (median age, 75± 11 vs. 80±11, p<0.01), more likely to be African American (p<0.01) and male (p<0.01) (Table 1, first panel). Patients who underwent feeding tube placement were more likely to be African American (p<0.01) compared to patients who did not undergo a life sustaining procedure.
Table 1.
Demographics, clinical characteristics, Medicare payments and hospital disposition of Medicare Beneficiaries Hospitalized for ICH.
| Variable | Patients receiving no chronic life sustaining procedure (n=29,322) | Patients receiving feeding tube (n= 2,076) | P value for no procedure vs. feeding tube | Patients receiving tracheostomy (n= 812) | P value for no procedure vs. tracheostomy |
|---|---|---|---|---|---|
| Age, years, median (IQR) | 80±11 | 80±10 | 0.71 | 75±11 | <0.01 |
| Male | 43 % | 45 % | 0.14 | 57 % | <0.01 |
| Race/Ethnicity | |||||
| Caucasian | 85 % | 77 % | <0.01 | 70 % | <0.01 |
| Black | 9 % | 16 % | 22 % | ||
| Other | 6 % | 7 % | 7 % | ||
| High Modified Charlson Score | 16 % | 17 % | 0.57 | 16 % | 0.62 |
| Coma | 7 % | 4 % | <0.01 | 6 % | 0.456 |
| Ventilator | 22 % | 19 % | <0.01 | NA | |
| Craniotomy | 4 % | 10 % | <0.01 | 31 % | <0.01 |
| Ventriculostomy | 3 % | 6 % | <0.01 | 29 % | <0.01 |
| LOS, median (IQR) | 4 ±5days | 14 ±10days | <0.01 | 25 ±18days | <0.01 |
| Medicare Payments, median (IQR) | $ 6,008 ±2,217 | $6,786 ±5,927 | <0.01 | $ 81,479 ±49,354 | <0.01 |
| Discharge Location | <0.01 | <0.01 | |||
| Home | 19 % | 7 % | 2 % | ||
| Inpatient Rehab | 14 % | 12 % | 10 % | ||
| Skilled Nursing Facility | 22 % | 62 % | 29 % | ||
| Long term Care Facility | 1 % | 6 % | 29 % | ||
| Hospice | 5 % | 3 % | 3 % | ||
| In hospital Mortality | 36 % | 8 % | 20 % | ||
| Other | 4 % | 2 % | 8 % |
The proportion of patients undergoing ventriculostomy was different for patients who did not undergo a chronic life sustaining procedure compared to those who received a tracheostomy (p<0.01) or feeding tube (p<0.01). Similar findings were noted for the proportion of patients undergoing craniotomy (Table 1, second panel).
Differences in length of stay and Medicare payment were also noted (Table 1, third panel). Compared with patients who did not undergo a chronic life sustaining procedure, patients who received a tracheostomy had higher median Medicare payment ($81,479 vs. $6,008, p<0.01) and median length of stay (25 vs. 4 days, p<0.01) for the initial hospitalization. This finding was also true when comparing patients who received a feeding tube compared to patients who did not undergo a chronic life sustaining procedure (14 vs. 4 days, p<0.01) and median Medicare payment ($6,786 vs. $6,008, p<0.01) for the initial hospitalization. Medicare payments and length of stay among patients who died during their hospitalization were also examined. Median Medicare payment for patients who underwent tracheostomy before their in-hospital death was substantially higher ($ 98,368 vs. $6,066, p<0.01) and median length of stay was longer (23 vs. 2 days, p<0.01) than for patients who did not undergo a chronic life sustaining procedure. The same was true for patients who underwent feeding tube placement ($7,132 vs. $6,066, p<0.01) and median length of stay (14 days vs. 2 days, p<0.01) compared to patients who did not undergo a chronic life sustaining procedure.
Discharge locations differed among patients (Table 1, fourth panel). Nineteen percent of patients who did not undergo a chronic life sustaining procedure were discharged to home, compared to only 7% of patients who underwent feeding tube placement (p<0.01) and 2% of patients who underwent a tracheostomy (p<0.01). Discharge to a long-term acute care hospital was more common in patients who underwent a tracheostomy (29%, p<0.01) or a feeding tube (6%, p<0.01), than those who did not undergo a chronic life sustaining procedure (1%). Thirty six percent of patients who did not undergo a chronic life sustaining procedure died in the hospital compared to 8% of those who underwent a feeding tube placement (p<0.01) and 20% of patients who underwent tracheostomy placement (p<0.01).
A survival curve for 32,189 patients representing 4,305,163 person-days after their ICH is shown in Figure 1. The one-year all-cause mortality risk for all elderly ICH patients was 58% (95% CI 58-59%). Patients who did not undergo chronic life sustaining procedures had a median survival time of 57 days, while those who underwent tracheostomy placement had a median survival time of 110 days and those who only underwent feeding tube placement had a median survival of 266 days. One-year mortality risk was highest for patients who underwent a tracheostomy (65%, 95% CI 62-69%) followed by patients who did not undergo a chronic life sustaining procedure (59%, 95% CI 58-59%) or feeding tube placement (53%, 95% CI 51-56%) (p<0.01, log rank test across groups) (Table 2). Among patients who survived to hospital discharge, the one-year mortality risk among patients who did not undergo a chronic life sustaining procedure was 35% (95% CI 34-36%) (Table 2, Figure 2). Those who underwent a tracheostomy had a 57% (95% CI 53-61%) risk of mortality and those who had a feeding tube placed had a 49% (95% CI 46-51%) risk of mortality (p<0.01, log rank test across the three groups).
Figure 1.
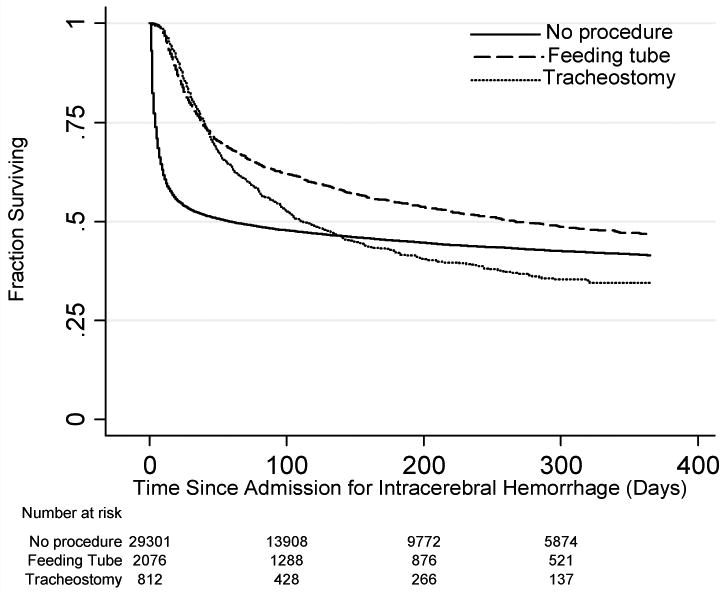
Kaplan-Meier survival curves showing survival in patients with ICH stratified by procedures (p<0.01, log rank test).
Table 2. Cumulative Mortality Risk among elderly ICH patients.
| Total Cohort: Percent (95% confidence interval) | Conditional on Survival to Hospital: Discharge: Percent (95% confidence interval) | |||||||
|---|---|---|---|---|---|---|---|---|
| 30 day | 90 day | 180 day | 365 day | 30 day | 90 day | 180 day | 365 day | |
| No chronic life sustaining procedures | 47 % (46,48) | 52 % (51,52) | 55 % (54,55) | 59 % (58,59) | 17 % (17,18) | 25 % (24,25) | 30 % (29,30) | 35 % (34,36) |
| Patients receiving feeding tube | 21 % (19,22) | 37 % (35,39) | 45 % (43,47) | 53 % (51,56) | 14 % (13,16) | 31 % (29,33) | 40 % (38,43) | 49 % (46,51) |
| Patients receiving tracheostomy | 19 % (16,21) | 45 % (41,48) | 58 % (54,61) | 65 % (62,69) | 6 % (5,8) | 32 % (28,35) | 47 % (43,51) | 57 % (53,61) |
Figure 2.
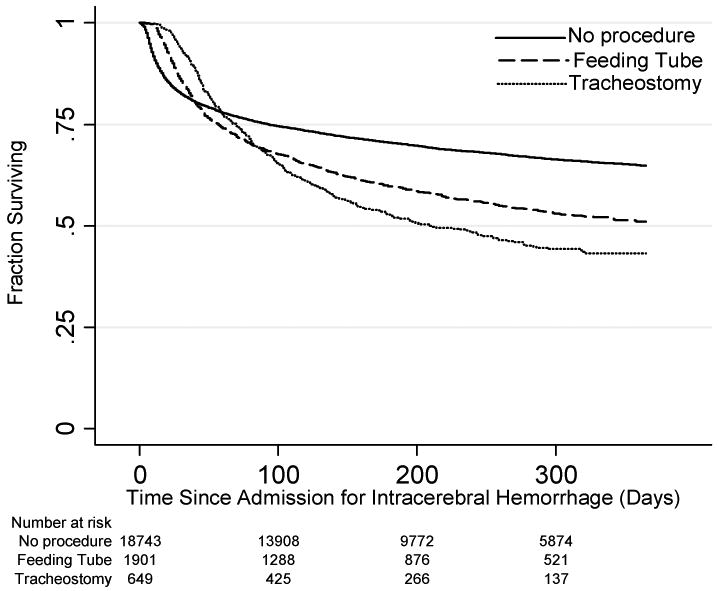
Kaplan-Meier survival curve showing survival of patients with ICH conditional on survival to hospital discharge (p<0.01, log rank test).
Discussion
This study demonstrates that while few elderly ICH patients underwent chronic life sustaining procedures, those that did experienced high one-year mortality and incurred substantial Medicare spending. Over 60% of patients who received a tracheostomy and over 50% of patients who received a feeding tube died in the first year. Patients who underwent chronic life sustaining procedures continued to accrue mortality throughout the first year whereas the majority of deaths among those who did not undergo chronic life sustaining procedures occurred within the first 30 days. Not surprisingly, important differences in the risk of mortality were seen among patients who were discharged from the hospital. While patients who did not undergo a life sustaining procedure remain at elevated risk of death, those that underwent a chronic life sustaining procedure had an approximately 50% risk of one-year mortality even after surviving to hospital discharge. Our finding of substantial one-year mortality, even after survival to hospital discharge, among elderly ICH patients who undergo chronic life sustaining procedure is important to families and physicians as they make management decisions for ICH patients.
The vast majority of patients who underwent feeding tube placement were discharged to a skilled nursing facility while those who underwent a tracheostomy were evenly divided between skilled nursing facility and long-term acute care facility, suggesting significant functional limitations in this population. The importance of functional outcome cannot be underestimated as many patients with a limited life expectancy would forego treatment rather than receive treatment that would leave them with severe functional impairment.23 On the other hand, ICH patients can have functional improvement, continuing even out to a year, after hospital discharge.24-26 Further investigation of long-term functional outcomes among patients who undergo chronic life sustaining procedure is needed.
ICH patients who underwent a tracheostomy incurred considerable Medicare expenses. Medicare paid an average of over 12 times more for the initial hospitalization of patients who underwent a tracheostomy than for patients who underwent only feeding tube placement or no chronic life sustaining procedures. Compared to patients who underwent feeding tube placement, patients who underwent a tracheosotmy had increased length of stay which may, partially, explain the Medicare payment difference. Additionally, the increased proportion of patients undergoing craniotomy and ventriculostomy placement may also contribute to the increased Medicare payment among patients who underwent tracheostomy. The care for the 812 ICH patients who underwent tracheostomy placement resulted in over $66 million in Medicare spending for their initial hospitalizations in 2004. Of this $66 million, over $16 million was spent on patients who died during their hospitalization. The discrepancy in spending is likely even greater if costs of rehabilitation, long-term nursing care, caregiver loss of income, or outpatient visits are considered. While we have identified significantly higher Medicare spending for patients who receive tracheostomy after ICH, the high mortality raises the concern that such care may not meet usual standards for cost effectiveness.
This work has limitations. ICH patients were identified using ICD-9 codes. ICD-9 code 431 has been shown to have a positive predictive value of 89% for ICH against a gold standard of medical record review.13 Tracheostomy, feeding tube placement and discharge location are also dependent on the accuracy of administrative coding. 21 Markers of ICH severity such as ICH volume or glascow coma scale are not available in this dataset. Differences in survival among patients who received a chronic life sustaining procedure is likely, in part, due to ICH severity. Additionally, there are at least two distinct reasons that patients do not undergo chronic life sustaining procedures-either chronic life sustaining procedures were not medically required or patients' families elected to limit care. We were unable to separate these reasons in our dataset. However, the focus of this study was on patients who received chronic life sustaining procedures. This study was limited to those aged 65 and above; the experiences of younger ICH patients may be different. Finally, we did not consider Medicare managed care plans and thus our study may underestimate the total burden of mortality and spending for ICH in those over 65 years of age.
Conclusion
Despite undergoing chronic life sustaining procedures, one-year mortality among elderly intracerebral hemorrhage patients is high. ICH patients who undergo tracheostomy placement incur substantial Medicare payments. Therefore, better prognostic models for survival and functional outcome among ICH patients who receive chronic life sustaining procedures are required to help families and physicians make informed decisions about treatment. These improved models may benefit from considering a time frame more relevant to patients – the months to years after admission, rather than just the acute setting.
Supplementary Material
Appendix 1: Demographics, clinical characteristics, Medicare payments and hospital disposition of Medicare Beneficiaries Hospitalized for ICH.
Appendix 2: Kaplan-Meier survival curves showing survival in patients with ICH stratified by procedures (p<0.01, log rank test).
Acknowledgments
Funding: Dr. Skolarus is supported by an American Academy of Neurology Foundation Clinical Research Training Fellowship. Dr. Burke is supported by the Robert Wood Johnson Clinical Scholars program. Dr. Iwashyna is supported by an NHLBI career development award (K08 HL091249).
We appreciate the expert programming of Tish Shapiro.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lloyd-Jones D, Adams RJ, Brown TM, et al. Heart disease and stroke statistics--2010 update: A report from the american heart association. Circulation. 2010;121:e46–215. doi: 10.1161/CIRCULATIONAHA.109.192667. [DOI] [PubMed] [Google Scholar]
- 2.Andaluz N, Zuccarello M. Recent trends in the treatment of spontaneous intracerebral hemorrhage: Analysis of a nationwide inpatient database. J Neurosurg. 2009;110:403–410. doi: 10.3171/2008.5.17559. [DOI] [PubMed] [Google Scholar]
- 3.Broderick JP, Brott T, Tomsick T, et al. Intracerebral hemorrhage more than twice as common as subarachnoid hemorrhage. Journal of Neurosurgery. 1993;78:188–191. doi: 10.3171/jns.1993.78.2.0188. [DOI] [PubMed] [Google Scholar]
- 4.Qureshi AI, Suri MFK, Nasar A, et al. Changes in cost and outcome among us patients with stroke hospitalized in 1990 to 1991 and those hospitalized in 2000 to 2001. Stroke. 2007;38:2180–2184. doi: 10.1161/STROKEAHA.106.467506. [DOI] [PubMed] [Google Scholar]
- 5.Feigin VL, Lawes CMM, Bennett DA, et al. Stroke epidemiology: A review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. Lancet Neurology. 2003;2:43–53. doi: 10.1016/s1474-4422(03)00266-7. [DOI] [PubMed] [Google Scholar]
- 6.Zahuranec DB, Brown DL, Lisabeth LD, et al. Early care limitations independently predict mortality after intracerebral hemorrhage. Neurology. 2007;68:1651–1657. doi: 10.1212/01.wnl.0000261906.93238.72. [DOI] [PubMed] [Google Scholar]
- 7.Hemphill JC, 3rd, Newman J, Zhao S, et al. Hospital usage of early do-not-resuscitate orders and outcome after intracerebral hemorrhage. Stroke. 2004;35:1130–1134. doi: 10.1161/01.STR.0000125858.71051.ca. [DOI] [PubMed] [Google Scholar]
- 8.Becker KJ, Baxter AB, Cohen WA, et al. Withdrawal of support in intracerebral hemorrhage may lead to self-fulfilling prophecies. Neurology. 2001;56:766–772. doi: 10.1212/wnl.56.6.766. [DOI] [PubMed] [Google Scholar]
- 9.Morgenstern LB, Hemphill JC, 3rd, Anderson C, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: A guideline for healthcare professionals from the american heart association/american stroke association. Stroke. 2010;41:2108–2129. doi: 10.1161/STR.0b013e3181ec611b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Broderick JP, Brott TG, Duldner JE, et al. Volume of intracerebral hemorrhage. A powerful and easy-to-use predictor of 30-day mortality. Stroke. 1993;24:987–993. doi: 10.1161/01.str.24.7.987. [DOI] [PubMed] [Google Scholar]
- 11.Hemphill JC, III, Bonovich DC, Besmertis L, et al. The ich score : A simple, reliable grading scale for intracerebral hemorrhage editorial comment: A simple, reliable grading scale for intracerebral hemorrhage. Stroke. 2001;32:891–897. doi: 10.1161/01.str.32.4.891. [DOI] [PubMed] [Google Scholar]
- 12.Piriyawat P, Smajsova M, Smith MA, et al. Comparison of active and passive surveillance for cerebrovascular disease: The brain attack surveillance in corpus christi (basic) project. Am J Epidemiol. 2002;156:1062–1069. doi: 10.1093/aje/kwf152. [DOI] [PubMed] [Google Scholar]
- 13.Tirschwell DL, Longstreth WT., Jr Validating administrative data in stroke research. Stroke. 2002;33:2465–2470. doi: 10.1161/01.str.0000032240.28636.bd. [DOI] [PubMed] [Google Scholar]
- 14.Kokotailo RA, Hill MD. Coding of stroke and stroke risk factors using international classification of diseases, revisions 9 and 10. Stroke. 2005;36:1776–1781. doi: 10.1161/01.STR.0000174293.17959.a1. [DOI] [PubMed] [Google Scholar]
- 15.Kurek CJ, Cohen IL, Lambrinos J, et al. Clinical and economic outcome of patients undergoing tracheostomy for prolonged mechanical ventilation in new york state during 1993: Analysis of 6,353 cases under diagnosis-related group 483. Critical Care Medicine. 1997;25:983–988. doi: 10.1097/00003246-199706000-00015. [DOI] [PubMed] [Google Scholar]
- 16.Cox CE, Carson SS, Holmes GM, et al. Increase in tracheostomy for prolonged mechanical ventilation in north carolina, 1993-2002. Critical Care Medicine. 2004;32:2219–2226. doi: 10.1097/01.ccm.0000145232.46143.40. [DOI] [PubMed] [Google Scholar]
- 17.Teno JM, Mitchell SL, Gozalo PL, et al. Hospital characteristics associated with feeding tube placement in nursing home residents with advanced cognitive impairment. JAMA. 2010;303:544–550. doi: 10.1001/jama.2010.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in icd-9-cm and icd-10 administrative data. Medical Care. 2005;43:1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 19.Goldstein LB, Samsa GP, Matchar DB, et al. Charlson index comorbidity adjustment for ischemic stroke outcome studies. Stroke. 2004;35:1941–1945. doi: 10.1161/01.STR.0000135225.80898.1c. [DOI] [PubMed] [Google Scholar]
- 20.Icd-9-cm volumes 1 and 2. Alpharetta, GA: 2003. [Google Scholar]
- 21.Kahn JM, Iwashyna TJ. Accuracy of the discharge destination field in administrative data for identifying transfer to a long-term acute care hospital. BMC Res Notes. 2010;3:205. doi: 10.1186/1756-0500-3-205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Allison PD. Event history analysis: Regression for longitudinal event data. Newbury Park, California: Sage; 1984. [Google Scholar]
- 23.Fried TR, Bradley EH, Towle VR, et al. Understanding the treatment preferences of seriously ill patients. N Engl J Med. 2002;346:1061–1066. doi: 10.1056/NEJMsa012528. [DOI] [PubMed] [Google Scholar]
- 24.Kelly PJ, Furie KL, Shafqat S, et al. Functional recovery following rehabilitation after hemorrhagic and ischemic stroke. Archives of Physical Medicine and Rehabilitation. 2003;84:968–972. doi: 10.1016/s0003-9993(03)00040-6. [DOI] [PubMed] [Google Scholar]
- 25.Paolucci S, Antonucci G, Grasso MG, et al. Functional outcome of ischemic and hemorrhagic stroke patients after inpatient rehabilitation: A matched comparison. Stroke. 2003;34:2861–2865. doi: 10.1161/01.STR.0000102902.39759.D3. [DOI] [PubMed] [Google Scholar]
- 26.Hemphill JC, III, Farrant M, Neill TA., Jr Prospective validation of the ich score for 12-month functional outcome. Neurology. 2009;73:1088–1094. doi: 10.1212/WNL.0b013e3181b8b332. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix 1: Demographics, clinical characteristics, Medicare payments and hospital disposition of Medicare Beneficiaries Hospitalized for ICH.
Appendix 2: Kaplan-Meier survival curves showing survival in patients with ICH stratified by procedures (p<0.01, log rank test).


