Abstract
Objectives
To examine regional and Black-White differences in mean age at self-reported menopause among community-dwelling women in the US.
Study Design
Cross-sectional survey conducted in the context of the REasons for Geographic And Racial Differences in Stroke and Myocardial Infarction study.
Results
We studied 22,484 menopausal women. After controlling for covariates, Southern women reported menopause 10.8 months earlier than Northeastern women, 8.4 months earlier than Midwestern women, and 6.0 months earlier than Western women (p<0.05 for all). No difference was observed in menopausal age between Black and White women after controlling for covariates (p=0.69).
Conclusions
Women in the South report earlier menopause than those in other regions, but the cause remains unclear. Our study's large sample size and adjustment for multiple confounders lends weight to our finding of no racial difference in age at menopause. More study is needed of the implications of these findings with regard to vascular health.
Keywords: menopause, race, region
Introduction
Menopause occurs most often between the ages of 50 and 52, with 95% of women having final menstrual period between ages 44 and 561-2. Early menopause has been associated with higher all-cause mortality and an increased incidence in cardiovascular disease (CVD) risk factors, both significant public-health concerns3-5. Several factors have been associated with age at menopause. Women who smoke stop menstruating 1-2 years earlier than comparable non-smokers6-8. Women who use oral contraceptives, who have higher socio-economic status and higher parity have later menopause9. Mother's age at menopause is also an important predictor of daughter's age at menopause10. Data regarding racial differences in age at menopause have been mixed with several small studies reporting that menopause occurs approximately six months earlier in Black women when compared to age-matched White women7, while other larger studies have reported no racial difference8.
Though CVD has been associated with an earlier age at menopause5, the reasons for this association are not known. The Southeastern US is a region described to have higher stroke and coronary heart disease mortality than elsewhere in the country11-12. Whether women living in these higher CVD mortality regions also have lower age at menopause has not been reported. This type of analysis is complicated by the clustering of Blacks in the Southeast.
In this paper, we examined the relationship of age at menopause with race and geographic region in the US. We hypothesized that menopause occurs earlier in the South compared to other regions in the US, consistent with the high CVD mortality there. Furthermore, we sought to determine if any observed regional differences could be explained by race or other factors thought to affect age at menopause.
Materials and Methods
The REasons for Geographic And Racial Differences in Stroke (REGARDS) Study is a national, community-based study of over 43,000 Black and White men and women aged 45 years and older, designed to examine underlying mechanisms leading to regional and racial differences in stroke13. An ancillary study examines differences in acute coronary heart disease outcomes. In order to construct the cohort, individuals were consented and interviewed by computer-assisted telephone interview (CATI), and if they also agreed to an in-home examination, were entered into the cohort. This report includes the 22,484 women who completed the CATI survey regardless of having a home visit and reported having already undergone menopause at the time of the interview.
REGARDS recruitment took place from 2003-2007, and methods are detailed elsewhere13. Briefly, community-dwelling women interviewed for REGARDS resided in all regions in the continental US, both rural and urban areas, and 48.9% (N=10,998) were White and 51.1% (N=11,486) were Black. Race was self-reported, and our cohort includes only two racial groups - Blacks and Whites. The use of “racial differences” in this manuscript refers only to these two racial groups.
The Southern region had a larger number of participants than other regions due to statistical power required to test regional differences in stroke incidence and mortality in the larger study13. The CATI survey included questions on medical history, including reproductive history. To assess for menopausal status, participants were asked, “Have you gone through the change of life?” and “How old were you at the time of your last natural menstrual period?” To identify those with surgical menopause, participants were asked, “Have you ever had a hysterectomy, that is, surgery to remove your uterus or womb?” and “Have you ever had an ovary removed?” If they answered “yes” to the latter, participants were asked, “How many ovaries were removed?” Women who underwent an iatrogenic early menopause were identified if they answered positively to the following question: “Have you had any condition or treatment that caused your menstrual periods to permanently stop, other than the surgeries we just discussed or natural menopause?” Other surgical procedures involving the fallopian tubes and uterus, such as tubal ligation, endometrial ablation, and myomectomy were not included in the reproductive history portion of the interview. Women with a history of hormone use, both for contraceptive and replacement purposes, were included in the analysis.
We divided the study sample into “naturally” and “surgically” menopausal women. Naturally-menopausal women were defined as those reporting that their last menstrual period was 12 months or more prior to their CATI interview. Women who stopped menstruating 12 months prior to having hysterectomy and/or oophorectomy were also considered naturally-menopausal. Surgically menopausal women included those who reported a history of hysterectomy or removal of both ovaries. The relatively small number of women reporting unilateral oophorectomy without hysterectomy (3%) was included in the “natural” menopause group in the analysis since loss of one ovary was not expected to confer a large difference in age at menopause. Participants were excluded if they reported still having regular menstrual periods at the time of initial CATI interview or reported their last period within 12 months of the initial CATI interview. Participants who reported undergoing menopause either naturally or surgically, but did not identify a specific age, were included in separate analyses.
Univariate analyses of variance were used to test associations between self-reported age at menopause and race (Black and White) and region among women in the natural and surgical menopause groups. The self-reported age at menopause was defined as the age in years reported by study participants at which their last menstrual period occurred. For the surgical menopause analysis, the age at menopause was defined as the self-reported age in years when the participants underwent the earliest surgical procedure that met the surgical criteria stated previously. Regions were defined by four geographical regions utilized by the U.S. Census Bureau: South, Northeast, Midwest and West (Figure 1)14. A sub-analysis of the South region was performed to evaluate differences in age at menopause among areas of increased stroke mortality, the Stroke Belt and Stroke Buckle12. The Stroke Buckle includes the coastal plain region of North and South Carolina and Georgia, and the Stroke Belt includes remainder of North and South Carolina and Georgia, and the states of Tennessee, Alabama, Mississippi, Louisiana, and Arkansas.
Figure 1.
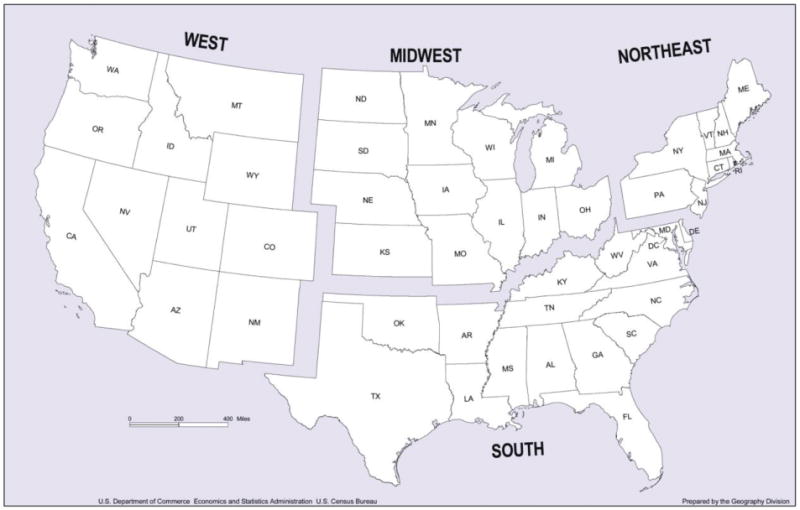
Geographical regions of the Continental United States: United States Census Bureau.
We used multiple linear regression to examine racial and regional differences in age at menopause, and pair-wise comparisons were performed in both racial and regional analyses to adjust for variables known to be associated with menopausal age: chronological age, parity, smoking history, and socioeconomic status. All variables were examined simultaneously. Annual income and education were utilized as surrogates for socioeconomic status. History of CVD was also included as a covariate given an association with earlier menopause as previously discussed. The CVD variable included self-reported history of myocardial infarction, stroke, transient ischemic event (TIA), carotid endarterectomy, coronary intervention, repair of aortic aneurysm, and/or peripheral arterial intervention. Physical activity was entered as a covariate in the analysis because a European study recently illustrated an association between earlier menopause and both decreased physical activity and higher body mass index (BMI)15. Extent of physical activity was assessed by the CATI interview with the following question: “How many times per week do you engage in intense physical activity, enough to work up a sweat.” Measured BMI was entered as a covariate in a separate analysis for those participants that underwent an in-home visit (7,167 women or 68.5%) to elucidate if this might explain differences observed in age at menopause. Less than 0.5% of all data points were missing after interviewing REGARDS respondents, with the exception of annual income and physical activity, where 16.9% and 1.6% of respondents respectively did not provide an answer. For income those with missing data were included in the analysis and coded as missing.
Results
Sample characteristics
Women in the natural (n=10,440) and surgical menopause (n=9,944) groups differed somewhat with respect to age, parity, and smoking history (Table 1). A greater proportion of women in the surgical menopause group was Black and resided in the South. In addition, women in the surgical menopause group tended to have lower education and lower annual income. Women with surgical menopause had a proportionately greater prevalence of self-reported CVD.
Table 1.
Total number of female REGARDS interview respondents with natural menopause, surgical menopause, and menopausal age not reported.
| Natural (N = 10,440) n (%) |
Surgical (N = 9944) n (%) |
P-value compa red to Natural | Not reported age at Natural (N =1,361) n (%) |
P-value compared to Natural | Not reported age atSurgical (N =739) n (%) |
P-value compared to Surgical | |
|---|---|---|---|---|---|---|---|
| Region | |||||||
| South | 6750 (64.7) | 7307 (73.5) | <0.0001 | 899 (66.1) | 0.35 | 555 (75.2) | 0.48 |
| Northeast | 945 (9.1) | 517 (5.2) | 106 (7.8) | 37 (5.0) | |||
| Midwest | 1555 (14.9) | 1279 (12.9) | 193 (14.2) | 96 (13.0) | |||
| West | 1185 (11.4) | 833 (8.4) | 162 (11.9) | 50 (6.8) | |||
|
| |||||||
| Race | |||||||
| White | 5479 (52.5) | 4738 (47.7) | <0.0001 | 781 (57.4) | <0.0001 | 201 (27.2) | <0.0001 |
| Black | 4961 (47.5) | 5206 (52.4) | 580 (42.6) | 538 (72.8) | |||
|
| |||||||
| Age | |||||||
| <55 | 987 (9.5) | 1144 (11.5) | <0.0001 | 55 (4.0) | <0.0001 | 20 (2.7) | <0.0001 |
| 55-64 | 4334 (41.5) | 3959 (39.8) | 394 (29.0) | 164 (22.2) | |||
| 65-74 | 3184 (30.5) | 3230 (32.5) | 466 (34.2) | 287 (38.8) | |||
| ≥75 | 1935 (18.5) | 1611 (16.2) | 446 (32.8) | 268 (36.3) | |||
|
| |||||||
| Parity | |||||||
| 0 | 1261 (12.1) | 1032 (10.4) | 0.0004 | 171 (12.7) | 0.28 | 93 (12.7) | 0.09 |
| 1 | 1441 (13.8) | 1441 (14.5) | 206 (15.2) | 94 (12.8) | |||
| ≥ 2 | 7710 (74.1) | 7456 (75.1) | 975 (72.1) | 546 (74.5) | |||
|
| |||||||
| Annual income | |||||||
| < $20,000 | 2538 (24.3) | 2523 (25.4) | .003 | 342 (25.1) | <0.0001 | 251 (34.0) | <0.0001 |
| $20,000-34,999 | 2594 (24.9) | 2596 (26.1) | 273 (20.1) | 155 (21.0) | |||
| $35,000-74,999 | 2628 (25.2) | 2415 (24.3) | 196 (14.4) | 91 (12.3) | |||
| ≥$75,000 | 1076 (10.3) | 896 (9.0) | 95 (7.0) | 11 (1.5) | |||
| Refused | 1604 (15.4) | 1514 (15.2) | 455 (33.4) | 231 (31.3) | |||
|
| |||||||
| Education level | |||||||
| < HS | 1503 (14.4) | 1724 (17.4) | <0.0001 | 320 (23.6) | <0.0001 | 217 (29.4) | <0.0001 |
| Graduated HS | 2881 (27.6) | 3020 (30.4) | 379 (27.9) | 229 (31.1) | |||
| Some collegea | 2793 (26.8) | 2802 (28.2) | 314 (23.1) | 145 (19.7) | |||
| Graduated college | 3248 (31.2) | 2387 (24.0) | 346 (25.5) | 146 (19.8) | |||
|
| |||||||
| Self-reported history of CVDb | |||||||
| No | 8607 (82.4) | 7844 (78.9) | <0.0001 | 1083 (79.6) | 0.009 | 541 (73.2) | 0.0003 |
| Yes | 1833 (17.6) | 2100 (21.1) | 278 (20.4) | 198 (26.8) | |||
|
| |||||||
| Physical activity per week | |||||||
| none | 4058 (39.5) | 4084 (41.6) | 0.0003 | 644 (48.9) | <0.0001 | 368 (51.3) | <0.0001 |
| 1-3 | 3570 (34.7) | 3415 (34.8) | 386 (29.3) | 220 (30.7) | |||
| ≥4 | 2658 (25.8) | 2312 (23.6) | 288 (21.9) | 129 (18.0) | |||
|
| |||||||
| Smoking | |||||||
| Never | 5407 (52.0) | 5302 (53.5) | 0.09 | 761 (56.5) | 0.002 | 423 (58.1) | 0.01 |
| Current | 1622 (15.6) | 1476 (14.9) | 170 (12.6) | 83 (11.4) | |||
| Past | 3365 (32.4) | 3128 (31.6) | 415 (30.8) | 222 (30.5) | |||
Indicates some college, trade school or technical classes taken
Reported personal history of myocardial infarction, stroke, TIA, carotid endarterectomy, coronary intervention, repair of aortic aneurysm and/or peripheral artery intervention
Women who reported being menopausal but did not report an age at menopause (n=1,361) did not differ from those in the natural menopause group with respect to parity and region of residence (Table 1). They tended to be older, with 67% (N=912) older than 64 years, and slightly more were White (57.4% vs. 52.5%). This group also contained fewer smokers, reported CVD more frequently, had lower annual income, and had less formal education when compared to the naturally-menopausal group. Similarly, the group with surgical menopause that did not report a menopausal age tended to be older, had lower annual income and less formal education; however, the majority of this group was Black (72.8%) (Table 1).
Multiple linear regression analyses for age at menopause
The unadjusted mean age at natural menopause in this cohort was 49.0 years, with a median age of 50.0 years. In the univariate analyses, Black women reported becoming naturally menopausal 4.8 months earlier than White women (p=0.003) (Table 2). However, age at natural menopause did not differ between Blacks and Whites after controlling for age, parity, smoking, region, income, education, physical activity, and history of CVD (p=0.69) (Table 3).
Table 2.
Unadjusted mean age at menopause for REGARDS interview respondents with natural and surgical menopause.
| Natural (n = 10,440) |
Surgical (n = 9,944) |
|||||
|---|---|---|---|---|---|---|
| Region | Age | STD | p-value | Agec | STD | p-value |
| South | 48.7 | 6.5 | -- | 39.5 | 8.7 | -- |
| Northeast | 49.7 | 5.8 | <0.0001 | 40.7 | 8.4 | 0.002 |
| Midwest | 49.4 | 6.1 | 0.0002 | 40.4 | 8.8 | 0.0002 |
| West | 49.6 | 6.1 | <0.0001 | 41.0 | 8.4 | <0.0001 |
|
| ||||||
| Race | ||||||
| White | 49.2 | 5.9 | -- | 39.5 | 8.7 | -- |
| Black | 48.8 | 6.8 | 0.003 | 40.0 | 8.7 | 0.004 |
|
| ||||||
| Age | ||||||
| <55 | 46.4 | 5.4 | -- | 38.2 | 7.6 | -- |
| 55-64 | 49.1 | 6.1 | <0.0001 | 38.7 | 8.4 | 0.13 |
| 65-74 | 49.4 | 6.7 | <0.0001 | 40.3 | 8.6 | <0.0001 |
| ≥75 | 49.3 | 6.6 | <0.0001 | 42.5 | 9.5 | <0.0001 |
|
| ||||||
| Parity | ||||||
| 0 | 48.3 | 6.5 | -- | 38.7 | 9.0 | -- |
| 1 | 48.4 | 6.5 | 0.79 | 38.8 | 8.7 | 0.86 |
| ≥ 2 | 49.2 | 6.3 | <0.0001 | 40.1 | 8.6 | <0.0001 |
|
| ||||||
| Annual income | ||||||
| < $20,000 | 48.4 | 7.1 | -- | 39.3 | 9.3 | -- |
| $20,000-34,999 | 49.1 | 6.3 | <0.0001 | 39.6 | 8.4 | 0.20 |
| $35,000-74,999 | 49.4 | 5.8 | <0.0001 | 39.7 | 8.1 | 0.08 |
| ≥$75,000 | 49.3 | 5.4 | <0.0001 | 40.1 | 8.2 | 0.02 |
| Refused | 49.0 | 6.7 | 0.0010 | 40.6 | 9.1 | <0.0001 |
|
| ||||||
| Education level | ||||||
| < HS | 48.1 | 7.5 | -- | 39.3 | 9.5 | -- |
| Graduated HS | 48.9 | 6.5 | <0.0001 | 39.4 | 8.8 | 0.83 |
| Some collegea | 49.0 | 6.4 | <0.0001 | 39.6 | 8.5 | 0.33 |
| Graduated college | 49.6 | 5.6 | <0.0001 | 40.8 | 8.0 | <0.0001 |
|
| ||||||
| Self-reported history of CVDb | ||||||
| No | 49.1 | 6.2 | -- | 40.0 | 8.5 | -- |
| Yes | 48.6 | 6.9 | 0.003 | 39.0 | 9.1 | <0.0001 |
|
| ||||||
| Physical activity per week | ||||||
| none | 48.7 | 6.6 | -- | 39.8 | 8.8 | -- |
| 1-3 | 49.3 | 6.1 | <0.0001 | 39.8 | 8.6 | 0.96 |
| ≥4 | 49.2 | 6.2 | 0.002 | 39.7 | 8.6 | 0.56 |
|
| ||||||
| Smoking | ||||||
| Never | 49.4 | 6.3 | -- | 40.6 | 8.7 | -- |
| Current | 47.4 | 6.5 | <0.0001 | 37.3 | 8.4 | <0.0001 |
| Past | 49.1 | 6.3 | 0.02 | 39.6 | 8.6 | <0.0001 |
Indicates some college, trade school or technical classes taken
Reported personal history of myocardial infarction, stroke, TIA, carotid endarterectomy, coronary intervention, repair of aortic aneurysm and/or peripheral artery intervention
Age equal to age at hysterectomy and/or oophorectomy
Table 3.
Adjusted mean age at menopause for REGARDS interview respondents with natural menopause.
| Age (years) (n= 10,198c) |
||
|---|---|---|
| Region | Age | p-value |
| South | 47.5 | -- |
| Northeast | 48.4 | <0.0001 |
| Midwest | 48.2 | 0.0001 |
| West | 48.0 | 0.02 |
|
| ||
| Race | ||
| White | 48.1 | -- |
| Black | 48.0 | 0.69 |
|
| ||
| Age | ||
| <55 | 45.9 | -- |
| 55-64 | 48.5 | <0.0001 |
| 65-74 | 48.9 | <0.0001 |
| ≥75 | 48.9 | <0.0001 |
|
| ||
| Parity | ||
| 0 | 47.6 | -- |
| 1 | 47.9 | 0.33 |
| ≥ 2 | 48.6 | <0.0001 |
|
| ||
| Annual income | ||
| < $20,000 | 47.7 | -- |
| $20,000-34,999 | 48.0 | 0.04 |
| $35,000-74,999 | 48.4 | 0.0005 |
| ≥$75,000 | 48.2 | 0.03 |
| Refused | 47.9 | 0.23 |
|
| ||
| Education level | ||
| < HS | 47.4 | -- |
| Graduated HS | 48.1 | 0.0007 |
| Some collegea | 48.2 | 0.0002 |
| Graduated college | 48.6 | <0.0001 |
|
| ||
| Self-reported history of CVDb | ||
| No | 48.2 | -- |
| Yes | 47.9 | 0.04 |
|
| ||
| Physical activity per week | ||
| none | 47.8 | -- |
| 1-3 | 48.2 | 0.0007 |
| ≥4 | 48.1 | 0.01 |
|
| ||
| Smoking | ||
| Never | 48.7 | -- |
| Current | 47.1 | <0.0001 |
| Past | 48.3 | 0.005 |
Indicates some college, trade school or technical classes taken
Reported personal history of myocardial infarction, stroke, TIA, carotid endarterectomy, coronary intervention, repair of aortic aneurysm and/or peripheral artery intervention
Indicates total participants with complete data for all covariates considered in analysis
Naturally-menopausal women in the South region underwent menopause 12 months earlier than women in the Northeast, 8.4 months earlier than in the Midwest, and 10.8 months earlier than women in the West (p=<0.0001, 0.0002, and <0.0001 respectively) (Table 2). Statistical significance persisted after controlling for the covariates mentioned above (Table 3). Within the South region, naturally-menopausal women in the Stroke Belt and Stroke Buckle did not undergo menopause significantly earlier than other women residing in the South (data not shown).
In the adjusted analyses, current smokers reported entering menopause 1.6 years earlier than never-smokers (p<0.0001), while past smokers reported entering menopause 4.8 months earlier (p=0.005) (Table 3).
Accounting for other factors, older age at the time of interview was not associated with reported age at natural menopause. Women aged 55-64, 65-74, and ≥ 75 years reported menopause at 48.5, 48.9 and 48.9 years, respectively. However, the mean reported menopausal age among women less than 55 years old was 45.9 years, which was significantly younger than the three other groups (p<0.001) (Table 3).
After controlling for covariates, women with two or more children reported a mean age at menopause 1 year later than those with no children (p<0.0001) and 3.6 months later than those with one child, although the latter did not reach statistical significance (p=0.33) (Table 3).
Annual income less than $20,000 was associated with menopause 3.63, 8.4, and 6.0 months earlier than incomes of $20,000-34,999; $35,000-74,999; and greater than $75,000. These differences were statistically significant (p=0.04, 0.00054, and 0.03, respectively). The three higher-income groups did not differ in age at menopause. Women in the cohort were divided into four groups with respect to educational level: did not complete high school; graduated high school; completed some college; and graduated college. Menopause occurred later in women with more education, with a maximum difference of 1.2 years between women who did not complete high school compared with those who graduated college (Table 3).
Self-reported history of cardiovascular disease (CVD) was associated with an earlier reported menopause by 3.6 months (p=0.04). Weekly intense physical activity was associated with a later menopause, 4.8 months later for activity 1-3 times per week and 3.6 months later for activity greater than 3 times per week (p=0.0007 and 0.01 respectively) (Table 3).
Comment
In this study, we report that women in the South reported menopause significantly earlier than those in the Northeast, Midwest, and West even after controlling for covariates including race, parity, smoking, socioeconomic status, amount of weekly physical activity, and history of CVD. However, women in regions other than the South did not have a significant difference in age at menopause when compared to each other. To our knowledge this is the first report of a regional difference in age at menopause in the United States. The low p-value associated with the findings suggests that the findings are unlikely to be due to chance, although we acknowledge that multiple tests were conducted as part of the analyses. These findings are significant due to the association between early menopause and both increased cardiovascular disease and mortality4,16. The regional finding may also guide patient counseling regarding timing of menopause for women residing in the South.
The reason for the observed regional difference is not clear. It is possible that a higher burden of cardiovascular disease in the area could be contributory and that our crude adjustment using history of CVD did not fully account for this burden. The Framingham Heart Study illustrated an inverse relationship between age at menopause and stroke risk, which lends support to an association between vascular compromise and earlier menopause17. Decreased ovarian perfusion, which may be reflective of poorer ovarian vascular health, has been implicated in earlier menopause18; however, it is unclear at this time if a decrease in perfusion may be the cause or effect of menopause.
The overall reported mean age at natural menopause in our cohort was 49.0 years, which is earlier than the previously reported age of approximately 51.4 years4,19-21. Cooper et al. utilized a cohort of university students in Minnesota beginning in the 1930s. The study participants likely differed from our cohort with respect to socioeconomic status given college education, as only 27.3% of women in our study graduated from college. In addition, lifestyle factors such as diet, exercise, and smoking may be dissimilar between the two cohorts given the different time periods: recruitment in 1930s versus 2000s. Brambilla et al. recruited women residing in Massachusetts in the 1980s, while our cohort includes women from across the United States.
The Study of Women's Health Across the Nation (SWAN) reported a median age at natural menopause of 51.4 years in a cohort of 2,247 women8. SWAN included community-dwelling women residing in 7 US states, none of which were in the South, with similar covariates to our study. Our cohort included Southern women, those in rural areas, and a greater proportion of Black women (47.6% versus 26.8%)8. The lower socioeconomics in the South and rural areas as well as among Black women may contribute to the lower median age at menopause in our cohort.
It is unclear whether selection bias can account for the lower mean age in menopause in our cohort. A large proportion of the overall cohort underwent surgical menopause, which is likely a function of the large proportion of women residing in the South, where hysterectomy occurs more frequently than other regions. Abnormal menses is a common reason for hysterectomy and symptom of impending menopause22. It is conceivable that some of the women in the surgical group were experiencing such symptoms, and excluding these women would increase the mean age at menopause of our naturally-menopausal sample rather than decrease it. In addition, our cohort included 987 women (9.9%) aged 45-55 who identified themselves as menopausal, which would be expected to decrease the overall mean age at menopause. These women were evenly distributed among geographical regions and racial groups. However, Black women reported early natural menopause (prior to age 45) more often than White women. Regional and racial differences in overall age at menopause persisted when women aged 45-55 years were excluded from the cohort in a sub-analysis (data not shown).
It is possible that the menopausal age is declining in American women. Dratva and colleagues recently reported that obesity was associated with earlier menopause in European women15. With increasing obesity in America, and particularly with obesity rates of nearly 30% in the Southern region, the age of natural menopause may be trending downward in regions with the greatest obesity. We obtained measured BMI values for 7,167 REGARDS women. In this subanalysis, after adjusting for other covariates, BMI did not predict age at menopause in our cohort, nor did it explain the regional differences we observed (data not shown). Though missing BMI data was the same across natural and surgical menopause groups, conclusions regarding BMI and menopausal age are difficult to make since 31.5% of participants did not undergo a home visit with BMI measurement. Dratva also reported that low physical activity decreased the age of natural menopause15; we had similar findings in our cohort with respect to weekly physical activity. Future prospective studies are needed to elucidate if the menopausal age has declined in American women.
We found a small difference in the mean age at menopause between Black and White women in this cohort which disappeared after adjusting for covariates including history of CVD. These findings are consistent with those in the SWAN study8. Two smaller studies of less than 1500 women, previously reported a 6-month difference in menopausal age between the two groups7,23. Both of these studies controlled for covariates considered in our study, except region and history of CVD, but had significantly smaller proportions of Black women in the samples. One study included women all residing in the same state, while the other utilized a national cohort, but did not control for region7,23. In our large cohort, no difference in age at menopause was seen between Black and White women after adjusting for region and other covariates. Black women reported hysterectomy more often than White women in our cohort, findings that are consistent with previous studies23. It is unlikely that this result would skew the mean menopausal age for naturally-menopausal Black women, since studies reporting a positive race difference in age at natural menopause found the same relationship between race and hysterectomy as we observed7. In addition, a selection bias would conceivably increase the age at menopause rather than decrease it since menstrual irregularities are one of the most common reasons for hysterectomy and can be a sign of impending menopause as previously stated22. The SWAN study, which did not find a racial difference in age at menopause, also identified a racial disparity in hysterectomy, with Black women undergoing surgery more commonly than White women8. The reasons for this disparity remain unclear; while Black women have a significantly higher incidence of uterine fibroids24, a recent study found excess risk for hysterectomy even after controlling for this confounder25. Studies have also shown that in addition to undergoing hysterectomy more frequently than White women, Black women tend to have hysterectomies at an earlier age than their White counterparts24.
We studied self-reported age at menopause, which might be prone to bias. However, recall of age at menopause has been shown to be fairly reproducible and has a 70-80% overall validity within one year compared with actual age at menopause based on recorded age at menopause at the time of occurrence26-27. The mean age of self-reported menopause may be slightly earlier than that determined in a prospective manner, since women tend to recall their age rounded to the lowest whole year. However, this phenomenon should not decrease the average age more than one year and should be consistent across geographical regions and racial groups. As expected, the validity of the timing of menopause declines with time since menopause and with lower educational levels23. In our cohort, greater than 85% of the naturally-postmenopausal women graduated from high school, and only 18.5% were ≥ 75 years old at the time of initial interview. Therefore, the validity of the self-reported age of menopause of the women in our study is likely to be adequate. Regardless, any misclassification would bias our findings to the null hypothesis, leading to underestimation of associations.
Current smokers reported menopause an average of 1.6 years earlier than never-smokers. Higher parity (≥ 2 children) was associated with menopause 1 year later than in nulliparous women, however having one child did not increase the age at menopause significantly. The association between higher parity and later menopause and current smoking and earlier menopause are consistent with those found in previous studies6-9. The strengths of this study include a large sample size, inclusion of women from rural areas in the United States, and inclusion of a large number of Black women. To our knowledge it is the first epidemiological study to report regional differences in the age at menopause in the US. This finding is important given the association between early menopause and health concerns such as osteoporosis and CVD. The study was limited by utilizing self-reported age at menopause and lack of minority groups other than Blacks. We also did not have available environmental or genetic factors that could further elucidate the mechanisms leading to earlier menopause in the South.
In conclusion, in this cohort of 10,440 naturally menopausal women, those residing in the South reported earlier menopause by 6-11 months compared to other regions after adjusting for covariates. Age at menopause did not differ significantly in Black and White women, however. Further work is needed to determine whether menopausal age may in some way be associated with the excess cardiovascular mortality risk in the South.
Acknowledgments
Support provided by R01 HL80477 from the National Heart, Lung and Blood Institute, and by a cooperative agreement U01 NS041588 from the National Institute of Neurological Disorders and Stroke, National Institutes of Health, Department of Health and Human Services. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Neurological Disorders and Stroke or the National Institutes of Health. The authors acknowledge the participating REGARDS investigators and institutions for their valuable contributions: The University of Alabama at Birmingham, Birmingham, Alabama (Study PI, Statistical and Data Coordinating Center, Survey Research Unit): George Howard DrPH, Leslie McClure PhD, Virginia Howard PhD, Libby Wagner MA, Virginia Wadley PhD, Rodney Go PhD, Monika Safford MD, Ella Temple PhD, Margaret Stewart MSPH, J. David Rhodes BSN; University of Vermont (Central Laboratory): Mary Cushman MD; Wake Forest University (ECG Reading Center): Ron Prineas MD, PhD; Alabama Neurological Institute (Stroke Validation Center, Medical Monitoring): Camilo Gomez MD, Susana Bowling MD; University of Arkansas for Medical Sciences (Survey Methodology): LeaVonne Pulley PhD; University of Cincinnati (Clinical Neuroepidemiology): Brett Kissela MD, Dawn Kleindorfer MD; Examination Management Services, Incorporated (In-Person Visits): Andra Graham; Medical University of South Carolina (Migration Analysis Center): Daniel Lackland DrPH; Indiana University School of Medicine (Neuropsychology Center): Frederick Unverzagt PhD; National Institute of Neurological Disorders and Stroke, National Institutes of Health (funding agency): Claudia Moy PhD.
Financial support:
REGARDS funding: NSI.2U01NS041588-07A1 (Safford, Cushman)
REGARDS-MI funding: NHLBI R01 HL80477-01A1 (Safford, Roth, Halanych)
K23-HL-87114 (Wellons)
Footnotes
Disclosure: None of the authors have a conflict of interest to report
Abstract presented at the American Society for Reproductive Medicine (ASRM) annual meeting on November 11, 2008 in San Francisco, California
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Treolar AE. Menstrual cyclicity and the premenopause. Maturitas. 1981;3:249–64. doi: 10.1016/0378-5122(81)90032-3. [DOI] [PubMed] [Google Scholar]
- 2.McKinlay SM, Brambilla DJ, Posner JG. The normal menopause transition. Maturitas. 1992;14(2):103–15. doi: 10.1016/0378-5122(92)90003-m. [DOI] [PubMed] [Google Scholar]
- 3.Jacobsen BK, Heuch I, Kvale G. Age at natural menopause and all-cause mortality: a 37-year follow-up of 19,731 Norwegian women. Am J Epidemiol. 2003;157(10):923–9. doi: 10.1093/aje/kwg066. [DOI] [PubMed] [Google Scholar]
- 4.Cooper GS, Sandler DP. Age at natural menopause and mortality. Ann Epidemiol. 1998;8:229–35. doi: 10.1016/s1047-2797(97)00207-x. [DOI] [PubMed] [Google Scholar]
- 5.Kok HS, van Asselt KM, van der Schouw YT, van der Tweel I, Peeters PH, Wilson PW, et al. Heart disease risk determines menopausal age rather than the reverse. J Am Coll Cardiol. 2006;47:1976–83. doi: 10.1016/j.jacc.2005.12.066. [DOI] [PubMed] [Google Scholar]
- 6.Sowers MR, La Pietra MT. Menopause: its epidemiology and potential association with chronic diseases. Epidemiol Rev. 1996;17:287–302. doi: 10.1093/oxfordjournals.epirev.a036194. [DOI] [PubMed] [Google Scholar]
- 7.Bromberger JT, Matthews KA, Kuller LH, Wing RR, Meilahn EN, Plantinga P. Prospective study of the determinants of age at menopause. Amer J Epidemiol. 1997;145:124–33. doi: 10.1093/oxfordjournals.aje.a009083. [DOI] [PubMed] [Google Scholar]
- 8.Gold EB, Bromberger JT, Crawford S, Samuels S, Greendale GA, Harlow SD, et al. Factors associated with age at natural menopause in a multi-ethnic sample of midlife women. Amer J Epidemiol. 2001;153:865–74. doi: 10.1093/aje/153.9.865. [DOI] [PubMed] [Google Scholar]
- 9.vanNoord PA, Dubas JS, Dorland M, Boersma H, te Velde E. Age at natural menopause in a population-based screening cohort: the role of menarche, fecundity, and lifestyle factors. Fertil Steril. 1997;68(1):95–102. doi: 10.1016/s0015-0282(97)81482-3. [DOI] [PubMed] [Google Scholar]
- 10.Torgerson DJ, Avenell A, Russell IT, Reid DM. Factors associated with onset of menopause in women aged 45-49. Maturitas. 1994;19(2):83–92. doi: 10.1016/0378-5122(94)90057-4. [DOI] [PubMed] [Google Scholar]
- 11.Lanska DJ. Geographic distribution of stroke mortality in the United States: 1939-1941 to 1979-1981. Neurology. 1993;43(9):1839–51. doi: 10.1212/wnl.43.9.1839. [DOI] [PubMed] [Google Scholar]
- 12.Casper ML, Wing S, Anda RF, Knowles M, Pollard RA. The shifting stroke belt. Changes in the geographic pattern of stroke mortality in the United States, 1962 to 1998. Stroke. 1995;26(5):755–60. doi: 10.1161/01.str.26.5.755. [DOI] [PubMed] [Google Scholar]
- 13.Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, et al. The reasons for geographic and racial differences in stroke study: objectives and design. Neuroepidemiol. 2005;25(3):135–43. doi: 10.1159/000086678. [DOI] [PubMed] [Google Scholar]
- 14.United States Census Bureau. http://www.census.gov.
- 15.Dratva J, Gomez Real F, Schindler C, Ackermann-Liebrich U, Gerbase MW, Probst-Hensch NM, et al. Is age at menopause increasing across Europe? Results on age at menopause and determinants from two population-based studies. Menopause. 2009;16(2):385–94. doi: 10.1097/gme.0b013e31818aefef. [DOI] [PubMed] [Google Scholar]
- 16.Atsma F, Bartelink ML, Grobbee DE, van der Schouw YT. Postmenopausal status and early menopause as independent risk factors for cardiovascular disease: a meta-analysis. Menopause. 2006;13(2):265–79. doi: 10.1097/01.gme.0000218683.97338.ea. [DOI] [PubMed] [Google Scholar]
- 17.Lisabeth LD, Beiser AS, Brown DL, Murabito JM, Kelly-Hayes M, Wolf P. Age at natural menopause and risk of ischemic stroke: the Framingham Heart Study. Stroke. 2009;40:1044–9. doi: 10.1161/STROKEAHA.108.542993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kurjak A, Kupesic S. Ovarian senescence and its significance on uterine and ovarian perfusion. Fertil Steril. 1995;64(3):532–537. doi: 10.1016/s0015-0282(16)57788-7. [DOI] [PubMed] [Google Scholar]
- 19.Cooper GS, Sandler DP, Bohlig M. Active and passive smoking and the occurrence of natural menopause. Epidemiology. 1999;10(6):771–3. [PubMed] [Google Scholar]
- 20.Brambilla DJ, McKinlay SM. A prospective study of factors affecting age at menopause. J Clin Epidemiol. 1989;42(11):1031–39. doi: 10.1016/0895-4356(89)90044-9. [DOI] [PubMed] [Google Scholar]
- 21.North American Menopause Society. Menopause core curriculum study guide. Cleveland, OH: North American Menopause Society; 2002. [Google Scholar]
- 22.Falcone T, Walters MD. Hysterectomy for benign disease. Obstet Gynecol. 2008;111(3):753–67. doi: 10.1097/AOG.0b013e318165f18c. [DOI] [PubMed] [Google Scholar]
- 23.Stanford JL, Hartge P, Brinton LA, Hoover RN, Brookmeyer R. Factors influencing the age at natural menopause. J Chronic Dis. 1987;40(11):995–1002. doi: 10.1016/0021-9681(87)90113-5. [DOI] [PubMed] [Google Scholar]
- 24.Kjerulff KH, Guzinski GM, Langenberg PW, Stolley PD, Moye NE, Kazandjian VA. Hysterectomy and race. Obstet Gynecol. 1993;82(5):757–64. [PubMed] [Google Scholar]
- 25.Bower JK, Schreiner PJ, Sternfeld B, Lewis CE. Black-White differences in hysterectomy prevalence: the CARDIA study. Am J Public Health. 2009;99(2):300–7. doi: 10.2105/AJPH.2008.133702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Den Tonkelaar I. Validity and reproducibility of self-reported age at menopause in women participating in the DOM-project. Maturitas. 1997;27(2):117–23. doi: 10.1016/s0378-5122(97)01122-5. [DOI] [PubMed] [Google Scholar]
- 27.Bean JA, Leeper JD, Wallace RB, Sherman BM, Jagger H. Variations in the reporting of menstrual histories. Am J Epidemiol. 1979;109(2):181–5. doi: 10.1093/oxfordjournals.aje.a112673. [DOI] [PubMed] [Google Scholar]


