Abstract
The authors used data from 6 waves of the Health and Retirement Study to evaluate changes in the prevalence of cognitive impairment among adults 70 years of age or older from 1993 to 2004. Having sampling weights for each wave enabled the authors to create merged waves that represented cross-sections of the community-dwelling older population for that year. Logistic regression analyses with year as the predictor were used to estimate trends and determine the contribution of sociodemographic and health status variables to decreasing trends in the prevalence of cognitive impairment over time (score ≤8 on a modified Telephone Interview Cognitive Screen). Results showed an annual decline in the prevalence of cognitive impairment of 3.4% after adjustment for age, gender, and prior test exposure (odds ratio (OR) = 0.966, 95% confidence interval (CI): 0.941, 0.992). The addition of socioeconomic variables to the model attenuated the trend by 72.1%. The annual percentage of decline in impairment was larger for blacks (OR = 0.943, 95% CI: 0.914, 0.973) and Hispanics (OR = 0.954, 95% CI: 0.912, 0.997) than for whites (OR = 0.971, 95% CI: 0.936, 1.006), although the differences were not statistically significant. Linear probability models used in secondary analyses showed larger percentage-point declines for blacks and Hispanics. Improvements in educational level contributed to declines in cognitive impairment among older adults—particularly blacks and Hispanics—in the United States.
Keywords: African Americans; aged; aged, 80 and over; cognition disorders; health status disparities; Hispanic Americans; prevalence; socioeconomic factors
Improvements in health and increases in life expectancy have contributed to the expansion of the older population over the past century. Moreover, the number and proportion of older adults in the United States will increase from 2010 to 2030, as the “Baby Boomer” generation starts turning 65 years old (1). The older population will become more diverse as it grows, and projections suggest that by 2050, 61% of older adults will be non-Hispanic white, compared with 81% in 2006 (1).
Cognitive impairment and dementia could burden the medical care system in the United States as the older population grows. Researchers have estimated that the number of adults with dementia will increase 2.5–4-fold by 2050 because of population aging (2–4). However, projections assume that age-specific rates of dementia will remain constant, and even modest delays in age-specific onset can have significant public health implications (4). In addition, these estimates are not nationally representative; they combine US census data with population-based prevalence estimates from community studies.
Recent studies have examined population-level changes in the prevalence of cognitive impairment in the 1980s and 1990s by using nationally representative samples of older Americans (5–8). Although preliminary evidence suggests that there has been an overall reduction in the proportion of older adults with cognitive impairment, most studies examined changes between 2 time points only (5, 6), and results have been inconsistent (8). This has been described as an important gap in the knowledge of health trends in older adults (9). Moreover, trends in disparities among racial and socioeconomic groups have not been examined. Racial/ethnic and socioeconomic disparities in cognitive impairment have been widely documented (10–13). The purpose of the present study was to investigate recent trends in cognitive impairment in a nationally representative sample of older adults, establish whether racial/ethnic and socioeconomic disparities have widened or narrowed, and explore the contributions of demographic, socioeconomic, and health status variables to observed trends.
MATERIALS AND METHODS
Data source
Data were taken from the Health and Retirement Study (HRS), a nationally representative longitudinal survey of older Americans. The HRS was initially designed as 2 separate but related panel studies, the HRS and the Assets and Health Dynamics of the Oldest Old (AHEAD) Study, that were merged in 1998 into a single survey representative of the US population aged 51 years or older. New cohorts are added to the HRS every 6 years.
The original HRS used a longitudinal survey initially administered in 1992 to a nationally representative sample of Americans born from 1931 to 1941 and their spouses. Respondents continue to be contacted biennially as part of the ongoing HRS. The AHEAD Study was a longitudinal survey of a nationally representative sample of community-dwelling adults 70 years of age or older and their spouses (of any age) in 1993 and 1994. Respondents were re-interviewed in 1995 as part of the AHEAD Study and in later years as part of the HRS. HRS and AHEAD respondents were selected using a multistage probability sample design, with oversampling of minorities and Florida residents. Table 1 shows the birth cohorts, sample sizes, and years of data collection for the HRS and the AHEAD Study.
Table 1.
Birth Cohorts, Sample Sizes, and Years of Data Collection a in the Health and Retirement Study and the Assets and Health Dynamics of the Oldest Old Survey, 1992–2004
| Survey Cohort | Year |
||||||||
| 1992 | 1993 | 1994 | 1995 | 1996 | 1998 | 2000 | 2002 | 2004 | |
| Health and Retirement Survey, 1931–1941 | 12,521 | 11,596 | 10,964 | 10,865 | 10,045 | 9,725 | 9,362 | ||
| Assets and Health Dynamics of the Oldest Old, before 1924 | 8,222 | 7,802 | 6,947 | 5,000 | 4,107 | 3,365 | |||
| Children of the Depression, 1924–1930 | 2,320 | 2,215 | 1,951 | 1,777 | |||||
| War Baby, 1942–1947 | 2,529 | 2,410 | 2,384 | 2,295 | |||||
| Early Baby Boomers, 1948–1953 | 3,330 | ||||||||
Online documentation of the Health and Retirement Study data collection path is available in reference 27.
Study sample
We used the 6 waves of data in this project (AHEAD: 1993 and 1995; HRS: 1998, 2000, 2002, and 2004) as repeated cross-sections to examine changes in the prevalence of cognitive impairment over time in Americans aged 70 years or older. Respondents who participated in any wave of the study were included in the analysis for that year. Therefore, respondents interviewed in multiple examination cycles were included in our analyses for every wave to which they contributed data after turning 70 years old. For example, an AHEAD respondent interviewed in 1993 and again in 1995 and 1998 contributed data to each data-collection wave. Similarly, an original HRS respondent would have contributed data for all waves in which he/she participated after turning 70 years old.
Inclusion and exclusion criteria.
Our study sample at each wave was restricted to noninstitutionalized adults aged 70 years or older at the time of interview. Nursing home residents were excluded, but respondents who resided in assisted living communities were included in the study sample. Respondents who did not identify themselves as white, black, or Hispanic were excluded. Respondents whose information was provided via proxy informant were not included in the results presented here; however, we used sensitivity analyses to examine changes in cognitive impairment among these “proxy respondents.” Table 2 shows the study sample size for each wave by race/ethnicity. The total sample size for the analyses with merged waves of data was 38,391.
Table 2.
Sample Size of Adults Aged 70 Years or Older by Year of Study and Race/Ethnicity in the Study Sample Drawn From the Health and Retirement Study, 1993–2004
| Race/Ethnicity | Year of Study |
|||||
| 1993 | 1995 | 1998 | 2000 | 2002 | 2004 | |
| Non-Hispanic white | 5,363 | 4,368 | 5,591 | 5,474 | 5,419 | 5,546 |
| Non-Hispanic black | 877 | 652 | 757 | 690 | 696 | 767 |
| Hispanic | 340 | 261 | 367 | 386 | 389 | 448 |
| All races | 6,580 | 5,281 | 6,715 | 6,550 | 6,504 | 6,761 |
Variables
Cognitive impairment.
We assessed cognitive functioning among those who responded to the survey on their own behalf by using a multidimensional measure based on a modified version of the Telephone Interview Cognitive Screen and tests of immediate and delayed verbal recall. The total cognition score comprised scores for 3 areas of functioning: memory (immediate word recall list and 5-minute delayed word recall task), working memory (Serial 7’s subtraction test), and mental status (backward count and date and object naming). Scores from each component measure were combined into a summary measure of cognitive function that ranged from 0 to 35, with higher scores representing better functioning. Cognitive impairment was defined as a score of 8 or less on the summary measure, according to the practice of AHEAD investigators and previous research (5, 14, 15).
Year trend.
The key independent variable was a continuously scaled variable representing the survey year. The “year” variable took the value of 0 in 1993 and increased by 1 each subsequent calendar year to 11 in 2004. The year variable assumed linearity of slope. Quadratic and cubic specifications of the trend variable were not statistically significant after adjustment for age, gender, and design effects.
Sociodemographic characteristics.
Race/ethnicity was categorized as non-Hispanic white, non-Hispanic black, or Hispanic. Other sociodemographic characteristics included age, gender, marital status, and region of birth. Educational level and net worth were used to indicate the socioeconomic status of respondents. Highest grade of school completed was classified into 4 categories by number of years: 0–8, 9–11, 12, and >12 years. Net worth was adjusted to 1993 dollars and stratified into tertiles. Maternal educational level (<8 years vs. ≥8 years) was included as an early life indicator of socioeconomic status.
Health status and health behavior.
Respondents reported whether a doctor had ever told them that they had high blood pressure, diabetes, cancer, lung disease, heart disease, stroke, or a psychiatric disorder. Obesity (body mass index, measured as weight (kg)/height (m)2, ≥30) and smoking status were also included. Respondents were asked to rate their vision (with glasses if typically used) and hearing (with a hearing aid if typically used) as falling into one of the following categories: excellent, very good, good, fair, or poor.
Prior test exposure.
Prior test exposure was included as a covariate to adjust for potential effects of repeat testing in this sample. Consistent with what was done in previous research, we measured prior test experience as a dichotomous variable that indicated whether or not a respondent had been previously tested (8).
Statistical analysis
Cross-sectional sample weights were available for each wave of the HRS. Respondent-level weights for 1993–2004 were drawn from the HRS tracker file (16). Cross-sectional sample weights were adjusted for nonresponse and loss to follow-up and were constructed to match the noninstitutionalized population for that year. Thus, the weighted waves of data approximated comparable cross-sections of the community-dwelling population of older Americans in the years 1993, 1995, 1998, 2000, 2002, and 2004.
We used descriptive and bivariate analyses to show percentage distributions for sociodemographic, health behavior, and health status variables at each wave. Chi-squared tests were used to assess changes in sample characteristics over the 6-wave study period. The prevalence of cognitive impairment was calculated for each wave, and the unadjusted trend was tested using logistic regression with year as the predictor. The annual percent decline in the prevalence of cognitive impairment was estimated as (1 − odds ratio) × 100.
In our main data analyses, we used multiple logistic regression analysis to evaluate the temporal trend in the prevalence of cognitive impairment, sequentially adjusting for demographic characteristics, socioeconomic status, and health to determine which factors attenuated observed trends. To test for modification of trends by race/ethnicity and socioeconomic status, we included terms for interactions between the year variable and these factors in models that were adjusted for age, gender, and prior test exposure. Analyses were also repeated using linear probability models to examine absolute (percentage point) rather than relative (percent) change in outcome.
As most respondents appeared in more than 1 wave, observations were not independent and the intraindividual errors were likely to be correlated. To adjust for overlap in samples across waves, respondent identity was set as a cluster variable using the STATA svyset procedure (17). In analyses, results were adjusted for the complex survey design of the HRS; that is, data were weighted to account for oversampling and poststratification adjustments to Current Population Survey estimates, and standard errors were adjusted to account for geographic clustering.
RESULTS
Table 3 presents weighted descriptive characteristics of the study samples in 1993 and 2004 stratified by race/ethnicity. Only 2 years of data are shown for simplicity; however, the P values represent changes in means or proportions across all years of study. The composition of the older white, black, and Hispanic populations changed between 1993 and 2004.
Table 3.
Trends in Demographic, Socioeconomic, and Health Status and Behavior Variables in Adults Aged 70 Years or Older, by Race/Ethnicity, Health and Retirement Study, 1993–2004a
| Race/Ethnicity, Year,b and Sample Size | Whites |
Blacks |
Hispanics |
||||||||||||
| 1993 (n = 5,363) |
2004 (n = 5,546) |
P Valuec | 1993 (n = 877) |
2004 (n = 767) |
P Valuec | 1993 (n = 340) |
2004 (n = 448) |
P Valuec | |||||||
| % | Mean (SE) | % | Mean (SE) | % | Mean (SE) | % | Mean (SE) | % | Mean (SE) | % | Mean (SE) | ||||
| Demographic characteristics | |||||||||||||||
| Age, years | 77.49 (0.10) | 77.73 (0.11) | <0.001 | 77.59 (0.24) | 77.01 (0.28) | <0.05 | 77.17 (0.32) | 77.09 (0.33) | <0.05 | ||||||
| Female gender | 59.84 | 57.90 | <0.05 | 61.91 | 63.33 | 59.48 | 60.16 | ||||||||
| Region of birth | <0.01 | <0.001 | |||||||||||||
| Northeastern United States | 25.41 | 26.06 | 5.37 | 4.18 | 1.99 | 10.40 | |||||||||
| Midwestern United States | 34.43 | 35.56 | 4.38 | 5.58 | 0.69 | 3.17 | |||||||||
| Southern United States | 25.85 | 24.98 | 85.83 | 84.67 | 29.77 | 19.92 | |||||||||
| Western United States | 7.53 | 8.30 | 0.60 | 1.41 | 11.55 | 21.34 | |||||||||
| US territory/outside the United States | 6.79 | 5.10 | 3.82 | 4.15 | 56.00 | 54.53 | |||||||||
| Veteran | 24.55 | 31.80 | <0.001 | 18.07 | 20.24 | 9.89 | 11.54 | ||||||||
| Marital status | |||||||||||||||
| Married | 54.05 | 55.01 | 36.80 | 34.93 | 48.55 | 49.63 | |||||||||
| Not married | 42.79 | 42.64 | 59.63 | 60.88 | 47.00 | 46.41 | |||||||||
| Never married | 3.16 | 2.35 | 3.57 | 4.19 | 4.50 | 3.96 | |||||||||
| Socioeconomic status | |||||||||||||||
| Maternal educational level, years | <0.001 | <0.001 | <0.05 | ||||||||||||
| <8 | 38.12 | 23.02 | 48.32 | 36.85 | 68.77 | 61.28 | |||||||||
| ≥8 | 51.11 | 66.44 | 28.48 | 41.04 | 18.60 | 20.76 | |||||||||
| Missing | 10.77 | 10.54 | 23.20 | 22.10 | 12.63 | 17.96 | |||||||||
| Educational level | <0.001 | <0.001 | <0.01 | ||||||||||||
| 0–8 years | 20.33 | 10.45 | 50.82 | 32.72 | 72.77 | 60.46 | |||||||||
| 9–11 years | 17.15 | 13.99 | 22.57 | 24.17 | 6.78 | 11.11 | |||||||||
| High school or equivalent | 33.00 | 37.42 | 15.51 | 24.34 | 12.17 | 18.58 | |||||||||
| More than high school | 29.52 | 11.50 (0.07) | 38.14 | 12.44 (0.06) | 11.10 | 8.30 (0.26) | 18.77 | 9.92 (0.21) | 8.27 | 6.12 (0.60) | 9.85 | 7.33 (0.50) | |||
| Total wealth (in 1993), $ | <0.001 | <0.05 | <0.05 | ||||||||||||
| <0–<40,000 | 25.96 | 19.06 | 64.75 | 58.69 | 64.56 | 56.06 | |||||||||
| 40,000–<145,000 | 35.37 | 25.87 | 25.88 | 30.72 | 24.36 | 21.94 | |||||||||
| ≥145,000 | 38.67 | 55.08 | 9.37 | 10.58 | 11.08 | 22.00 | |||||||||
| Health status and behavior | |||||||||||||||
| Chronic conditions | |||||||||||||||
| Hypertension | 47.75 | 60.94 | <0.001 | 64.23 | 74.58 | <0.001 | 50.81 | 62.84 | <0.001 | ||||||
| Diabetes | 11.07 | 17.57 | <0.001 | 22.44 | 29.93 | <0.001 | 21.40 | 29.79 | <0.05 | ||||||
| Cancer | 14.57 | 20.49 | <0.001 | 10.31 | 15.68 | <0.001 | 9.78 | 10.04 | |||||||
| Lung disease | 12.40 | 12.27 | 6.96 | 8.24 | 9.71 | 5.64 | <0.05 | ||||||||
| Heart disease | 32.69 | 35.91 | <0.001 | 26.89 | 30.59 | 24.12 | 23.52 | ||||||||
| Stroke | 10.43 | 9.97 | 12.01 | 13.58 | 8.05 | 9.14 | |||||||||
| Psychiatric disorder | 10.64 | 13.26 | <0.001 | 10.52 | 12.25 | 15.72 | 16.59 | ||||||||
| Depressive symptoms | 1.49 (0.03) | 1.41 (0.03) | 1.87 (0.08) | 1.85 (0.07) | 2.34 (0.14) | 1.83 (0.74) | |||||||||
| Obesity (body mass indexd ≥30) | 12.04 | 17.45 | <0.001 | 22.89 | 29.89 | <0.05 | 18.22 | 23.02 | |||||||
| Smoking | <0.001 | <0.01 | |||||||||||||
| Current | 9.51 | 7.31 | 12.53 | 9.31 | 11.27 | 6.34 | |||||||||
| Former | 43.29 | 48.55 | 37.20 | 46.49 | 43.37 | 43.03 | |||||||||
| Never | 47.20 | 44.14 | 50.27 | 44.20 | 45.35 | 50.63 | |||||||||
| Self-rated vision | <0.001 | <0.01 | <0.001 | ||||||||||||
| Excellent/very good | 38.97 | 32.53 | 27.44 | 20.05 | 31.23 | 21.61 | |||||||||
| Good | 36.07 | 44.05 | 35.86 | 41.75 | 34.52 | 36.73 | |||||||||
| Fair/poor/blind | 24.96 | 23.42 | 36.71 | 38.20 | 34.25 | 41.67 | |||||||||
| Self-rated hearing | <0.05 | ||||||||||||||
| Excellent/very good | 37.13 | 34.87 | 38.03 | 32.92 | 33.69 | 25.53 | |||||||||
| Good | 37.02 | 35.76 | 36.64 | 39.09 | 32.42 | 36.87 | |||||||||
| Fair/poor | 25.85 | 29.37 | 25.33 | 27.99 | 33.89 | 37.60 | |||||||||
Abbreviation: SE, standard error.
Estimates were weighted using the Health and Retirement Study respondent population weights to adjust for the complex sampling design of the Health and Retirement Study survey.
Only estimates for 1993 and 2004 are shown here; however, reported P value is for all years.
P value for chi-squared or t test (for year trend variable from linear regression) for a significant difference in proportion or mean across years.
Weight (kg)/height (m)2.
Socioeconomic status increased over time among all 3 racial/ethnic groups. Older adults in 2004 were less likely to report mothers who had fewer than 8 years of education, and the mean educational levels of respondents increased over time. In 1993, 63% of whites, 27% of blacks, and 20% of Hispanics had completed high school, compared with 76%, 43%, and 28%, respectively, in 2004. Total wealth (in constant 1993 dollars) increased over time for whites, blacks, and Hispanics.
Prevalence rates of hypertension, diabetes, and obesity increased among all groups, although the change in the obesity rate was not statistically significant for Hispanics. There were increases in the number of reports of cancer for whites and blacks, whereas lung disease decreased among Hispanics. Smoking rates decreased for all groups from 1993 to 2004, but the change was not statistically significant for Hispanics (P = 0.07). There were increases in reports of psychiatric disorders and hearing problems among whites, and the number of vision problems increased for blacks and Hispanics.
Overall trends in cognitive impairment
Table 4 shows trends in mean cognitive scores and the prevalence of cognitive impairment overall and by race/ethnicity. The prevalence of cognitive impairment declined from 4.17% to 2.00% (P < 0.001) between 1993 and 2004, representing an absolute decrease of 2.17% points and an annual percent change of −4.34%. The improvements in cognitive scores did not appear to be due to increased scores in any particular subscale (data not shown). Mean scores increased across time for each subscale, as well as for total cognition score.
Table 4.
Percentage With Cognitive Impairment Overall and by Race/Ethnicity in Self-Respondents Aged 70 Years or Older in the United States, Health and Retirement Study 1993–2004a
| Year |
Average Annual % Changeb | P Valuec | ||||||||||||
| 1993 |
1995 |
1998 |
2000 |
2002 |
2004 |
|||||||||
| Mean (SD) | % (SE) | Mean (SD) | % (SE) | Mean (SD) | % (SE) | Mean (SD) | % (SE) | Mean (SD) | % (SE) | Mean (SD) | % (SE) | |||
| Total cognition score (range: 0–35) | 19.73 (0.10) | 20.14 (0.12) | 20.99 (0.09) | 21.02 (0.10) | 21.10 (0.09) | 21.05 (0.08) | 0.0089 | <0.001 | ||||||
| Percent with severe impairment (≤8 of 35) | 4.17 (0.34) | 3.30 (0.26) | 2.55 (0.23) | 2.19 (0.19) | 2.15 (0.22) | 2.00 (0.21) | −4.336 | <0.001 | ||||||
| Percent with mild impairment (≤10 of 35) | 7.02 (0.39) | 6.15 (0.32) | 4.19 (0.29) | 3.97 (0.27) | 4.13 (0.28) | 3.72 (0.24) | −3.917 | <0.001 | ||||||
| Percent with severe impairment by race/ethnicity | ||||||||||||||
| White | 2.89 (0.31) | 2.38 (0.28) | 1.83 (0.20) | 1.60 (0.17) | 1.52 (0.21) | 1.55 (0.18) | −3.864 | <0.0001 | ||||||
| Black | 15.91 (1.87) | 13.09 (2.04) | 8.47 (1.22) | 8.20 (1.21) | 8.15 (1.44) | 5.92 (1.35) | −5.233 | <0.0001 | ||||||
| Hispanic | 11.55 (1.93) | 5.94 (1.10) | 7.31 (1.84) | 3.64 (1.14) | 4.71 (1.01) | 4.98 (0.93) | −4.740 | <0.0001 | ||||||
Abbreviations: SD, standard deviation; SE, standard error.
Estimates were weighted using the Health and Retirement Study respondent population weights to adjust for the complex sampling design of the Health and Retirement Study.
Year trend estimate from logistic regression analysis with cognitive impairment as the dependent variable (coded 1 for score ≥8 on cognitive measure, 0 otherwise) and year of study as the predictor. Year trend estimates for changes in total cognition score were from linear regression analysis with total cognition score as the dependent variable and year of study as the predictor.
P value for year trend estimate from logistic regression analysis for a significant difference in the proportion across years.
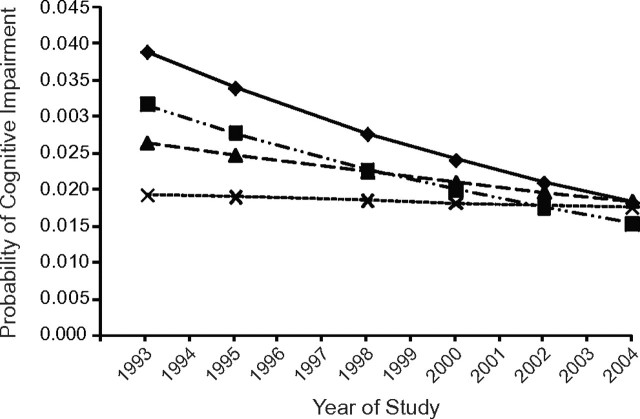
Figure 1 shows unadjusted and adjusted trends in the probability of cognitive impairment among older adults. The figure displays results from successive logistic regression models with a year variable. When plotting results, we substituted 78 years for age, 0.75 for prior testing (i.e., retesting for 75% of sample), and 11 years for educational level. Adding prior testing to the age-adjusted model attenuated the slope of the trend line. After adjustment for educational level, the slope of the trend line was nearly 0.
Figure 1.
Unadjusted and adjusted trends in the probability of cognitive impairment among older Americans in the US Health and Retirement Study, 1993–2004. Estimates are from successive logistic regression models with a year trend variable: unadjusted (diamonds; P < 0.001); age-adjusted (squares; P < 0.001); adjusted for age and prior exposure to the cognitive test (triangles; P = 0.012); and adjusted for age, prior exposure to the cognitive test, and educational level (x's; P = 0.546). When plotting results, we substituted 78 years for age, 0.75 for prior testing (i.e. retesting for 75% of sample), and 11 years for educational level.
Multivariate logistic regression models were estimated to test for trends in the prevalence of cognitive impairment. The base model adjusted for age and gender showed a significant decline in the prevalence of cognitive impairment of 6.6% per year (odds ratio = 0.934, 95% confidence interval: 0.913, 0.956). Adjustment for prior exposure to the cognitive test reduced the trend to 3.4% (odds ratio = 0.966, 95% confidence interval: 0.941, 0.992). Covariates were added to the model sequentially (results not shown). When we included race/ethnicity, birthplace, and marital status in the models, the trend slightly increased to a 3.5% annual decline. Adding socioeconomic variables to the model attenuated the cognitive impairment trend by 72.1%; that is, the trend was reduced from 3.5% to 1%, which was not statistically significant (odds ratio = 0.990, 95% confidence interval: 0.961, 1.020). Including health status and behavior variables in the models changed the trend by less than 10%. Health variables were also added individually to the model so that we could investigate the influence of each factor. The inclusion of vision impairment and smoking attenuated the trend estimate by 8.8% and 2.1%, respectively. Adding psychiatric disorders, obesity, stroke, hearing impairment, and diabetes increased the trend by 2%–7%.
Trends by race/ethnicity and socioeconomic status
The prevalence of cognitive impairment decreased for all racial/ethnic groups, but improvements were larger for blacks and Hispanics than for non-Hispanic whites (Table 4). The annual percent decline in cognitive impairment was 3.9% for whites, 5.2% for blacks, and 4.7% for Hispanics. Racial/ethnic disparities in cognitive impairment were substantial in 1993: 15.91% of blacks and 11.55% of Hispanics were impaired, compared with 2.89% of whites. The magnitude of the differences declined considerably between 1993 and 2004; the decline was 8.65 percentage points between whites and blacks and 5.23 percentage points between whites and Hispanics.
Multivariate analyses with interaction terms.
Multivariate logistic regression models with interaction terms were used to test for differences in trends between groups. Odds ratios indicating annual percent decline in cognitive impairment are presented for each group in Table 5. The differences in trends across racial/ethnic, educational and wealth groups were not statistically significant, though declines were somewhat larger for blacks and Hispanics than for non-Hispanic whites. In sensitivity analyses, general conclusions were robust to alternative categorizations of race/ethnicity (black, nonblack; white, nonwhite) and educational level.
Table 5.
Adjusted Odds Ratiosa From Logistic Regression Models Showing Time Trends in Cognitive Impairment by Race/Ethnicity, Educational Level, and Total Wealth Among Adults Aged 70 Years or Older in the Health and Retirement Study, 1993–2004
| Variable | Model 1 |
Model 2 |
Model 3 |
Model 4 |
||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Year trend | 0.966 | 0.941, 0.992 | ||||||
| Year trend × race/ethnicityb | ||||||||
| White | 0.971 | 0.936, 1.006 | ||||||
| Black | 0.943 | 0.914, 0.973 | ||||||
| Hispanic | 0.954 | 0.912, 0.997 | ||||||
| Year trend × educational levelc | ||||||||
| 0–8 years | 0.987 | 0.955, 1.021 | ||||||
| 9–11 years | 0.966 | 0.924, 1.010 | ||||||
| 12 years | 1.005 | 0.958, 1.055 | ||||||
| ≥12 years | 0.994 | 0.948, 1.042 | ||||||
| Year trend × wealthd | ||||||||
| <$0–<$40,000 | 0.966 | 0.936, 0.997 | ||||||
| $40000–<$145,000 | 0.975 | 0.936, 1.017 | ||||||
| ≥$145,000 | 0.991 | 0.947, 1.038 | ||||||
| Covariates | ||||||||
| Age | 1.130 | 1.12, 1.15 | 1.14 | 1.13, 1.15 | 1.12 | 1.11, 1.13 | 1.12 | 1.11, 1.13 |
| Female gender | 0.970 | 0.82, 1.14 | 0.94 | 0.79, 1.11 | 1.00 | 0.84, 1.20 | 0.77 | 0.64, 0.92 |
| Prior test exposure | 0.630 | 0.54, 0.74 | 0.65 | 0.55, 0.76 | 0.66 | 0.56, 0.78 | 0.69 | 0.58, 0.81 |
| Main effects | ||||||||
| Race/ethnicity(reference group = white) | ||||||||
| Black | 6.99 | 4.77, 10.24 | ||||||
| Hispanic | 4.33 | 2.83, 6.63 | ||||||
| Educational level (reference group = ≥12 years) | ||||||||
| 0–8 years | 7.63 | 4.80, 12.11 | ||||||
| 9–11 years | 2.75 | 1.76, 4.28 | ||||||
| 12 years | 1.33 | 0.79, 2.23 | ||||||
| Wealth, $ (reference group = ≥145,000) | ||||||||
| <0–<40,000 | 5.70 | 4.00, 8.12 | ||||||
| 40,000–<145,000 | 2.31 | 1.72, 3.11 | ||||||
Abbreviations: CI, confidence interval; OR, odds ratio.
Odds ratios were from weighted logistic regression models adjusted for the complex survey design of the Health and Retirement Study. The annual percent decline in the prevalence of cognitive impairment was estimated as (1 − OR) × 100.
Test for equality of the trend between race/ethnicity groups (reference group = white): black, P = 0.187; Hispanic, P = 0.519.
Test for equality of the trend between educational level groups (reference group = ≥12 years): 0–8 years, P = 0.804; 9–11 years, P = 0.367; and 12 years, P = 0.662.
Test for equality of the trend between wealth groups (reference group = ≥$145,000): <$40,000, P = 0.300; $40,000–<$145,000, P = 0.526.
Analyses were also repeated using linear probability models (data not shown), which provided estimates of absolute (percentage-point change) decline over time. Linear probability models were used to examine trends because descriptive results showed large absolute declines in cognitive impairment among blacks and Hispanics. Results from linear probability models showed that interaction terms for race/ethnicity, educational level, and wealth were statistically significant. The rate of percentage point decline was significantly higher among blacks (b = −0.694, P < 0.001) and Hispanics (b = −0.360, P = 0.011) than among whites (b = −0.008, P = 0.827). Rates of decline were higher in the lowest educational level group (b = −0.272, P = 0.019) than in those with more than 12 years of education (b = 0.066, P = 0.055). Cognitive function declined faster in the lowest wealth group (b = −0.270, P = 0.001) than in the highest group (b = 0.048, P = 0.091).
DISCUSSION
The present results show a downward trend in the prevalence of cognitive impairment from 1993 to 2004 that was independent of changes in the age and gender distributions of the population. Socioeconomic variables attenuated the observed relative decline by 72%, which suggests that improvements in socioeconomic status—particularly educational level—contributed to changes in the prevalence of cognitive impairment over time. Changes in health status and behavior changed the trends in cognitive impairment by about 10%. Including psychiatric disorders, obesity, stroke, hearing impairment, and diabetes in the models actually increased the trend, which suggests that cognitive impairment may have declined more were it not for increases in the rates of chronic diseases in the older population.
Although the prevalence of cognitive impairment declined in each racial/ethnic group, larger declines were observed for blacks and Hispanics. Substantial changes in the prevalence of cognitive impairment among these groups likely contributed to the observed trend for the total population. Absolute changes in the prevalence of cognitive impairment were larger for blacks and Hispanics than for whites, which caused racial/ethnic disparities in cognitive impairment to narrow over time. To the extent that these trends represent real changes, these results are encouraging for the state of health disparities in the United States.
Population health trends can be characterized using various measurement approaches, which could provide different trend estimates or answers about health trends (18, 19). Our results showed that annual relative trends in cognitive impairment were not significantly different across subgroups, but absolute changes were larger for minorities and lower socioeconomic groups. The base (prevalence of cognitive impairment in 1993) for calculating the annual percentage of decline was much lower for advantaged groups, so small percentage-point improvements yielded relative annual trends similar to those of disadvantaged groups, for whom absolute changes were much larger.
Previous research on trends in cognitive impairment did not examine trends in disparities across sociodemographic groups. However, results from the present investigation are consistent with descriptive results from the study by Freedman et al. (5), which showed that the prevalence of impairment decreased more steeply between 1993 and 1998 for nonwhites (15.9%–7.6%) than for whites (3.3%–1.8%) and for Hispanics (11.7%–6.7%) than for non-Hispanics (4.5%–2.2%). However, Freedman et al. presented only crude results and did not test for interactions among the racial/ethnic groups. Other studies (6, 7, 20) did not examine race/ethnicity- or socioeconomic-specific trends in cognitive impairment.
Repeated exposure to cognitive measures could result in learning effects, which could improve respondents’ scores in later years and confound comparisons over time. This investigation included a variable that indicated prior exposure to the cognitive test to adjust trend estimates for potential learning effects. Adjustment for prior test exposure in multivariate analyses reduced the annual trend considerably, from −6.6% to −3.4%. This trend represented a statistically significant decline in cognitive impairment. Researchers in previous studies have used data from panel surveys to investigate trends in cognitive impairment (5–8); however, only one group (8) attempted to adjust trend estimates for prior test exposure. Rodgers et al. (8) found little change in levels of cognitive functioning from 1993 to 2000 after adjustment for age and prior testing.
Increases in the educational levels of older adults in the United States appear to have contributed to declines in the prevalence of cognitive impairment. Interpretation of these results is somewhat complicated, however, because education is causally related to cognitive functioning, improves test-taking ability, and represents a proxy for an array of available resources and opportunities over the life course. Increases in the quantity and quality of education could be responsible for the downward trends in cognitive impairment among blacks and Hispanics relative to whites. Descriptive results showed that increases in educational level occurred at a faster rate among blacks and Hispanics than among whites. Mean years of education increased approximately 20% for blacks and Hispanics and 9% for whites from 1993 to 2004. Other research has shown that the difference in mean years of education completed by blacks and whites declined from 3.46 for those born in the early 1900s to 0.83 for those born in the 1950s (21).
There are several limitations to the present study. First, prevalence estimates for the current project were based on the noninstitutionalized population. Changes in rates of institutionalization of older adults in the United States during the study period could have affected trend estimates. Second, the HRS is a longitudinal survey that has new cohorts added every 6 years. Increases over time in loss to follow-up or death could bias prevalence estimates downward in later years, inflating the trend estimate. To address these issues, changes in rates of death, attrition, and institutionalization were examined over subsequent 2-wave intervals of the HRS. Rates of death and attrition declined significantly, whereas rates of institutionalization did not significantly change over the study period. These results suggested that survey design issues do not explain the declines in cognitive impairment from 1993 to 2004. Nevertheless, selection bias remains a concern, to the extent that sample replenishment did not adequately replace participants who were lost between waves. Changes in the composition of the institutionalized population (e.g., an increased number of impaired individuals) could also bias trend estimates. The prevalence of disability in the nursing-home population increased slightly from 1995 to 1999 (22). The percentage of residents receiving assistance with 4–6 activities of daily living increased from 75.3% to 77.2%. The proportion of nursing home residents who were black increased from 8.6% in 1995 to 11.0% in 2004 (23); however, the percentage of black residents receiving assistance with 4–6 activities of daily living did not change from 1995 to 1999 (22). Only those who responded on their own behalf were included in this study, and changes in proxy respondents over the study period may influence results. However, though the proportion of proxy respondents decreased over time (data not shown), additional analyses showed no statistically significant changes in cognitive impairment among proxy respondents, as measured by global ratings of memory and judgment, and behavioral symptoms (1993–2002) and the Jorm IQCODE (1995–2004), as judged by individuals providing data for proxy respondents.
Third, the cognitive function measure used in these analyses identified any type of cognitive impairment in the older population. The cognitive measure indicated symptomatic cognitive impairment rather than a clinical diagnosis. The identification and classification of diagnosed forms of cognitive impairment, including mild cognitive impairment, dementia, and Alzheimer disease, in population-based survey research is a major challenge. The cutoff score of 8 was chosen for the cognitive function measure in the present study to identify cognitive impairment consistent with dementia. This threshold has been shown to be a sensitive and specific indicator of clinical dementia (24–26). Nevertheless, trends in the prevalence of diagnosable forms of cognitive impairment might not parallel those observed for the cognitive impairment measure in the present study.
Fourth, it is possible that the measurements of health status and behaviors in the HRS limited our ability to detect the influence of these factors on trends in cognitive impairment. The prevalence of self-reported health conditions might not capture the health status changes that would be important for trends in cognitive impairment. Self-report measures provide no indication of the severity, management, treatment, or control of the disease, and they are subject to recall bias, error, and changes in diagnostic criteria over time.
Measurement of health trends in older adults is important for determining public health and policy priorities and is relevant given the aging of the US population. It is important to identify and understand the mechanisms responsible for population-level changes in the health of older adults. It is unclear whether the trends observed in the present investigation may be expected to continue and what patterns may characterize future periods. Different trends in population health could result, depending on relative changes in the processes of disease, cognitive impairment, and mortality (19).
Acknowledgments
Author affiliations: Department of Surgery, University of Texas Medical Branch, Galveston, Texas (Kristin M. Sheffield); and Department of Preventive Medicine and Community Health, Division of Sociomedical Sciences, University of Texas Medical Branch, Galveston, Texas (M. Kristen Peek).
This work was supported by the National Institute on Aging (grant T32-AG00270).
The authors thank Drs. Laura Rudkin, Mukaila Raji, Rebeca Wong, and Fredric Wolinsky for their valuable comments and contributions.
Conflict of interest: none declared.
Glossary
Abbreviations
- AHEAD
Assets and Health Dynamics of the Oldest Old
- HRS
Health and Retirement Study
References
- 1.Federal Interagency Forum on Aging Related Statistics. Older Americans 2000: Key Indicators of Well-Being. Washington, DC: US GPO; 2000. [Google Scholar]
- 2.Evans DA. Estimated prevalence of Alzheimer's disease in the United States. Milbank Q. 1990;68(2):267–289. [PubMed] [Google Scholar]
- 3.Hebert LE, Scherr PA, Bienias JL, et al. Alzheimer disease in the US population: prevalence estimates using the 2000 census. Arch Neurol. 2003;60(8):1119–1122. doi: 10.1001/archneur.60.8.1119. [DOI] [PubMed] [Google Scholar]
- 4.Brookmeyer R, Gray S, Kawas C. Projections of Alzheimer's disease in the United States and the public health impact of delaying disease onset. Am J Public Health. 1998;88(9):1337–1342. doi: 10.2105/ajph.88.9.1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Freedman VA, Aykan H, Martin LG. Aggregate changes in severe cognitive impairment among older Americans: 1993 and 1998. J Gerontol B Psychol Sci Soc Sci. 2001;56(2):S100–S111. doi: 10.1093/geronb/56.2.s100. [DOI] [PubMed] [Google Scholar]
- 6.Langa KM, Larson EB, Karlawish JH, et al. Trends in the prevalence and mortality of cognitive impairment in the United States: is there evidence of a compression of cognitive morbidity? Alzheimers Dement. 2008;4(2):134–144. doi: 10.1016/j.jalz.2008.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Manton KC, Gu XL, Ukraintseva SV. Declining prevalence of dementia in the U.S. elderly population. Adv Gerontol. 2005;16:30–37. [PubMed] [Google Scholar]
- 8.Rodgers WL, Ofstedal MB, Herzog AR. Trends in scores on tests of cognitive ability in the elderly U.S. population, 1993–2000. J Gerontol B Psychol Sci Soc Sci. 2003;58(6):S338–S346. doi: 10.1093/geronb/58.6.s338. [DOI] [PubMed] [Google Scholar]
- 9.Kramarow E, Lubitz J, Lentzner H, et al. Trends in the health of older Americans, 1970–2005. Health Aff (Millwood) 2007;26(5):1417–1425. doi: 10.1377/hlthaff.26.5.1417. [DOI] [PubMed] [Google Scholar]
- 10.Sloan FA, Wang J. Disparities among older adults in measures of cognitive function by race or ethnicity. J Gerontol B Psychol Sci Soc Sci. 2005;60(5):P242–P250. doi: 10.1093/geronb/60.5.p242. [DOI] [PubMed] [Google Scholar]
- 11.Mehta KM, Simonsick EM, Rooks R, et al. Black and white differences in cognitive function test scores: what explains the difference? J Am Geriatr Soc. 2004;52(12):2120–2127. doi: 10.1111/j.1532-5415.2004.52575.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gurland BJ. Rates of dementia in three ethnoracial groups. Int J Geriatr Psychiatry. 1999;14(6):481–493. [PubMed] [Google Scholar]
- 13.Perkins P. Incidence and prevalence of dementia in a multiethnic cohort of municipal retirees. Neurology. 1997;49(1):44–50. doi: 10.1212/wnl.49.1.44. [DOI] [PubMed] [Google Scholar]
- 14.Herzog AR, Wallace RB. Measures of cognitive functioning in the AHEAD study. J Gerontol B Psychol Sci Soc Sci. 1997;52(special issue):37–48. doi: 10.1093/geronb/52b.special_issue.37. [DOI] [PubMed] [Google Scholar]
- 15.Suthers K, Kim JK, Crimmins E. Life expectancy with cognitive impairment in the older population of the United States. J Gerontol B Psychol Sci Soc Sci. 2003;58(3):S179–S186. doi: 10.1093/geronb/58.3.s179. [DOI] [PubMed] [Google Scholar]
- 16.University of Michigan. Health and Retirement Study: Tracker 2008: Version 1.0. Ann Arbor, MI: University of Michigan; 2008. ( http://hrsonline.isr.umich.edu/modules/meta/tracker/desc/trk2008.pdf). (Accessed August 22, 2009) [Google Scholar]
- 17.Stata Corporation, LP. Stata Statistical Software: Release 10. College Station, TX: StataCorp LP; 2007. [Google Scholar]
- 18.Freedman VA, Crimmins E, Schoeni RF, et al. Resolving inconsistencies in trends in old-age disability: report from a technical working group. Demography. 2004;41(3):417–441. doi: 10.1353/dem.2004.0022. [DOI] [PubMed] [Google Scholar]
- 19.Crimmins EM. Trends in the health of the elderly. Annu Rev Public Health. 2004;25:79–98. doi: 10.1146/annurev.publhealth.25.102802.124401. [DOI] [PubMed] [Google Scholar]
- 20.Liao Y, McGee DL, Cao G, et al. Quality of the last year of life of older adults: 1986 vs 1993. JAMA. 2000;283(4):512–518. doi: 10.1001/jama.283.4.512. [DOI] [PubMed] [Google Scholar]
- 21.Kalmijn M, Kraaykamp G. Race, cultural capital, and schooling: an analysis of trends in the United States. Sociol Educ. 1996;69(1):22–34. [Google Scholar]
- 22.Federal Interagency Forum on Aging Related Statistics. Older Americans 2004: Key Indicators of Well-Being. Washington, DC: US GPO; 2004. [Google Scholar]
- 23.Federal Interagency Forum on Aging Related Statistics. Older Americans 2008: Key Indicators of Well-Being. Washington, DC: US GPO; 2008. [Google Scholar]
- 24.Plassman BL, Langa KM, Fisher GG, et al. Prevalence of cognitive impairment without dementia in the United States. Ann Intern Med. 2008;148(6):427–434. doi: 10.7326/0003-4819-148-6-200803180-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Plassman BL, Newman T, Welsh KA, et al. Telephone interview for cognitive status: application in epidemiological and longitudinal studies. Neuropsychiatry Neuropsychol Behav Neurol. 1994;7(3):235–241. [Google Scholar]
- 26.Welsh KA, Breitner JCS, Magruder-Habib KM. Detection of dementia in the elderly using telephone screening of cognitive status. Neuropsychiatry Neuropsychol Behav Neurol. 1993;6(2):103–110. [Google Scholar]
- 27.Health and Retirement Study. Data Collection Path. Ann Arbor, MI: University of Michigan; 1992. ( http://hrsonline.isr.umich.edu/index.php?p=dflow). Accessed November 1, 2010. [Google Scholar]