Abstract
The present study was carried out to evaluate the role of Uttar Basti in tubal blockage, in order to establish it as a safer and cost-effective Ayurvedic treatment modality. The criteria for selection of patients and assessment of results were unilateral or bilateral tubal blockage diagnosed in hysterosalpingography (HSG). A total of 16 patients in the reproductive age group were registered for the study, with 62.50% unilateral and 37.50% bilateral tubal blockage. Fifteen patients completed the course of treatment. The patients with an evidence of active infection or chronic diseases were excluded. Kumari Taila was selected for its Vata Kapha Shamaka and Lekhana properties. The dose of Uttar Basti was 5 ml with duration of two consecutive cycles (six days of Uttar Basti in each cycle with an interval of three days in between). Uttar Basti was administered, after cessation of menstruation, to the screened patients, through hematological, urinary, and serological (HIV, VDRL, HBsAg) investigations. The tubal blockage was removed in 80% of the patients, and 40% of the patients had conceived within the follow-up period of two months. The results suggest that Uttar Basti is a highly significant treatment modality for tubal blockage, with no apparent complications.
Keywords: Tubal blockage, Uttar Basti, Kumari Taila, HSG
Introduction
It is always difficult to describe and understand something very large and covering several things. It is true with Ayurvedic principles that Ayurveda covers all the physical, mental, and spiritual aspects of human life, and hence, description becomes more abstract. Artavavaha Srotas is also the same. It covers the whole female reproductive tract and encompasses it as a structural and functional unit from the hypothalamus to the uterus. It represents not only the hormones related to reproduction at the physiological level, but also covers all the structures related to female reproductive organs at the anatomical level. Fallopian tubes are very important structures of the Artavavaha Srotas, as they carry Bija Rupi Artava. Artava is also termed as Raja at various places in the classics. Thus, fallopian tubes can be termed as Artava Bija Vaha Srotas to prevent any ambiguity and controversy. Tubal blockage is responsible for 25 – 35% of female infertility.[1] It is one of the most notorious factors of female infertility and very difficult to manage. Claims have been made with regard to the effect of intrauterine Uttar Basti (IUUB) on tubal blockage. However, no database evidence of research study is available. Hence, this study was carried out as a very preliminary, but sincere step on the path of infertility management through Ayurveda.The aims and objectives of the study include: (i) Evaluation of the efficacy of Kumari Taila Uttar Basti in tubal blockage and (ii) a study of the complications, if any, during and after the course of treatment.
Materials and Methods
Patients attending the OPD of the Stree Roga and Prasooti Tantra, Institute for Post Graduate Teaching and Research in Ayurveda Hospital, Jamnagar fulfilling the criteria for selection, were incorporated into the study.
Criteria for selection of cases
Patients of childbearing age having complaints of failure to conceive due to tubal factor, diagnosed on the basis of hysterosalpingogram (HSG) were registered for the study.Patients having any urogenital infection, history of excessive menstruation, suffering from any chronic debilitating disease, sexually transmitted diseases, human immunodeficiency virus (HIV), hepatitis B, contagious diseases, and so on, were excluded from the study. A total of 16 patients were registered and 15 patients completed the course of treatment. One patient had to discontinue the treatment due to personal family problems.Routine hematological investigations and urinary analysis were done before and after the treatment.
Selection of the drug
Tubal blockage was considered as a Vata-Kapha-dominated Tridoshaja condition, as Vata was responsible for Samkocha,[2] Kapha for Shopha, and Pitta for Paka.[3] Thus, all the three Dosha were collectively responsible for the stenosis or the obstructing type of pathology of the fallopian tubes. The drug was selected on the basis of Vata–Kaphashamaka and Tridoshaghna, having Ushna–Tikshna–Sara–Laghu–Pramathi and Sukshma properties, so that it could remove the blockage by reaching up to the minute channels. Hence, Kumari Taila mentioned in Bhava Prakasha,[4] was selected for its contents with the same type of properties. The drug was prepared in the Pharmacy of Gujarat Ayurved University, Jamnagar, as per the method mentioned in the text after the pharmacognostical analysis of the raw drugs. The prepared drug was analyzed pharmaceutically. Considering the organoleptic parameters, the drug had a dark-red color, aromatic odor, dark appearance, and thick consistency. The results on the physicochemical parameters, such as, loss on drying, refractive index, specific gravity, acid value, saponification value, and iodine value were 0.25%, 1.454, 0.522, 9.986 w/w, 192.95 w/w, and 92.50 w/w, respectively.
Treatment protocol
Five milliliters of Uttar Basti for six days, in one cycle (after cessation of menstruation), was given with an interval of three days in between,[5] for two consecutive cycles, with the consent of the patient. The patient was admitted for Uttar Basti, a day after cessation of menstruation. Snehana (oleation) of Bala Taila[6] on the lower abdomen, back, and lower limbs followed by Nadi Sveda (fomentation) with water steam on the lower abdomen and back was given to patients before each Uttar Basti. Yoni Prakshalana with Panchavalkala Kvatha[7] was performed to sterilize the peri vaginal part. The procedure was carried out in the operation theater. The oil and instruments were autoclaved. The patient was placed on the operation table in a dorsal lithotomy position. The private part (already shaved) was cleaned with antiseptic solution. The vagina and cervix were visualized with the help of the Sim's speculum[8] and an anterior vaginal wall retractor.[9] The anterior lip of the cervix was held with the help of the Allis’ forceps.[10] Uterine sounding was done and then Uttar Basti cannula, already attached with 5 mL syringe filled with Kumari Taila was passed into the uterine cavity after making a head low position. The drug was pushed above the level of the internal os with constant force, but quickly to make the drug reached up to the tubes. The patient was sent to bed and the bed was kept with head low for two hours. The lower abdomen was fomented with hot water bag. Patients were asked to avoid very spicy food during treatment. Coitus was prohibited during the course of Uttar Basti and proper care was taken to see that patients did not suffer from constipation.
Notification of complications
As the Taila prepared with Ushna–Tikshna Dravya was administered inside the uterus, the possibility of complications could not be neglected totally. Per vaginal bleeding and lower abdominal pain were the most probable complaints during and after the procedure. They were considered as complications, only if were very troublesome for the patient. The feature of urogenital infection during and after the procedure was also considered as a complication. Hence, close surveillance was kept to detect complications as early as possible.
End points
If some conditions developed during treatment, it was decided to stop the treatment; for example: (i) if the patient conceived in between the course of the study, (ii) if signs of any type of urogenital infections were observed, (iii) if heavy per vaginal bleeding started, and (iv) if abdominal pain occurred, which troubled the patient lot.
Follow-up study
A follow-up study for pregnancy was carried out for two months after completion of the treatment. Any new complaint that emerged during the follow-up period related to the study was also noted.
Observations and Results
The observations of the study are presented in Figures 1–4 and Table 1. The X-ray of patients with cornual block are given in Figures 5–7. The effect of therapy is shown in Tables 2–5.
Figure 1.
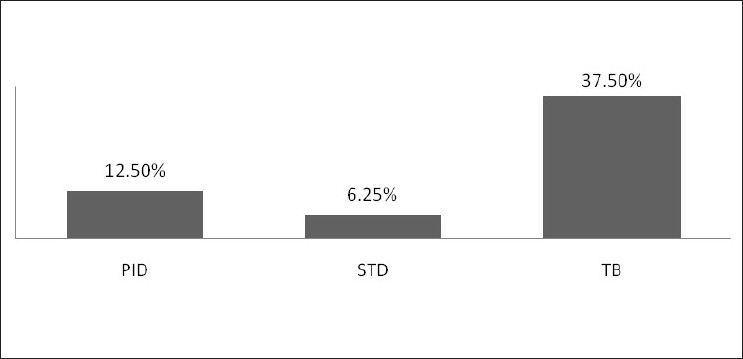
Number (%) of patients with previous history of infection (n = 16)
Figure 4.
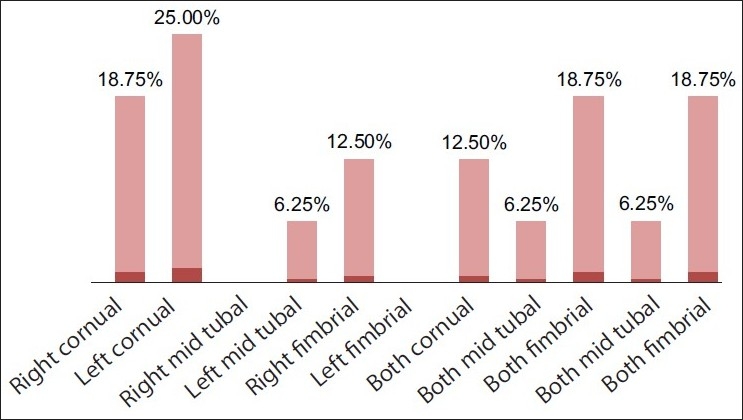
Number (%) of patients with various sites of tubal blockage (n = 16)
Table 1.
Number (%) of patients with various clinical manifestations during and after procedure (n = 15)
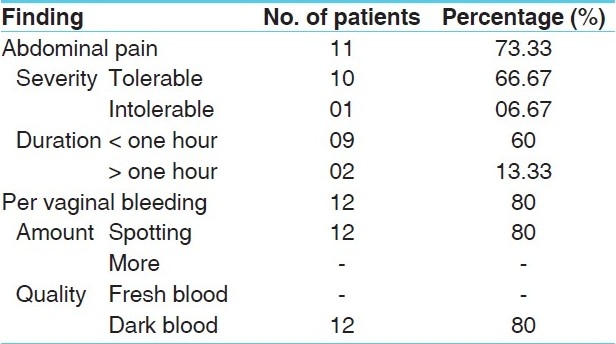
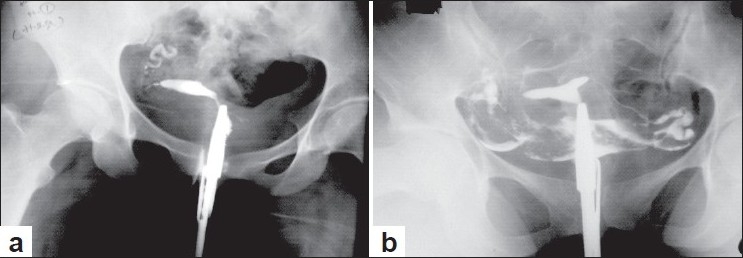
Figure 5.
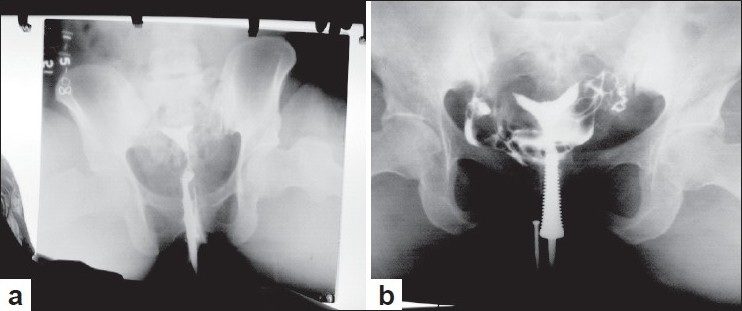
a) Bilateral cornual block before treatment, b) Patent bilateral tubes after treatment
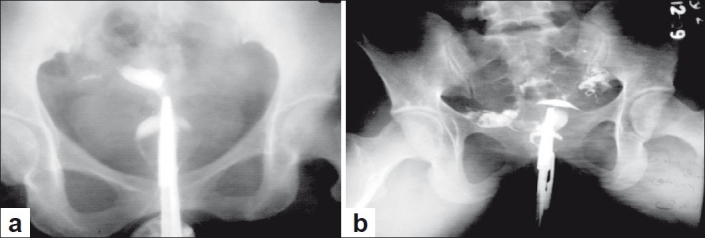
Figure 7.
a) Right cornual block before treatment, b) Patent bilateral tubes after treatment
Table 2.
Effect of therapy
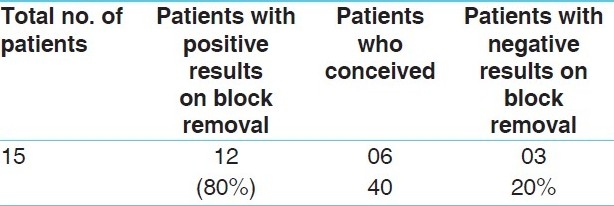
Table 5.
Effect of therapy on Artavakshaya
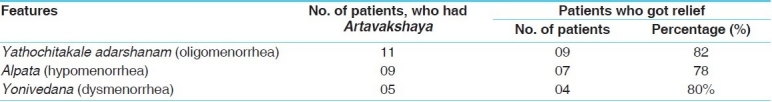
Figure 6.
a) Right cornual, left mid tubal block,before treatment, b) Patent bilateral tubes after treatment
Discussion
It has been established that in only 40% of the cases of tubal blockage, a previous history of pelvic inflammatory disease (PID) has been found, and in 60% of the patients, it has not been possible to elicit the history of PID, although it is the most important etiological factor of tubal blockage.[11] It is supported by the fact that 12.50% of the patients in this study had a history of PID [Figure 1]. This data is not large enough to show the significance of PID in the generation of tubal blockage and supports the same point. A history of tuberculosis has been found in 37.50% of the patients, which is a significant data [Figure 1]. Most of the time, tuberculosis is missed by the consultant and is evaluated at the end. The data suggest that it must be given due importance and must not be missed. It also suggests that the health system in India has not yet come up to the mark to prevent the society from infective diseases like tuberculosis. Tuberculosis is still responsible for several health hazards in the Indian population. Infertility is no exception to this. A history of sexually transmitted diseases (STDs), which are considered very important etiological factors of infertility due to tubal blockage, has been found in only one patient (6.25%) [Figure 1]. It suggests that these diseases have become less prevalent in the population than previously. It is because of the increasing use of antibiotics. As an associated finding, the features of Artavakshaya, reported by Sushruta[12] as, Yathochita Kale Adarshanam, Alpata, and Yonivedana have been found in 68.75, 56.25, and 31.25% of the patients, respectively [Figure 2].There was no significant difference observed in the unilateral and bilateral tubal blockage; 62.50% patients had unilateral tubal blockage, while 37.50% patients had bilateral tubal blockage [Figure 3]. Enough authentic data are not available on the incidence of unilateral and bilateral tubal blockage. Hence, it is difficult to correlate the incidence of bilateral and unilateral tubal blockage obtained in the present study in this pattern. The most significant point that has emerged from this observation is cornual tubal blockage. It is the most prevalent, as it is 18.75% right cornual and 25% left cornual among all the patients [Figure 4]. Proximal tubal occlusion is mostly due to an inflammatory phenomenon, secondary to an ascending sexually transmitted disease, puerperal infection or septic abortion. It may also be associated with salpingitis isthmica nodusa, endometriosis, tubal polyposis or other rare causes of endosalpingitis.[13] The observations show that the factors related to cornual blocks have been found to be more in the study population, and hence, it is found to be more common.
Figure 2.
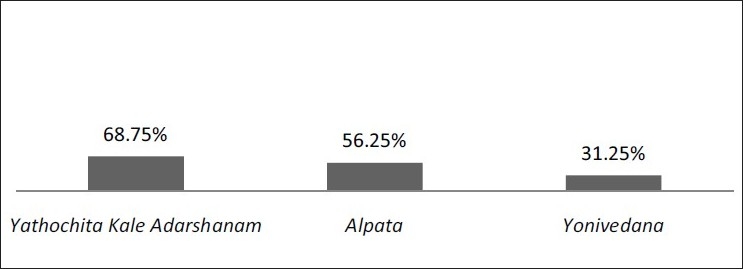
Number (%) of patients with Lakshana (features) of Artavakshaya (n = 16)
Figure 3.
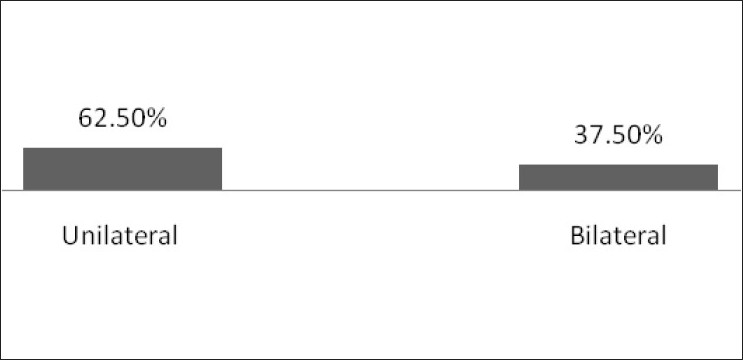
Findings of tubal blockage in patients by HSG (n = 16)
It seems to be a coincidence that the findings of bilateral (B/L) tubal blockage show a very symmetrical incidence of B/L cornual, B/L mid tubal, and B/L fimbrial tubal blockage. Although, the incidence of one side cornual and other side block on another site and vice versa are also possible. The 12.50% B/L cornual blockage, 18.75% B/L fimbrial blockage, and 6.25% patients of B/L mid tubal blockages are suggestive of a similar type of pattern in patients of B/L tubal blockage [Figure 4]. These data support the same fact that tubal blockage on any site other than the cornua or fimbria is the least common.[13]
Interpretation of observations during and after the procedure
The observations regarding various complaints after the procedure were supportive of the hypothesis that IUUB with the Ushna–Tikshna drug act on tubal blockage by removing the whole inner lining and by the mechanical effect of stimulating contractions of the uterus. Lower abdominal pain was found as a post-procedural complaint in 73.33% of the patients; 66.67% of the patients had pain within their tolerating capacity and 6.67% (one) patients beyond their tolerating capacity [Table 1]. A hot water bag was given as a post-procedure measurement to all the patients and it relieved the pain completely. One patient who was not able to tolerate the abdominal pain was managed with two Shankha Vati[14] tablets of 500 mg. In 60% of the patients, the duration of pain was less than one hour, whereas, in 13.33% of the patients, the duration of pain was more than one hour [Table 1]. Lower abdominal pain was not taken as a bad sign when it was within tolerating limit, because it denoted the contractile response of the uterus to remove the obstruction from the blockage site. Eighty percent of the patients complained of per vaginal bleeding as a post-procedure feature [Table 1]. The blood was dark colored and spotting in all patients. It denoted the endometrial scraping action of the Tikshna and Lekhana drugs administered through Uttar Basti, which was already hypothesized.
The most probable complications of Uttar Basti, are genitourinary infections and oil embolism. Good surveillance was carried out to diagnose any such complications as early as possible. However, the most encouraging point was that no feature of infection or oil embolism was observed during or after the procedure and even in the follow-up period. Proper antiseptic care, before and after the procedure does not allow any infection to grow. Uttar Basti carried out gently with a steady pace and confident skill prevents any complication like oil embolism. As it was a research study, it was mandatory not to give any drug other than the test drug to evaluate its exact role in tubal blockage. No modern antibiotics or any other Ayurvedic drugs were given. Yet patients did not show any sign of infection. It was because of the potent anti-inflammatory and anti-infective effect of various herbal drugs and Tila Taila. These results were encouraging and prove that there should not be any unnecessary fear toward Ayurvedic procedures because of modern influence.
Interpretation of the results obtained
After analyzing the complicated conditions of tubal infertility, more than 50% of the results to remove the blockage were considered as highly significant before study was started. The tubal block was removed in 80% of the patients [Table 2], as was evident by HSG [Figures 5–7]. These results were very encouraging for the Ayurvedic gynecologists as well as those who care for the infertile population. Moreover, 40% of the patients conceived within the follow-up period of two months after the treatment [Table 2].
On analyzing the effect of Uttar Basti on tubal blockage, highly significant results show the potency of the drugs used and also the efficacy of Uttar Basti. It is clear that its action on various disorders acts in both ways, local as well as systemic. In case of tubal blockage, this effect seems to be more local than systemic. The Tila Taila[15–17] is Vranashodhaka and Vranapachaka. It is Krimighna too. Other than that its specific role on the uterus and reproductive tract is also mentioned as Garbhashayashodhana and Yonishulaprashamana. All these properties indicate its antiseptic and anti-inflammatory effects. Its Vyavayi and Vikasi Guna show its potency to enter the minute channels and to spread easily. Thus, it is the best medium for any drug to reach the tubal cavity and remove the blockage. It is suggested that only the effect of Tila Taila Uttar Basti on tubal blockage must be studied to find out a cost-effective and easily available alternative. Kumari (Aloe vera)[18–20] is well-established for its anti-inflammatory, ulcer healing, and antibacterial properties. It is Tikshna and Vata-Kaphavardhaka by Karma. Thus, it removes the outer fibrosis of the endometrium and helps in its rejuvenation. Its anti-inflammatory action decreases the inflammation and its ulcer-healing property helps the inner lining of the tubes and uterus to heal. Another important content of Kumari Taila, Bhringaraja (Eclipta alba)[21] is a very potent Vata-Kapha Shamaka drug, which contains antiviral, antibacterial, antioxidant, and antihemorrhagic qualities. These properties make the medicine more potent in removing the chronic inflammation and fibrosis. Its Shothahara and Vishahara Karma reduce the swelling and edema of the tube and render it in a healthier atmosphere. Another major content of Kumari Taila and Dhatura (Datura metel)[22–24] is Krimighna, Vranahara, and Vishaghna. It is known for its anti-inflammatory property, and hence, it helps the inner lining of tubes to heal and rejuvenate. Thus, Kumari Taila helps in the scraping of the obstructing substance and also removes the endometrial lining of the tubes and uterus. It is supported by 73.33% of the patients, who complained of dark colored bleeding after Uttar Basti. It removes the fibrosed and damaged endometrium that leads to its rejuvenation. This description expresses the fact that the IUUB of Tila Taila with Vata-Kaphaghna and Lekhana properties scrape the inner lining of endometrium (Lekhana Karma). Thus, the inner fibrosed layer is removed. It rejuvenates later, as the endometrium has the capacity to regenerate, and the antioxidant and healing properties of various contents also help it for the same.
It is not only the patency of the tubal lumen that is needed for the treatment of tubal infertility. Restoration of the tubal functions is also another very important objective of the study. It can be achieved by pacifying the vitiation of Vata. The Snigdha Guna of the Taila is definitely helpful to relieve the abnormality generated by the Ruksha, Daruna, and Khara Guna of Vata. It restores the tonic phasic contractions of the tube and movement of the cilia. It is supported by the results of Uttar Basti, because totally 40% patients conceived, but no ectopic pregnancy was reported. Another supporting fact is that all these patients conceived within two months of the follow up-period; most of them in the very next cycle after treatment. Hence, IUUB with Vatashamaka drugs not only helps to get the patency of the tubal lumen, but also restores its normal physiological functions.
Analyzing the results and the available literature, the mode of action of Uttar Basti on tubal blockage can be summarized in the following points: (i) it removes the blockage of the tubal lumen by directly acting on the obstruction mechanically and restores the normal endometrium, as the endometrial covering exists on the inner side of the tubes also; its scraping and regenerating also leads to normalization of tubal functions, (ii) it restores the normal functions of the cilia by stimulating them, and (iii) it may break the tuboperitoneal adhesions, as it is observed with several studies that hysterosalpingography with an oil-based dye helps to break the adhesions.[25]
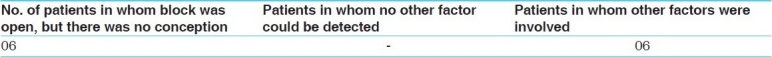
Logic behind some negative results
With regard to the negative results in which the tubal block could not be removed, which were found in a limited number of patients, an effort was made to analyze whether they all possessed a similar type of clinical picture or pathology. The number of such patients was three, two of them had a history of genital tuberculosis. Along with this, both the patients were suffering from anovulation. It showed the strong adverse effect of genital tuberculosis on infertility. Strong and highly effective antitubercular drugs, although they killed the mycobacterium, could not repair the damage caused by it on various organs. This fact is supported by the results of present study also. The IUUB gave more than 80% positive results, even then it could not remove the blockage in 20%[3] of the patients. Of those three patients, 66.67% had a history of genital tuberculosis [Table 3]. Hence, to obtain a peculiar conclusion regarding the significance of the therapy in cases with history of tuberculosis, some more research is definitely needed. It is suggested to carry out researches with no short-time limit, to evaluate the effect of Uttar Basti on tubal blockage and infertility with a history of genital tuberculosis. All the patients, who did not conceive within the follow-up period, after block removal, were having one or more factors of infertility other than tubal blockage [Table 4]. Hence, it was not possible to interpret the exact rate of conception as per the data obtained from the present study.
Table 3.
Patients in whom the block could not be removed
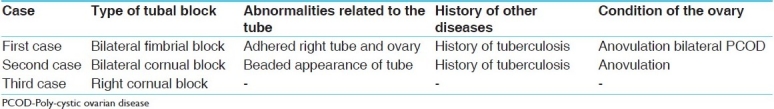
Table 4.
Evaluation of patients who did not conceive within the follow-up period after block removal
Interpretation of the associated results of therapy
Several contents of Kumari Taila are highly efficacious and established for their role on menstrual disorders and hormonal imbalance. For pacification of Vata too, Kumari Taila seems to be very efficient. Thus, it is hypothesized that it can not only remove tubal blockage, but it can also correct the ovarian functions, and hence, restore normal menstrual physiology in its entirety. This has been proved with the 40% conception and results of the Artavakshaya features. Eighty-two percent of the patients have had relief in features of Yathochita Kale Adarshanam (oligomenorrhea), 78% of the patients have shown relief in the symptoms of Alpartava (hypomenorrhea), and 80% of the patients have got relief from Yonivedana (dysmenorrhea) [Table 5]. These findings may be because of the Vata pacifying properties and hormonal regulatory functions of the drugs. Tila Taila, which is the medium of the drug, has already been stated to be very good for menstrual and gynecological problems. It is an encouraging, but unexpected, finding of the study, therefore, the statistical analysis of the results by various tests of significance may not be possible. However, it can be taken under consideration for future researches. Uttar Basti works on all three features of Artavakshaya through its local and systemic effects. It can be considered responsible for: (i) Uttar Basti with Ushna-Tikshna drugs help to remove fibrosis (due to the Khara and Daruna Guna of Vata) of the endometrium, and thus help in its rejuvenation, (ii) after stimulating the endometrial receptors, it stimulates the hypothalamus–pituitary–ovarian–uterine axis to restore the normal physiological neuroendocrine state, and (iii) after peritoneal spillage, it can also directly stimulate the dysfunctioning ovary with its potential drugs.
Conclusion
Intrauterine Uttar Basti of Kumari Taila is highly effective in removing the tubal blockage with an amazing rate of conception, as is evident by the results of the study. It may also be effective for other factors of female infertility and menstrual disorders, namely, oligomenorrhea, hypomenorrhea, and dysmenorrhea; due to its various contents having an effect on the ovarian and hormonal functions. No significant complication is evident in this study, with this procedure. After some further researches, IUUB can be established as an easily accessible, cost-effective Ayurvedic therapy for tubal blockage, with minimum adverse effects. With a long-term study, its effect on the tubal infertility in the patients with history of genital tuberculosis can also be evaluated. Although Uttar Basti is a nonsurgical procedure and the possibility of fibrosis after its completion, in due course of time, is the least, still further studies to evaluate the recurrence of tubal blockage are needed, to establish it as a reliable therapeutic measure.
References
- 1.Dutta DC. 5th ed. Calcutta: New Central Book Agency; 2009. Text Book of Gynaecology; p. 216. [Google Scholar]
- 2.Sharma H. Varanasi, Sutra: 2009. Vidyotni Hindi Commentary, Kashyapa Samhita, Chaukhamba Samskrita samsthana; pp. 30–1. [Google Scholar]
- 3.Shastry Ambikadutta. Varanasi, Sutra: 2006. Ayurveda-Tattva-Samdipika Vyakhya, Sushruta Samhita, Chaukhamba Samskrita Samsthana; pp. 17–12. [Google Scholar]
- 4.Srikantha Murthy KR. Vol. 2. Varanasi: Krishnadasa Academy; 2002. Bhavaprakasha of Bhavamishra; pp. 680–62/42-48. [Google Scholar]
- 5.70. Vol. 9. Varanasi, Chikitsa: Chaukhamba Bharati Academy; 2005. Kashinath Shastri and Gorakhnath Chaturvedi. Vidyotini Vyakhya, Charaka Samhita. [Google Scholar]
- 6.Srikantha Murthy KR. 73-81. Vol. 21. Varanasi, Chikitsa: Krishnadasa Academy; 2006. Vagbhata, Ashtanga Hridaya. [Google Scholar]
- 7.Himsagar Chandra Murty, Chaukhamba Surabharati series. Varanasi: Madhyama Khanda; 2007. Sharangdharacharya. Sharangadhara Samhita, Tra; pp. 40–9. [Google Scholar]
- 8.Harish Doshi. India: Arihant Publishers; 2007. Companion for Obstetrics and Gynaecology examinations; pp. 1–2. [Google Scholar]
- 9.Ibid, Companion for Obstetrics and Gynaecology examinations. :5. [Google Scholar]
- 10.Ibid, Companion for Obstetrics and Gynaecology examinations. :22–23. [Google Scholar]
- 11.2nd ed. London: Churchill Livingstone; 1993. Vaclav Insler and Bruno Lunenfeld. Infertility: Male and Female; p. 253. [Google Scholar]
- 12.Ibid, Ayurveda-Tattva-Samdipika Vyakhya, Sushruta Samhita, Su. Su. 15/12 [Google Scholar]
- 13.2nd ed. London: Churchill Livingstone; 1993. Vaclav Insler and Bruno Lunenfeld. Infertility: Male and Female; p. 254. [Google Scholar]
- 14.Bhaishajaya Ratnavali. Varansi: 2002. Ambikadatta Shastri, Chaukhamba Sanskrit Sansthana; pp. 182–3. [Google Scholar]
- 15.Ibid, Bhav Prakash Dhanya varga. :652. [Google Scholar]
- 16.Ministry of Health and Family Welfare, Department of ISM and H, Government of India. New Delhi: API; 1999. Anonymous. The Ayurvedic Pharmacopia of India; p. 4e. [Google Scholar]
- 17.Ibid, Sushruta Samhita,Sutra sthana, 45/112 [Google Scholar]
- 18.Ibid, Bhav Prakash Guduchyadi Varga, Shloka 230. :419. [Google Scholar]
- 19.C.C.R.A.S., Department of ISM and H, Ministry of Health and Family Welfare, Department of ISM and H, Government of India. Vol. 1. New Delhi: 2004. Anonymous. Database on Medicinal Plants in Ayurveda; p. 225. [Google Scholar]
- 20.Sabnis M. Varanasi: Chaukhamba Amarabharatin Prakashana; 2006. Chemistry and Pharmacology of Ayurvedic medicinal plants; p. 100. [Google Scholar]
- 21.Ibid, Database on Medicinal Plants in Ayurveda. 2e:112. [Google Scholar]
- 22.Ibid, Bhav Prakash Guduchyadi Varga, Shloka 85-87. :317. [Google Scholar]
- 23.Ibid, API. 3e [Google Scholar]
- 24.Ibid, Database in Medicinal Plants in Ayurveda. 2e:200. [Google Scholar]
- 25.Alper MM, Gareus PR, Spence JE, Quaringtom AM. Pregnancy rate after HSG in oil and water based contrast media. Obstet Gynael. 1986;68:6–9. [PubMed] [Google Scholar]


