Abstract
Objective
To estimate trends and risk factors for cesarean delivery for twins in the United States.
Methods
This was a cross-sectional study in which we calculated cesarean rates for twins from 1995 to 2008 using National Center for Health Statistics data. We compared cesarean rates by year and for vertex vs. breech presentation. The order of presentation for a given twin pair could not be determined from the available records and therefore analysis was based on individual discrete twin data. Multivariable logistic regression was used to estimate independent risk factors, including year of birth and maternal factors, for cesarean delivery.
Results
Cesarean rates for twin births increased steadily from 53.4% to 75.0% in 2008. Rates rose for the breech twin category (81.5% to 92.1%) and the vertex twin category (45.1% to 68.2%). The relative increase in cesarean rate for preterm and term infants was similar. After risk adjustment, there was an average increase noted in cesarean delivery of 5% each year during the study period (risk ratio 1.05, 95% confidence interval 1.04, 1.05).
Conclusions
Cesarean delivery rates for twin births increased dramatically from 1995 to 2008. This increase is significantly higher than that which could be explained by an increase in cesarean delivery for breech presentation of either the presenting or second twin.
Introduction
Cesarean delivery has increased in the United States over the past decade, with current rates approaching 1 in 3 deliveries occurring by cesarean section.(1) This increase has resulted in focused discussions surrounding current indications for cesarean delivery in hopes of curtailing this trend. Examples of these include the study of vaginal trial of labor after cesarean (TOLAC), elective inductions of labor prior to 39 weeks gestation, re-classification and management recommendations for intra-partum electronic fetal monitoring, and revisiting the efficacy of external cephalic version near term for fetuses in breech presentation.(2–10) Despite recent data, a clear rationale for the dramatic increase in cesarean delivery has not been identified, and whether this rise has resulted in improvements in maternal or neonatal outcomes remains unclear. In a study which aimed to identify potential reasons for the recent increase in primary cesarean rates, 16% of the rise was attributable to multiple gestation.(11) Because cesarean delivery can increase both short-term and long-term maternal morbidity, justifications for its routine use, such as potential neonatal benefit, are warranted.(12)
Recently, optimal mode of delivery has been a point of debate for twin gestations, particularly in regard to its impact on neonatal outcomes.(13–20) Though most providers feel comfortable delivering vertex-vertex twins vaginally, fewer are comfortable with breech delivery of the second twin in cases of vertex-non-vertex twins, despite data suggesting similar neonatal outcomes in experienced hands.(14, 21) Epidemiologic studies have shown a potential benefit of cesarean delivery when the second twin is non-vertex, and it has been suggested that this situation may be amenable to counseling patients of risk-benefit in a similar fashion as in singleton breech presentation or trial of vaginal delivery after cesarean.(22–24) Ultimately, there is not a clear evidence base for routine cesarean delivery for twin gestation.(25)
A previous report of U.S. twin births demonstrated a relatively high cesarean rate for twin gestation, which rose modestly from 50% to 56% from 1995 to 1998.(26) On the other hand, a decrease in cesarean for twins was seen in France from 50% in 2000–2001 to 36% in 2006.(27) The recent secular trend in cesarean delivery rates for twin gestations in the United States has not been characterized. The objective of our study was to estimate trends in cesarean delivery rates for twin births in the United States over the past two decades, and to estimate risk factors associated with cesarean delivery in twins during this time period.
Methods
A cross-sectional population study using the United States Birth Cohort datasets from 1995 to 2008, as collected by the National Center for Health Statistics from all 50 states and the District of Columbia was performed.
The publicly available U.S. Birth Certificate records during this study period note whether the gestation was singleton, twin, or higher order, but do not allow for matching of siblings. Therefore we considered each infant as a single unit of analysis. As twins are not matched, the order of presentation and the presentation of the corresponding twin is unavailable. The U.S. Birth Certificate is only recorded for live births, and therefore, twin gestations which ended with one twin in stillbirth would only have one twin reported in birth certificate data.
The primary outcome was mode of delivery, which was characterized as either vaginal or cesarean birth. The main predictor variable of interest was the year of birth. We also considered fetal presentation (defined as “vertex” or “breech” by the certificate data), fetal distress, cephalopelvic disproportion, preterm birth (<37 weeks gestation), small for gestational age (defined as < 10th percentile according to published norms),(28) prior cesarean delivery, induction of labor, and maternal factors including hypertensive disease and diabetes, as variables. For some states in earlier years of data collection, “breech” was also categorized as “breech / malpresentation.”
Cesarean delivery rates were calculated for all twin births, "vertex" and "breech" presentation by year of delivery, and by maternal and neonatal characteristics noted above. Univariable analysis using chi-square test and multivariable analysis using logistic regression were used to estimate independent risk factors for cesarean delivery. For each medical risk factor, we tested whether there was a significant change across the study period by including year as a linear variable in logistic regression in an analysis stratified by that risk factor. In order to test the difference in the trend between those that did or did not have a medical risk factor, the logistic model included the following predictor variables: the medical risk factor, year, and the interaction between the risk factor and year. Statistical significance was determined by p < 0.05. For 2007 and 2008, the variables noting fetal distress or cephalopelvic disproportion were no longer recorded on the standard birth certificate, and therefore, those two years were not included in the multivariable logistic regression analyses.
Risk factors were included in a multivariable logistic regression model with mode of delivery as an outcome, and odds ratios with 95% confidence intervals were estimated. This was completed for years 1995 to 2006 as a whole with year as a linear variable, then separately for each of 1995 and 2006. We converted odds to relative risk or risk ratio using the method outlined by Zhang.(29) As we could not directly adjust for the statistical effects of clustering within twin pairs, we performed a sensitivity analysis by inflating the standard errors in our analyses upwards by a factor of 1.41, a maximally conservative adjustment which assumes nearly perfect levels of intra-twin correlation.
This study was considered exempt from review by the University of California, San Francisco Committee on Human Research. All statistical analyses were completed using SAS 9.2 (SAS, Cary, NC).
Results
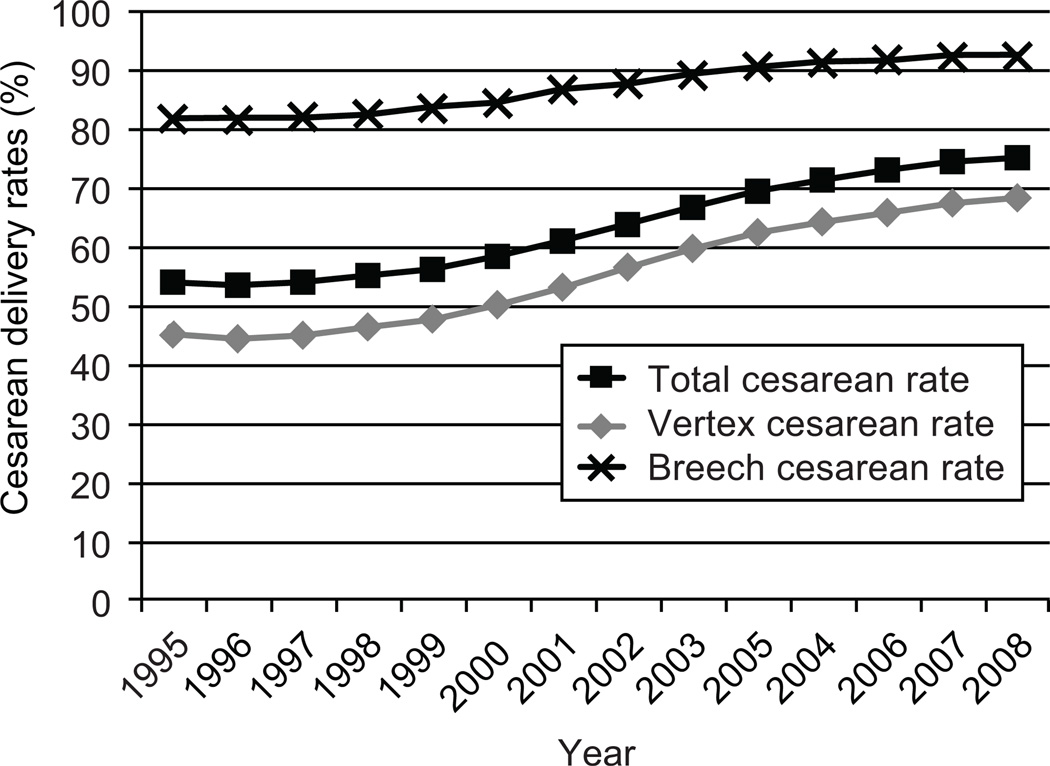
There were 1,702,365 twins born in the U.S. from 1995 to 2008 representing 3.0% of all live births. In this cohort, the proportion of records with unknown delivery mode was 9,034 (0.53%). Maternal demographic characteristics with group-specific cesarean delivery rates for twin births are shown in Table 1. The proportion of twins from multiple gestation pregnancies increased from 2.6% of all births in 1995 to a plateau of 3.4% from 2007 to 2008 (Table 2). Cesarean delivery rates were stable at 53.4–53.9% from 1995 to 1997, then increased steadily up to 75.0% in 2008 (Table 2 and Figure 1). Over the 14 year period, cesarean delivery for twins in the breech presentation increased from 81.5% to 92.1% and for those in the vertex presentation from 45.1% to 68.2% (Figure 1).
Table 1.
Maternal characteristics and mode of delivery for twins in the United States 1995 to 2008.
| Twin mode of delivery N (%) |
|||
|---|---|---|---|
| Maternal characteristic | N | Vaginal | Cesarean |
| Maternal age (years)* | |||
| < 20 | 98,995 | 40,510 (40.9%) | 58,485 (59.1%) |
| 20 – 24 | 310,314 | 122,733 (39.6%) | 187,581 (60.4%) |
| 25 – 29 | 441,233 | 166,689 (37.8%) | 274,544 (62.2%) |
| 30 – 34 | 484,390 | 170,182 (35.1%) | 314,208 (64.9%) |
| 35 – 39 | 282,853 | 90,054 (31.8%) | 192,799 (68.2%) |
| >= 40 | 74,858 | 18,023 (24.1%) | 56,835 (75.9%) |
| Race / Ethnicity | |||
| Non-Hispanic White | 1,080,519 | 395,831 (36.6%) | 684,688 (63.4%) |
| Black | 288,540 | 107,392 (37.2%) | 181,148 (62.8%) |
| Hispanic White | 241,398 | 77,674 (32.2%) | 163,724 (67.8%) |
| Asian | 69,336 | 22,262 (32.1%) | 47,074 (67.9%) |
| American Indian | 13,538 | 5,182 (38.3%) | 8,356 (61.7%) |
Maternal age missing for n = 688.
Table 2.
Cesarean delivery rates for vertex and breech presentation for twins in the United States 1995 to 2008.
| Year | N | % twins | % breech | % cesarean total |
|---|---|---|---|---|
| 1995 | 96,785 | 2.5 | 24.2 | 53.9 |
| 1996 | 100,815 | 2.6 | 24.6 | 53.4 |
| 1997 | 104,208 | 2.7 | 24.3 | 53.9 |
| 1998 | 110,743 | 2.8 | 24.2 | 55.0 |
| 1999 | 114,412 | 2.9 | 24.2 | 56.1 |
| 2000 | 119,008 | 2.9 | 24.2 | 58.3 |
| 2001 | 121,368 | 3.0 | 23.9 | 60.9 |
| 2002 | 125,246 | 3.1 | 23.6 | 63.7 |
| 2003 | 128,783 | 3.1 | 23.9 | 66.6 |
| 2004 | 132,356 | 3.2 | 24.7 | 69.3 |
| 2005 | 133,297 | 3.2 | 26.0 | 71.2 |
| 2006 | 137,239 | 3.2 | 27.0 | 72.9 |
| 2007 | 145,647 | 3.4 | 27.6 | 74.3 |
| 2008 | 145,175 | 3.4 | 27.8 | 75.0 |
Figure 1.
Cesarean delivery rates for twins, by presentation.
Cesarean rates increased 38.4% for twins born at term and increased 39.5% for twins born preterm (p < 0.0001 for both trends and for difference between groups). The largest relative increases in cesarean delivery occurred for twins with one or more of the following factors: no previous cesarean, vertex presentation, without fetal distress or cephalopelvic disproportion, and non-diabetic mother (Table 3). In sensitivity analysis where the maximum potential effect of clustering at the twin pair level was accounted for, all results remained statistically significant except for the yearly trend for infants with cephalopelvic disproportion.
Table 3.
Cesarean rates for twins in the United States 1995 to 2008 – by maternal and neonatal factors.
| Year | GA < 37 | GA >=37 |
Small for GA | Hypertension | Diabetes | Fetal distress | CPD | Previous C/S | Induction | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | ||||
| N | 971,438 | 708,505 | 561,550 | 1,118,393 | 170,096 | 1,523,235 | 76,556 | 1,616,775 | 40,947 | 1,374,889 | 8,074 | 1,407,762 | 221,889 | 1,470,372 | 199,586 | 1,493,745 | |
| Cesarean delivery rate (%) | 1995 | 54.7 | 52.9 | 52.7 | 54.5 | 63.7 | 52.9 | 61.7 | 53.6 | 74.8 | 53.1 | 95.4 | 53.5 | 89.5 | 48.9 | 26.3 | 57.4 |
| 1996 | 54.9 | 51.8 | 52.4 | 54.0 | 63.1 | 52.4 | 61.7 | 53.1 | 72.1 | 52.7 | 92.5 | 53.0 | 87.9 | 48.6 | 25.5 | 57.4 | |
| 1997 | 54.9 | 52.8 | 52.6 | 54.6 | 64.3 | 52.8 | 62.5 | 53.6 | 72.5 | 53.3 | 92.6 | 53.6 | 88.9 | 49.0 | 23.6 | 58.6 | |
| 1998 | 56.5 | 53.1 | 53.7 | 55.7 | 63.7 | 54.1 | 63.6 | 54.7 | 73.5 | 54.3 | 91.6 | 54.7 | 90.2 | 50.2 | 26.0 | 59.7 | |
| 1999 | 57.2 | 54.8 | 55.3 | 56.6 | 65.4 | 55.2 | 63.0 | 55.9 | 74.1 | 55.5 | 94.6 | 55.9 | 90.9 | 51.4 | 25.5 | 61.0 | |
| 2000 | 59.6 | 56.5 | 57.3 | 58.8 | 67.3 | 57.3 | 66.2 | 58.0 | 74.8 | 57.7 | 91.5 | 58.0 | 92.7 | 53.4 | 26.5 | 63.3 | |
| 2001 | 62.0 | 59.5 | 59.8 | 61.4 | 70.6 | 59.8 | 69.1 | 60.6 | 76.8 | 60.4 | 95.2 | 60.7 | 94.8 | 56.0 | 26.9 | 65.9 | |
| 2002 | 64.7 | 62.3 | 62.5 | 64.3 | 73.1 | 62.6 | 71.2 | 63.3 | 78.0 | 63.2 | 93.4 | 63.5 | 95.9 | 58.9 | 28.9 | 68.5 | |
| 2003 | 67.6 | 65.0 | 65.6 | 67.1 | 74.9 | 65.7 | 73.5 | 66.3 | 78.7 | 66.3 | 96.1 | 66.5 | 96.8 | 62.0 | 29.5 | 71.3 | |
| 2004 | 70.2 | 67.9 | 68.7 | 69.6 | 77.9 | 68.3 | 75.9 | 69.0 | 81.3 | 69.0 | 95.4 | 69.2 | 97.2 | 65.1 | 30.7 | 74.1 | |
| 2005 | 72.4 | 69.4 | 70.3 | 71.6 | 78.8 | 70.3 | 79.2 | 70.8 | 80.9 | 71.0 | 94.9 | 71.1 | 97.6 | 67.0 | 31.0 | 76.1 | |
| 2006 | 74.0 | 71.3 | 72.2 | 73.3 | 80.5 | 72.0 | 79.6 | 72.5 | 81.1 | 72.8 | 95.9 | 72.9 | 97.0 | 69.0 | 31.1 | 77.7 | |
| 2007 | 75.3 | 72.8 | 73.7 | 74.6 | 81.0 | 73.5 | 81.1 | 73.9 | 97.4 | 70.3 | 31.4 | 78.9 | |||||
| 2008 | 76.3 | 73.2 | 74.2 | 75.5 | 81.9 | 74.2 | 81.0 | 74.6 | 97.6 | 71.1 | 32.5 | 79.7 | |||||
After risk adjustment, we found that there was an average 5% increase in cesarean delivery rate during each year of the study period (risk ratio 1.05, 95% confidence interval 1.04, 1.05). In comparing the predictors for mode of delivery in twin gestations over the time interval, risk factors such as hypertension, diabetes, cephalopelvic disproportion, fetal distress, and previous cesarean delivery continued to increase the risk for cesarean delivery, but the magnitude of their overall impact decreased over time (Table 4). On the other hand when analyzing trends in the lowest risk group, those lacking any of the risk factors identified previously, the cesarean delivery rate rose from 33.6% in 1995 to 56.6% in 2006.
Table 4.
Risk factors for cesarean delivery for twins in the United States 1995 to 2008.
| Years included |
1995–2006 | 1995 | 2006 | |||
|---|---|---|---|---|---|---|
| Risk ratio | 95% CI | Risk ratio | 95% CI | Risk ratio | 95% CI | |
| Preterm birth (< 37 weeks) | 0.99 | (0.99, 0.99) | 1.01 | (1.00, 1.03) | 0.98 | (0.97, 0.99) |
| Small for gestational age | 1.00 | (0.99, 1.00) | 0.98 | (0.97, 1.00) | 1.00 | (0.99, 1.01) |
| Hypertension | 1.26 | (1.25, 1.26) | 1.31 | (1.29, 1.33) | 1.17 | (1.16, 1.18) |
| Diabetes | 1.08 | (1.07, 1.09) | 1.07 | (1.03, 1.11) | 1.08 | (1.07, 1.10) |
| Cephalopelvic disproportion | 1.58 | (1.58, 1.58) | 1.84 | (1.82, 1.85) | 1.36 | (1.34, 1.36) |
| Fetal distress | 1.36 | (1.36, 1.37) | 1.51 | (1.48, 1.53) | 1.20 | (1.18, 1.21) |
| Breech | 1.62 | (1.62, 1.62) | 1.85 | (1.83, 1.86) | 1.40 | (1.39, 1.40) |
| Previous cesarean | 1.65 | (1.65, 1.65) | 1.86 | (1.85, 1.87) | 1.41 | (1.40, 1.41) |
| Induction | 0.43 | (0.41, 0.43) | 0.45 | (0.44, 0.48) | 0.44 | (0.42, 0.44) |
| One year advance | 1.05 | (1.04, 1.05) |
Discussion
The Cesarean delivery rate for twin gestations in the United States had increased modestly in the years just prior to the current study period, from 50% to 53% over the years 1989 to 1994.(26) We found a substantially more dramatic and steady rise in cesarean delivery rates from 1995 to 2008. Cesarean rates for twins in breech presentation were already above 80% at the beginning of the study period and rose to greater than 90%. The relative increase in cesarean delivery for twins in vertex presentation was dramatically higher, increasing more than 50% from 45.1 to 68.2%.
We were unable to explain this increase in cesarean births for twins on the basis of higher rates of obstetric and medical complications necessitating operative delivery during the period analyzed. We found that the highest relative increases in cesarean rates occurred in what would usually be considered lower risk conditions, such as no fetal distress and no cephalopelvic disproportion (Table 3). After risk adjustment for factors such as hypertension, diabetes, and prematurity, there was a 5% increase in cesarean delivery each year.
When considering singletons in breech presentation, studies have tended to show a potential benefit for cesarean delivery, yet the American College of Obstetricians and Gynecologists allows for experienced practitioners to consider vaginal breech delivery in certain circumstances, while recognizing that cesarean delivery may be preferred in general.(24) It is possible that some of the increase in twin cesarean delivery may be attributable to what may be considered appropriate use of cesarean delivery for breech presentation of either the presenting or second twin.(15, 22, 23) We were not able to account for order of presentation in our study, and therefore could not refine our analysis to answer this specific question. As the proportion of twins in breech presentation remained relatively low, ranging from 23% to 28%, we suspect that the cesarean rate for twins in any combination of presentations, including vertex-vertex presentation, increased significantly during the study period. A study of U.S. twin births that were 34 weeks gestation and greater found that when the first twin presented in vertex position, 87% of second twins were also vertex, so that the vertex-vertex combination comprised the majority of presentations.(21)
Although birth certificate data does not characterize the order of presentation in twin gestations, we can estimate the approximate contribution of first twin breech presentation to what may be considered appropriate cesarean delivery of the second twin in vertex presentation. Knowing that approximately 75% of twins in the dataset are vertex, if we estimate that 20% of twin pregnancies have first twin breech,(16, 30) we would expect that < 10% of the vertex twins in this analysis would have been delivered by cesarean due to first twin being breech. We found that by 2008, 68.2% of vertex twins were delivered by cesarean. If we presumed that 10% of these were second twins following a first twin in breech position and that 100% of these were delivered by cesarean, the cesarean rate for vertex / vertex would still be 64.7%.
In prior studies of singletons and twins, induction of labor has been variably found to have positive, inverse, and no association with cesarean delivery, depending on the circumstances of induction and gestational age.(31–34) We found that induction of twin gestation pregnancies increased from 11.3% in 1995 to 13.8 % for 1998–1999, then steadily decreased to 9.7% to 9.9% in 2007 and 2008. The recent decline in inductions might indicate that some obstetricians were more inclined to proceed straight to cesarean delivery as opposed to a trial of labor in some circumstances. Although induction of labor was associated with significantly lower rates of cesarean than non-induced deliveries, there was still an increase in the rate of cesarean for induced deliveries from 26.3% to 32.5% during the study period.
We considered that the increasing trend in cesarean delivery overall could have contributed to the trend for twins, as women who had a previous cesarean delivery are more likely to undergo cesarean delivery for subsequent pregnancies. Indeed, previous cesarean was one of the strongest risk factors associated with cesarean delivery in this cohort of twin deliveries. However, this could only have been a partial contributor, as the large majority of deliveries occurred in mothers without a previous cesarean throughout the study period. Neonates born to mothers with a prior cesarean rose from 12.4% in 1995 to 14.9% in 2008.
Maternal morbidity associated with cesarean delivery, including peripartum infection and bleeding, is largely influenced by unplanned cesareans occurring during a trial of labor. It has been suggested that elective cesarean delivery for twins at 37 weeks could potentially reduce maternal morbidity by decreasing the need for unplanned cesareans.(20) Though overall planned cesarean deliveries have fewer adverse maternal effects than unplanned cesareans, planned cesareans still confer longer hospital stays, higher bleeding, and infection rates when compared with planned vaginal deliveries.(35, 36) Maternal morbidity data for planned cesarean delivery versus planned vaginal delivery in multiple gestations remains limited. In a French study, women undergoing vaginal delivery were more likely to have postpartum hemorrhage than planned cesarean deliveries, but composite morbidity was not different between groups.(16) Given their overall low frequency, larger studies are necessary in order to adequately study adverse maternal outcomes among women with multiple gestations. Regardless, cesarean delivery does increase abnormal placentation including placenta previa and accreta with future pregnancies. (35)
A limitation of our analysis was an inability to characterize cases in which the first twin delivered vaginally and the second by cesarean. Previous study of U.S. birth certificates has shown that this may occur up to 4–6% of the time.(19, 21) As those studies were performed on births during 1995 to 1997, we would presume that this occurrence would have decreased in frequency over time with the increase in cesarean delivery. Furthermore, for those cases in which there was an initial vaginal delivery followed by cesarean, our study would have counted this as one vaginal and one cesarean birth. For an analysis at the maternal level, this would count as one cesarean delivery, and therefore it is possible that our study would be an underestimate of cesarean rates. We also did not have data on births in which there may have been stillbirth of a co-twin. It is unclear how incorporation of this data would have impacted the results of this study. A further limitation of this analysis is that some conditions which were considered as “low risk” may have had other risk factors that were not listed or considered in our analysis.
The strength of our study is that this is not a sampling, but represents the entire United States population over a 14 year period. Although twins are a relatively small proportion of all births, the number of twin gestations increased 36% during the study period. The number of twin births in 2008 was 145,175, and 75% of those twins being delivered by cesarean would translate to more than 50,000 mothers having undergone cesarean delivery in that year.
As the cesarean rate for twin gestation continues to increase, it is possible that the skills required for vaginal delivery of multiples may be lost by clinicians. As it appears that cesarean delivery has now become the norm, an increasing number of clinicians may opt to avoid vaginal delivery for a variety of reasons, including medico-legal, as well as comfort level. Training and practice for vaginal delivery of singleton breech infants can occur with vaginal delivery of the second twin in breech position. Now this opportunity has become very rare, as less than 10% of breech twins are delivered vaginally.
There is a growing interest in stemming the rise in cesarean delivery rates for all pregnancies.(37, 38) In that context, we note that cesarean delivery for most twin gestations, especially those in vertex-vertex presentation, has no proven clinical benefit for either mother or child. The dramatic rise in cesarean delivery rates for twins undoubtedly has adverse implications for maternal morbidity and health care costs. Curtailing elective cesareans in this cohort may prove to be beneficial for both the individual mother and society at large.
Acknowledgments
Supported by NIH/NCRR/OD UCSF-CTSI Grant Number KL2 RR024130. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial Disclosure: The authors did not report any potential conflicts of interest.
REFERENCES
- 1.Menacker F, Hamilton BE. Recent trends in cesarean delivery in the United States. NCHS Data Brief. 2010 Mar;(35):1–8. [PubMed] [Google Scholar]
- 2.Aaronson D, Harlev A, Sheiner E, Levy A. Trial of labor after cesarean section in twin pregnancies: maternal and neonatal safety. J Matern Fetal Neona. 2010 Jun;23(6):550–554. doi: 10.3109/14767050903156700. [DOI] [PubMed] [Google Scholar]
- 3.Landon MB, Hauth JC, Leveno KJ, Spong CY, Leindecker S, Varner MW, et al. Maternal and perinatal outcomes associated with a trial of labor after prior cesarean delivery. N Engl J Med. 2004 Dec 16;351(25):2581–2589. doi: 10.1056/NEJMoa040405. [DOI] [PubMed] [Google Scholar]
- 4.Oshiro BT, Henry E, Wilson J, Branch DW, Varner MW. Decreasing elective deliveries before 39 weeks of gestation in an integrated health care system. Obstet Gynecol. 2009 Apr;113(4):804–811. doi: 10.1097/AOG.0b013e31819b5c8c. [DOI] [PubMed] [Google Scholar]
- 5.Macones GA, Hankins GD, Spong CY, Hauth J, Moore T. The 2008 National Institute of Child Health and Human Development workshop report on electronic fetal monitoring: update on definitions, interpretation, and research guidelines. Obstet Gynecol. 2008 Sep;112(3):661–666. doi: 10.1097/AOG.0b013e3181841395. [DOI] [PubMed] [Google Scholar]
- 6.Hutton EK, Hannah ME, Ross SJ, Delisle MF, Carson GD, Windrim R, et al. The Early External Cephalic Version (ECV) 2 Trial: an international multicentre randomised controlled trial of timing of ECV for breech pregnancies. BJOG. 2011 Apr;118(5):564–577. doi: 10.1111/j.1471-0528.2010.02837.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hutton EK, Hofmeyr GJ. External cephalic version for breech presentation before term. Cochrane Database Syst Rev. 2006;(1):CD000084. doi: 10.1002/14651858.CD000084.pub2. [DOI] [PubMed] [Google Scholar]
- 8.National Institutes of Health Consensus Development conference statement: vaginal birth after cesarean: new insights March 8–10, 2010. Obstet Gynecol. 2010 Jun;115(6):1279–1295. doi: 10.1097/AOG.0b013e3181e459e5. [DOI] [PubMed] [Google Scholar]
- 9.Grobman WA, Lai Y, Landon MB, Spong CY, Rouse DJ, Varner MW, et al. The change in the rate of vaginal birth after caesarean section. Paediatr Perinat Epidemiol. 2011 Jan;25(1):37–43. doi: 10.1111/j.1365-3016.2010.01169.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.ACOG Practice bulletin no. 115: Vaginal birth after previous cesarean delivery. Obstet Gynecol. 2010 Aug;116(2 Pt 1):450–463. doi: 10.1097/AOG.0b013e3181eeb251. [DOI] [PubMed] [Google Scholar]
- 11.Barber EL, Lundsberg LS, Belanger K, Pettker CM, Funai EF, Illuzzi JL. Indications contributing to the increasing cesarean delivery rate. Obstet Gynecol. 2011 Jul;118(1):29–38. doi: 10.1097/AOG.0b013e31821e5f65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Deneux-Tharaux C, Carmona E, Bouvier-Colle MH, Breart G. Postpartum maternal mortality and cesarean delivery. Obstet Gynecol. 2006 Sep;108(3 Pt 1):541–548. doi: 10.1097/01.AOG.0000233154.62729.24. [DOI] [PubMed] [Google Scholar]
- 13.D' Alton ME. Delivery of the second twin: revisiting the age-old dilemma. Obstet Gynecol. 2010 Feb;115(2 Pt 1):221–222. doi: 10.1097/AOG.0b013e3181cd3380. [DOI] [PubMed] [Google Scholar]
- 14.Fox NS, Silverstein M, Bender S, Klauser CK, Saltzman DH, Rebarber A. Active second-stage management in twin pregnancies undergoing planned vaginal delivery in a U.S. population. Obstet Gynecol. 2010 Feb;115(2 Pt 1):229–233. doi: 10.1097/AOG.0b013e3181c8b462. [DOI] [PubMed] [Google Scholar]
- 15.Hogle KL, Hutton EK, McBrien KA, Barrett JF, Hannah ME. Cesarean delivery for twins: a systematic review and meta-analysis. Am J Obstet Gynecol. 2003 Jan;188(1):220–227. doi: 10.1067/mob.2003.64. [DOI] [PubMed] [Google Scholar]
- 16.Schmitz T, Carnavalet Cde C, Azria E, Lopez E, Cabrol D, Goffinet F. Neonatal outcomes of twin pregnancy according to the planned mode of delivery. Obstet Gynecol. 2008 Mar;111(3):695–703. doi: 10.1097/AOG.0b013e318163c435. [DOI] [PubMed] [Google Scholar]
- 17.Smith GC, Shah I, White IR, Pell JP, Dobbie R. Mode of delivery and the risk of delivery-related perinatal death among twins at term: a retrospective cohort study of 8073 births. BJOG. 2005 Aug;112(8):1139–1144. doi: 10.1111/j.1471-0528.2005.00631.x. [DOI] [PubMed] [Google Scholar]
- 18.Herbst A, Kallen K. Influence of mode of delivery on neonatal mortality in the second twin, at and before term. BJOG. 2008 Nov;115(12):1512–1517. doi: 10.1111/j.1471-0528.2008.01899.x. [DOI] [PubMed] [Google Scholar]
- 19.Yang Q, Wen SW, Chen Y, Krewski D, Fung Kee Fung K, Walker M. Neonatal mortality and morbidity in vertex-vertex second twins according to mode of delivery and birth weight. J Perinatol. 2006 Jan 1;26(1):3–10. doi: 10.1038/sj.jp.7211408. [DOI] [PubMed] [Google Scholar]
- 20.Zipori Y, Smolkin T, Makhoul IR, Weissman A, Blazer S, Drugan A. Optimizing outcome of twins by routine cesarean section beyond 37 weeks. Am J Perinatol. 2011 Jan;28(1):51–56. doi: 10.1055/s-0030-1262511. [DOI] [PubMed] [Google Scholar]
- 21.Kontopoulos EV, Ananth CV, Smulian JC, Vintzileos AM. The impact of route of delivery and presentation on twin neonatal and infant mortality: a population-based study in the USA, 1995–97. J Matern Fetal Neona. 2004 Apr;15(4):219–224. doi: 10.1080/14767050410001668707. [DOI] [PubMed] [Google Scholar]
- 22.Yang Q, Wen SW, Chen Y, Krewski D, Fung Kee Fung K, Walker M. Neonatal death and morbidity in vertex-nonvertex second twins according to mode of delivery and birth weight. Am J Obstet Gynecol. 2005 Mar;192(3):840–847. doi: 10.1016/j.ajog.2004.09.132. [DOI] [PubMed] [Google Scholar]
- 23.Meyer MC. Translating data to dialogue: how to discuss mode of delivery with your patient with twins. Am J Obstet Gynecol. 2006 Oct;195(4):899–906. doi: 10.1016/j.ajog.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 24.ACOG Committee Opinion No. 340. Mode of term singleton breech delivery. Obstet Gynecol. 2006 Jul;108(1):235–237. doi: 10.1097/00006250-200607000-00058. [DOI] [PubMed] [Google Scholar]
- 25.Vayssiere C, Benoist G, Blondel B, Deruelle P, Favre R, Gallot D, et al. Twin pregnancies: guidelines for clinical practice from the French College of Gynaecologists and Obstetricians (CNGOF) Eur J Obstet Gynecol Reprod Biol. 2011 May;156(1):12–17. doi: 10.1016/j.ejogrb.2010.12.045. [DOI] [PubMed] [Google Scholar]
- 26.Ananth CV, Joseph Ks K, Smulian JC. Trends in twin neonatal mortality rates in the United States, 1989 through 1999: influence of birth registration and obstetric intervention. Am J Obstet Gynecol. 2004 May;190(5):1313–1321. doi: 10.1016/j.ajog.2003.11.029. [DOI] [PubMed] [Google Scholar]
- 27.Vendittelli F, Riviere O, Crenn-Hebert C, Riethmuller D, Schaal JP, Dreyfus M. Is a planned cesarean necessary in twin pregnancies? Acta Obstet Gynecol Scand. 2011 Mar 23; doi: 10.1111/j.1600-0412.2011.01130.x. [DOI] [PubMed] [Google Scholar]
- 28.Oken E, Kleinman KP, Rich-Edwards J, Gillman MW. A nearly continuous measure of birth weight for gestational age using a United States national reference. BMC Pediatr. 2003 Jul 8;3:6. doi: 10.1186/1471-2431-3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang J, Yu KF. What' s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. Jama. 1998 Nov 18;280(19):1690–1691. doi: 10.1001/jama.280.19.1690. [DOI] [PubMed] [Google Scholar]
- 30.Sibony O, Touitou S, Luton D, Oury JF, Blot P. Modes of delivery of first and second twins as a function of their presentation. Study of 614 consecutive patients from 1992 to 2000. Eur J Obstet Gynecol Reprod Biol. 2006 Jun 1;126(2):180–185. doi: 10.1016/j.ejogrb.2005.08.013. [DOI] [PubMed] [Google Scholar]
- 31.Rasmussen OB, Rasmussen S. Cesarean section after induction of labor compared to expectant management: No added risk from gestational week 39. Acta Obstet Gynecol Scand. 2011 May 4; doi: 10.1111/j.1600-0412.2011.01160.x. [DOI] [PubMed] [Google Scholar]
- 32.Osmundson S, Ou-Yang RJ, Grobman WA. Elective induction compared with expectant management in nulliparous women with an unfavorable cervix. Obstet Gynecol. 2011 Mar;117(3):583–587. doi: 10.1097/AOG.0b013e31820caf12. [DOI] [PubMed] [Google Scholar]
- 33.Yeast JD, Jones A, Poskin M. Induction of labor and the relationship to cesarean delivery: A review of 7001 consecutive inductions. Am J Obstet Gynecol. 1999 Mar;180(3 Pt 1):628–633. doi: 10.1016/s0002-9378(99)70265-6. [DOI] [PubMed] [Google Scholar]
- 34.Maslow AS, Sweeny AL. Elective induction of labor as a risk factor for cesarean delivery among low-risk women at term. Obstet Gynecol. 2000 Jun;95(6 Pt 1):917–922. doi: 10.1016/s0029-7844(00)00794-8. [DOI] [PubMed] [Google Scholar]
- 35.NIH State-of-the-Science Conference Statement on cesarean delivery on maternal request. NIH consensus and state-of-the-science statements. 2006 Mar 27–29;23(1):1–29. [PubMed]
- 36.Liu S, Liston RM, Joseph KS, Heaman M, Sauve R, Kramer MS. Maternal mortality and severe morbidity associated with low-risk planned cesarean delivery versus planned vaginal delivery at term. CMAJ : Canadian Medical Association journal = journal de l' Association medicale canadienne. 2007 Feb 13;176(4):455–460. doi: 10.1503/cmaj.060870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Caughey AB. Reducing primary cesarean delivery: can we prevent current and future morbidity and mortality? J Perinatol. 2009 Nov;29(11):717–718. doi: 10.1038/jp.2009.132. [DOI] [PubMed] [Google Scholar]
- 38.Chaillet N, Dumont A. Evidence-based strategies for reducing cesarean section rates: a meta-analysis. Birth. 2007 Mar;34(1):53–64. doi: 10.1111/j.1523-536X.2006.00146.x. [DOI] [PubMed] [Google Scholar]