Abstract
The objective of this study was to explore the association between psychosocial risk and protective factors and cannabis use disorders (CUDs) in a cohort of African American and Puerto Rican young adults. A representative sample (N=838) from the East Harlem area of New York City was assessed at four points in time (at mean ages 14.1, 19.2, 24.5, and 29.2). The psychosocial measures came from six domains: personality attributes, family, peer, work, neighborhood, and substance use The psychosocial measures were assessed at each of the first three waves of the study, and CUDs were assessed at the fourth and final wave of the study. Multivariate logistic regression and a cumulative risk analysis were conducted. Increased psychological symptoms (OR=1.21; 95% CI, 1.05–1.39; p<.01), problems resulting from cannabis use (OR=2.69; 95% CI, 1.33–5.46; p<.01), frequent arguments with one’s partner (OR=1.84; 95% CI, 1.09–3.10; p<.05), high levels of deviance (OR=1.81; 95% CI, 1.21–2.71; p<.01), and frequent acts of violence directed toward the participant (OR=1.19; 95% CI, 1.01–1.42; p<.05) were all associated with an increased risk for CUDs. An increase in the number of risks was associated with an increase in the probability of having CUDs at the fourth wave (again, at a mean age of 29.2). A decrease in the number of risk factors may lead to a decrease in CUDs.
Keywords: Cannabis use disorders, logistic regression analysis, cumulative risk index, risk analysis
INTRODUCTION
Cannabis abuse and dependence are related to indices of poor psychological well-being, such as symptoms of anxiety, depression, and psychosis (1–3). Frequent and/or long term cannabis use, as is typical of cannabis use disorders (CUDs), is associated with measures of impaired physical well-being, such as upper respiratory symptoms (4–5). Given the harmful effects of CUDs, there is a clear public health imperative to identify the factors leading and contributing to their development and persistence.
CUDs do not arise from a limited set of underlying causes (6), but out of a constellation of factors, across multiple domains. In particular, variables in the domains of personality attributes, family, peer, work, neighborhood, and substance use all contribute to cannabis abuse and dependence (6).
The prevalence of CUDs varies across demographic groups. In particular, males and younger adults (e.g., between the ages of 18 and 29) demonstrate higher rates of CUDs than females and older adults (7, 8). As regards personality attributes, several recent longitudinal studies have found that personality traits associated with a syndrome of undercontrol, including impulsivity, disinhibition, and aggression, are related to the subsequent development of CUDs (9–11). Additionally, both anxiety and depressive disorders (12, 13), as well as sub-clinical symptoms of anxiety and depression (14–16) are associated with an increased risk of CUDs. With regard to family factors, only one study to our knowledge has looked at the association between partner relationships and the use of marijuana. Maume and colleagues (17) found that low levels of marital attachment are related to the continuation of marijuana use. Investigators have found that associating with delinquent and drug-using peers in adolescence is significantly related to one’s own cannabis abuse and dependence in emerging adulthood at 20–22 years of age (9, 18, 19).
Several cross-sectional studies demonstrate that employment-related variables, such as greater absenteeism and lower occupational achievement, are related to the use of marijuana (20, 21). However, there are no longitudinal studies demonstrating that earlier measures of employment are related to later CUDs. Since the frequency of drug use predicts the development of CUDs (22), we postulate a relationship between work-related variables and the development of CUDs. Recent studies have shown that neighborhood disorganization and disadvantage, including violence and drugs sales, are related to the use of marijuana (23–26). Limited longitudinal research demonstrate that such neighborhood characteristics in adolescence predict the development of CUDs later in young adulthood (27).Finally, substance use is related to later CUDs. Smoking, drinking, and marijuana use represent risk factors for developing CUDs (22, 28).
According to Family Interactional Theory (FIT; 6),the cumulative number of risk factors is related to the development of psychopathology and CUDs. Based on FIT, we hypothesize that there is an increase in the probability of the occurrence of CUDs as the total number of risks the individual must cope with increases. In a related vein, Newcomb & Felix-Ortiz (29)reported that as the number of risks increased there was an associated increase in the probability of the occurrence of marijuana abuse.
The current study advances prior research in a number of ways: 1) we assess the predictors of CUDs among relatively understudied ethnic groups—namely, inner-city African Americans and Puerto Ricans (30–32); 2) we follow our sample up to the mean age of 29, in contrast to the majority of prior research using younger samples; 3) we examine the predictors of CUDs, while the bulk of existing research has been on the use of cannabis; 4) we identify the predictors of CUDs from several psychosocial domains; and, 5) we evaluate not only the individual effects of specific risk factors, but their cumulative effects.
In light of the above findings, we hypothesize the following: (1) Risk factors in each of the psychosocial domains predict CUDs. These risk factors include personal attributes (demographic and other personality factors), interpersonal (family, peer, and neighborhood factors), occupational, and those related to substance use; and (2) As the total number of risk factors increases, there will be a corresponding increase in the likelihood of CUDs..
METHODS
Participants
Data on the participants were initially collected in 1990 at Time 1 (T1) when the participants were attending schools in the East Harlem area of New York City. The questionnaires were completed in the classrooms with teachers not present. Each participant could choose to have a questionnaire in either English or Spanish. At Time 1, the mean age was 14.1 years with a standard deviation (S.D.) of 1.3 years. At Time 2 (T2; 1994–1996), the National Opinion Research Center located and interviewed the participants in person. The mean age of the participants was 19.2 years with a S.D. of 1.5 years. Interviewers of the same gender and ethnicity as the participants were used to the greatest extent possible. Participants could choose either an English or Spanish interview. At Time 3 (T3; 2000–2001), The Survey Research Center of The University of Michigan interviewed the participants. The mean age of the participants was 24.5 years with a S.D. of 1.4 years. As before, interviewers were matched to the participants’ gender and ethnicity as much as possible. The psychosocial risk factors were assessed at each of the first three waves (Times 1, 2, and 3).
There were 838 participants who participated at Time 4 (T4; 2004–2006). The mean age of the sample at T4 was 29.2 years, with a S.D. of 1.7 years. The sample was 41% male and 59% female. The sample was composed of 460 (54%) African American and 378 (46%) Puerto Rican respondents. The median educational level was having completed at least one year of business or technical school; 25% were employed in semi-skilled jobs (e.g., bus driver), 11% in skilled jobs (e.g., mechanic), 45% in clerical positions, 17% had professional level jobs, and 2% were unemployed at the time of the interview. In addition, 22% of the sample was married and living together at the time of the interview. Cannabis use disorders were assessed at the final wave (T4).
We compared the demographic variables for the participants who were interviewed at T1 (N=1332) and those who participated at T1 and T4, using the chi-square test of independence (33).Males, older people, Puerto Ricans, and those who had higher scores of socioeconomic status (SES) were more likely to drop out (χ2 = 29.77 , p<0.001; χ2 = 11.84 , p<0.001; χ2 = 6.54 , p<0.05; χ2 = 46.94 , p<0.001, respectively). We also compared both groups of participants on (a) problems caused by drugs at T1, and (b) the psychosocial risk factors at T1. In all cases, these two groups were not significantly different at a p value of .01.
The study procedures were in accordance with appropriate National Institute of Health (NIH) guidelines and were approved by the Institutional Review Board of the New York University School of Medicine. An NIH Certificate of Confidentiality was obtained for this data from the National Institute on Drug Abuse. Written informed consent was obtained from all participants. Additional information regarding the study methodology is available from previous reports (6).
Psychosocial Measures
The psychosocial scales used in this study are presented in Table 1. Some measures were administered at T1 and T3; others at T2 and T3, and some at only T3 (see Table 2). The scales have adequate reliabilities (Cronbach’s alphas). The measures have been found to predict substance use, dependence, and psychopathology (6, 43). The measures in Table 1 were grouped into the following domains: personality attributes, family, peer, work, neighborhood, and substance use. CUDs as defined in DSM IV included cannabis dependence or cannabis abuse (44). The assessment of CUDs was made using an adaptation of the UMCIDI (45).
Table 1.
Psychological Measures: Sources and Cronbach’s Alphas
| Domain/Scale (no. of items) | Cronbach’s Alpha | Source | Sample Items |
|---|---|---|---|
| Demographics | |||
| Gender | NA | ||
| Age | NA | Age at Time 4 | |
| Ethnicity | NA | Are you Hispanic? | |
| Socioeconomic status (5) | NA | Combination of educational level and job status of parents | |
| Personality Attributes | |||
| Ego integration (6) | .53 | Original | Do you feel like losing your tempter at people? |
| Violence toward others (10) | .84 | Chavez, Oetting, & Swaim, 1994 (34) | How often have you held a weapon (gun or club) to someone? |
| Psychological symptoms (17) | .89 | Derogatis & Melisaratos, 1983 (35) | Do you sometimes feel hopeless about the future? |
| Impulsivity (4) | .64 | Brook et al., 1990 (6) Jackson, 1974 (36) |
Do you often act on the spur of the moment without stopping to think? |
| Partner Relationships | |||
| Satisfaction with partner (9) | .73 | Spanier, 1976 (37) | All things considered, how satisfied are you with your marriage/relationship |
| Marital harmony (7) | .91 | Spanier, 1976 (37) | Do you act very affectionately with each other? |
| Arguments with partner (5) | .81 | Original | How often do the two of you argue or fight about things? |
| Peers | |||
| Deviance (6) | .76 | Huizinga, Menard & Elliott, 1989 (38) | How many of your friends have gotten in trouble with the police or the law for something they did? |
| Illegal drug use (4) | NA | Original | How many friends have ever used cannabis, or other illegal drugs, like cocaine, crack, heroin, uppers, and downers? |
| Association with drug using peers (8) | .74 | Oetting & Beauvais, 1987 (39) | How much have close friends influenced your use of illegal drugs? |
| Work | |||
| Skipped work (2) | .77 | Original | How often have you called in sick when you were not sick? |
| Work achievement (1) | NA | Original | At your most recent job, how often have you received good evaluations from your boss? |
| Neighborhood | |||
| Drug offering (1) | NA | Original | How often has someone on the street offered you cannabis or any other illegal drug? |
| Violence toward subject (10) | .79 | Chavez, Oetting, & Swaim, 1994 (34) | How often has someone held a weapon (gun, club or knife) to you? |
| Drug availability (8) | .79 | Monitoring the Future Questionnaire 2002, Form 40 Part F (40) | How difficult is it to get cannabis, cocaine, crack, or other illegal drugs like uppers, downers, LSD or Heroin? |
| Substance Use | |||
| Nicotine dependence (6) | .94 | Heatherton, Kozlowski, Frecker & Fagerstrom, 1991 (41) | How many cigarettes have you smoked in the past 30 days? |
| Alcohol use (8) | .96 | Monitoring the Future Questionnaire 1994, Form 3 Part D (42) | During the last 5 years, has your use of alcohol caused you to behave in ways that you later regretted? |
| Problems with cannabis use (9) | .98 | Monitoring the Future Questionnaire 1994, Form 3 Part D (42) | During the last 5 years, has your use of cannabis damaged your social life, popularity, or reputation? |
Note: 1. The alphas are estimated from our data.
2. N/A = Not Applicable
Table 2.
Predictors of Cannabis Use Disorders (CUDs) at T4 (Mean Age 29.2): Odds Ratios (OR) and 95% Confidence Intervals (CI)
| Predictors | Cannabis Use Disorders |
||||
|---|---|---|---|---|---|
| Bivariate | Multivariate | Time Points for Measured Predictors | |||
| OR | CI | OR | CI | ||
| Demographics | |||||
| Gender R (Male) | 3.88** | 2.00 – 7.54 | |||
| Age at T4 R (Older) | 0.60*** | 0.41 – 0.87 | |||
| Ethnicity (1: AA, 2: PR) | 0.89 | 0.45 – 1.78 | |||
| Socioeconomic status at T2 | 1.02 | 0.90 – 1.16 | |||
| Personality Attributes | |||||
| Ego integration (High) | 0.70*** | 0.62 – 0.79 | 0.79 | 0.61 – 1.02 | 1, 3 |
| Violence toward others R (High) | 1.37*** | 1.25 – 1.50 | 1.19* | 1.02 – 1.39 | 2, 3 |
| Psychological symptoms R (High) | 1.15*** | 1.09 – 1.21 | 1.21** | 1.05 – 1.39 | 1, 3 |
| Impulsivity (High) | 1.47*** | 1.24 – 1.74 | 1.02 | 0.65 – 1.60 | 3 |
| Partner Relationships | |||||
| Satisfaction with partner (High) | 0.75*** | 0.63 – 0.88 | 1.23 | 0.67 – 2.26 | 2, 3 |
| Marital harmony (High) | 0.76** | 0.64 – 0.90 | 0.84 | 0.51 – 1.37 | 3 |
| Arguments with partner R (High) | 1.40*** | 1.18 – 1.66 | 1.84* | 1.09 – 3.10 | 3 |
| Peers | |||||
| Deviance R (High) | 1.63*** | 1.46 – 1.82 | 1.81** | 1.21 – 2.71 | 1, 3 |
| Illegal drug use (High) | 1.46*** | 1.30 – 1.65 | 0.73 | 0.48 – 1.13 | 1, 3 |
| Association with drug using peers R (High) | 1.60*** | 1.42 – 1.81 | 1.45* | 1.07 – 1.96 | 2, 3 |
| Work | |||||
| Skipped work R (Frequent) | 1.55*** | 1.31 – 1.85 | 1.55* | 1.10 – 2.19 | 3 |
| Work achievement (High) | 0.82* | 0.69 – 0.98 | 0.91 | 0.55 – 1.51 | 3 |
| Neighborhood | |||||
| Drug offering (High) | 1.20*** | 1.08 – 1.33 | 1.05 | 0.86 – 1.29 | 1, 3 |
| Violence toward subject R (High) | 1.33*** | 1.22 – 1.46 | 1.19* | 1.01 – 1.42 | 2, 3 |
| Drug availability (High) | 1.23** | 1.09 – 1.38 | 1.09 | 0.86 – 1.38 | 1, 3 |
| Substance use | |||||
| Nicotine dependence (High) | 1.57*** | 1.34 – 1.82 | 1.25 | 0.85 – 1.86 | 3 |
| Alcohol use (High) | 2.74*** | 2.04 – 3.69 | 1.11 | 0.52 – 2.40 | 3 |
| Problems with cannabis use R (High) | 5.12*** | 3.84 – 6.84 | 2.69** | 1.33 – 5.46 | 3 |
p<.05,
p<.01,
p<.001.
Note: 1. Each multivariate logistic regression analysis is controlled by the demographic variables and the remaining variables within the domain.
2. The last column represents the time points when the data were collected.
3. “R”-Scale is used in risk analysis.
4. AA = African American, PR = Puerto Rican
Analytic Plan
We used the full information maximum likelihood (FIML) method to impute missing data (46). The advantage of FIML is that the results are less likely to be biased even if the data are not missing completely at random.47 Only scores on the predictor variables were imputed, not scores on the outcome measure of CUDs. SAS was used to compute the proposed statistics. The dependent variable in all logistic regression analyses was whether a participant had CUDs at T 4. In the bivariate analyses, each of the independent variables in Table 2 was used to predict CUDs.
We computed six separate multiple logistic regression analyses using variables from the six domains (i.e. personality, family, peer, work, neighborhood, and substance use). In each multiple logistic regression analysis, the independent variables were the demographic variables (gender, age, ethnicity, and SES) and the variables in that particular domain. In Table 2, we report the multivariate odds ratio for each variable in a domain controlling for the demographic variables and the other variables in the domain. For each variable in the psychosocial domains, we summed the measures at the time points listed in the far right column (see Table 2) and standardized each. One limitation of this approach is that one runs the risk of grouping together participants who have demonstrated disparate prospective patterns of psychosocial risk. For instance, a participant who reported high levels of psychological symptoms at T1 (at a mean age of 14.1), but low levels at T3 (at a mean age of 24.5), would be grouped together with a participant who reported low levels of psychological symptoms at T1, but high levels at T3. Treating both such participants as equivalent may be suboptimal, in that they may be at different levels of risk for CUDs at T4 (at age 29.2). However, scores on each of our predictor variables were highly correlated across different waves of the study, indicating that, in practice, there was considerable stability in levels of each risk factor over time.
We defined ten risk indicators for a CUD. The gender risk variable was 1 for males and 0 for females. The age risk indicator was 1 if the participant’s age was in the lowest 16th percentile and zero otherwise. At T4, participants in the lowest 16th percentile were 26 or 27 years of age. The rest of the sample ranged from ages 28 to 35. We treated younger age as a risk factor because the prevalence of marijuana use declines throughout the age range of our sample (48), and, therefore, younger participants would be at greater risk. Thus, the younger participants were considered at risk. The eight psychosocial risk variables were indicated by a superscript “R” in the far left column of Table 2. To be consistent with our prior work, a risk score of 1 is assigned when the participant’s score is in the 84th percentile or higher on the summed and standardized variable. Furthermore, receiving a risk score in the 84th percentile or above does predict drug use, violent behaviors and psychopathology. The cumulative risk index is the sum of the 10 risk indicators for CUDs. A bivariate logistic regression analysis was computed to examine the relation of the cumulative risk index and CUDs at T 4.
Results
Logistic Regression Analyses
Table 3 presents the proportions of respondents with CUDs at T4 (at mean age 29.2), as well as the proportions of participants who reported problems resulting from cannabis use (or the closest available measure) at the other waves. The proportion of respondents we identified who had CUDs at this age is slightly higher than that found in representative national samples.8 Table 2 presents the results of the bivariate and multivariate logistic regression analyses. In the bivariate logistic regression analysis, each of the variables in each domain was significant. Among the demographic variables, male gender (OR, 3.88; 95% CI, 2.00 – 7.54; p< .01) and younger age (OR, .60; 95% CI, .41 – .87; p< .001) were associated with an increased risk for having T4 CUDs.
Table 3.
Proportion of Respondents with CUDs at T4 (Mean Age 29.2), and Problems with Cannabis Use at Earlier Waves
| Female | Male | |||
|---|---|---|---|---|
| AA | PR | AA | PR | |
| T1: Problems with drug use1 | .75 | .32 | .35 | 1.62 |
| T2: Problems with cannabis use | 5.30 | 11.16 | 17.28 | 21.47 |
| T3: Problems with cannabis use | 11.54 | 13.82 | 26.71 | 31.54 |
| T4: Problems with cannabis use | 8.83 | 22.60 | 7.91 | 14.81 |
Note: AA = African American, PR = Puerto Rican
Closest measure available to problems with marijuana use at this wave.
In the multivariate logistic regression analyses, eight of the standardized psychosocial variables were significant. In the personality domain, more frequent violence directed toward others (OR, 1.19; 95% CI, 1.02 – 1.39; p< .05) and increased psychological symptoms (OR, 1.21; 95% CI, 1.05 – 1.39; p< .01) were associated with an increased risk of having CUDs at T4. In the family domain, more frequent arguments with one’s partner were associated with an increased risk for having CUDs at T4 (OR, 1.84; 95% CI, 1.09 – 3.10; p< .05). In the peer domain, number of friends who are deviant (OR, 1.81; 95% CI, 1.21 – 2.71; p< .01) and susceptibility to peer drug use (OR, 1.45; 95% CI, 1.07 – 1.96; p< .05) were associated with an increased risk for having CUDs at T4. In the work domain, skipping work more often was associated with an increased risk for having CUDs at T4 (OR, 1.55; 95% CI, 1.10 – 2.19; p< .05). In the neighborhood domain, more frequent violence directed toward the participant was associated with an increased risk of having CUDs at T4 (OR, 1.19; 95% CI, 1.01 – 1.42; p< .05). Cannabis use was associated with an increased risk for having CUDs at T4 (OR, 2.69; 95% CI, 1.33 – 5.46; p< .01).
Cumulative Risk Analysis
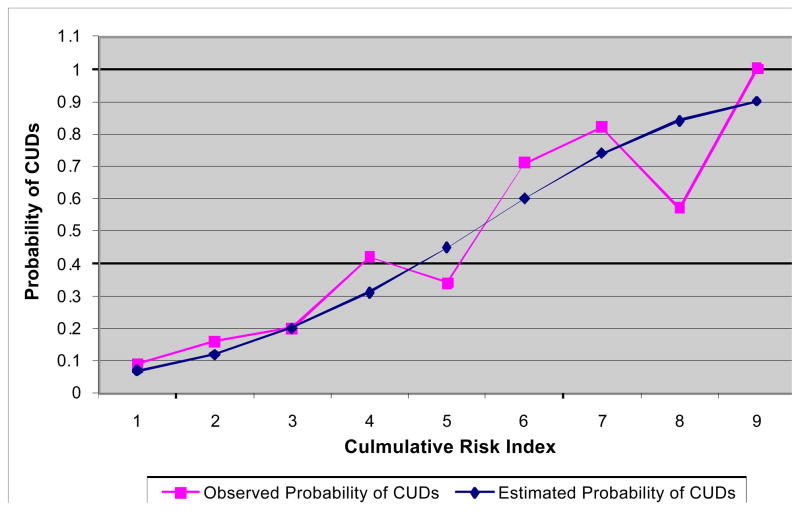
Figure 1 plots the estimated probability of CUDs at T4 against the cumulative risk index, as well as the observed probability of CUDs at each level of risk. An increase in the number of risks is associated with an increase in the estimated probability of having CUDs at T4. The estimated probabilities are well within the confidence interval of the observed probabilities. (Data available upon request.) In performing the analysis, two risks served as the baseline. We estimated the probability of having CUDs at T4 for every additional risk factor beyond the baseline. For example, having four risk factors were associated with a factor of 2.6 increase in the probability of having CUDs at T4 (i.e., 0.31 probability for four risks versus 0.12 for two risks), having five risks with a factor of 3.8 increase, and having six risks with a factor of 5 increase.
Figure 1.
Probability of Having CUDs as a Function of the Number of Risk Factors
Note 1. Cumulative Risk Index refers to the sum of the 10 risk indicators for CUDs. 2. The vertical bars represent 99.9% confidence intervals for observed probability.
DISCUSSION
As hypothesized, our results demonstrate that many earlier variables, assessed over three waves spanning the mean ages of 14.1 to 24.5, are significantly related to CUDs at T4, at a mean age of 29.2. The domains include: personality attributes, family, peer, occupational difficulties, neighborhood, and substance use assessed during the periods of early adolescence, middle and late adolescence, and early adulthood. In addition, an increase in the number of risk factors is approximately linearly associated with an increase in the probability of CUDs at T4.
Our findings are unique in three ways. First, the analysis reports results from a 15-year longitudinal study of CUDs at T4, beginning when the participants were in adolescence and continuing into adulthood. Second, this is the first study of the predictors of CUDs assessed in African Americans and Puerto Ricans. Third, we investigate the relationship between the cumulative risk of significant psychosocial factors and CUDs at T4.
Violence directed by participants toward others or violence directed toward the participants is of great importance in predicting CUDs at T4, when the participants were at a mean age of 29.2 years. This is manifested in the personality domain (e.g., violence towards others), the family domain (e.g., in partner arguments), violence in the peer group (e.g., friends in trouble with the police), and violence in the neighborhood (e.g., violence directed toward the participant).
With respect to psychological symptoms, individuals who are depressed and anxious are more likely to have CUDs at T4. These findings are in accord with the self-medication theory of substance abuse as expressed by Khantzian (49), which states that cannabis may be used to cope with depression and anxiety.
Two mechanisms may explain the relationship between peer drug associations and CUDs at T4. Some individuals may select friends who use drugs. Alternatively, such individuals may imitate the drug use of their friends (18, 50). Moreover, it is possible that both mechanisms are operative.
According to Problem Behavior Theory (51), low achievement and marijuana use are related components of a more inclusive syndrome of problem behavior. Individuals who are low achievers are more likely to be absent from work and have CUDs.
Adolescents who experience a greater number of problems resulting from cannabis use are more likely to develop CUDs in adulthood. The multivariate odds ratio of 2.69 indicates that there is a strong association between problems resulting from cannabis use in adolescence and CUDs in adulthood. These findings are in accord with the results of Winters & Lee (52). From a public health preventive perspective, although CUDs develops over a long period of time, cannabis use in the early 20’s should be considered a potential risk factor.
Our findings indicate that older adults are less likely to have a diagnosis of CUDs than younger adults. These findings are in accord with Bachman et al. (53), who reported that older adults are less likely to use drugs as a result of a more conventional life style. The results of this study suggest that male adults are almost four times as likely to have a diagnosis of CUDs as females. These findings are in line with those of Stinson, Ruan, Pickering, and Grant (54), who have reported gender differences in the prevalence of CUDs.
The results of this investigation indicate that CUDs are also predicted by the cumulative number of psychosocial and demographic risks. These results are in accord with FIT (6), which postulates that an increase in the total number of psychosocial risks with which an individual must cope is associated with a corresponding increase in substance use in adolescents and young adults. Moreover, our research extends the conclusions of Castro, Brook, Brook, and Rubenstone (55), as well as Bry, McKeon, and Pandina (56), who note that assessing risks that are relatively uncorrelated from diverse areas of the lives of adolescents and young adults over time increases the accuracy of the prediction of drug use/abuse/dependence. In a related vein, multiple-risk models have also been used effectively to explain psychiatric disorders (57).
Limitations
Our results suggest that a multiple-risk model is effective in predicting CUDs. Adding other psychosocial dimensions as well as genetic factors would likely increase the accuracy of the prediction of CUDs.
Our data are based on self-reports rather than on external measurements from official records, such as police records. Studies have shown that use of this type of self-report data yields reliable results (58). However, wherever possible, for each variable we combined measures from multiple time points; this enhanced the reliability and validity of these measures.
Lastly, our risk model was only tested on a minority sample of African Americans and Puerto Ricans. Future work is need to test whether our model predicts CUDs in other populations as well.
Despite these limitations, the study supports and extends the literature in a number of ways. First, we assess variables over a span of up to 15 years. The prospective nature of the data allowed us to go beyond a cross-sectional analysis and to consider the temporal sequencing of variables. A major contribution of the paper is a set of findings relating earlier manifestations of violence in adolescence to the occurrence of adult CUDs.
From a clinical perspective, it would be important to reduce the number of risk factors in order to reduce the probability of having CUDs. This extends the research of Kliewer and Murrelle (58), who found that an increase in the number of risk factors an individual is exposed to was related to an increase in the probability of having problems resulting from marijuana use. Finally, prevention or treatment interventions should be directed toward both internal psychological distress and aggression. One might also focus on decreasing violence whether rooted in the person, the family, in the peer group, or in the neighborhood.
Acknowledgments
This research was supported by grant DA005702 from the National Institute on Drug Abuse, and Senior Scientist Award DA00244 from the National Institute on Drug Abuse, both awarded to Dr. Judith S. Brook.
References
- 1.Budney AJ, Moore BA. Development and consequences of cannabis dependence. J Clin Pharmacol. 2002;42:1S–6S. doi: 10.1002/j.1552-4604.2002.tb06000.x. [DOI] [PubMed] [Google Scholar]
- 2.Copeland J, Swift W, Rees V. Clinical profile of participants in a brief intervention program for cannabis use disorder. J Subst Abuse Treat. 2001;20:45–52. doi: 10.1016/s0740-5472(00)00148-3. [DOI] [PubMed] [Google Scholar]
- 3.Hall WD. Cannabis use and the mental health of young people. Australian & New Zealand Journal of Psychiatry. 2006;40:105–113. doi: 10.1080/j.1440-1614.2006.01756.x. [DOI] [PubMed] [Google Scholar]
- 4.Reilly D, Didcott P, Swift W, Hall W. Long-term cannabis use: characteristics of users in an Australian rural area. Addiction. 1998;93:837–846. doi: 10.1046/j.1360-0443.1998.9368375.x. [DOI] [PubMed] [Google Scholar]
- 5.Tetrault JM, Crother K, Moore BA, Mehra R, Concato J, Fiellin DA. Effects of marijuana smoking on pulmonary function and respiratory complications. A systematic review. Arch Intern Med. 2007;167:221–228. doi: 10.1001/archinte.167.3.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brook JS, Brook DW, Gordon AS, Whiteman M, Cohen P. The psychosocial etiology of adolescent drug use: a family interactional approach. Genet Soc Gen Psychol Monogr. 1990;116:111–267. [PubMed] [Google Scholar]
- 7.Coffey C, Carlin JB, Degenhardt L, Lynskey M, Sanci L, Patton GC. Cannabis dependence in young adults: an Australian population study. Addiction. 2002;97:187–194. doi: 10.1046/j.1360-0443.2002.00029.x. [DOI] [PubMed] [Google Scholar]
- 8.Compton WM, Grant BF, Colliver JD, Glantz MD, Stinson FS. Prevalence of marijuana use disorders in the United States: 1991–1992 and 2001–2002. JAMA. 2004;17:2114–2121. doi: 10.1001/jama.291.17.2114. [DOI] [PubMed] [Google Scholar]
- 9.Feske U, Tarter RE, Kirisci L, Gao Z, Reynolds M, Vanyukov M. Peer environment mediates parental history and individual risk in the etiology of cannabis use disorder in boys: a 10-year prospective study. Am J Drug Alcohol Abuse. 2008;34:307–320. doi: 10.1080/00952990802013631. [DOI] [PubMed] [Google Scholar]
- 10.Tarter RE, Kirisci L, Ridenour T, Vanyukov M. Prediction of cannabis use disorder between childhood and young adulthood using the child behavior checklist. J Psychopathol Behav Assess. 2008;30:272–278. [Google Scholar]
- 11.Hayatbakhsh MR, McGee TR, Bor W, Najman JM, Jamrozik K, Mamun AA. Child and adolescent externalizing behavior and cannabis use disorders in early adulthood: an Australian prospective birth cohort study. Addict Behav. 2008;33:422–438. doi: 10.1016/j.addbeh.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 12.Buckner JD, Schmidt NB, Lang AR, Small JW, Schlauch RC, Lewinsohn PM. Specificity of social anxiety disorder as a risk factor for alcohol and cannabis dependence. J Psychiatr Res. 2008;42:230–239. doi: 10.1016/j.jpsychires.2007.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wittchen HC, Fröhlich C, Behrendt S, Günther A, Rehm J, Zimmermann P, Lieb R, Perkonigg A. Cannabis use and cannabis use disorders and their relationship to mental disorders: a 10-year prospective-longitudinal community study in adolescents. Drug Alcohol Depend. 2007;88:S60–S70. doi: 10.1016/j.drugalcdep.2006.12.013. [DOI] [PubMed] [Google Scholar]
- 14.Buckner JD, Schmidt NB, Bobadilla L, Taylor J. Social anxiety and problematic cannabis use: evaluating the moderating role of stress reactivity and perceived coping. Behav Res Ther. 2006;44:1007–1015. doi: 10.1016/j.brat.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 15.Guy D, Panichelli-Mindel SM, Shera D, Dennis M, Tims F, Ungemack J. Psychiatric symptoms in adolescents with marijuana abuse and dependency in outpatient treatment. J Child Adolesc Subst Abuse. 2006;15:37–54. [Google Scholar]
- 16.Rowe CL, Liddle HA, Dakof GA. Classifying clinically referred adolescent substance abusers by level of externalizing and internalizing symptoms. J Child Adolesc Subst Abuse. 2001;11:41–65. [Google Scholar]
- 17.Maume MO, Ousey GC, Beaver K. Cutting the grass: a reexamination of the link between marital attachment, delinquent peers, and desistance from marijuana. Journal of Quantitative Criminology. 2005;21:27–53. [Google Scholar]
- 18.Fergusson DM, Swain-Campbell NR, Horwood LJ. Deviant peer affiliations, crime and substance use: a fixed effects regression analysis. J Abnorm Child Psychol. 2002;30:419–432. doi: 10.1023/a:1015774125952. [DOI] [PubMed] [Google Scholar]
- 19.Gil AG, Vega WA, Turner RJ. Early and mid-adolescence risk factors for later substance abuse by African Americans and European Americans. Public Health Rep. 2002;117:S15–S29. [PMC free article] [PubMed] [Google Scholar]
- 20.Brook JS, Adams RE, Balka EB, Johnson E. Early adolescent marijuana use: risks for the transition to young adulthood. Psychol Med. 2002;32:79–91. doi: 10.1017/s0033291701004809. [DOI] [PubMed] [Google Scholar]
- 21.French MT, Roebuck MC, Alexander PK. Illicit drug use, employment, and labor force participation. Southern Economic Journal. 2001;68:349–368. [Google Scholar]
- 22.Swift W, Coffey C, Carlin JB, Degenhardt L, Patton GC. Adolescent cannabis users at 24 years: trajectories to regular weekly use and dependence in young adulthood. Addiction. 2008;103:1361–1370. doi: 10.1111/j.1360-0443.2008.02246.x. [DOI] [PubMed] [Google Scholar]
- 23.Wilson N, Syme SL, Boyce W, Battistich VA, Selvin S. Adolescent and alcohol, tobacco, and marijuana use: the influence of neighborhood disorder and hope. Am J Health Promot. 2005;20:11–19. doi: 10.4278/0890-1171-20.1.11. [DOI] [PubMed] [Google Scholar]
- 24.Wright DA, Bobashev G, Folsom R. Understanding the relative influence of neighborhood, family, and youth on adolescent drug use. Subst Use Misuse. 2007;42:2159–2171. doi: 10.1080/10826080701212675. [DOI] [PubMed] [Google Scholar]
- 25.Lambert SF, Brown TL, Phillips CM, Ialongo NS. The relationship between perceptions of neighborhood characteristics and substance use among urban African American adolescents. Am J Community Psychol. 2004;35:205–218. doi: 10.1007/s10464-004-7415-3. [DOI] [PubMed] [Google Scholar]
- 26.Reboussin BA, Hubbard S, Ialongo NS. Marijuana use patterns among African-American middle-school students: a longitudinal latent class regression analysis. Drug Alcohol Depend. 2007;90:12–24. doi: 10.1016/j.drugalcdep.2007.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tarter RE, Vanyukov M, Kirisci L, Reynolds M, Clark DB. Predictors of marijuana use in adolescents before and after licit drug use: examination of the gateway hypothesis. Am J Psychiatry. 2006;163:2134–2140. doi: 10.1176/ajp.2006.163.12.2134. [DOI] [PubMed] [Google Scholar]
- 28.Patton GC, Coffey C, Carlin JB, Sawyer SM, Wakefield M. Teen smokers reach their mid twenties. J Adolesc Health. 2006;39:214–220. doi: 10.1016/j.jadohealth.2005.11.027. [DOI] [PubMed] [Google Scholar]
- 29.Newcomb MD, Felix-Ortiz M. Multiple protective and risk factors for drug use and abuse: cross-sectional and prospective findings. J Pers Soc Psychol. 1992;63:280–296. doi: 10.1037//0022-3514.63.2.280. [DOI] [PubMed] [Google Scholar]
- 30.Brown TL, Miller JD, Clayton RR. The generalizibilty of substance use predictors across racial groups. The Journal of Early Adolescence. 2004;24:274–309. [Google Scholar]
- 31.Wallace JM, Muroff JR. Preventing substance abuse among African American children and youth: race differences in risk factor exposure and vulnerability. J Prim Prev. 2002;22:235–261. [Google Scholar]
- 32.Abbey A, Jacques AJ, Hayman LW, Sobeck J. Predictors of early substance use among African American and Caucasian youth from urban and suburban communities. Merrill-Palmer Quarterly. 2006;52:305–326. [Google Scholar]
- 33.Wayne WD. Biostatistics: A Foundation for Analysis in the Health Sciences. Hoboken, NJ: John Wiley & Sons; 2005. [Google Scholar]
- 34.Chavez EL, Oetting ER, Swaim RC. Dropout and delinquency: Mexican-American and Caucasian non-Hispanic youth. J Clin Child Psychol. 1994;23:47–55. [Google Scholar]
- 35.Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychol Med. 1983;13(3):595–605. [PubMed] [Google Scholar]
- 36.Jackson DN. Personality research form. Goshen, NY: Research Psychologists Press; 1974. [Google Scholar]
- 37.Spanier GB. Measuring dyadic adjustment: new scales for assessing the quality of marriage and similar dyads. Journal of Marriage and the Family. 1976;38:15–28. [Google Scholar]
- 38.Huizinga DH, Menard S, Elliot DS. Delinquency and drug use: temporal and developmental patterns. Justice Quarterly. 1989;6:419–455. [Google Scholar]
- 39.Oetting ER, Beauvais F. Peer cluster theory, socialization characteristics, and adolescent drug use: A path analysis. Journal of Counseling Psychology. 1987;34:205–213. [Google Scholar]
- 40.Johnston JD, Bachman JG, O’Malley PM. Monitoring the Future study, 2002. Ann Arbor: Institute for Social Research, University of Michigan, Survey Research Center; 2002. [Google Scholar]
- 41.Heatherton TF, Kozlowski LT, Frecker RC, Fagerström K. The Fagerstrom test for nicotine dependence: a revision of the Fagerstrom Tolerance Questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- 42.Johnston JD, Bachman JG, O’Malley PM. Monitoring the Future study, 1994. Ann Arbor: Institute for Social Research, University of Michigan, Survey Research Center; 1994. [Google Scholar]
- 43.Cohen P, Cohen J. Life values and adolescent mental health. Mahwah, New Jersey: Lawrence Erlbaum Associates; 1996. [Google Scholar]
- 44.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: American Psychiatric Press; 1994. [Google Scholar]
- 45.Kessler RC, Wittchen HU, Abelson JM, McGonagle K, Schwartz N, Kendler KS, Knäuper B, Zhao S. Methodological studies of the Composite International Diagnostic Interview (CIDI) in the US National Comorbidity Survey (NCS) Int J Methods Psychiatr Res. 1998;7:33–55. [Google Scholar]
- 46.Myrtveit I, Stensrud E, Olsson UH. Analyzing data sets with missing data: an empirical evaluation of imputation methods and likelihood-based methods. IEEE Transactions on Software Engineering. 2001;27(11):999–1013. [Google Scholar]
- 47.Muthén B, Kaplan D, Hollis M. On stuctural equation modeling with data that are not missing completely at random. Psychometrika. 1987;52:431–462. [Google Scholar]
- 48.Chen K, Kandel DB. The natural history of drug use from adolescence to the mid-thirties in a general population sample. Am J Public Health. 1995;85:41–47. doi: 10.2105/ajph.85.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Khantzian EJ, Albanese MJ. Understanding Addiction as Self Medication: Finding Hope Behind the Pain. Lanham, MD: Rowman & Littlefield Publishers, Inc; 2008. [Google Scholar]
- 50.Bandura A. Social Learning Theory. Englewood Cliffs, NJ: Prentice-Hall; 1977. [Google Scholar]
- 51.Jessor R, Jessor SL. Problem Behavior and Psychosocial Development: A Longitudinal Study. New York: Academic Press; 1997. [Google Scholar]
- 52.Winters KC, Lee CY. Likelihood of developing an alcohol and cannabis use disorder during youth: association with recent use and age. Drug Alcohol Depend. 2008;92:239–247. doi: 10.1016/j.drugalcdep.2007.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bachman JG, O'Malley PM, Schulenberg JE, Johnston LD, Bryant AL, Merline AC. The Decline of Substance Use in Young Adulthood: Changes in Social Activities, Roles, and Beliefs. Mahwah, New Jersey: Lawrence Erlbaum Associates; 2002. [Google Scholar]
- 54.Stinson FS, Ruan WJ, Pickering R, Grant BF. Cannabis use disorders in the USA: prevalence, correlates and co-morbidity. Psychol Med. 2006;36:1447–1460. doi: 10.1017/S0033291706008361. [DOI] [PubMed] [Google Scholar]
- 55.Castro FG, Brook JS, Brook DW, Rubenstone ER. Paternal, maternal, and youth risk factors as predictors of youth stage of substance use: a longitudinal study. J Addict Dis. 2006;25:65–75. doi: 10.1300/J069v25n02_10. [DOI] [PubMed] [Google Scholar]
- 56.Bry BH, McKeon P, Pandina RJ. Extent of drug use as a function of a number of risks. J Abnorm Psychol. 1982;91:273–279. doi: 10.1037//0021-843x.91.4.273. [DOI] [PubMed] [Google Scholar]
- 57.Dohrenwend BP, Turner JB, Turse NA, Lewis-Fernandez R, Yager TJ. War-related posttraumatic stress disorder in Black, Hispanic, and majority White Vietnam veterans: the roles of exposure and vulnerability. J Trauma Stress. 2008;21:133–141. doi: 10.1002/jts.20327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mennes CE, Abdallah AB, Cottler LB. The reliability of self-reported cannabis abuse, dependence and withdrawal symptoms: a multisite study of differences between general population and treatment groups. Addict Behav. 2009;34:223–226. doi: 10.1016/j.addbeh.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 59.Kliewer W, Murrelle L. Risk and protective factors for adolescent substance use: findings from a study in selected Central American countries. J Adolesc Health. 2007;40:448–455. doi: 10.1016/j.jadohealth.2006.11.148. [DOI] [PubMed] [Google Scholar]