Abstract
Fragile X syndrome (FXS) is the most common form of inherited intellectual disability and the leading known genetic cause of autism. Fragile X mental retardation protein (FMRP), which is absent or expressed at substantially reduced levels in FXS, binds to and controls the postsynaptic translation of amyloid β-protein precursor (AβPP) mRNA. Cleavage of AβPP can produce β-amyloid (Aβ), a 39–43 amino acid peptide mis-expressed in Alzheimer's disease (AD) and Down syndrome (DS). Aβ is over-expressed in the brain of Fmr1KO mice, suggesting a pathogenic role in FXS. To determine if genetic reduction of AβPP/Aβ rescues characteristic FXS phenotypes, we assessed audiogenic seizures (AGS), anxiety, the ratio of mature versus immature dendritic spines and metabotropic glutamate receptor (mGluR)-mediated long-term depression (LTD) in Fmr1KO mice after removal of one App allele. All of these phenotypes were partially or completely reverted to normal. Plasma Aβ1–42 was significantly reduced in full-mutation FXS males compared to age-matched controls while cortical and hippocampal levels were somewhat increased, suggesting that Aβ is sequestered in the brain. Evolving therapies directed at reducing Aβ in AD may be applicable to FXS and Aβ may serve as a plasma-based biomarker to facilitate disease diagnosis or assess therapeutic efficacy.
Introduction
FXS is an X chromosome-linked disorder characterized by highly variable intellectual disability, autistic-like behavior and seizures [1]. In the vast majority of cases, FXS results from a >200 trinucleotide (CGG) repeat expansion in the 5′-UTR of the FMR1 gene [2] leading to transcriptional silencing and loss or reduction of expression of FMRP [3]. FMRP is a multi-functional mRNA binding protein involved in the dendritic transport, localization and translational regulation of several hundred mRNA ligands [4]–[9]. In the absence of FMRP, dendritic spine morphology and function are abnormal [10]. Thus, FXS is likely caused by the inappropriate, post-synaptic expression of one or more FMRP mRNA targets. We have previously demonstrated that post-synaptic translation of App mRNA is regulated by FMRP through a mGluR5-dependent pathway. In the absence of FMRP, excess AβPP and its catabolites Aβ1–40 and Aβ1–42, accumulate in the brains of middle-aged Fmr1KO mice [11].
There is very limited data regarding the roles of AβPP mRNA, protein and catabolites in persons with FXS. One group showed elevated App mRNA in the cerebral cortex, hippocampus and cerebellar cortex in Fmr1KO mice [12], but we have not observed differences in cortical synaptoneurosomes [11]. Increased Aβ levels would predict an increased incidence of AD pathology in aged FXS individuals, which has not been observed in neuropathological analyses of a very small number of specimens [13]–[15]. Likewise, there are no reports of an increased incidence of AD in FXS, but it is difficult to assess age-related dementia in the mentally retarded and very few elderly individuals with FXS have been studied in significant numbers. Recent data suggests that AβPP or its proteolytic derivatives may be aberrantly expressed in children with severe autism [16], [17], which is extremely prevalent in FXS (67% of males and 23% of females) [18] and DS (7%) [19]. Thus, the increased production or altered processing of AβPP may contribute to the intellectual disabilities observed in all of these disorders.
Herein, we demonstrate rescue of several Fmr1KO phenotypes in model mice by genetic modulation of AβPP/Aβ levels. Treatment of primary neurons with Aβ1–42 rapidly triggered extracellular-regulated kinase (ERK) signaling and altered the translation of multiple FMRP target mRNAs including App. Conversely, anti-Aβ antibody decreased dendritic AβPP levels. These data suggest that Aβ modulates its own production through a positive feedback loop. Finally, we show that plasma Aβ1–42 is significantly reduced while cerebral Aβ1–42 is likely increased in full-mutation FXS males. These data suggest evolving therapies directed at reducing Aβ in AD may be applicable to FXS and plasma Aβ1–42 may be a biomarker for disease severity and drug efficacy in FXS.
Results
Genetic Modulation of AβPP Levels in Fmr1KO Mice Reduces AGS
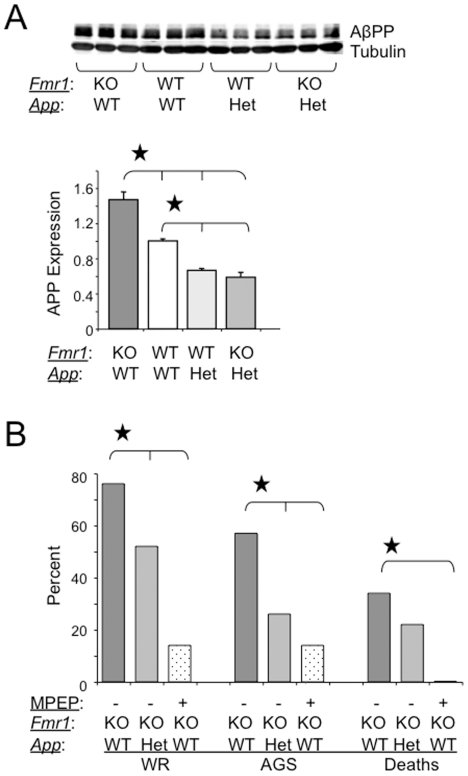
Compared to WT, Fmr1KO mice exhibit AGS [20], altered anxiety [21]–[23] and dendritic spine dysmorphogenesis [24]–[26], features shared with patients with FXS [1], [27], [28]. In order to establish if AβPP or Aβ directly contributed to FXS pathogenesis, we modulated AβPP and Aβ expression in Fmr1KO mice. Thus, we generated Fmr1KO/AppHET and Fmr1KO/AppKO mice all in a pure C57BL/6 background to evaluate the effects of genetic modulation of AβPP and Aβ expression. Western blot analyses confirmed that AβPP levels were reduced by 50% in Fmr1KO/AppHET mice (Figure 1A). At 21 days of age, animals were evaluated for AGS. Wild running (WR) and seizures decreased 32% and 54%, respectively, in Fmr1KO/AppHET mice (Figure 1B). These data suggest that seizures are enhanced when AβPP is absent or over-expressed and that AβPP or one of its metabolites significantly contributes to the AGS phenotype seen in Fmr1KO mice.
Figure 1. AGS are rescued by genetic manipulation of App or mGluR5 blockade.
(A) western blot analyses of AβPP levels in Fmr1KO, WT, AppHE T and Fmr1KO/AppHET mice (n = 3 male mice per strain, 1 month old). Statistics: one-way ANOVA p<0.0001, F = 53.95. Stars (★) denote statistically different levels by Student T-test analyses and by Bonferroni's multiple comparison test (p<0.05). Error bars represent SEM. (B) Assessment of WR, AGS and death rates in Fmr1KO mice (age P21, n = 58)) after genetic manipulation of AβPP levels (n = 23) or treatment with MPEP (n = 14). Stars (★) denote rates that are statistically different from untreated mice (p<0.5) by Fisher exact tests.
Pharmacological antagonists directed at or genetic reduction of mGluR5 correct many Fmr1KO phenotypes [22], [26], [29]–[31]. We compared the efficacy of mGluR5 antagonists with genetic manipulation of AβPP/Aβ in reducing AGS in Fmr1KO mice. A 30 min pretreatment with 2-methyl-6-(phenylethynyl)pyridine hydrochloride (MPEP) delivered by I.P. injection reduced WR, AGS and deaths by 82%, 75% and 100%, respectively (Figure 1B). An alternative mGluR5 antagonist, fenobam, reduced WR, AGS and deaths to 0% (data not shown).
Fmr1KO/AppHET Mice Lack FXS Behavioral, Dendritic Spine and mGluR-LTD Phenotypes
Hyperactivity, social anxiety and autistic-like behaviors are characteristic features of FXS [1]. We first assessed marble burying in these mice as a measure of repetitive behavior [32]. Fmr1KO male mice buried significantly fewer marbles than WT (p = 0.04) (Figure 2A), which was rescued in male Fmr1KO/AppHET mice (statistically different compared to Fmr1KO, p = 0.03; not different from WT, p = 0.95). Thus, repetitive digging is a normal mouse behavior that can be rescued in Fmr1KO male mice by genetically reducing AβPP/Aβ levels.
Figure 2. Rescue of behavioral phenotypes in adult Fmr1KO mice by genetic manipulation of App.
(A) male AppKO (n = 8), AppHET (n = 14), WT (n = 7), Fmr-1KO (n = 8), Fmr1KO/AppHET (n = 10) and Fmr1KO/AppKO (n = 4) mice (8–10 weeks old) were assessed for marble burying activity. Statistics: one-way ANOVA p<0.022, F = 2.95. (B, C and D) Mice were assessed for anxiety levels and locomotion in the open field. Both genders were included as the males and females exhibited equivalent locomotion and anxiety in the open field [AppKO (n = 11), AppHET(n = 23), WT (n = 15), Fmr1KO (n = 14), Fmr-1KO/AppHET (n = 18) and Fmr1KO/AppKO (n = 7)]. (B) Total distance (cm) traveled is plotted against mouse strain. Statistics: one-way ANOVA p<0.0005, F = 4.59. (C) Time (sec) spent in the center of the arena is plotted versus mouse strain. Statistics: one-way ANOVA p<0.0001, F = 5.98. (D) Distance (cm) traveled in the center of the arena is plotted versus mouse strain. Statistics: one-way ANOVA p<0.0001, F = 9.17. Stars (★) denote statistically different levels by Student T-test analyses (p<0.5). All error bars represent SEM.
Next, we assessed hyperactivity (Figure 2B) and anxiety (Figure 2C, D) in the open field test. Fmr1KO exhibit increased center time (reflecting a loss of anxiety) but equivalent locomotion in the open field compared with WT mice [21], [22]. AppHET and AppKO mice exhibited significantly more anxiety/thigmotaxis than WT mice (Figure 2C). The increased thigmotaxis in the AppHET is partially due to decreased locomotion compared with WT mice (Figure 2B); however, total distance traveled was equivalent between AppKO and AppHET indicating that decreased AβPP /Aβ levels correlate with increased anxiety. Fmr1KO/AppHET mice exhibited equivalent center time as WT mice and significantly less than Fmr1KO mice indicating that thigmotaxis was rescued. Total distance traveled in the open field was not statistically different between Fmr1KO/AppHET, WT and/or Fmr1KO mice indicating equivalent locomotion.
Pathological examination of brains from FXS patients has shown an increased density of long and tortuous dendritic spines suggesting a delay in spine maturation [15], [33]. We assessed dendritic spine length in primary cultured neurons and found a statistically significant 1.6-fold increase in protrusion length in the Fmr1KO cells compared to WT (Figure 3A, B) in agreement with the literature [24]–[26]. A 4 hr treatment with mGluR5 antagonists (MPEP or fenobam) rescued the spine/filopodia ratio in Fmr1KO mice to WT levels [26]. Likewise, we observed that both dendritic spine length and the percentage of filopodia in primary cultured Fmr1KO neurons were reverted to WT levels within 15 min of MPEP treatment (Figure 3B). Average protrusion length was reduced by 11% in the Fmr1KO/AppHET cells (statistically significant p<0.03 compared to Fmr1KO), and the percentage of filopodia (immature spines) versus mature spines was completely reverted to WT levels. Similarly, minocycline treatment of Fmr1KO neurons has been reported to rescue the percentage of mature spines to WT levels albeit without a significant change in dendritic protrusion length [24].
Figure 3. Dendritic spine morphology is partially rescued in Fmr1KO/AppHET or MPEP treated Fmr1KO mice.
(A) Representative fluorescent images of primary cultured neurons prepared from WT (upper left), Fmr1KO (upper right and lower left) and Fmr1KO/AppHET (lower right) embryos stained with DiI and visualized by fluorescent microscopy (100× objective). The arrows denote dendritic spines. (B) The lengths of dendritic protrusions were quantitated with StereoInvestigator software and plotted against mouse strain/treatment. The percentage of filopodia versus spines for each condition is given below the histogram. Statistics: one-way ANOVA comparison of the three genotypes (untreated) p<0.0001, F = 27.18. All genotypes are statistically different from each other by Student T-Test and Bonferroni's multiple comparison tests. Two-way ANOVA comparison of WT versus Fmr1KO ± MPEP: p<0.0001, F = 12.89 (interaction), F = 35.01 (genotype) and F = 27.62 (MPEP). The untreated and 15 min MPEP treated WT spines are statistically different from the corresponding Fmr1KO spines by the Bonferroni multiple comparison test (p<0.5). Stars (★) denote statistically different spine lengths by Student T-test analyses (p<0.5). Error bars indicate SEM [Fmr1KO: untreated (n = 746 spines), 15 min MPEP (n = 263), 1 hr MPEP (n = 300), 4 hr MPEP (n = 293); WT: untreated (n = 994), 15 min MPEP (n = 535), 1 hr MPEP (n = 373), 4 hr MPEP (n = 1221); Fmr1KO/AppHET (n = 2469)].
Fmr1KO mice exhibit enhanced hippocampal mGluR-long term depression (LTD), which requires rapid protein synthesis [34], [35]. We assessed hippocampal mGluR-LTD by field recordings in 3-month-old male WT, Fmr1KO, AppHET and Fmr1KO/AppHET mice. mGluR-dependent synaptic depression was enhanced in the CA1 in Fmr1KO slices, equivalent in WT and AppHET and reduced in Fmr1KO/AppHET (statistically significant p<0.0002 comparing Fmr1KO/AppHET and Fmr1KO) (Figure 4). The time course of CA1 fEPSP slopes after DHPG treatment reveals a significant difference between Fmr1KO animals relative to wild type, AppHET and Fmr1KO/AppHET mice. Input/output relationships and paired-pulse facilitation (ppf) were analyzed to assess the basal synaptic properties of the different groups (Figure S1), and did not show significant changes between experimental groups indicating unaltered synaptic transmission in the Fmr1KO hippocampus.
Figure 4. Rescue of mGluR-dependent synaptic depression in the CA1 in Fmr1KO/AppHET mice.
(Top) Representative fEPSP taken before the addition of DHPG (solid lines) and at the end of the recordings (dotted lines). (Bottom) Time course of CA1 fEPSP slope after incubation with DHPG (50 µM, 10 min) in hippocampal slices from WT (black circles) (n = 20), Fmr1KO (white circles) (n = 13), AppHET (black triangles) (n = 15) and Fmr1KO/AppHET (white triangles) (n = 10) male mice (3 months old). WT, AppHET and Fmr1KO/AppHET were all statistically different from Fmr1KO by two-way ANOVA/Bonferroni multiple comparison tests. WT versus AppHET, p = 0.92; WT versus Fmr1KO, p<0.006; WT versus Fmr1KO/AppHET, p<0.02; AppHET versus Fmr1KO/AppHET, p<0.04; AppHET versus Fmr1KO, p = 0.02; Fmr1KO versus Fmr1KO/AppHET, p<0.0002. Error bars indicate SEM.
Aβ1–42 Alters Dendritic Expression of FMRP Targets
To begin to understand how excessive production and/or processing of AβPP mediates cell signaling events, we examined dendritic expression of select FMRP targets after treating WT primary neurons with soluble Aβ1–42. There was a >2-fold increase in the expression of AβPP, no change in Arc, 40% increase in Map1B, 85% increase in RhoB and 50% decrease in PSD95 (Figure 5A). The Aβ1–42-mediated increase in dendritic AβPP could be blocked with MPEP or anisomycin indicating that it was mGluR5- and translation-dependent (Figure 5B). Conversely, reduction of Aβ in the cell culture media by treatment with anti-Aβ antibody through a transwell reduced dendritic AβPP expression by 31% (Figure 5C). We utilized transwells to avoid direct contact between the antibody and the cells as direct application of anti-Aβ to the culture media dramatically increased AβPP expression presumably due to cell signaling events initiated by anti-Aβ binding to cell surface receptors (data not shown). MPEP and Aβ1–42 altered phosphorylated levels of ERK (Figure S2), suggesting that the mitogen activated protein kinase pathway is as an intermediate in Aβ-mediated AβPP translation.
Figure 5. Aβ1–42 alters dendritic protein levels.
(A) WT neuronal cells treated with vehicle, 20 or 100 nM Aβ1–42 for 1 hr followed by fixation and staining for AβPP, Arc/Arg, Map1B, RhoB and PSD95 and analyses by confocal fluorescent microscopy. (B) WT neuronal cells pre-treated with vehicle, 2.5 µM MPEP or 40 µM anisomycin for 15 min prior to treatment with 20 nM Aβ1–42 for 1 hr and fixation and staining for AβPP. Statistics: one-way ANOVA p<0.0001, F = 7.04. All treatments are statistically different from the 20 nM Aβ1–42 treatment by the Bonferroni multiple comparison test (p<0.05). A minimum of 1793 particles were analyzed per treatment cohort. (C) WT neuronal cells treated with mouse IgG or anti-Aβ antibody in transwells for 3 days prior to fixation and staining for AβPP. Statistics: one-way ANOVA p<0.05, F = 3.03. A minimum of 2,644 particles were analyzed per treatment cohort. Stars (★) denote statistical differences by Student T-test analyses (p<0.5). Error bars indicate SEM.
Aβ1–42 Levels are Abnormal in Humans with FXS
We are unaware of any published data evaluating AβPP or its products in the blood of adult FXS patients. We found that plasma AβPP/AβPPα and Aβ1–40 levels were comparable in adult FXS patients and controls (Figure 6A, B). These results are distinct from those previously observed in children [16] and suggest that AβPP expression and processing decrease with age. Indeed, AβPPα levels are higher in children 7 years and younger than those 10 years and older [16]. While plasma Aβ1–40 levels were unchanged between FXS and controls, Aβ1–42 was significantly lower in the FXS group (2.1-fold decrease, p<0.004) (Figure 6B). As seen in other amyloidogenic diseases, the Aβ1–42/Aβ1–40 ratio (1.4∶1) in blood plasma was substantially reduced compared to controls (3.4∶1) suggesting decreased clearance from the brain. There was no statistically significant increases in cell-associated AβPP, secreted AβPPα nor APP 695/751/770 mRNA in peripheral blood mononuclear cells (PBMC) samples from FXS and control donors (Figure 6A and data not shown).
Figure 6. AβPP/Aβ are abnormal in blood and brain from FXS patients.
(A) AβPPα levels in control (n = 7) and FXS (n = 10) plasma and PBMC culture media (n = 7 controls and 4 FXS) and AβPP in PBMC (n = 7 controls and 5 FXS). For the plasma and PBMC culture media data, AβPPα is expressed as ng/mL and for the PBMC lysate measurements, AβPP is expressed as ng/mL/µg lysate. (B) Aβ1–40 and Aβ1–42 levels in control (n = 7) and FXS (n = 10) plasma. For Aβ1–42, p<0.004 as determined by Student T-Test analyses. (C) AβPP/AβPPα in control (n = 3) and FXS (n = 4) neocortex and hippocampus. Controls were gender- and age-matched to FXS donors by the University of Maryland Brain Bank. All of the donors were Caucasian males and their ages ranged from 21–85 years old. (D) Soluble Aβ1–40 levels in control (n = 3) and FXS (n = 4) neocortex and hippocampus. White bars = control samples and gray bars = FXS. Error bars represent SEM.
We next assessed AβPP/AβPPα, Aβ1–40 and Aβ1–42 in hippocampal and neocortical control and FXS autopsy brain tissue. The data represents analyses of four FXS and three control brains. There is a strong trend toward increased soluble Aβ1–40 in lysates of FXS brain samples (Figure 6D) while AβPP/AβPPα levels are reciprocally decreased (Figure 6C) in both the neocortex and hippocampus. Despite the small sample size due to the unavailability of tissue, the 1.7-fold decrease in AβPP/AβPPα in neocortex approaches statistical significance. These data suggest that the brain may act as a sink for Aβ and that lower blood plasma levels may indicate increased brain deposition. These results are similar to those in Fmr1KO mice, which exhibited elevated Aβ in the brain [11]. Murine Aβ levels in blood plasma were below the ELISA detection limit and could not be determined.
These data strongly support the hypothesis that modest over-expression of AβPP and/or Aβ, in the context of the Fmr1KO, is necessary for many of the pathological phenotypes including AGS, anxiety, dendritic dysmorphogenesis and mGluR-LTD observed in the mice and that these effects are likely mediated by mGluR5 signaling. Furthermore, these data suggest a positive feedback loop whereby extracellular Aβ stimulates dendritic translation of AβPP through a mGluR5 signaling pathway providing more target for amyloidogenic processing and the generation of additional Aβ.
Discussion
FXS is the most common form of inherited mental retardation and autism. It is caused by the loss of FMRP, an mRNA binding protein, which localizes to dendrites and regulates protein synthesis. Considerable effort has focused on characterizing the FMRP mRNA ligands and signaling pathways, particularly mGluR5 [36], that contribute to FXS phenotypes. We have demonstrated that App mRNA is an FMRP mRNA ligand whose translation is regulated through mGluR5 [11].
AβPP plays a critical physiological role in synapse formation and maintenance [37], [38] with expression increasing during neuronal differentiation, maximal during synaptogenesis and decline when mature connections are completed [39]–[42]. Maximal AβPP expression coincides with the critical period of sensory development in rodents (postnatal weeks 2–6) [43]. FMRP is also developmentally regulated in the neonatal brain where it peaks at the end of the first postnatal week and declines thereafter [44]. AβPP is processed by α-, β- and/or γ-secretases to produce soluble N-terminal domains of AβPP (sAβPPα and sAβPPβ), Aβ and C-terminal fragments. Aβ, which is over-expressed in AD and DS [45], is strongly implicated in impaired synaptic function and synapse loss observed early in the development of AD [46], [47], and we propose that their dysregulated production in FXS contributes to disease pathology. From conception, DS individuals over-express APP mRNA, AβPP and extracellular amyloid [48], [49]. Like FXS, DS patients show mental retardation, craniofacial abnormalities and dendritic dysmorphogenesis [1], [50]. Thus, increased AβPP and/or AβPP proteolytic products could provide a common effector at the molecular level for the neuroanatomic and behavioral phenotypes observed in all of these disorders [51].
We found that the peripheral concentration of Aβ1–42 and the Aβ1–42/Aβ1–40 ratio were significantly decreased in full-mutation FXS males compared to control donors. A reduced Aβ1–42/Aβ1–40 ratio is an independent risk factor for AD irrespective of the total Aβ load [52]–[58]. Plasma Aβ1–42 levels are increased in patients with mild cognitive impairment, but drop to control levels by the time of AD diagnosis [59]. In DS, elevated plasma Aβ1–42 is associated with earlier onset of AD [60] and the Aβ1–42/Aβ1–40 blood plasma ratio is lower than in controls [61]. Thus, our finding of a reduced Aβ1–42/Aβ1–40 ratio in FXS patients compared to control plasma is consistent with other amyloidogenic diseases.
The effectiveness of drug therapy in FXS is currently assessed exclusively by behavioral testing. Perhaps most importantly, the availability of a plasma biomarker for FXS may permit the monitoring of drug therapy as well as predict disease progression. Other studies have demonstrated reduced cAMP production in platelets [62] and delayed early-phase phosphorylation of ERK in lymphocytes [63] from FXS patients. Our data demonstrates that Aβ1–42 is significantly lower in FXS plasma than control subjects, and in conjunction with two studies demonstrating elevated sAβPPα in autistic children [16], [17], suggests that both AβPP and Aβ are viable biomarkers for FXS. We did not observe increased sAβPPα in adult FXS plasma suggesting that AβPP expression and processing decrease with age consistent with prior studies [16]. Previously reported control plasma levels of Aβ range from 130–208 pg/mL for Aβ1–40 and 15 pg/mL–85.7 ng/mL for Aβ1–42 [53], [58], [64], [65]. Thus, there is wide range of reported plasma Aβ1–40 and Aβ1–42 levels in the literature and our studies fall within that range. A critical question remains regarding if these catabolites are associated with disease severity or progression. There is a paucity of human FXS brain tissue available for analyses. Our preliminary studies indicate a trend for elevated Aβ in FXS brain, which agrees with data in Fmr1KO mice [11].
FXS patients exhibit hyper-reactivity to visual, olfactory, tactile and auditory stimulation [1], [66]–[69]. This hypersensitivity phenotype is manifested as AGS in Fmr1KO mice [20]. If Aβ contributes to AGS, then AD and DS mice would also be susceptible to seizures. Consistent with this, Tg2576, FRAXAD and DS mice, which all over-express hAβPP with the Swedish familial mutation and/or mouse AβPP, exhibit AGS [70]. Fmr1KO/AppHET male mice exhibited a statistically significant decrease in AGS but not in WR whereas MPEP significantly reduced WR in Fmr1KO mice. These data suggest that the reduction of AβPP/Aβ in Fmr1KO mice is not particularly effective at reducing the induction of AGS, but does retard progression to clonic-tonic seizures. Fmr1KO mice also exhibit enhanced mGluR-LTD [34], which is lost in Fmr1KO/AppHET mice. The Fmr1KO reduces mGluR-LTD in an AppHET background, but enhances mGluR-LTD in an AppWT background. The large difference in the maximal depression of synaptic transmission between Fmr1KO/AppHET and Fmr1KO in opposite directions from WT mice, which exhibit equivalent mGluR-LTD as AppHET, suggests that FMRP and AβPP/Aβ play important and synergistic roles in modulating mGluR-LTD. Thus, the over-expression of AβPP or an AβPP catabolite lowers seizure threshold and enhances mGluR-LTD, and approaches to attain normal synaptic levels of these proteins could prove therapeutic.
MPEP is a potent and highly selective noncompetitive antagonist of mGluR5 [71], [72] that reduces AGS, anxiety phenotypes and dendritic spine protrusion morphology in Fmr1KO [22], [26]. We have previously demonstrated that mGluR5 blockade inhibits translation of AβPP in synaptoneurosomes [11] and herein demonstrate reversion of several FXS phenotypes by genetic manipulation to reduce AβPP/Aβ. Minocycline, a second-generation tetracycline compound, reverts several FXS phenotypes [24], possibly by altered Aβ fibril formation [73] or Aβ-induced neuronal death and glial activation [74]. In aggregate, these data suggest that mGluR5 antagonists and minocycline therapies converge on a similar signaling pathway resulting in decreased Aβ levels/activity as obligatory for the rescue of FXS phenotypes.
How Aβ mediates synaptic dysfunction remains unclear. Aβ promotes AD-like cytoskeletal abnormalities and can promote intracellular accumulation of sAβPP in primary cultured neurons [75]. Soluble oligomers of Aβ increase LTD in WT hippocampal slices and inhibit long-term potentiation [76]–[80]. A similar enhancement of mGluR5-mediated LTD occurs in the hippocampus of Fmr1KO mice [34], and MPEP prevents the block in long-term potentiation [81]. Aβ causes membrane depolarization and calcium influx, activates mGluR1 [82] and functions as an extracellular scaffold for mGluR5 [83]. In vitro, Aβ1–42 altered the expression of important dendritic proteins regulated by FMRP including AβPP, Map1B and PSD95 with known roles in synaptogenesis and/or dendritic spine morphology [37], [38], [44], [84]. A previous report utilizing neuronal hybrid cells demonstrated that Aβ1–40 increases AβPP levels also supporting the existence of an Aβ-driven positive feedback loop [85]. Lower levels of PSD95 are observed in Tg2576 neurons, which constitutively overexpress Aβ and ADDLs [84]. In our hands, levels of the immediate-early gene Arc were not changed during a 1 hr stimulation with low molecular weight oligomers of Aβ1–42; however, others have observed that higher molecular weight Aβ oligomers (10–100 kDa) bind in a punctate pattern to the surface of neurons, colocalize with PSD95 and upregulate Arc [47]. We can block the Aβ-induced increase in AβPP levels with either MPEP or anisomycin suggesting that an mGluR5- and translation-dependent pathway is involved. The varied expression of known FMRP targets in response to Aβ suggests that dendritic translation can be modulated through FMRP-dependent and independent pathways. Aβ1–42 rapidly increases phosphorylated ERK levels suggesting that ERK mediates downstream signaling.
In conclusion, our work demonstrates that AβPP translation is regulated through an mGluR5/FMRP-mediated pathway. Excessive signaling through mGluR5 in the absence of FMRP leads to increased AβPP production and processing and we have observed elevated AβPP and Aβ levels in Fmr1KO mice [11]. Genetic reduction of AβPP levels in Fmr1KO mice has reverted or partially rescued FXS seizure, behavioral, dendritic spine and mGluR-LTD phenotypes. Furthermore, treatment of primary neurons with Aβ1–42 increased while anti-Aβ reduced dendritic AβPP expression suggesting that an Aβ-driven positive feedback loop drives synthesis/processing of AβPP through a mGluR5 signaling pathway. Our results have potential implications for the treatment of FXS as plasma AβPP/Aβ can be readily screened as biomarkers to evaluate potential therapies including mGluR5 antagonists as well as secretase inhibitors and anti-Aβ, which are currently undergoing testing for the treatment AD.
Materials and Methods
Ethics Statement
Adequate measures were taken to minimize pain or discomfort to the mice, and all husbandry, seizure and euthanasia procedures were performed in accordance with NIH and an approved University of Wisconsin-Madison animal care protocol administered through their Research Animal Resources Center (approval #G00468). Males with FXS and age-matched controls were recruited from the FXS Clinic at Rush University Medical Center (RUMC) in Chicago, IL. The study was approved by the RUMC Institutional Review Board and all donors or their legal guardians signed the appropriate consent forms for study participation.
Mouse Husbandry
WT and Fmr1KO mice (C57BL/6 background) were bred and housed as previously described) [11]. Fmr1KO females [86] were crossed with AppKO males [87] (Jackson Laboratories #004133, C57BL/6 background) to generate Fmr1HET/AppHET females and Fmr1KO/AppHET males that were crossed to generate Fmr1KO/AppKO mice. For the behavioral testing, littermate controls were generated by crossing Fmr1KO/AppHET females with Fmr1KO/AppHET males to generate Fmr1KO/AppWT, Fmr1KO/AppHET and Fmr1KO/AppKO progeny and by crossing Fmr1WT/AppHET females with Fmr1WT/AppHET males to generate Fmr1WT/AppWT, Fmr1WT/AppHET and Fmr1WT/AppKO progeny. Genotypes were determined by PCR analysis of DNA extracted from tail biopsies. The WT, HET or KO state of the App gene was determined by genotyping with primer 1: 5′-CTG CTG CAG GTG GCT CTG CA-3′, primer 2: 5′-CAG CTC TAT ACA AGC AAA CAA G-3′, and primer 3: 5′-CCA TTG CTC AGC GGT GCT GTC CAT-3′ to generate a 250 base pair WT allele with primers 1 and 2 and a 470 base pair targeted KO allele with primers 2 and 3.
Assessment of AβPP by Western Blot Analyses
Left hemispheres from WT, Fmr1KO, AppHET and Fmr1KO/AppHET mice (1 month old males; n = 3 per genotype) were homogenized in protein extraction buffer [10 mM Tris (pH 7.6), 2 mM EDTA, 150 mM NaCl, 1% Triton X-100, 0.25% NP-40, 1× protease inhibitor cocktail (Research Products International Corp., Mount Prospect, IL, USA, catalog #P50600)], mixed for 30 min at 4°C and spun at 12,000 rpm for 10 min at 4°C. The protein concentrations of the supernatants were determined by BCA assay (Thermo Fisher/Pierce, Rockford, IL, USA). Lysates (18.75 µg per lane) were separated by 12% SDS-PAGE, transferred to nitrocellulose and western blotted as previously described [11] with anti-AβPP antibody (Life Technologies Corporation, Carlsbad, CA, USA, catalog #51-2700; diluted 1∶250) and anti-tubulin (Santa Cruz Biotechnology, Santa Cruz, CA, catalog #sc-8035; diluted 1∶250). AβPP signals were normalized to tubulin and plotted as a percentage compared to WT levels. Error bars represent the SEM of three mice.
Audiogenic Seizures
All mouse strains were tested at postnatal day 21, the peak of AGS sensitivity in C57BL/6. The experimental apparatus consisted of a clear, Plexiglas box (13″L×8″W×7″H) with the sound source located inside the box (LOUD KEY™ jogger's alarm). Mice were weighed and then placed individually into the center of the chamber and exposed to a siren that generated noise at 118 dB for 5 min. Loud, acoustic stimulation causes WR within 20–30 sec followed by erratic leaping, clonic convulsions and tonic hind limb extension by 40–50 sec followed by respiratory arrest and death [32]. The percentage of mice exhibiting WR, AGS and death were scored versus gender and genotype and assessed for statistical significance by the Fisher exact test. The Fmr1KO/AppHET mice used in the AGS studies were offspring generated by crossing Fmr1KO females with Fmr1KO/AppKO males to avoid effects due to maternal genotype in comparing Fmr1KO and Fmr1KO/AppHET. MPEP was a kind gift from FRAXA Research Foundation (Newburyport, MA) and was dissolved at 1 mg/mL in DPBS before I.P. injection at 30 mg/kg body weight 30 min prior to AGS testing at age P21.
Marble Burying
Mice were acclimated to the behavioral testing room for at least 15 min prior to transfer to a clean cage containing corn cob bedding and 20 black marbles arranged in a rectangular 4×5 grid over 2/3 of the cage. The mouse was placed into the cage at the end that did not contain marbles and allowed to explore the new cage with the marbles for 30 min after which the mouse was returned to its homecage and the number of visible marbles (more than half not buried) counted. Background white noise in the room was set to 70 dB. There is variability in this assay with some laboratories observing that Fmr1KO mice bury more marbles than WT (R. Paylor, personal communication); however, differences in behavioral outcomes can vary between facilities due to genetic background or altered environmental factors such as housing conditions and diet.
Open Field
Mice were acclimated to the behavioral testing room for at least 30 min before placement into the center of a clear, Plexiglas chamber measuring 14.5″L×14.5″W×10″H. Mouse movement was monitored in the chamber for 15 minutes with LimeLight2 software interfaced with an overhead camera. The open field arena was arranged into a 16 square grid in the camera window with 4 squares in the center and 12 squares around the perimeter. Time spent in the center 4 squares (measure of anxiety) and total distance traveled (measure of locomotion) were compared between genotypes.
DiI Labeling and Analyses of Dendritic Spines
Primary mouse neurons were prepared from embryonic (age E15–17) dissected brains from timed pregnant WT and Fmr1KO female mice as previously described) [11]. To generate Fmr1KO/AppHET cells, Fmr1KO females were mated with Fmr1KO/AppKO males. Cells were cultured for 15 days on poly(D)-lysine coated glass coverslips inside of 12-well tissue culture dishes, fixed with 4% paraformaldehyde and stained with lipophilic DiI dye (Life Technologies Corporation, Carlsbad, CA, USA). For the staining, the wells were aspirated and sprinkled with DiI crystals and a small amount of DBPS was added to the edge of the wells to prevent dehydration of the cells. Cells were stained for 10 min, copiously washed with DPBS to remove all crystals and fixed to slides with ProLong Gold Antifade (Life Technologies Corporation, Carlsbad, CA, USA). Slides were allowed to dry for at least 3 days to allow complete migration of the DiI into dendritic spines. Dendritic spines were imaged on a Zeiss Axioplan 2 Imaging Photomicroscope equipped with a MBF Biosciences automated XYZ stage and MicroFire A/R camera. Images were taken using the 100× objective (Zeiss FLUAR 100×/1.30 oil) and Zeiss Immersol™ 518F oil at ambient temperature. Spine length was quantitated with StereoInvestigator v9 software. Contours were drawn around the protrusions and the feret max (length) and feret min (widest width) of the contours were calculated. A minimum of 2–6 coverslips were analyzed per neuronal cell prep and images of neurons were taken from multiple areas of those coverslips. Data is representative of multiple batches of neuronal cells. A minimum of 746 spines were quantitated per genotype. The feret width was divided by feret max and protrusions having a ratio less than 0.5 were classified as filopodia and those with a ratio greater than or equal to 0.5 were classified as spines. For MPEP treatments, 2.5 µM MPEP was added to the neurons for the indicated times followed by washing the cells with DPBS and fixation and staining as previously described. A minimum of 263 protrusions were quantitated per MPEP treatment.
Hippocampal Slice Preparation and mGluR-LTD Field Recordings
WT, Fmr1KO, AppHET and Fmr1KO/AppHET mice were rapidly decapitated by cervical dislocation (3-month old males). Hippocampal slices were prepared and electrophysiology performed as previously described [88]. After a 50 min stable baseline, slices were bathed in 50 µM S-DHPG for 10 min to induce mGluR-LTD. A 2 min trace of an average of four 30 sec traces was recorded over 100 min post-drug application and the slope of the fEPSP was measured and graphed as a function of time.
Treatment, Staining and Immunofluorescence Analyses of Primary Neurons
For inhibitor treatments, cells were pretreated with vehicle, 2.5 µM MPEP or 40 µM anisomycin for 15 min prior to culture for 1 hr with vehicle or 20 nM Aβ1–42. Aβ1–42 (CalBiochem, catalog #171596) was prepared as previously described to generate oligomers, but not high molecular weight or fibrillar aggregates [89], [90]. For antibody treatments, 10 µg mouse IgG (Sigma #I5381) or anti-Aβ (Santa Cruz, catalog #28365LS) were added to 0.5 mL culture media inside transwells (Corning, catalog #3460, 0.4 µm pore size) that were situated above neuron-coated glass coverslips in 12-well tissue culture dishes. Each well contained 1 mL culture media and the transwell contained an additional 0.5 mL of culture media. Neurons were cultured for 3 days with the indicated antibodies prior to fixation and staining. Cells were stained overnight with: anti-22C11 against the amino-terminus of AβPP (Chemicon, catalog #MAB348, 1∶2000), anti-phosphERK (Santa Cruz, catalog #sc-23759, 1∶100), anti-Arc/Arg (Santa Cruz, catalog #sc-17839, 1∶100), anti-Map1B (Santa Cruz, catalog #58784, 1∶100), anti-RhoB (Santa Cruz, catalog #sc-180, 1∶100) and anti-PSD95 (Santa Cruz, catalog #sc-71935, 1∶100) followed by visualization with appropriate goat anti-mouse or anti-rabbit rhodamine-conjugated secondary antibodies (Invitrogen, 1∶500 for 30 min in the dark). Images were acquired with a Nikon C1 Laser Scanning Microscope (Nikon Eclipse E600 upright microscope) using the 543 Diode (1 mw Mellet Griot) laser, the Nikon Plan Apo 60×/1.40 oil objective with Zeiss Immersol™ 518F oil at ambient temperature, and Nikon EZ-C1, v3.91 software (Nikon Corp, Tokyo, Japan). Stained protein levels in the puncta of 4–7 dendrites per sample were quantitated with IMAGE J software using the Analyze Particles function (Rasband, W.S., Image J, U.S. National Institutes of Health, Bethesda, Maryland, USA, http://rsb.info.nih.gov/ij/, 1997–2006). Statistical significance was determined by one-way ANOVA and Student T-test analyses.
Blood Collection
Males with FXS and age-matched controls were recruited from the FXS Clinic at Rush University Medical Center (RUMC) in Chicago, IL. All FXS subjects (ages 9–32 years old) were positive by DNA analyses for a fully methylated expansion mutation in the FMR1 gene. Controls (age 23–33) were normal volunteers working at RUMC and had no history of cognitive or mental health disorders. The age and medications of the donors are listed in Table S1. Blood was drawn from donors into lithium heparin-coated blood collection tubes and spun at 1,500 rpm. The plasma supernatant was removed and frozen at −80°C. The anti-coagulated blood was mailed by overnight delivery from RUMC to the University of Wisconsin-Madison where PBMC were isolated within 24 hr.
Assessment of AβPP/AβPPα, Aβ1–40 and Aβ1–42 by ELISA
Plasma was thawed and clarified at 12,000 rpm for 10 min at 4°C prior to ELISA assays for AβPP/AβPPα, Aβ1–40 and Aβ1–42 per the manufacturer's instructions (BioSource #KHB0051, KHB3482, KHB3442) with the following modifications for the Aβ assays: (1) the sample volume was doubled from 50 µL to 100 µL, (2) the incubation time was extended from 3 hr to overnight at 4°C, and (3) after the overnight incubation, the samples were removed from the antibody-coated wells prior to addition of the detection antibody. PBMC were isolated as previously described [91] and cultured for 24 hr prior to harvesting the cells and culture media for ELISA analyses. Hippocampus and neocortex (pre and post central gyri) samples were sectioned from left cerebral hemispheres of control and FXS brain autopsy tissue. Detergent-soluble lysates were prepared as previously described) [11] for analyses of AβPP and Aβ1–40.
Statistical Analyses
One-way ANOVA was performed using GraphPad Prism version 5.0 d for Mac OS X (GraphPad Software, San Diego, CA) to compare the means of three or more unmatched groups for the behavioral and dendritic spine analyses. Student T-test analyses were used to quantitate statistical significance for the western blotting, marble burying, open field, dendritic spine protrusion length, immunofluoresence and ELISA data. Fisher exact tests were used to quantitate statistical significance for the AGS data. Two-way ANOVA with Bonferroni posthoc tests was used to quantitate statistical significance for the mGluR-LTD analyses.
Supporting Information
Assessment of hippocampal slice health. Hippocampal slices from WT (black circles), Fmr1KO (white circles), AppHET (black triangles) and Fmr1KO/AppHET (white triangles) mice exhibit equivalent synaptic transmission as determined by the input/output relationship (A) and ppf (B). i/o was also measured at the end of the recordings to assess slice health and showed similar i/o relationships to those shown in (A) (data not shown). (B) fEPSP size as percent of first stimulus versus interstimulus interval (msec). Data were analyzed by two-way ANOVA/Bonferroni multiple comparison analyses. There were no statistically significant differences in the i/o relationships. The WT ppfs were statistically different (p<0.05) from AppHET (many time points), WT versus Fmr1KO (50 msec time point); WT versus Fmr1KO/AppHET (first four time points). There were no other statistically significant differences in ppfs for the remaining datasets.
(TIFF)
MPEP and Aβ1–42 alter dendritic phosphoERK levels. (A) WT and Fmr1KO neurons were treated with 10 µM MPEP [one-way ANOVA p<0.05, F = 2.1], and (B) WT neurons were treated with 20 nM Aβ1–42 for the indicated times prior to fixation and staining with anti-phosphoERK [one-way ANOVA p<0.0001, F = 13]. Stars (★) denote statistically different results by Student T-test analyses (p<0.05).
(TIFF)
Age and medications of donors.
(XLS)
Acknowledgments
We especially thank the FXS patients and their families who participated in this study. Human autopsy brain tissue was obtained from the NICHD Brain and Tissue Bank for Developmental Disorders at the University of Maryland, Baltimore, MD. We thank Dr. Hui Zheng at Baylor College of Medicine, Houston, TX for the AppKO genotyping protocol, Dr. Matt Andrzejewski, Manager of the Waisman Center Behavioral Suite at the University of WI-Madison, WI, for advice with statistical analyses and behavioral testing, Dr. Dan Bolt at the University of WI-Madison for advice with statistical analyses, Dr. Rich Paylor at Baylor College of Medicine, Houston, TX for consultation on behavioral testing with Fmr1KO mice, and Dr. Erik Dent and Elliott Merriam at the University of WI-Madison for advice on dendritic spine length measurements.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: This work was supported by FRAXA Research Foundation (http://www.FRAXA.org) (C.J.W. and J.S.M.), the Illinois-Eastern Iowa Kiwanis Spastic Paralysis and Related Disorders Foundation (E.B.K.), National Institutes of Health Grants P30 HD03352 (Waisman Center) and R01DA026067 (J.S.M.) and University of WI start-up funds (C.B.). The funders had no role in data collection and analyses or decision to publish. Mike Tranfaglia from FRAXA Research Foundation assisted with study design and critical review of the manuscript.
References
- 1.Hagerman RJ, Hagerman PJ. Physical and behavioral phenotype. Baltimore: John Hopkins University Press; 2002. pp. 3–109. [Google Scholar]
- 2.Verkerk AJ, Pieretti M, Sutcliffe JS, Fu YH, Kuhl DP, et al. Identification of a gene (FMR-1) containing a CGG repeat coincident with a breakpoint cluster region exhibiting length variation in fragile X syndrome. Cell. 1991;65(5):905–914. doi: 10.1016/0092-8674(91)90397-h. [DOI] [PubMed] [Google Scholar]
- 3.Oberle I, Rousseau F, Heitz D, Kretz C, Devys D, et al. Instability of a 550-base pair DNA segment and abnormal methylation in fragile X syndrome. Science. 1991;252(5010):1097–1102. doi: 10.1126/science.252.5009.1097. [DOI] [PubMed] [Google Scholar]
- 4.Brown V, Jin P, Ceman S, Darnell JC, O'Donnell WT, et al. Microarray identification of FMRP-associated brain mRNAs and altered mRNA translational profiles in fragile X syndrome. Cell. 2001;107(4):477–487. doi: 10.1016/s0092-8674(01)00568-2. [DOI] [PubMed] [Google Scholar]
- 5.Miyashiro KY, Beckel-Mitchener A, Purk TP, Becker KG, Barret T, et al. RNA cargoes associating with FMRP reveal deficits in cellular functioning in Fmr1 null mice. Neuron. 2003;37(3):417–431. doi: 10.1016/s0896-6273(03)00034-5. [DOI] [PubMed] [Google Scholar]
- 6.Zalfa F, Giorgi M, Primerano B, Moro A, Di Penta A, et al. The fragile X syndrome protein FMRP associates with BC1 RNA and regulates the translation of specific mRNAs at synapses. Cell. 2003;112(3):317–327. doi: 10.1016/s0092-8674(03)00079-5. [DOI] [PubMed] [Google Scholar]
- 7.Laggerbauer B, Ostareck D, Keidel EM, Ostareck-Lederer A, Fischer U. Evidence that fragile X mental retardation protein is a negative regulator of translation. Hum Mol Genet. 2001;10(4):329–338. doi: 10.1093/hmg/10.4.329. [DOI] [PubMed] [Google Scholar]
- 8.Li Z, Zhang Y, Ku L, Wilkinson KD, Warren ST, et al. The fragile X mental retardation protein inhibits translation via interacting with mRNA. Nucleic Acids Res. 2001;29(11):2276–2283. doi: 10.1093/nar/29.11.2276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mazroui R, Huot ME, Tremblay S, Filion C, Labelle Y, et al. Trapping of messenger RNA by fragile X mental retardation protein into cytoplasmic granules induces translation repression. Hum Mol Genet. 2002;11(24):3007–3017. doi: 10.1093/hmg/11.24.3007. [DOI] [PubMed] [Google Scholar]
- 10.Bagni C, Greenough WT. From mRNP trafficking to spine dysmorphogenesis: The roots of fragile X syndrome. Nat Rev Neurosci. 2005;6(5):376–387. doi: 10.1038/nrn1667. [DOI] [PubMed] [Google Scholar]
- 11.Westmark CJ, Malter JS. FMRP mediates mGluR5-dependent translation of amyloid precursor protein. PLoS Biol. 2007;5(3):e52. doi: 10.1371/journal.pbio.0050052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.D'Agata V, Warren ST, Zhao W, Torre ER, Alkon DL, et al. Gene expression profiles in a transgenic animal model of fragile X syndrome. Neurobiol Dis. 2002;10(3):211–218. doi: 10.1006/nbdi.2002.0506. [DOI] [PubMed] [Google Scholar]
- 13.Rudelli RD, Brown WT, Wisniewski K, Jenkins EC, Laure-Kamionowska M, et al. Adult fragile X syndrome. clinico-neuropathologic findings. Acta Neuropathol. 1985;67(3–4):289–295. doi: 10.1007/BF00687814. [DOI] [PubMed] [Google Scholar]
- 14.Wisniewski KE, Segan SM, Miezejeski CM, Sersen EA, Rudelli RD. The fra(X) syndrome: Neurological, electrophysiological, and neuropathological abnormalities. Am J Med Genet. 1991;38(2–3):476–480. doi: 10.1002/ajmg.1320380267. [DOI] [PubMed] [Google Scholar]
- 15.Hinton VJ, Brown WT, Wisniewski K, Rudelli RD. Analysis of neocortex in three males with the fragile X syndrome. Am J Med Genet. 1991;41(3):289–294. doi: 10.1002/ajmg.1320410306. [DOI] [PubMed] [Google Scholar]
- 16.Sokol DK, Chen D, Farlow MR, Dunn DW, Maloney B, et al. High levels of Alzheimer beta-amyloid precursor protein (APP) in children with severely autistic behavior and aggression. J Child Neurol. 2006;21(6):444–449. doi: 10.1177/08830738060210062201. [DOI] [PubMed] [Google Scholar]
- 17.Bailey AR, Giunta BN, Obregon D, Nikolic WV, Tian J, et al. Peripheral biomarkers in autism: Secreted amyloid precursor protein-alpha as a probable key player in early diagnosis. Int J Clin Exp Med. 2008;1(4):338–344. [PMC free article] [PubMed] [Google Scholar]
- 18.Clifford S, Dissanayake C, Bui QM, Huggins R, Taylor AK, et al. Autism spectrum phenotype in males and females with fragile X full mutation and premutation. J Autism Dev Disord. 2007;37(4):738–747. doi: 10.1007/s10803-006-0205-z. [DOI] [PubMed] [Google Scholar]
- 19.Kent L, Evans J, Paul M, Sharp M. Comorbidity of autistic spectrum disorders in children with Down syndrome. Dev Med Child Neurol. 1999;41(3):153–158. doi: 10.1017/s001216229900033x. [DOI] [PubMed] [Google Scholar]
- 20.Chen L, Toth M. Fragile X mice develop sensory hyperreactivity to auditory stimuli. Neuroscience. 2001;103(4):1043–1050. doi: 10.1016/s0306-4522(01)00036-7. [DOI] [PubMed] [Google Scholar]
- 21.Yan QJ, Asafo-Adjei PK, Arnold HM, Brown RE, Bauchwitz RP. A phenotypic and molecular characterization of the fmr1-tm1Cgr fragile X mouse. Genes Brain Behav. 2004;3(6):337–359. doi: 10.1111/j.1601-183X.2004.00087.x. [DOI] [PubMed] [Google Scholar]
- 22.Yan QJ, Rammal M, Tranfaglia M, Bauchwitz RP. Suppression of two major fragile X syndrome mouse model phenotypes by the mGluR5 antagonist MPEP. Neuropharmacology. 2005;49(7):1053–1066. doi: 10.1016/j.neuropharm.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 23.Qin M, Kang J, Smith CB. A null mutation for Fmr1 in female mice: Effects on regional cerebral metabolic rate for glucose and relationship to behavior. Neuroscience. 2005;135(3):999–1009. doi: 10.1016/j.neuroscience.2005.06.081. [DOI] [PubMed] [Google Scholar]
- 24.Bilousova TV, Dansie L, Ngo M, Aye J, Charles JR, et al. Minocycline promotes dendritic spine maturation and improves behavioural performance in the fragile X mouse model. J Med Genet. 2009;46(2):94–102. doi: 10.1136/jmg.2008.061796. [DOI] [PubMed] [Google Scholar]
- 25.Antar LN, Li C, Zhang H, Carroll RC, Bassell GJ. Local functions for FMRP in axon growth cone motility and activity-dependent regulation of filopodia and spine synapses. Mol Cell Neurosci. 2006;32(1–2):37–48. doi: 10.1016/j.mcn.2006.02.001. [DOI] [PubMed] [Google Scholar]
- 26.de Vrij FM, Levenga J, van der Linde HC, Koekkoek SK, De Zeeuw CI, et al. Rescue of behavioral phenotype and neuronal protrusion morphology in Fmr1 KO mice. Neurobiol Dis. 2008;31(1):127–132. doi: 10.1016/j.nbd.2008.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Berry-Kravis E. Epilepsy in fragile X syndrome. Dev Med Child Neurol. 2002;44(11):724–728. doi: 10.1017/s0012162201002833. [DOI] [PubMed] [Google Scholar]
- 28.Musumeci SA, Hagerman RJ, Ferri R, Bosco P, Dalla Bernardina B, et al. Epilepsy and EEG findings in males with fragile X syndrome. Epilepsia. 1999;40(8):1092–1099. doi: 10.1111/j.1528-1157.1999.tb00824.x. [DOI] [PubMed] [Google Scholar]
- 29.Bear MF, Huber KM, Warren ST. The mGluR theory of fragile X mental retardation. Trends Neurosci. 2004;27(7):370–377. doi: 10.1016/j.tins.2004.04.009. [DOI] [PubMed] [Google Scholar]
- 30.McBride SM, Choi CH, Wang Y, Liebelt D, Braunstein E, et al. Pharmacological rescue of synaptic plasticity, courtship behavior, and mushroom body defects in a drosophila model of fragile X syndrome. Neuron. 2005;45(5):753–764. doi: 10.1016/j.neuron.2005.01.038. [DOI] [PubMed] [Google Scholar]
- 31.Dolen G, Osterweil E, Rao BS, Smith GB, Auerbach BD, et al. Correction of fragile X syndrome in mice. Neuron. 2007;56(6):955–962. doi: 10.1016/j.neuron.2007.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Thomas A, Burant A, Bui N, Graham D, Yuva-Paylor LA, et al. Marble burying reflects a repetitive and perseverative behavior more than novelty-induced anxiety. Psychopharmacology (Berl) 2009;204(2):361–373. doi: 10.1007/s00213-009-1466-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Irwin SA, Patel B, Idupulapati M, Harris JB, Crisostomo RA, et al. Abnormal dendritic spine characteristics in the temporal and visual cortices of patients with fragile-X syndrome: A quantitative examination. Am J Med Genet. 2001;98(2):161–167. doi: 10.1002/1096-8628(20010115)98:2<161::aid-ajmg1025>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 34.Huber KM, Gallagher SM, Warren ST, Bear MF. Altered synaptic plasticity in a mouse model of fragile X mental retardation. Proc Natl Acad Sci U S A. 2002;99(11):7746–7750. doi: 10.1073/pnas.122205699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Huber KM, Kayser MS, Bear MF. Role for rapid dendritic protein synthesis in hippocampal mGluR-dependent long-term depression. Science. 2000;288(5469):1254–1257. doi: 10.1126/science.288.5469.1254. [DOI] [PubMed] [Google Scholar]
- 36.Dolen G, Bear MF. Role for metabotropic glutamate receptor 5 (mGluR5) in the pathogenesis of fragile X syndrome. J Physiol. 2008;586(6):1503–1508. doi: 10.1113/jphysiol.2008.150722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Torroja L, Packard M, Gorczyca M, White K, Budnik V. The drosophila beta-amyloid precursor protein homolog promotes synapse differentiation at the neuromuscular junction. J Neurosci. 1999;19(18):7793–7803. doi: 10.1523/JNEUROSCI.19-18-07793.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mucke L, Masliah E, Johnson WB, Ruppe MD, Alford M, et al. Synaptotrophic effects of human amyloid beta protein precursors in the cortex of transgenic mice. Brain Res. 1994;666(2):151–167. doi: 10.1016/0006-8993(94)90767-6. [DOI] [PubMed] [Google Scholar]
- 39.Hung AY, Koo EH, Haass C, Selkoe DJ. Increased expression of beta-amyloid precursor protein during neuronal differentiation is not accompanied by secretory cleavage. Proc Natl Acad Sci U S A. 1992;89(20):9439–9443. doi: 10.1073/pnas.89.20.9439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Loffler J, Huber G. Beta-amyloid precursor protein isoforms in various rat brain regions and during brain development. J Neurochem. 1992;59(4):1316–1324. doi: 10.1111/j.1471-4159.1992.tb08443.x. [DOI] [PubMed] [Google Scholar]
- 41.Masliah E, Mallory M, Ge N, Saitoh T. Amyloid precursor protein is localized in growing neurites of neonatal rat brain. Brain Res. 1992;593(2):323–328. doi: 10.1016/0006-8993(92)91329-d. [DOI] [PubMed] [Google Scholar]
- 42.Moya KL, Benowitz LI, Schneider GE, Allinquant B. The amyloid precursor protein is developmentally regulated and correlated with synaptogenesis. Dev Biol. 1994;161(2):597–603. doi: 10.1006/dbio.1994.1055. [DOI] [PubMed] [Google Scholar]
- 43.Berardi N, Pizzorusso T, Maffei L. Critical periods during sensory development. Curr Opin Neurobiol. 2000;10(1):138–145. doi: 10.1016/s0959-4388(99)00047-1. [DOI] [PubMed] [Google Scholar]
- 44.Lu R, Wang H, Liang Z, Ku L, O'donnell WT, et al. The fragile X protein controls microtubule-associated protein 1B translation and microtubule stability in brain neuron development. Proc Natl Acad Sci U S A. 2004;101(42):15201–15206. doi: 10.1073/pnas.0404995101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Masters CL, Simms G, Weinman NA, Multhaup G, McDonald BL, et al. Amyloid plaque core protein in Alzheimer disease and Down syndrome. Proc Natl Acad Sci U S A. 1985;82(12):4245–4249. doi: 10.1073/pnas.82.12.4245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kamenetz F, Tomita T, Hsieh H, Seabrook G, Borchelt D, et al. APP processing and synaptic function. Neuron. 2003;37(6):925–937. doi: 10.1016/s0896-6273(03)00124-7. [DOI] [PubMed] [Google Scholar]
- 47.Lacor PN, Buniel MC, Chang L, Fernandez SJ, Gong Y, et al. Synaptic targeting by Alzheimer's-related amyloid beta oligomers. J Neurosci. 2004;24(45):10191–10200. doi: 10.1523/JNEUROSCI.3432-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Beyreuther K, Pollwein P, Multhaup G, Monning U, Konig G, et al. Regulation and expression of the Alzheimer's beta/A4 amyloid protein precursor in health, disease, and Down 's syndrome. Ann N Y Acad Sci. 1993;695:91–102. doi: 10.1111/j.1749-6632.1993.tb23035.x. [DOI] [PubMed] [Google Scholar]
- 49.Wisniewski KE, Wisniewski HM, Wen GY. Occurrence of neuropathological changes and dementia of Alzheimer's disease in Down's syndrome. Ann Neurol. 1985;17(3):278–282. doi: 10.1002/ana.410170310. [DOI] [PubMed] [Google Scholar]
- 50.Kaufmann WE, Moser HW. Dendritic anomalies in disorders associated with mental retardation. Cereb Cortex. 2000;10(10):981–991. doi: 10.1093/cercor/10.10.981. [DOI] [PubMed] [Google Scholar]
- 51.Westmark CJ, Malter JS. Translating memories: The role of protein biosynthesis in synaptic plasticity. New York: Nova Science Publishers, Inc; 2009. 29 [Google Scholar]
- 52.Graff-Radford NR, Crook JE, Lucas J, Boeve BF, Knopman DS, et al. Association of low plasma Abeta42/Abeta40 ratios with increased imminent risk for mild cognitive impairment and Alzheimer disease. Arch Neurol. 2007;64(3):354–362. doi: 10.1001/archneur.64.3.354. [DOI] [PubMed] [Google Scholar]
- 53.van Oijen M, Hofman A, Soares HD, Koudstaal PJ, Breteler MM. Plasma abeta(1–40) and abeta(1–42) and the risk of dementia: A prospective case-cohort study. Lancet Neurol. 2006;5(8):655–660. doi: 10.1016/S1474-4422(06)70501-4. [DOI] [PubMed] [Google Scholar]
- 54.Sobow T, Flirski M, Kloszewska I, Liberski PP. Plasma levels of alpha beta peptides are altered in amnestic mild cognitive impairment but not in sporadic Alzheimer's disease. Acta Neurobiol Exp (Wars) 2005;65(2):117–124. doi: 10.55782/ane-2005-1544. [DOI] [PubMed] [Google Scholar]
- 55.Schupf N, Tang MX, Fukuyama H, Manly J, Andrews H, et al. Peripheral abeta subspecies as risk biomarkers of Alzheimer's disease. Proc Natl Acad Sci U S A. 2008;105(37):14052–14057. doi: 10.1073/pnas.0805902105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ringman JM, Younkin SG, Pratico D, Seltzer W, Cole GM, et al. Biochemical markers in persons with preclinical familial Alzheimer disease. Neurology. 2008;71(2):85–92. doi: 10.1212/01.wnl.0000303973.71803.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mehta PD, Pirttila T, Mehta SP, Sersen EA, Aisen PS, et al. Plasma and cerebrospinal fluid levels of amyloid beta proteins 1–40 and 1–42 in Alzheimer disease. Arch Neurol. 2000;57(1):100–105. doi: 10.1001/archneur.57.1.100. [DOI] [PubMed] [Google Scholar]
- 58.Hansson O, Zetterberg H, Blennow K. Evaluation of plasma Abeta40 and Abeta42 as predictors of conversion to Alzheimer's disease in patients with mild cognitive impairment. Neurobiol Aging. 2008 doi: 10.1016/j.neurobiolaging.2008.03.027. [DOI] [PubMed] [Google Scholar]
- 59.Assini A, Cammarata S, Vitali A, Colucci M, Giliberto L, et al. Plasma levels of amyloid beta-protein 42 are increased in women with mild cognitive impairment. Neurology. 2004;63(5):828–831. doi: 10.1212/01.wnl.0000137040.64252.ed. [DOI] [PubMed] [Google Scholar]
- 60.Schupf N, Patel B, Pang D, Zigman WB, Silverman W, et al. Elevated plasma beta-amyloid peptide abeta(42) levels, incident dementia, and mortality in Down syndrome. Arch Neurol. 2007;64(7):1007–1013. doi: 10.1001/archneur.64.7.1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mehta PD, Capone G, Jewell A, Freedland RL. Increased amyloid beta protein levels in children and adolescents with Down syndrome. J Neurol Sci. 2007;254(1–2):22–27. doi: 10.1016/j.jns.2006.12.010. [DOI] [PubMed] [Google Scholar]
- 62.Berry-Kravis E, Sklena P. Demonstration of abnormal cyclic AMP production in platelets from patients with fragile X syndrome. Am J Med Genet. 1993;45(1):81–87. doi: 10.1002/ajmg.1320450120. [DOI] [PubMed] [Google Scholar]
- 63.Weng N, Weiler IJ, Sumis A, Berry-Kravis E, Greenough WT. Early-phase ERK activation as a biomarker for metabolic status in fragile X syndrome. Am J Med Genet B Neuropsychiatr Genet. 2008;147B(7):1253–1257. doi: 10.1002/ajmg.b.30765. [DOI] [PubMed] [Google Scholar]
- 64.Mayeux R, Honig LS, Tang MX, Manly J, Stern Y, et al. Plasma A[beta]40 and A[beta]42 and Alzheimer's disease: Relation to age, mortality, and risk. Neurology. 2003;61(9):1185–1190. doi: 10.1212/01.wnl.0000091890.32140.8f. [DOI] [PubMed] [Google Scholar]
- 65.Kuo YM, Emmerling MR, Vigo-Pelfrey C, Kasunic TC, Kirkpatrick JB, et al. Water-soluble abeta (N-40, N-42) oligomers in normal and Alzheimer disease brains. J Biol Chem. 1996;271(8):4077–4081. doi: 10.1074/jbc.271.8.4077. [DOI] [PubMed] [Google Scholar]
- 66.Hagerman RJ, Hills J, Scharfenaker S, Lewis H. Fragile X syndrome and selective mutism. Am J Med Genet. 1999;83(4):313–317. [PubMed] [Google Scholar]
- 67.Merenstein SA, Sobesky WE, Taylor AK, Riddle JE, Tran HX, et al. Molecular-clinical correlations in males with an expanded FMR1 mutation. Am J Med Genet. 1996;64(2):388–394. doi: 10.1002/(SICI)1096-8628(19960809)64:2<388::AID-AJMG31>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 68.Frankland PW, Wang Y, Rosner B, Shimizu T, Balleine BW, et al. Sensorimotor gating abnormalities in young males with fragile X syndrome and Fmr1-knockout mice. Mol Psychiatry. 2004;9(4):417–425. doi: 10.1038/sj.mp.4001432. [DOI] [PubMed] [Google Scholar]
- 69.Miller LJ, McIntosh DN, McGrath J, Shyu V, Lampe M, et al. Electrodermal responses to sensory stimuli in individuals with fragile X syndrome: A preliminary report. Am J Med Genet. 1999;83(4):268–279. [PubMed] [Google Scholar]
- 70.Westmark CJ, Westmark PR, Malter JS. Alzheimer's disease and Down syndrome rodent models exhibit audiogenic seizures. J Alzheimers Dis. 2010;20(4):1009–13. doi: 10.3233/JAD-2010-100087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wallberg A, Nilsson K, Osterlund K, Peterson A, Elg S, et al. Phenyl ureas of creatinine as mGluR5 antagonists. A structure-activity relationship study of fenobam analogues. Bioorg Med Chem Lett. 2006;16(5):1142–1145. doi: 10.1016/j.bmcl.2005.11.092. [DOI] [PubMed] [Google Scholar]
- 72.Porter RH, Jaeschke G, Spooren W, Ballard TM, Buttelmann B, et al. Fenobam: A clinically validated nonbenzodiazepine anxiolytic is a potent, selective, and noncompetitive mGlu5 receptor antagonist with inverse agonist activity. J Pharmacol Exp Ther. 2005;315(2):711–721. doi: 10.1124/jpet.105.089839. [DOI] [PubMed] [Google Scholar]
- 73.Familian A, Boshuizen RS, Eikelenboom P, Veerhuis R. Inhibitory effect of minocycline on amyloid beta fibril formation and human microglial activation. Glia. 2006;53(3):233–240. doi: 10.1002/glia.20268. [DOI] [PubMed] [Google Scholar]
- 74.Ryu JK, Franciosi S, Sattayaprasert P, Kim SU, McLarnon JG. Minocycline inhibits neuronal death and glial activation induced by beta-amyloid peptide in rat hippocampus. Glia. 2004;48(1):85–90. doi: 10.1002/glia.20051. [DOI] [PubMed] [Google Scholar]
- 75.Henriques AG, Vieira SI, da Cruz E Silva EF, da Cruz E Silva OA. Abeta promotes Alzheimer's disease-like cytoskeleton abnormalities with consequences to APP processing in neurons. J Neurochem. 2010;113(3):761–771. doi: 10.1111/j.1471-4159.2010.06643.x. [DOI] [PubMed] [Google Scholar]
- 76.Li S, Hong S, Shepardson NE, Walsh DM, Shankar GM, et al. Soluble oligomers of amyloid beta protein facilitate hippocampal long-term depression by disrupting neuronal glutamate uptake. Neuron. 2009;62(6):788–801. doi: 10.1016/j.neuron.2009.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Shankar GM, Li S, Mehta TH, Garcia-Munoz A, Shepardson NE, et al. Amyloid-beta protein dimers isolated directly from Alzheimer's brains impair synaptic plasticity and memory. Nat Med. 2008;14(8):837–842. doi: 10.1038/nm1782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lambert MP, Barlow AK, Chromy BA, Edwards C, Freed R, et al. Diffusible, nonfibrillar ligands derived from Abeta1–42 are potent central nervous system neurotoxins. Proc Natl Acad Sci U S A. 1998;95(11):6448–6453. doi: 10.1073/pnas.95.11.6448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Walsh DM, Klyubin I, Fadeeva JV, Cullen WK, Anwyl R, et al. Naturally secreted oligomers of amyloid beta protein potently inhibit hippocampal long-term potentiation in vivo. Nature. 2002;416(6880):535–539. doi: 10.1038/416535a. [DOI] [PubMed] [Google Scholar]
- 80.Wang HW, Pasternak JF, Kuo H, Ristic H, Lambert MP, et al. Soluble oligomers of beta amyloid (1–42) inhibit long-term potentiation but not long-term depression in rat dentate gyrus. Brain Res. 2002;924(2):133–140. doi: 10.1016/s0006-8993(01)03058-x. [DOI] [PubMed] [Google Scholar]
- 81.Wang Q, Walsh DM, Rowan MJ, Selkoe DJ, Anwyl R. Block of long-term potentiation by naturally secreted and synthetic amyloid beta-peptide in hippocampal slices is mediated via activation of the kinases c-jun N-terminal kinase, cyclin-dependent kinase 5, and p38 mitogen-activated protein kinase as well as metabotropic glutamate receptor type 5. J Neurosci. 2004;24(13):3370–3378. doi: 10.1523/JNEUROSCI.1633-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Blanchard BJ, Thomas VL, Ingram VM. Mechanism of membrane depolarization caused by the Alzheimer Abeta1–42 peptide. Biochem Biophys Res Commun. 2002;293(4):1197–1203. doi: 10.1016/S0006-291X(02)00346-7. [DOI] [PubMed] [Google Scholar]
- 83.Renner M, Lacor PN, Velasco PT, Xu J, Contractor A, et al. Deleterious effects of amyloid beta oligomers acting as an extracellular scaffold for mGluR5. Neuron. 2010;66(5):739–754. doi: 10.1016/j.neuron.2010.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Almeida CG, Tampellini D, Takahashi RH, Greengard P, Lin MT, et al. Beta-amyloid accumulation in APP mutant neurons reduces PSD-95 and GluR1 in synapses. Neurobiol Dis. 2005;20(2):187–198. doi: 10.1016/j.nbd.2005.02.008. [DOI] [PubMed] [Google Scholar]
- 85.Le W, Xie WJ, Nyormoi O, Ho BK, Smith RG, et al. Beta-Amyloid1–40 increases expression of beta-amyloid precursor protein in neuronal hybrid cells. J Neurochem. 1995;65(5):2373–2376. doi: 10.1046/j.1471-4159.1995.65052373.x. [DOI] [PubMed] [Google Scholar]
- 86.[Anonymous] Fmr1 knockout mice: A model to study fragile X mental retardation. the dutch-belgian fragile X consortium. Cell. 1994;78(1):23–33. [PubMed] [Google Scholar]
- 87.Zheng H, Jiang M, Trumbauer ME, Sirinathsinghji DJ, Hopkins R, et al. Beta-amyloid precursor protein-deficient mice show reactive gliosis and decreased locomotor activity. Cell. 1995;81(4):525–531. doi: 10.1016/0092-8674(95)90073-x. [DOI] [PubMed] [Google Scholar]
- 88.O'Riordan KJ, Huang IC, Pizzi M, Spano P, Boroni F, et al. Regulation of nuclear factor kappaB in the hippocampus by group I metabotropic glutamate receptors. J Neurosci. 2006;26(18):4870–4879. doi: 10.1523/JNEUROSCI.4527-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Serrano F, Chang A, Hernandez C, Pautler RG, Sweatt JD, et al. NADPH oxidase mediates beta-amyloid peptide-induced activation of ERK in hippocampal organotypic cultures. Mol Brain. 2009;2(1):31. doi: 10.1186/1756-6606-2-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Bell KA, O'Riordan KJ, Sweatt JD, Dineley KT. MAPK recruitment by beta-amyloid in organotypic hippocampal slice cultures depends on physical state and exposure time. J Neurochem. 2004;91(2):349–361. doi: 10.1111/j.1471-4159.2004.02722.x. [DOI] [PubMed] [Google Scholar]
- 91.Westmark CJ, Malter JS. Extracellular-regulated kinase controls beta-amyloid precursor protein mRNA decay. Brain Res Mol Brain Res. 2001;90(2):193–201. doi: 10.1016/s0169-328x(01)00112-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Assessment of hippocampal slice health. Hippocampal slices from WT (black circles), Fmr1KO (white circles), AppHET (black triangles) and Fmr1KO/AppHET (white triangles) mice exhibit equivalent synaptic transmission as determined by the input/output relationship (A) and ppf (B). i/o was also measured at the end of the recordings to assess slice health and showed similar i/o relationships to those shown in (A) (data not shown). (B) fEPSP size as percent of first stimulus versus interstimulus interval (msec). Data were analyzed by two-way ANOVA/Bonferroni multiple comparison analyses. There were no statistically significant differences in the i/o relationships. The WT ppfs were statistically different (p<0.05) from AppHET (many time points), WT versus Fmr1KO (50 msec time point); WT versus Fmr1KO/AppHET (first four time points). There were no other statistically significant differences in ppfs for the remaining datasets.
(TIFF)
MPEP and Aβ1–42 alter dendritic phosphoERK levels. (A) WT and Fmr1KO neurons were treated with 10 µM MPEP [one-way ANOVA p<0.05, F = 2.1], and (B) WT neurons were treated with 20 nM Aβ1–42 for the indicated times prior to fixation and staining with anti-phosphoERK [one-way ANOVA p<0.0001, F = 13]. Stars (★) denote statistically different results by Student T-test analyses (p<0.05).
(TIFF)
Age and medications of donors.
(XLS)