Abstract
Objective
To systematically examine the relationship between sleep duration and subsequent weight gain in observational longitudinal human studies
Methods
Systematic review of twenty longitudinal studies published from 2004-October 31, 2010
Results
While adult studies (n=13) reported inconsistent results on the relationship between sleep duration and subsequent weight gain, studies with children (n=7) more consistently reported a positive relationship between short sleep duration and weight gain.
Conclusion
While shorter sleep duration consistently predicts subsequent weight gain in children, the relationship is not clear in adults. We discuss possible limitations of the current studies: 1.) the diminishing association between short sleep duration on weight gain over time after transition to short sleep, 2.) lack of inclusion of appropriate confounding, mediating, and moderating variables (i.e. sleep complaints and sedentary behavior), and 3.) measurement issues.
Keywords: sleep, obesity, weight gain, longitudinal studies
Introduction
According to the Centers for Disease Control and Prevention (CDC) more than one-third of adults and 17% of children in the United States (U.S.) are obese; in the past three decades, obesity rates for adults doubled while rates for children tripled (1). To stem this epidemic, the CDC recommends regular physical activity and healthy nutritional practices. A growing body of evidence points to another important risk factor for both weight gain and obesity: getting too little sleep (2, 3).
Previous literature reviews and meta-analyses have reported significant associations between sleep duration and obesity (2–9). These reviews indicate that there is evidence to suggest that sleep duration is associated with being overweight and/or experiencing weight gain over time. The majority of review conclusions support Nielsen, et al. (7) who state that “short sleep duration is consistently associated with development of obesity in children and young adults, but not consistently so in older adults”.
There are multiple mechanisms through which sleep deprivation is hypothesized to have a causal link with weight gain. First, there is experimental evidence at the physiologic level. Evidence indicates short sleep may result in hormonal and metabolic changes contributing to weight gain and obesity (10–13). For example, studies of young healthy men found sleep curtailment was associated with increased ghrelin levels and decreased leptin levels, corresponding to increased hunger and appetite (11, 14). Suppressed leptin levels (10, 12, 14) and elevated ghrelin levels (10, 14) related to short sleep duration have been confirmed by other studies. Also, an association between sleep deprivation and thermoregulation decreases the available energy expenditure and is related to increased food intake (15). In addition, short sleep duration has been associated with fatigue and reduced physical activity, a source of reduced caloric expenditure (16). And finally, being awake longer gives one more opportunity to eat, coupled with the fact that sleep deprivation may affect choices about food quality. While there is evidence that meal intake remains stable among sleep durations, sleep restriction is associated with an increased consumption of calories from snacks prior to bedtime (17) and an average daily increase in calories consumed from fat (18).
Media use (e.g., television, video games, computers) has grown dramatically in the U.S., which has also been associated with short sleep and obesity. With 24-hour media availability, the amount of time spent with entertainment media has risen, especially among youth (19, 20). In 2009 U.S. children aged 8–18 spent 7 hours and 38 minutes per day using entertainment media (21). Of those aged 8–18, 71% have a television in their bedroom, 50% have a game console in their bedroom (20), 33% have internet access in their bedroom, which makes parental monitoring difficult and may have direct effects on nighttime sleep schedules (20, 21).
Short sleep duration is a known risk factor for overweight (22) and obesity (23), and media use is associated with both short sleep and obesity in infants, children, and adolescents around the world (22–28). Taveras et al. (22) report that a combination of short sleep duration and high levels of television in infants predict a 17% probability of overweight in 3 years, more than twice the predicted probability of having either short sleep duration or high levels of television alone. Infant television and video viewing is associated with shorter sleep duration at age 1 and 2 years (25). Ortega, et al. (26) found that insufficient sleep and ≥3 hours/day television watching were significantly associated among adolescents in Spain. Vioque, et al. (23) found that people aged 15 years and older in Spain who watched television ≥4 hours a day were significantly more likely to be obese compared to those who watched ≤1 hour per day. Gortmaker, et al. (27) observed a strong dose-response relationship between the prevalence of overweight and the hours of television viewed. A randomized controlled trial found that relative to controls, an intervention group receiving instruction on reducing television, videotape and video game use had statistically significant decreases in children’s reported television viewing and statistically significant relative decreases in BMI, concluding that reducing media use may be a promising approach towards preventing childhood obesity (28).
As with the relationship between sleep duration and all-cause mortality (29, 30), some studies of adults have found that both short and long sleeping are associated with weight gain. Regarding the u-shaped curves, the proposed mechanisms behind an association between long sleep duration and weight gain are at least partially distinct from those of short sleep (9). For example, weight gain among the longer sleepers may be related to less physical activity among the long sleepers or other third factors such as co-morbidities.
Challenges in Interpreting the Results from Previous Studies on Sleep Duration and Weight Gain
There are numerous challenges in comparing the various associations between short sleep and weight gain across studies (2). First, the definition of short sleep measured in hours across studies is far from standard, with “short sleep” measurement varying from “two to four hours” per night in adults (31) to “less than eleven hours” per night in five-year old children (32). In addition, the inclusion of confounding variables varies widely among studies (2, 4–6). Finally, the majority of studies to date have been cross-sectional, limiting the ability to infer causal relationships (2–9). For starters, cross-sectional correlations may be capturing reverse causation – for example, excess weight may be the underlying cause of the short sleeping, through obstructive sleep apnea. (33). Secondly, there may be other potentially confounding, mediating, or moderating variables that are related to both short sleep duration and excess weight (i.e. depression, long hours using media, etc).
In our systematic literature review, we will only include studies that include longitudinal data on the association between sleep duration and subsequent weight gain over time. While there still may be limitations of the various studies included, the exclusion of cross-sectional studies will strengthen our ability to assess a causal association by reducing the influences of reverse causation.
Methods
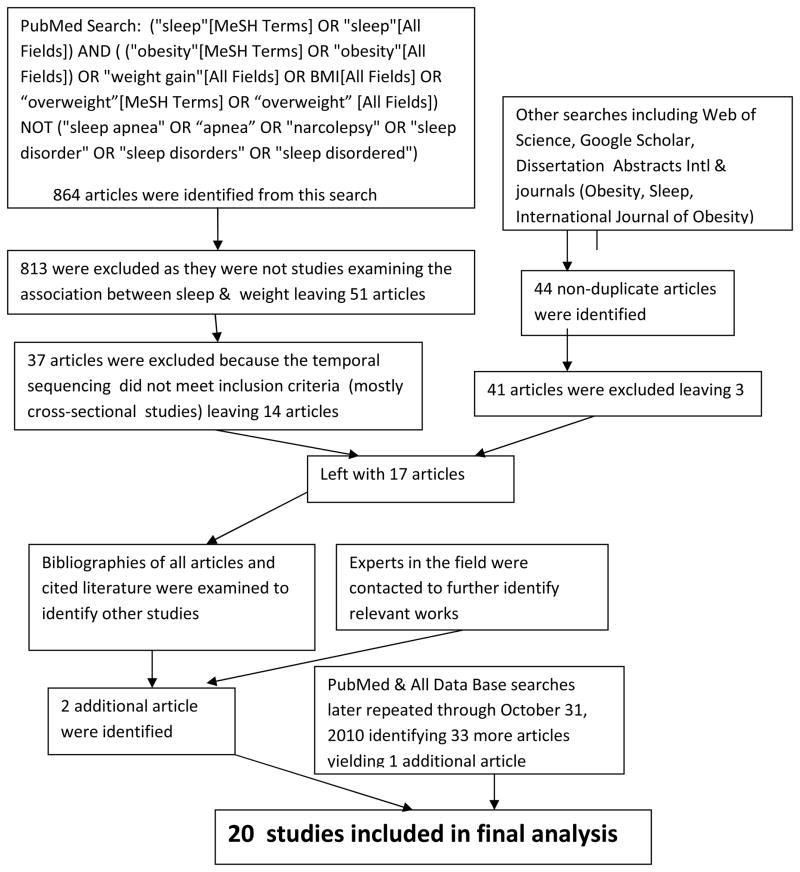
We performed a systematic literature search in PubMed for relevant original publications meeting the following criteria from 1990 through June 21, 2010 to identify original publications: (“sleep”[MeSH Terms] OR “sleep”[All Fields]) AND ( (“obesity”[MeSH Terms] OR “obesity”[All Fields]) OR “weight gain”[All Fields] OR “BMI”[All Fields] OR “overweight”[MeSH Terms] OR “overweight” [All Fields]) NOT (“sleep apnea” OR “apnea” OR “narcolepsy” OR “sleep disorder” OR “sleep disorders” OR “sleep disordered”). 864 abstracts from the initial search were reviewed, with 14 studies being identified as meeting inclusion/exclusion criteria. Searches in Web of Science, Google Scholar, Dissertation Abstracts International and various journals (Obesity, Sleep, International Journal of Obesity) identified 44 articles not duplicated in the PubMed search; 41 of these were excluded yielding 3 more articles. Bibliographies and cited literature were examined, and experts in the field were contacted to identify missing relevant works, yielding 2 more articles. A later PubMed search with the same criteria as above was performed through October 31, 2010, yielding 1 more article. The total of original articles included in the study is 20. Inclusion of studies was through discussion and consensus of authors.
Inclusion and Exclusion Criteria
This review is limited to studies which are longitudinal and are examining associations between short sleep duration and subsequent weight gain, and is not limited to any geographical area, age, or gender.
Where data from the same cohort were present in more than one study, only the most relevant article was included, and three articles were excluded for this reason (34–36). We excluded two examined articles (37, 38) that used longitudinal analyses to investigate the relationship between sleep duration and weight gain because the measure of sleep duration came at the end of the longitudinal period rather than at the beginning. We excluded another study because it measured the effect of BMI during childhood on sleep duration change (39).
Studies were divided into those that examined adults and those that examined children (i.e. if the sleep measurements and the baseline weight measurement occurred in the first 18 years of the subject’s life).
Results
In total, we reviewed 20 longitudinal studies. While adult studies (n=13) reported inconsistent results on the association between sleep duration and subsequent weight gain, studies with children (n=7) consistently reported a negative association between sleep duration and subsequent weight gain.
Table 1 summarizes the identified 13 adult studies. Four found an association between short sleep and weight gain but no association between long sleep and weight gain (16, 40–42). Four found an association between both short sleep and weight gain and long sleep and weight gain, or u-shaped association (43–46), and five studies found no significant association between sleep and subsequent weight gain (31, 47–50). One of these studies which found no association (47) is the only adult study conducted using objectively-measured sleep duration (actigraphy).
Table 1.
Adult Studies
| First Author & Publication Year | Data Source | Sample Size for Analysis | Age at Baseline Weight | Follow-up Period | Country | Sleep Duration Variable | Association between Sleep Duration & Weight Gain | Results |
|---|---|---|---|---|---|---|---|---|
| Chaput 2008 (43) | Quebec Family Study | 276 males & females | 21–64 years | 6 years | Canada | Self-Report | Significant U-shaped | Those who slept 5–6 hours gained 1.84 kg more (95% CI: 1.13–2.62) and those who slept 9–10 hours gained 1.49 kg more (95% CI: 0.92–2.48) than those who slept 7–8 hours. Those sleeping 5–6 hours and 9–10 hours were 35% and 25% more likely respectively to experience a 5-kg weight gain compared with those sleeping 7–8 hours (p < 0.05). |
| Gangwisch 2005 (31) | National Health and Nutrition Examination Survey (NHANES I) | 3,208 males & females | 32 to 49 years | 8–10 years | United States | Self-Report | None | There was no significant longitudinal association between sleep duration and change in BMI (β = −0.053, p =0.27) |
| Gunderson 2008 (40) | Project VIVA | 940 females | mothers 6 months post-partum | 1 year post-partum | United States | Self-Report | Significant Negative | Adjusted odds ratios for retaining at least 5kg at 6 months postpartum were 3.13 (95% CI: 1.42, 6.94) for those sleeping ≤5 hours/day versus 7 hours/day (p = 0.012) |
| Hairston 2010 (44) | Insulin Resistance Atherosclerosis Study (IRAS) Family Study | 1,107 males and females | 18–81 years | 5 years | United States | Self-Report | Under 40: Significant U-shaped Over 40: None | For those who were younger than 40, short sleep duration (≤5h) was significantly related to increases in BMI (p<0.001) and long sleep duration (≥8h) was also significantly related to increases in BMI (p<0.001). In the older age group, there was no significant association between sleep duration and change in BMI. |
| Hasler 2004 (42) | Zurich Cohort Study | 496 males & females | 27 years | 13 years | Switzerland | Self-Report | Significant Negative | Short sleep duration at age 27 (OR=8.2, 95% CI: 1.9,36.3, p <0.01), age 29 (OR=4.6, 95% CI: 1.3,16.5, p <0.05), and age 34 (OR=3.5, 95% CI: 1.0–12.2, p <0.05) were significantly associated with obesity at later adjacent interviews. |
| Lauderdale 2009 (47) | Coronary Artery Risk Development in Young Adults (CARDIA) Study | 612 males & females | 33–45 years | 5 years | United States | Actigraphy | None | There were no longitudinal associations between sleep measurements and 5-year change in BMI with coefficient near zero (β = −0.02, 95% CI: −0.30,0.025, p=0.86). |
| Littman 2007 (48) | Post-menopausal sedentary overweight women | 173 females | 50–75 years | 1 year | United States | Self-Report | None | There were no significant longitudinal associations between categorically-measured changes in sleep duration and weight change. |
| Lopez-Garcia 2008 (45) | Elderly Spanish population | 3,235 males & females | ≥60 years | 2 years | Spain | Self-Report | Females: Significant U-shaped Males: None Overall: None | Weight gain of ≥5kg was more frequent in females sleeping ≤5h (OR: 3.41, 95% CI: 1.34, 8.69), 8h (OR: 3.03, 95% CI: 1.29, 7.12) and 9h (OR: 3.77, 95% CI: 1.55, 9.17) compared to 7h. No significant associations between sleep duration and weight gain were found in males or in the total study participants. |
| Marshall 2010 (50) | Swedish Obese Subjects Study | 2091 males & females | 37–60 years | 10 years | Sweden | Self-Report | None | There were no linear relationships between change in sleep duration and change in weight for baseline to 10-year comparison in either the control group (rho=0.00, p=0.90) or the surgical group (rho=0.04, p=0.14) |
| Nishiura 2010 (41) | Annual health checkups at Tokyo Gas Co, Ltd | 3,803 males | 40–59 years | 4 years | Japan | Self-report | Significant Negative | Those who slept ≤5 hours showed significant increases in BMI over 4 years (β = 0.015 kg/m2, 95% CI: 0.03,0.27) as compared with those sleeping 7 hours |
| Patel 2006 (16) | Nurses’ Health Study | 68,183 women | 39–65 years | 16 years | United States | Self-report | Significant Negative | Those sleeping ≤5 hours gained 0.78 kg (95% CI: 0.13, 1.44) more after 16 years than those sleeping 7 hours, and more than any other group. The relative risks of a 15-kg weight gain over 16 years were 1.28 (95% CI: 1.15,1.42) and 1.10 (95% CI: 1.04,1.17) for those sleeping ≤5 and 6 hours respectively compared to those sleeping 7 hours |
| Stranges 2008 (49) | Whitehall II Cohort (London) | 4,378 males & females | 35–55 years | 5 years | England | Self-report | None | Short sleep duration (≤5 hours) was not associated with significant changes in BMI during the 5-year follow-up period (β = −0.06, 95% CI: −0.26,0.014) |
| Watanabe 2010 (46) | Employees of an electric power company in Japan | 34,852 males & females | 30–60 years | 1 years | Japan | Self- report | Males: Significant U-shaped Females: None | Males showed a significant association between BMI gain and sleep duration <5 h (β =0.016, 95% CI: 0.024,0.146, p < 0.01), 5h to <6h (β =0.013, 95% CI 0.001, 0.061, p < 0.04), and >=9h (β =0.018, 95% CI 0.079,0.340, p < 0.01). No significant association between BMI gain and sleep duration was found in females. |
Table 2 summarizes the additional independent variables included in the final models for the adult studies. Among the adult studies, 46% adjusted for education, income and/or employment status, all adjusted or stratified by sex, 54% adjusted for alcohol intake and 38% adjusted for sleep problems. Physical activity and diet are known potential confounders, mediators, or moderators of the association between sleep duration and weight gain (51); 69% adjusted for physical activity and 15% adjusted for diet/energy intake.
Table 2.
Adult Study Independent Variables
| Independent Variables in Final Longitudinal Model (other than sleep duration) | Chaput 2008 (43) | Gangwisch 2005 (31) | Gunderson 2008 (40) | Hairston 2010 (44) | Hasler 2004 (42) | Lauderdale 2009 (47) | Littman 2007 (48) | Lopez-Garcia 2008 (45) | Marshall 2010 (50) | Nishiura 2010 (41) | Patel 2006 (16) | Stranges 2008 (49) | Watanabe 2010 (46) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sex | X | X | X | X | X | X | X | X | X | X | X | X | X |
| Race/Ethnicity | X | X | X | X | |||||||||
| Education | X | X | X | X | X | X | |||||||
| Income | X | ||||||||||||
| Employment status | X | X | |||||||||||
| Baseline weight | X | X | X | X | X | X | X | X | X | ||||
| Smoking status | X | X | X | X | X | X | X | X | X | ||||
| Alcohol intake | X | X | X | X | X | X | X | ||||||
| Diet/energy intake | X | X | |||||||||||
| Medications | X | X | X | X | |||||||||
| Mental Health | X | X | X | X | X | ||||||||
| Physical activity | X | X | X | X | X | X | X | X | X | ||||
| Length follow-up | X | ||||||||||||
| Marital Status | X | ||||||||||||
| Chronic diseases | X | ||||||||||||
| Caffeine intake | X | X | X | ||||||||||
| Work hours | X | X | X | ||||||||||
| Breastfeeding | X | ||||||||||||
| Sleep problems/snoring | X | X | X | X | X | ||||||||
| Other | X | X | X | X | X | X | X | X | X | X | X |
Table 3 summarizes the identified 7 longitudinal studies that involve children (22, 52–57), all of which consistently reported an association between short sleep duration and increased weight, overweight; obesity and/or adiposity. However, Snell et al. (56) found this relationship only held in younger children. In children ages 3.0–7.9 years, an additional hour of sleep at baseline was associated with the subsequent decreased probability of being overweight (β = −0.06, p <0.01) and a decrease in BMI by 0.153 standard deviations ( p <0.01) after five years, while in children ages 8.0–12.9 years, an additional hour of sleep at baseline was not significantly associated with the probability of being overweight or a decrease in BMI after five years.
Table 3.
Children Studies
| First Author & Publication Year | Data Source | Sample Size for Analysis | Age at Baseline Weight | Follow- Up Period | Country | Sleep Duration Variable | Association between Sleep Duration & Weight Gain | Results |
|---|---|---|---|---|---|---|---|---|
| Agras 2004 (52) | Newborns in San Francisco Bay Area | 150 boys & girls | 0 years | 9.5 years | United States | Parental Report | Significant Negative | Children’s hours of sleep at ages 3–4 years were a risk factor for overweight at 9.5 years of age (p <0.01). |
| Landhuis 2009 (53) | Dunedin Multidisciplinary Health and Development Study | 1,037 boys & girls | 5 years | 27 years | New Zealand | Parental Report | Significant Negative | Childhood sleep time was negatively associated with adult BMI (β = −0.99, 95% CI: −1.54,−0.31, p=0.003) and lower odds of obesity at age 32 (OR=0.65, 95% CI: 0.43,0.97, p=0.034) |
| Lumeng 2007 (54) | NICHD Study of Early Child Care and Youth Development | 785 boys & girls | 9 years | 3 years | United States | Parental Report | Significant Negative | Longer sleep duration in third grade was associated with reduced likelihood of overweight in sixth grade (OR=0.60, 95% CI: 0.36,0.99, p<0.05). |
| Reilly 2005 (55) | Avon Longitudinal Study of Parents and Children (ALSPAC) | 5,493 boys & girls | 0 years | 7 years | United Kingdom | Parental Report | Significant Negative | Short sleep duration at age 3 (<10.5 hours) was associated with a higher risk of obesity at 7 years (OR=1.45, 95% CI: 1.10,1.89, p<0.01). |
| Snell 2007 (56) | Child Development Supplement (CDS) of the Panel Survey of Income Dynamics (PSID) | 1,441 boys & girls | 3–12 years | 5 years | United States | Parental and Self- Report | Younger: Significant Negative Older: None Overall: Significant Negative | In younger children (3–7.9 years) an additional hour of sleep at baseline was associated with the subsequent probability of being overweight (β = −0.061, p<0.01) and a decrease in standardized BMI (β =0.153 p<0.01) after five years. Results were not significant in older children (8–12.9 years). |
| Taveras 2008 (22) | Project VIVA | 915 boys & girls | 0 years | 3 years | United States | Parental Report | Significant Negative | Short sleep duration (<12 h/day) was associated with both increased odds of overweight (OR=2.04, 95% CI: 1.07,3.91) and higher BMI z-score (β =0.16, 95%CI: 0.01,0.29). |
| Touchette 2008 (57) | Quebec Longitudinal Study of Child Development | 1,138 boys & girls | 0, .5, & 2.5 years | 5.5 years | Canada | Parental Report | Significant Negative | First adjusting for birth weight and weight at 5 months, and secondly adjusting additionally for weight at 2.5 months, persistent short sleepers (<10h) had higher risk of both overweight/obesity at 6 years (OR=4.2, CI: 1.6,11.1, |
Table 4 summarizes the independent variables in the final models for the children studies. Among the children studies, 50% adjusted for physical activity and 25% adjusted for diet/energy intake, all but one adjusted or stratified for sex, 50% adjusted for parental weight and 75% adjusted for education, income or SES.
Table 4.
Children Study Independent Variables
| Independent Variables in Final Longitudinal Model (other than sleep duration) | Agras 2004 (52) | Landhuis 2009 (53) | Lumeng 2007 (54) | Reilly 2005 (55) | Snell 2007 (56) | Taveras 2008 (22) | Touchette 2008 (57) |
|---|---|---|---|---|---|---|---|
| Sex | X | X | X | X | X | X | |
| Race/Ethnicity | X | X | X | X | |||
| Parental Education | X | X | X | X | X | ||
| Income | X | X | X | ||||
| SES | X | ||||||
| Baseline weight | X | X | X | X | X | X | |
| Parental Smoking status | X | X | X | X | |||
| Diet/energy intake | X | X | |||||
| Physical activity | X | X | X | ||||
| Media use | X | X | X | X | |||
| Family status | X | X | |||||
| Parental weight | X | X | X | ||||
| Adult behavior | X | X | |||||
| Child behavior | X | X | |||||
| Breastfeeding | X | X | |||||
| Sleep problems/snoring | X | ||||||
| Other | X | X | X |
Discussion
This study provides for the first time a systematic review of longitudinal-only studies examining the association between sleep duration and subsequent weight gain.
Children studies in this review consistently reported a relationship between short sleep duration and weight gain with the exception of the older children (8.0–12.9 years at baseline and followed for 5 years) in one study (56). The results of the adult studies were more varied, with four studies finding an association between only short sleep duration and weight gain, four finding an association between short sleep and weight gain and long sleep and weight gain, and the remaining five finding no significant association between sleep duration and weight gain.
In conducting our review, we identified three areas of limitations that need additional attention: Diminishing Association between Short Sleep Duration and Weight Gain after Time since Transition to Short Sleep Pattern, Inclusion of Appropriate Confounding Variables (specifically the omission of other sleep characteristics and changes in other health behaviors), and Measurement (of Weight and Sleep Duration Variables)
Diminishing of Association between Short Sleep Duration and Weight Gain over Time after Transition to Short Sleep Pattern
As pointed out in prior systematic reviews, there appear to be age-related changes in the association between sleep duration and weight gain. This may be simply because the proposed physiological and behavioral mechanisms underlying the relationship between sleep duration and weight gain are strongest at the younger age ranges. However, another possibility for the occasional lack of significant associations between short sleep and weight gain observed among the adults and older children is that individuals who are short sleepers do not continue to gain weight linearly over the course of their short sleeping (31, 42, 47–49). That is, as we note in a letter to the editor to the American Journal of Epidemiology, if a pattern of chronic short sleep duration had started three years before the study, and the change in sleep duration resulted in a net increase of 200 calories per day in a 120-pound (54.4kg) woman, by the time the study began three years later the woman would have reached a threshold weight of 150 pounds (68.0kg) and not gained any more weight during the study (58). While the short sleep starting prior to the study would be contributing to the woman’s current overweight condition (since the participant’s caloric increase due to short sleep would still be supporting the threshold weight of 150 pounds (68.0 kg)), the woman would not gain more weight during the study timeframe because the study’s longitudinal timeframe would have missed the crucial period when the short sleep began. In order for short sleep to predict any physiological or behavioral change, the longitudinal time frame examined would need to start “prior to or at the beginning of the short sleep transition for each participant (58).” This may also explain why studies are less likely to show an association between sleep duration and weight gain in older people, who are more likely to be studied after they have already experienced a potential weight gain related to sleep duration than younger people.
Inclusion of Appropriate Confounding Variables
As shown by Tables 2 and 4, on the whole these studies adjust for a wide range of potentially confounding variables in estimating the relationship between short sleep duration and weight gain. Yet there are important limitations and lessons learned by comparing the results of the studies that adjust for some variables with the results of studies that don’t adjust for the same variables. Here we discuss three important examples of confounding variables bias – omission of sleep complaints measures, omission of media use, insufficient attention to time-varying behavioral covariates.
Sleep problems may be due to obesity and influence sleep duration (33), yet they were not analyzed in most studies. Five adult studies adjusted for sleep problems; three (31, 47, 49) found no association between sleep duration and weight gain, one found a u-shaped curve in women but no significant association between sleep duration and weight gain in men or in the overall population (45), and one found only a modest weight gain associated with short sleep (2). Gangwisch, et al. (31) reported that in bivariate analysis a higher percentage of subjects who reported that sleeping problems (waking in the night and daytime sleepiness) had become worse compared with a year earlier had gained at least ten pounds over the last 6 months than other groups. In longitudinal linear regression analysis, controlling for potential confounders including sleep problems, while each additional hour of sleep at baseline was negatively associated with change in BMI, the association was not statistically significant (β = −0.053, p =0.27). Lauderdale, et al. (47), adjusting for snoring ( p =0.02), found no association between sleep duration and change in BMI. Stranges, et. al (49), controlling for sleep medication (hypnotics) found no significant association between sleep duration and changes in BMI (β =−0.06, 95% CI: −0.26, 0.014). While Lopez-Garcia, et al. (45) found weight gain of ≥5kg to be more frequent in women sleeping ≤5h (OR: 3.41, 95% CI: 1.34, 8.69), 8h (OR: 3.03, 95% CI: 1.29, 7.12) and 9h (OR: 3.77, 95% CI: 1.55, 9.17) compared to 7h, no significant associations between sleep duration and weight gain was found in men or in the total study participants. Patel, et al. (16) finds a modest weight gain for those sleeping ≤5 hours (0.78 kg, 95% CI: 0.13, 1.44) in the model adjusted for all covariates including snoring status. Over the 16 years considered, the relative risks of a 15-kg weight gain were 1.28 (95% CI: 1.15, 1.42) and 1.10 (95%CI: 1.04, 1.17) for those sleeping ≤5 and 6 hours respectively when adjusted all covariates. In summary, three out of five of the adult studies who adjust for sleep problems did not find a significant relationship between sleep duration and weight gain, Stranges, et al. found a u-shaped curve in women only, and the Patel, et al. study found only a modest increase in weight gain when adjusting for sleep problems. Eight adult studies do not adjust for sleeping problems and only three of these find no association between sleep duration and weight gain (42, 48, 50). These results may indicate that sleep problems may be an important confounder that should be included all studies related to sleep duration and weight gain, and that if they had been included in other studies in this review may have significantly mediated results. In fact, only one children’s study addressed a sleep problem as a potentially confounding variable (57).
Finally, there is the possibility that while many covariates are adjusted for, there are time-varying covariates that may be important for capturing changes in weight over time. For example, smoking cessation often leads to weight gain, and conversely smoking inception often leads to weight loss; these changes in body weight can be ascribed to increased metabolic rate and decreased caloric absorption when smoking (59–63). If smoking status had not changed for many years before study inception and did not change throughout the study, one might not expect smoking status to affect weight change during the study. However, if smoking started around the inception of the study, the participant might be expected to lose weight during the study due to the new smoking habit, and in addition there may be a dose response relationship in that the amount of weight lost might be associated with magnitude smoked. Conversely, if a participant was a heavy smoker and stopped smoking around time of study inception, we might expect to see that participant gain weight due to the smoking cessation. So if a participant started sleeping shorter hours but also started smoking, the two might possibly cancel each other out as far as subsequent weight gain. While eight of the 13 adults studies controlled for smoking, only the Lauderdale, et al. (47) study had a smoking status category indicating if a participant had started smoking after baseline (“new smoker”), and those participants who started smoking after baseline did gain less weight. Other behavioral changes (e.g., alcohol intake, diet and energy intake, medications, psychological problems) could have similar considerations regarding inception/cessation times and magnitude.
Media use was not adjusted for in any of the adult studies, and only was adjusted for in 63% of children studies. Four children studies controlled for television viewing and no other media (22, 39, 53, 55) and one study controlled for television and video games (57). Given the recent dramatic increase in use of entertainment media, the early evidence of associations between television with both sleep and obesity, and reports that television comprised only 58% of total media use for youth in the U.S. in 2009 (21), it would seem essential that a broader range of media be routinely included a list of potentially confounding variables. All studies adjusting for media use included in this review found a significant association between sleep duration and weight gain. While Taveras et al. (22) noted that adding television to the model only minimally changed the association between sleep and weight gain, they also report that a combination of low sleep and high levels of television in infants are associated with increased odds of overweight at 3 years old.
Measurement Issues
Only one reviewed study (47) used an objective measurement of sleep duration using actigraphy, with all others using some type of self-reported sleep (including parental-reported), including two studies which used sleep reported in 24-hour time diaries (35, 56). Some argue that any self-reported sleep is “by nature retrospective and therefore likely to be subject to errors”(7). Compared to actigraph-measured sleep, self-reported sleep has been reported to be biased by systematic over-reporting (64). Knutson and Lauderdale (65) found a weak correlation between self-reported and time-diary sleep, reporting a mean of 8 hours for self-reported “usual” sleep and a mean of nearly 9 hours for time-diary sleep. Juster et al. (66) report that information collected via time diaries is more accurate then self-reported information. However, Wolfson, et al. (67) found that survey sleep variables were significantly correlated with both time diary and actigraph-measured sleep variables among adolescents.
Most studies measured height and weight objectively, with the exception of five studies (16, 40, 42, 49, 57) which measured height and weight through self-report, and two studies (35, 56) which measured height objectively and weight through self-report at baseline and both height and weight objectively at follow-up. The only studies that found a U-shaped association were adult studies that measured height and weight objectively.
Nielsen, et al. (7) expresses the concern that given the difficulty in providing accurate and objective measures for exposures and effects, reliable estimations of association between sleep duration and weight change might require large groups of people followed over long time periods. Nielsen provides a detailed discussion of measurement challenges (7).
Revisiting the Conceptual Model
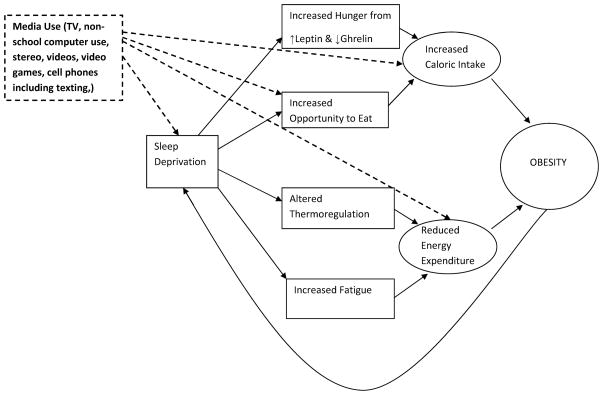
Modeling a causal pathway between short sleep and weight gain is extremely challenging. We previously mentioned the problems of reverse causality and several potential confounders, mediators and moderators; for further discussion refer to Nielsen, et al. (7). Patel & Hu (2) have proposed a model incorporating mechanisms discussed earlier to illustrate how short sleep might lead to increased caloric intake and reduce energy expenditure, both of which contribute to obesity. In Figure 2, we revisit the Patel and Hu (2) model by adding one of many potential confounders or mediators (Media Use) in dashed lines to illustrate the complications when adding just one additional covariate:
Figure 2.
Patel & Hu Model (2) with Media Use added
Figure 2 illustrates that Media Use may result in less time to sleep which in turn contributes to increased hunger (via the leptin and ghrelin pathways) leading to increased caloric intake and decreased energy expenditure; however, more hours of television viewing also directly relate to both an increase in sedentary activity and therefore decreased energy expenditure, and increase in caloric intake through the consumption of excess fat calories.
A revisited model may also contain important feedback loops. For example as mentioned earlier, obesity may exacerbate sleep apnea which may in turn decrease sleeping time (33). Other reported major factors associated with sleep and/or obesity are age, alcohol consumption, chronic diseases, psychological disorders, physical activity, smoking, caffeine consumption, socioeconomic status influencing sleep and eating conditions, number and timing of work hours, cultural norms, disabilities, pain limiting physical activity, medications (which may induce sleep disturbances and/or weight gain), parental body weight, education, income, parenting behaviors, and genetics (7, 68, 69). When suggesting a causal model, care must be taken to identify which factors truly represent straightforward cause and effect, which factors are mediators, which are underlying or spurious causes, which factors could be bidirectional, and the optimal measurement of factors temporally; however, as Nielson (7) points out, distinguishing between a confounder and a mediator in sleep research can be challenging, and many of our studies indicate more research needs to be done to tease out these relationships.
Summary and Next Steps
Overall, the results of this rigorous systematic literature review which restricts the studies to those with longitudinal design support prior evidence suggesting a temporal relationship between short sleep duration and subsequent weight gain. As with the cross-sectional studies, these results are more prevalent in younger populations compared to older populations. This may be due to the study designs themselves, or because the effect of short sleep duration on weight gain is attenuated over time. We also raised concerns about inclusion of appropriate potentially confounding or mediating variables (especially sleep problems such as insomnia, sleep disordered breathing, etc. and media use) and measurement issues. In addition to concerns about specifics of the individual studies included above, we are also concerned about the risk of publication bias. Publication bias may cause longitudinal studies finding no association between sleep duration and weight gain to remain unpublished.
Another limitation of our review is that of the 7 children studies, 3 did not use a standardized BMI measure (52, 53, 57), therefore increasing BMI in those studies may not be meaningful. Another limitation is that covariates not in the final model may have been excluded during analysis and were unknown to us.
Moving forward, in order to better assess the possible causal relationship between sleep deprivation and weight gain, a randomized clinical trials approach might be used. A clinical trial (clintrials.gov identifier #NCT00261898) sponsored by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) is currently recruiting participants who are 18–50 years old, obese and chronically sleep-deprived (≤6.5 hours sleep per night). Chronic sleep deprivation will be verified by sleep logs and actigraphy before the study inception. The study aims to have the intervention group increase their sleep to approximately 7.5 hours with the proposed treatment being “an educational and behavioral intervention aimed at increasing sleep in a non-pharmacological fashion” during the trial’s 12-month duration. This trial may be able to report results of sleeping longer for those who are obese, however will still not be able to report the results of curtailing sleep over a long period of time.
Another randomized control trial (clintrials.gov identifier #NCT00892983) funded by the Health Research Council of New Zealand is recruiting mothers in the later stages of pregnancy for a 24-month intervention with a 12-month follow-up. Participants will be randomized to one of four groups; control, sleep intervention, physical activity and eating intervention, and one group receiving all interventions. The study is aimed at determining if guidance and support might alter sleep duration, or eating and/or physical activity, and if any such alteration reduces excessive weight gain in children in the first 3 years of life.
While these studies will add to the knowledge base regarding the association between sleep duration and weight gain, neither study tests whether sleep curtailment leads to weight gain; this may be impossible given ethical and practical considerations regarding restricting sleep in study participants. Both experimental and observational exploration of the association between sleep curtailment and weight gain need to be performed to clarify the potential causal relationship.
Practice Points:
There is increasing evidence that short sleep duration is associated to subsequent weight gain in children, with less consistent reports in adults.
The effects of short sleep duration on subsequent weight gain may diminish over time. Although a causal relationship between short sleep duration and weight gain may exist, it may not be captured by longitudinal studies. For example, if there is no change in sleep duration near the inception of the study, a corresponding change in weight may not be observed.
Objective measurements of sleep duration would reduce measurement errors, however are often costly and impractical.
Research Agenda:
While causal pathways between sleep duration and weight changes have been suggested, the underlying mechanisms need elucidation.
Future studies need to be sensitive to including time-varying behavioral characteristics in a logical temporal manner.
While it may be unethical for a randomized controlled trial to deprive participants of sleep, alternative experimental studies need to be conducted to further explore the association between sleep duration and weight gain.
As we understand more about how, when, and why sleep duration may contribute to obesity, we should consider incorporating interventions related to sleep into obesity prevention programs, especially for children.
Figure 1.
Illustration of Literature Search
Abbreviations
- BMI
body mass index
- h
hour
- kg
kilograms
Footnotes
Financial Disclosure: This research is funded in part by grants R21HD060208 and R01AG036868
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Lorrie Magee, Email: lorrie.magee@stonybrook.edu, Doctoral Program in Population Health and Clinical Outcomes Research, Department of Preventive Medicine, HSC Level 3, Stony Brook University, Stony Brook, NY 11794-8338, 917-733-7231 (phone), (631) 444-3480 (fax).
Lauren Hale, Email: lhale@notes.cc.sunysb.edu, Associate Professor of Preventive Medicine, Graduate Program in Public Health, HSC Level 3, room 071, Stony Brook University, Stony Brook, NY 11794-8338, 631-444-1007 (phone), 631-444-3480 (fax).
References
- 1.CDC. Halting the epidemic by making health easier: at a glance 2010. Atlanta: Centers for Disease Control and Prevention; 2010. [Google Scholar]
- 2*.Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity. 2008;16(3):643–53. doi: 10.1038/oby.2007.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Van Cauter E, Knutson KL. Sleep and the epidemic of obesity in children and adults. European Journal of Endocrinology. 2008;159:S59–S66. doi: 10.1530/EJE-08-0298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4*.Marshall NS, Glozier N, Grunstein RR. Is sleep duration related to obesity? A critical review of the epidemiological evidence. Sleep Medicine Reviews. 2008;12:29–298. doi: 10.1016/j.smrv.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 5.Chen X, Beydoun MA, Wang Y. Is sleep duration associated with childhood obesity? A systematic review and metanalysis. Obesity. 2008;16:265–74. doi: 10.1038/oby.2007.63. [DOI] [PubMed] [Google Scholar]
- 6.Cappuccio FP, Taggart FM, Kandala N, Currie A, Peile E, Stranges S, et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31(5):619–26. doi: 10.1093/sleep/31.5.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nielsen LS, Danielsen KV, Sorensen TIA. Short sleep duration as a possibile cause of obesity: critical analysis of the epidemiologocal evidence. Obesity Reviews. 2010 doi: 10.1111/j.1467–789X.2010.00724.x. [DOI] [PubMed] [Google Scholar]
- 8.Hart CN, Jedalian E. Shortened sleep duration is associated with pediatric overweight. Behavioral Sleep Medicine. 2008;6:251–67. doi: 10.1080/15402000802371379. [DOI] [PubMed] [Google Scholar]
- 9.Knutson KL, Van Cauter E. Associations between sleep loss and increased risk of obesity and diabetes. Annals of the New York Academy of Sciences. 2008;a1129:287–304. doi: 10.1196/annals.1417.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated grehlin, and increased body mass index. PLos Medicine. 2004;(1):e62. doi: 10.1371/journal.pmed.0010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Spiegel K, Tasali E, Penev P, Van Cauter E. Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated grehlin levels, and increased hunger and appetite. Annals of Internal Medicine. 2004;141(11):846–50. doi: 10.7326/0003-4819-141-11-200412070-00008. [DOI] [PubMed] [Google Scholar]
- 12.Chaput JP, Despres JP, Bouchard C, Tremblay A. Short sleep duration is associated with reduced leptin levels and increased adiposity: results from the Quebec Family Study. Obesity. 2007;15:253–61. doi: 10.1038/oby.2007.512. [DOI] [PubMed] [Google Scholar]
- 13.Spiegel K, Leproult R, Van Couter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354:1435–9. doi: 10.1016/S0140-6736(99)01376-8. [DOI] [PubMed] [Google Scholar]
- 14.Brondel L, Romer MA, Nougues PM, Touyarou P, Davenne D. Acute partial sleep deprvation increases food intake in healthy men. American Journal of Clinical Nutrition. 2010;91(6):1550–9. doi: 10.3945/ajcn.2009.28523. [DOI] [PubMed] [Google Scholar]
- 15.Rechtschaffen A, Bergmann BM. Sleep deprivation in the rat by the disk-over-water method. Behavioral Brain Research. 1995;69:55–63. doi: 10.1016/0166-4328(95)00020-t. [DOI] [PubMed] [Google Scholar]
- 16.Patel SR, Malhotra A, White DP, Gottlieb DJ, Hu FB. Association between reduced sleep and weight gain in women. American Journal of Epidemiology. 2006;163(10):947–54. doi: 10.1093/aje/kwj280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nedeltcheva AV, Kilkus JM, Imperial J, Kasza K, Schoeller DA, Penev PD. Sleep curtailment is accompanied by increased intake of calories from snacks. American Journal of Clinical Nutrition. 2009;89:126–33. doi: 10.3945/ajcn.2008.26574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weiss A, Xu F, Storder-Isser A, Thomas A, Ievers-Landis CE, Redline S. The association of sleep duration with adolescents’ fat and carbohydrate consumption. Sleep. 2010;33(9):1201–9. doi: 10.1093/sleep/33.9.1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Taveras EM, Hohman KH, Price S, Gortmaker SL, Sonneville K. Televisions in the bedrooms of racial/ethnic minority children: how did they get there and how do we get them out? Clinical Pediatrics. 2009;48(7):715–9. doi: 10.1177/0009922809335667. [DOI] [PubMed] [Google Scholar]
- 20.KFF. Daily media use among children and teens is up dramatically from five years ago. Washington, D.C: The Henry J. Kaiser Family Foundation; 2010. [August 1, 2009]; Available from: http://www.kff.org/entmedia/entmedia012010nr.cfm. [Google Scholar]
- 21.Rideout VC, Foehr UG, Roberts DF. Generation M2: Media lives of 8- to 18-year-olds. Menlo Park, CA: The Henry J. Kaiser Family Foundation; 2010. Available from: http://www.kff.org/entmedia/upload/8010.pdf. [Google Scholar]
- 22*.Taveras EM, Rifas-Shiman SL, Oken E, Gunderson EP, Gillman MW. Short sleep duration in infancy and risk of childhood overweight. Archives of Pediatrics & Adolescent Medicine. 2008;162(4):305–11. doi: 10.1001/archpedi.162.4.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vioque J, Torres A, Quiles J. Time spent watching television, sleep duration and obesity in adults living in Valencia, Spain. International Journal of Obesity. 2000;24:1683–1688. doi: 10.1038/sj.ijo.0801434. [DOI] [PubMed] [Google Scholar]
- 24.Kuriyan R, Bhat S, Thomas T, Vaz M, Kurpad A. Television viewing and sleep are associated with overweight among urban and semi-urban South Indian children. Nutrition Journal. 2007;6(25):1–4. doi: 10.1186/1475-2891-6-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nevarez MD, Rifas-Shiman SL, Kleinman KP, Gillman MW, Taveras EM. Associations of early life risk factors with infant sleep duration. Academic Pediatrics. 2010;10:187–93. doi: 10.1016/j.acap.2010.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ortega FB, Chillon P, Ruiz JR, Delgado M, Albers U, Moreno LA, et al. Sleep patterns in Spanish adolescents: associationss with watching TV and leisure-time physical activity. European Journal of Applied Phsyiology. 2010;110:563–73. doi: 10.1007/s00421-010-1536-1. [DOI] [PubMed] [Google Scholar]
- 27.Gortmaker SL, Must A, Sobol AM, Peterson K, Colditz GA, Dietz WH. Television viewing as a cause of increasing obesity among children in the United States, 1986–1990. Archives of Pediatrics & Adolescent Medicine. 1996;150:356–62. doi: 10.1001/archpedi.1996.02170290022003. [DOI] [PubMed] [Google Scholar]
- 28.Robinson TN. Reducing children’s television viewing to prevent obesity. JAMA. 1999;282(16):1561–7. doi: 10.1001/jama.282.16.1561. [DOI] [PubMed] [Google Scholar]
- 29.Kripke DF, Langer RD, Elliott JA, Klauber MR, Rex KM. Mortality related to actigraphic long and short sleep. Sleep Medicine. 2010;12(1):28–33. doi: 10.1016/j.sleep.2010.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tamakoshi A, Ohno Y. Self-reported sleep duration as a predictor of all-cause mortality: Results from the JACC study, Japan. Sleep. 2004;27(1):51–4. [PubMed] [Google Scholar]
- 31*.Gangwisch JE, Malaspina D, Boden-Albala B, Heymsfield SB. Inadequate sleep as a risk factor for obesity: analyses of the NHANES I. Sleep. 2005;28(10):1289–96. doi: 10.1093/sleep/28.10.1289. [DOI] [PubMed] [Google Scholar]
- 32.Locard E, Marmelle N, Billette A, Miginiac M, Rey S. Risk factors of obesity in a five year old population. International Journal of Obesity and Related Metabolic Disorders. 1992;16(10):721–19. [PubMed] [Google Scholar]
- 33.Vgontzas AN, Bixler EO, Basta M. Obesity and sleep: A bidirectional association? Sleep. 2010;33(5):573–4. doi: 10.1093/sleep/33.5.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gillman MW, Rifas-Shiman SL, Kleinman K, Oken E, Rich-Edwards JW, Taveras EM. Developmental origins of childhood overweight: Potential public health impact. Obesity. 2008;16(7):1651–6. doi: 10.1038/oby.2008.260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bell JF, Zimmerman FJ. Shortened nighttime sleep duration in early life and subsequent childhood obesity. Archives of Pediatrics & Adolescent Medicine. 2010;164(9):840–5. doi: 10.1001/archpediatrics.2010.143. [DOI] [PubMed] [Google Scholar]
- 36.Chaput J, Leblanc C, Perusse L, Despres J, Bouchard C, Tremblay A. Risk factors for adult overweight and obesity in the Quebec Family Study: Have we been barking up the wrong tree? Obesity. 2009;10:1964–79. doi: 10.1038/oby.2009.116. [DOI] [PubMed] [Google Scholar]
- 37.Berkey CS, Rockett HRH, Colditz GA. Weight gain in older adolescent females: The internet, Sleep, Coffee, and Alcohol. Journal of Pediatrics. 2008;153:635–9. doi: 10.1016/j.jpeds.2008.04.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sugimori H, Yoshida K, Izuno T, Miyakawa M, Suka M, Sekine M, et al. Analysis of factors that influence body mass index from ages 3 to 6 years: A study based on the Toyama cohort study. Pediatrics International. 2004;46:302–10. doi: 10.1111/j.1442-200x.2004.01895.x. [DOI] [PubMed] [Google Scholar]
- 39.Rutters F, Gerver WJ, Nieuwenhuizen AG, Verhoef SPM, Westerterp-Plantenga MS. Sleep duration and body-weight development during puberty in a Dutch children cohort. International Journal of Obesity. 2010 doi: 10.1038/ijo.2010.161. [DOI] [PubMed] [Google Scholar]
- 40.Gunderson EP, Rifas-Shiman SL, Oken E, Rich-Edwards JW, Kleinman KP, Taveras EM, et al. Association of fewer hours of sleep and 6 months postpartum with substantial weight retention at 1 year postpartum. American Journal of Epidemiology. 2008;167(2):178–87. doi: 10.1093/aje/kwm298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nishiura C, Hashimoto H. A 4-year study of the association between short sleep duration and change in body mass index in Japanese male workers. Journal of Epidemilogy (Japan) 2010;20(5):385–90. doi: 10.2188/jea.JE20100019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42*.Hasler G, Buysse D, Klaghofer R, Gamma A, Ajdacic V, Eich D, et al. The association between short sleep duration and obesity in young adults: a 13-year prospective study. Sleep. 2004;27(4):661–6. doi: 10.1093/sleep/27.4.661. [DOI] [PubMed] [Google Scholar]
- 43*.Chaput J, Despres J, Bouchard C, Tremblay A. The association between sleep duration and weight gain in adults: A 6-year prospective study from the Quebec Family Study. Sleep. 2008;31(4):517–23. doi: 10.1093/sleep/31.4.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hairston KD, Bryor-Ash M, Norris JM, Haffner S, Bowden DW, Wagenknecht LE. Sleep duration and five-year abdominal fat accumulation in a minority cohort: The IRAS study. Sleep. 2010;33(3):289–95. doi: 10.1093/sleep/33.3.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lopez-Garcia E, Faubel R, Loan-Munoz L, Zuluaga MC, Banegas JR, Rodriguez-Artalejo F. Sleep duration, general and abdominal obesity, and weight change among the older adult population of Spain. American Journal of Clinical Nutrition. 2008;87:310–6. doi: 10.1093/ajcn/87.2.310. [DOI] [PubMed] [Google Scholar]
- 46.Watanabe M, Kikuchi H, Tanaka K, Takahashi M. Association of short sleep duration with weight gain and obesity at 1-year follow-up: A large-scale prospective study. Sleep. 2010;33(2):161–7. doi: 10.1093/sleep/33.2.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47*.Lauderdale DS, Knutson KL, Rathouz PJ, Yan LL, Hulley SB, Liu K. Cross-sectional and longitudinal associations between objectively measured sleep duration and body mass index. American Journal of Epidemiology. 2009;170(7):805–13. doi: 10.1093/aje/kwp230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Littman AJ, Vitiello MV, Foster-Schubert K, Ulrich CM, Tworoger SS, Potter JD. Sleep, ghrelin, leptin and changes in body weight during a 1-year moderate-intensity physical activity intervention. International Journal of Obesity. 2007;31:466–75. doi: 10.1038/sj.ijo.0803438. [DOI] [PubMed] [Google Scholar]
- 49.Stranges S, Cappuccio FP, Kandala N, Miller MA, Taggart FM, Kumari M, et al. Cross-sectional versus prospective associations of sleep duration with changes in relative weight and body fat distribution. American Journal of Epidemiology. 2008;167(3):321–9. doi: 10.1093/aje/kwm302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50*.Marshall NS, Grunstein RR, Peltonen M, Stenlof K, Hedner J, Sjostrom LV. Changes in sleep duration and changes in weight in obese patients: The Swedish Obese Subjects study. Sleep and Biological Rhythms. 2010;8(1):63–71. [Google Scholar]
- 51.Nishiura C, Noguchi J, Hashimoto H. Dietary patterns only partially explain the effect of short sleep duration on the incidence of obesity. Sleep. 2010;33(6):753–7. doi: 10.1093/sleep/33.6.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Agras WS, Hammer LD, McNicholas F, Kraemer H. Risk factors for childhood overweight: A prospective study from birth to 9.5 years. Journal of Pediatrics. 2004;145(1):20–5. doi: 10.1016/j.jpeds.2004.03.023. [DOI] [PubMed] [Google Scholar]
- 53.Landhuis CE, Poulton R, Welch D, Hancox RJ. Childhood sleep time and long-term risk for obesity: A 32-year prospective birth cohort study. Pediatrics. 2008;122:955–60. doi: 10.1542/peds.2007-3521. [DOI] [PubMed] [Google Scholar]
- 54.Lumeng JC, Somashekar D, Appugliese D, Kaciroti N, Corwyn RF, Bradley RH. Shorter sleep duration is associated with increased risk for being overweight at ages 9 to 12 years. Pediatrics. 2007;120:1020–9. doi: 10.1542/peds.2006-3295. [DOI] [PubMed] [Google Scholar]
- 55.Reilly JJ, Armstrong J, Dorosty AR, Emmett PM, Ness A, Rogers I, et al. Early life risk factors for obesity in childhood: cohort study. BMJ. 2005 doi: 10.1136/bmj.38470.670903.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56*.Snell EK, Adam EK, Duncan GJ. Sleep and the body mass index and overweight status of children and adolescents. Child Development. 2007;78(1):309–23. doi: 10.1111/j.1467-8624.2007.00999.x. [DOI] [PubMed] [Google Scholar]
- 57.Touchette E, Petit D, Tremblay RE, Boivin M, Falissard B, Genolini C, et al. Associations between sleep duration patterns and overweight/obesity at age 6. Sleep. 2008;31(11):1507–14. doi: 10.1093/sleep/31.11.1507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Magee LL, Hale LE. Re: Cross-sectional and longitudinal associations between objectively measured sleep duration and body mass index. American Journal of Epidemiology. 2010;171(6):745. doi: 10.1093/aje/kwq018. [DOI] [PubMed] [Google Scholar]
- 59.Matsushita Y, Nakagawa T, Yamamoto S, Takahashi Y, Noda M, Mizoue T. Associations of smoking cessation with visceral fat area and prevalence of metabolic syndrome in men: The hitachi health study. Obesity. 2010 doi: 10.1038/oby.2010.237. [DOI] [PubMed] [Google Scholar]
- 60.Williamson DF, Madans J, Anda RF, Kleinman JC, Giovano GA, Byers T. Smoking cessation and severity of weight gain in a national cohort. New England Journal of Medicine. 1991;324:739–45. doi: 10.1056/NEJM199103143241106. [DOI] [PubMed] [Google Scholar]
- 61.Shimokata H, Muller DC, Andres R. Studies in the distribution of body fat: III. Effects of cigraette smoking. Journal of the American Medical Association. 1989;261:1169–1173. [PubMed] [Google Scholar]
- 62.Flegal KM, Troiano RP, Pmuk ER, Kuczmarski RJ, Campbell SM. The influence of smoking cessation on the prevalence of overweight and obesity in the United States. New England Journal of Medicine. 1995;333:1165–70. doi: 10.1056/NEJM199511023331801. [DOI] [PubMed] [Google Scholar]
- 63.Klesges RC, Winders SE, Meyers AW, Eck LH, Ward KD, Hultquist CM, et al. How much weight gain occurs following smoking cessation? A comparison of weight gain using both continuous and point prevalence abstinence. Journal of consulting and clinical psychology. 1997;65(2):286–91. doi: 10.1037//0022-006x.65.2.286. [DOI] [PubMed] [Google Scholar]
- 64.Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Self-reported and measured sleep duration: How similar are they? Epidemiology. 2008;19(6):838–45. doi: 10.1097/EDE.0b013e318187a7b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Knutson KL, Lauderdale DS. Sleep duration and overweight in adolescents: Self-reported sleep hours versus time diaries. Pediatrics. 2007;119:e1056–e62. doi: 10.1542/peds.2006-2597. [DOI] [PubMed] [Google Scholar]
- 66.Juster FT, Ono H, Stafford FP. As assessment of alternate measures of time use. Sociological Methods. 2003;33:19–54. [Google Scholar]
- 67.Wolfson AR, Carskadon MA, Acebo C, Seifer R, Fallone G, Labyak SE, et al. Evidence for the validity of sleep habits survey for adolescents. Sleep. 2003;26(2):213–6. doi: 10.1093/sleep/26.2.213. [DOI] [PubMed] [Google Scholar]
- 68*.Magee CA, Iverson DC, Huang XF, Caputi P. A link between chronic sleep restriction and obesity: methodological considerations. Public Health. 2008;122:1373–81. doi: 10.1016/j.puhe.2008.05.010. [DOI] [PubMed] [Google Scholar]
- 69.Chouchane L, Danguir J, Beji C, Bouassida K, Camoin L, Sfar H, et al. Genetic variation in the stress protein hsp70–2 gene is highly associated with obesity. International Journal of Obesity. 2001;25:462–6. doi: 10.1038/sj.ijo.0801545. [DOI] [PubMed] [Google Scholar]