Abstract
The duodenal mucosa is exposed to endogenous and exogenous chemicals, including acid, CO2, bile acids and nutrients. Mucosal chemical sensors are necessary to exert physiological responses such as secretion, digestion, absorption, and motility. We propose a mucosal chemosensing system by which luminal chemicals are sensed via mucosal acid sensors and G-protein-coupled receptors. Luminal acid/CO2 sensing consists of ecto- and cytosolic carbonic anhydrases, epithelial ion transporters, and acid sensors expressed on the afferent nerves in the duodenum. Furthermore, a luminal L-glutamate signal is mediated via mucosal L-glutamate receptors, including metabotropic glutamate receptors and taste receptor 1 family heterodimers, with activation of afferent nerves and cyclooxygenase, whereas luminal Ca2+ is differently sensed via the calcium-sensing receptor in the duodenum. Recent studies also show the involvement of enteroendocrine G-protein-coupled receptors in bile acid and fatty acid sensing in the duodenum. These luminal chemosensors help activate mucosal defense mechanisms in or- der to maintain the mucosal integrity and physiological responses. Stimulation of luminal chemosensing in the duodenal mucosa may prevent mucosal injury, affect nutrient metabolism, and modulate sensory nerve activity.
Key Words: Acid sensor, Vanilloid receptor, Carbonic anhydrase, Luminal nutrient, G-protein-coupled receptors
Introduction
The duodenum, so named for its length of twelve fingers, is a prime segment of the gastrointestinal (GI) tract regarding luminal chemosensing due to its strategic positioning between the pylorus and the pancreaticobiliary ducts. The duodenal mucosa is regularly exposed to strong gastric acid (pH ∼2), high PCO2 (up to ∼400 mm Hg) from the neutralization of secreted HCO3–, digestive enzymes, bile acids, and foodstuffs. Physiological processes such as secretion, digestion, absorption, and motility occur in response to these luminal substances, implying the presence of mucosal chemosensors, which evoke protective mucosal defense mechanisms [1]. The duodenal mucosa rapidly responds to luminal chemical stimuli not only by enhancing local defense factors such as mucosal blood flow, and HCO3– and mucus secretion [2], but also by inhibiting gastric emptying and secretion through the release of gastric inhibitory hormones including incretins, the latter known as ‘duodenal brake’ [3].
Mucosal defense mechanisms consist of pre-epithelial, epithelial and subepithelial defense factors. In vivo microscopy and duodenal loop perfusion systems enable us to study these factors, including HCO3– and mucus secretion (pre-epithelial), intracellular pH (pHi) regulation with ion transporters and ecto- and cytosolic enzyme activities (epithelial), and blood flow regulated via afferent nerves and mediator releases (subepithelial). Since disruption of these defenses injures the mucosa, signals that enhance defense mechanisms may protect the mucosa from luminal substances in order to maintain epithelial integrity. Nevertheless, the mucosa needs to sense luminal acidity or substances in order to rapidly respond and enhance defense mechanisms.
Here, we will show how the duodenal mucosa senses luminal acidity under physiological conditions. We will also discuss the presence of chemosensing receptors for luminal nutrients in the duodenum, including amino acids and Ca2+. Amino acids or Ca2+ may be physiologically sensed by GI mucosa. Understanding how the GI mucosa ‘tastes’ luminal chemicals may help identify novel molecular targets in the treatment of mucosal injury, nutrient metabolism and sensory sensitivity.
Duodenal Acid/CO2 Sensing
The duodenal mucosa, which is constantly and cyclically exposed to luminal acid and high PCO2 due to gastric acid and the secreted HCO3–, has multilayered, multistep defense mechanisms to counter acid-induced mucosal injury [4]. These mechanisms coordinately regulate mucus and HCO3– secretion, pHi and cellular buffering, and submucosal neuronal activation and blood flow responses. Since duodenal luminal pH rapidly changes between 2 and 7 as a result of the constant mixture of secreted HCO3– with jets of antrally-propelled gastric acid, the duodenal mucosa must rapidly adjust its defense mechanisms according to luminal pH [5].
Using an in vivo microscopic system, we have studied, in addition to measuring the rate of HCO3– secretion using duodenal loop perfusion system, the integrated regulation of mucosal defense factors such as mucosal blood flow, mucus secretion, and enterocyte pHi in response to luminal acid in rat duodenum [2]. Luminal acid is sensed by the ‘capsaicin pathway’, which is comprised of epithelial cell acidification due to in-diffusing luminal acid, and H+ extrusion across the basolateral membrane via the Na+/H+ exchanger-1. The extruded H+ activates the cation channel transient receptor potential vanilloid 1 (TRPV1) on capsaicin-sensitive afferent nerves. Activated afferents release vasoactive mediators such as calcitonin gene-related peptide and nitric oxide. Finally, mucosal blood flow and mucus secretion are increased, followed by cyclooxygenase (COX)-dependent mucus and HCO3– secretion [2,4]. These results demonstrate that the duodenal mucosa senses luminal acidity using epithelial ion transporters and neuronal acid sensors, and that intracellular acidification triggers the enhancement of mucosal defense mechanisms [1].
How does luminal acid acidify the epithelial cells in order to trigger mucosal defense mechanisms? The high level of PCO2, generated in the proximal duodenum, gradually declines in the jejunum [6], consistent with rapid CO2 absorption by the duodenal mucosa. Since the duodenal mucosa has the highest carbonic anhydrase (CA) activity in the GI tract [7], which rapidly equilibrates H+ + HCO3– ↔ CO2 + H2O, we hypothesize that the duodenal mucosa absorbs luminal CO2 effectively by cytosolic and membrane-bound CA activities. Using duodenal loop perfusion with flow-through pH and CO2 electrodes, and simultaneous portal venous blood gas monitoring, we have reported that luminal CO2 is CA-dependently absorbed by the duodenal epithelium with stimulated HCO3– secretion, accompanied by portal venous acidification [8]. Furthermore, CO2-induced intracellular acidification of epithelial cells is also CA-dependent and accompanied by a TRPV1-dependent hyperemic response [9]. These results suggest that luminal H+ is actively absorbed into the epithelium as CO2, which is converted into H+ and HCO3–, facilitated by membrane-bound and cytosolic CAs. Intracellular H+ is extruded via Na+/H+ exchanger-1, and sensed by the ‘capsaicin pathway’. This suggests that luminal H+ and CO2 provide equivalent acid loads, in terms of intracellular acidification, that trigger protective effector mechanisms. The duodenum absorbs luminal H+ secreted by the stomach in order to maintain the acid-base balance between the stomach and duodenum. Acid-base balance between the stomach and duodenum is clinically important, since loss of gastric content by vomiting in the patients with the pyloric obstruction induces acute metabolic alkalosis and hypochloremia [10,11].
High PCO2-induced HCO3– secretion has also been confirmed by Sasaki et al. [12], reporting that CO2-induced HCO3– secretion is differently regulated in the stomach and duodenum. Acid-induced intracellular acidification of the duodenal epithelial cells is also reported by Sjöblom et al. [13], confirming the importance of CA activities in the acid-sensing pathway of the duodenum using knockout mice.
H+-sensitive G-protein-coupled receptors (GPCRs) are also candidates of acid sensors. So far, 4 GPCRs, GPR4, OGR1, TDAG8 and G2A, are the known H+-sensitive GPCRs [14], implicated in the detection of tissue or blood acidosis, although still controversial whether H+ is a receptor ligand or a modifier [15,16]. These GPCRs are also activated by phospholipids, whereas low pH-induced activation of these GPCRs is inhibited by phospholipids. H+-sensitive GPCRs are expressed in the afferent neurons as well as vasculature and immune cells [17,18,19], suggesting that H+-sensitive GPCRs may be involved in mucosal defense mechanisms in the upper GI tract, in addition to the acidosis and inflammation.
pH-Sensitive Surface pH Regulation via Purinergic Signaling
Another pH-sensitive luminal chemosensor is the brush border ecto-enzyme-related signaling system including ATP-P2Y receptor signals with intestinal alkaline phosphatase (IAP) activity in the duodenum [20,21]. At neutral luminal pH, extracellularly, non-lytically released ATP from the epithelial cells is rapidly degraded to adenosine (ADO), which is further degraded to inosine by adenosine deaminase. Once the surface pH is lowered by gastric acid, surface ATP concentration increases due to the accumulation of ATP and/or the stimulated ATP release, according to the decreased IAP activity at acidic pH. The increased surface ATP stimulates P2Y1 receptor on the apical membrane of epithelial cells, and then increases HCO3– secretion. The increased surface HCO3– concentration raises surface pH, close to the optimal pH for IAP. The recovered IAP activity degrades the surface ATP to terminate ATP-P2Y signals. The surface ADO-P1 receptor signal is also present to regulate HCO3– secretion [22]. These studies suggest that IAP acts as a pH sensor to modify the surface ATP concentration and serve negative feedback loop. The mechanisms of ATP-P2Y receptor signals are implicated in other epithelium secreting HCO3–, such as bile ducts, oviduct and bone [23].
Esophageal and Gastric Acid Sensing
Similar to the duodenal acid sensing, the esophageal mucosa also senses luminal acidity as the permeant gas CO2 with help of epithelial and neuronal CA activities and acid sensors, TRPV1 and acid-sensing ion channels (ASICs), in order to maintain the interstitial pH at a physiological level via the hyperemic response to luminal H+/CO2 [1,24]. The concept that CA activity and acid sensors are the essential components of H+/CO2 sensing is supported by the observation that taste of carbonation on the tongue is mediated and sensed by CA activity and an acid sensor [25].
Gastric acid sensing should be separately discussed as intragastric pH monitoring and the mucosal response to back-diffused acid. Intragastric pH monitoring, in terms of physiological gastric acid sensing, may be mediated by the calcium-sensing receptor (CaSR) expressed on gastric endocrine cells []for review, see [26]. This hypothesis is supported by the following observations: extracellular Ca2+ stimulates gastrin release from antral G cells [27]. CaSR is pH-sensitive and stimulated by L-type amino acids [28,29]. Finally, CaSR knockout stomach lacks gastrin release response to luminal pH increase, Ca2+ or peptone [30].
Once pathological acid back-diffuses into subepithelium or submucosa, acid may stimulate acid sensors TRPV1 or ASICs on afferent nerves with COX activation, implicated in not only protective afferent responses, but also noxious sensation conducted to the central nervous system [31,32].
Nutrient Sensing in the Duodenum
Recent molecular studies have identified the structure of specific receptors on the tongue for the basic tastes (sweet, sour, salty, bitter, umami) [33]. These receptors have also been found in the GI tract. In addition to the ‘salty’ taste sensed by epithelial Na+ channels and ‘sourness’ by H+-gated ion channels such as ASIC, the ‘sweet’ receptor heterodimer (T1R2/T1R3) is expressed in the small intestinal mucosa [34,35,36]. Bitter taste receptors of the type 2 taste receptor (T2R) family are also expressed in the GI tract [37]. The expression of these taste receptors in the GI mucosa suggests the need to sense the luminal contents, presumably to detect the presence of nutrients and unfavorable substances, in order to optimize digestion, absorption, secretion, and motility.
Luminal chemosensing has been reported for glucose, bitter substances and fatty acids in the GI tract [35,38,39]. We thus hypothesized that mucosal defense factors may be modulated by luminal nutrients, acting via taste receptors in the duodenum.
Luminal Amino Acid Sensing and Mucosal Defenses
The receptor on the tongue for L-glutamate (L-Glu), which is the primary nutrient conferring umami taste, is a heterodimer of taste receptor type 1 T1R1 and T1R3 [40,41] and/or a metabotropic L-Glu receptor (mGluR) [42,43]. These receptors, which belong to the GPCR superfamily, are localized, along with the specific G protein, α-gustducin in the epithelial cells of the GI tract [34,35,39,44]. Another candidate for L-Glu receptor is CaSR, whose activity is modified by aromatic amino acids [29]. CaSR is also localized in the duodenal epithelial cells [45]. These observations suggest that the mucosa directly senses luminal L-Glu or other amino acids, and may directly or indirectly conduct luminal information to the internal signaling systems. Indeed, luminal L-Glu stimulates gastric vagal afferents through the release of nitric oxide and 5-hydroxytryptamine [46]. Our study suggests that luminal L-Glu enhances mucosal defense mechanisms via multiple L-Glu receptors in the duodenum [47].
Using in vivo microscopic techniques, we have recently reported that luminal L-Glu (0.1–10 mM) dose-dependently increases epithelial pHi and mucus gel thickness, but not blood flow, in rat duodenum [48]. The gastric mucosa also similarly responds to luminal L-Glu [1]. These effects of L-Glu are mediated by capsaicin- and indomethacin-sensitive pathways in the duodenum, suggesting the involvement of capsaicin-sensitive afferent nerves and COX activity, respectively. Co-perfusion of L-Glu and 5′-inosine monophosphate (IMP) increases duodenal HCO3– secretion. Furthermore, pre-perfusion with L-Glu inhibits supraphysiological acid-induced epithelial injury in the duodenum [48], assessed by in vivo in situ propidium iodide staining [49]. These results suggest that luminal L-Glu enhances duodenal mucosal defenses possibly via L-Glu or amino acid receptor.
T1R1/R3 is activated by certain L-amino acids in the mM range with synergistic enhancement by the presence of IMP [40,41], representing the specific characteristic of umami taste [50]. The T1R1/R3 umami receptor and the T1R2/R3 sweet receptor are expressed in the intestinal mucosa [51,52,53]. Since the luminal concentration of free amino acids reaches mM levels (which is the optimal concentration for T1R1/R3), after a protein-rich meal in human jejunum and ileum [54], the presence of amino acid sensing is predicted in the intestinal epithelium.
We have demonstrated that luminal co-perfusion of L-Glu and IMP synergistically stimulates duodenal HCO3– secretion in rat duodenum [48], although L-Glu or IMP alone has a little effect, consistent with the activation of T1R1/R3. Furthermore, other amino acids, such as L-aspartate, L-leucine or L-alanine, increase HCO3– secretion, enhanced by the addition of IMP [48], also supporting the presence of T1R1/R3 in the duodenum. However, these amino acids do not mimic the effects of L-Glu on pHi and mucus gel thickness, suggesting that L-Glu-induced cellular alkalinization and mucus secretion are mediated via different pathways from T1Rs signaling.
We have also demonstrated that luminal perfusion of a mGluR1/5 agonist or mGluR4 agonist increases pHi and mucus gel thickness, and an mGluR4 antagonist inhibits L-Glu-induced increases of pHi and mucus gel thickness [48]. In contrast, mGluR agonists fail to affect duodenal HCO3– secretion, unlike L-Glu. These results suggest that L-Glu enhances duodenal mucosal defenses via mGluR4 activation, separately from T1R-mediated HCO3– secretion.
Calcium Sensing via Calcium-Sensing Receptors
CaSR is another candidate for an L-Glu or amino acid receptor. CaSR is directly activated by extracellular Ca2+ and positively modulated by L-amino acids [29]. Although calcium absorption is believed to occur mostly in the ileum [55], the duodenal mucosa also absorbs luminal Ca2+ via apical transporter TRPV6 (previously known as CaT1) and the intracellular carrier calbindin-D9k [56,57,58]. Calcium absorption and luminal sensing may thus also occur in duodenum.
We have examined the effect of high luminal Ca2+ or a CaSR agonist spermine on pHi, mucus gel thickness, blood flow and HCO3– secretion in rat duodenum. The CaSR agonists acidify epithelial cells, and increase blood flow, mucus gel thickness and HCO3– secretion [48]. These effects of CaSR activation on duodenal mucosal defenses are similar to the effects of luminal acid [1], but unlike the effects of luminal L-Glu. Selective CaSR agonists and antagonists will clarify the role of CaSR in L-Glu-induced mucosal protection. Nevertheless, luminal Ca2+ sensing is present in the duodenum and enhances mucosal defense mechanisms.
Recent Advances in Enteroendocrine GPCRs and Clinical Perspectives
Recent studies implicate the chemosensing GPCRs localized in the enteroendocrine cells in the release of peptide hormones [59]. Especially primary isolated L cells tagged with fluorescent protein-labeled proglucagon express GPR41 and 43, GPR40 and 120, GPR119, and TGR5 (GPR131), whose ligands are short-chain fatty acids, long-chain fatty acids, N-acylethanolamines, and bile acids, respectively [60]. Since K and L cells secrete the incretins gastric inhibitory peptide/glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1), the ligands for the chemosensing GPCRs may be new nutrient-based therapeutic tools for diabetes. α-Linolenic acid increases GLP-1 release via GPR120 [61]. GPR119 agonists are already in clinical trials. GPR40 and 120, and GPR41 are also expressed in cholecystokinin-expressing I cells, and implicated in host adiposity [62]. GPR40 mediates cholecystokinin release in response to luminal long-chain fatty acid in murine duodenum [63]. Activation of TGR5 improves glucose metabolism via GLP-1 release [64]. These studies suggest that luminal fatty acids and endogenous bile acids are sensed by corresponding GPCRs to release peptide hormones regulating energy balance and satiety.
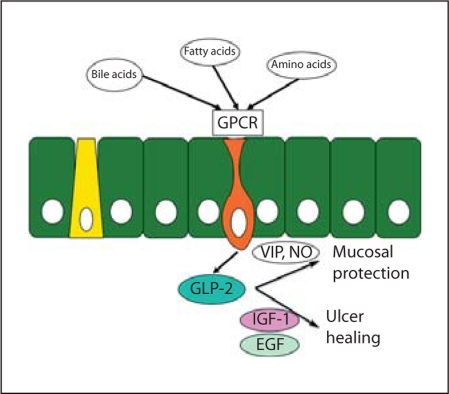
Not only for diabetes and obesity studies, but also for GI research, luminal nutrient-induced gut hormone release may also affect mucosal integrity (fig. 1). Enteroendocrine L cells also release GLP-2, another derivative from proglucagon, which mediates intestinal ion secretion [65] and intestinal cell growth [66], further suggesting that the activation of duodenal chemosensing GPCRs may increase HCO3– secretion. We found that L-Glu/IMP-induced HCO3– secretion was reduced by a GLP-2 receptor antagonist, accompanied by GLP-1 and GLP-2 release, and not by GIP release [67], supporting this hypothesis. The multiple effects of GLP-2 [68] may lead to oral nutritional therapies for short bowel syndrome and intestinal mucosal injury in addition to the metabolic syndrome, especially diabetes mellitus via GLP-1.
Fig. 1.
Luminal chemosensing and mucosal defenses via GLP-2 in the duodenum. The scheme shows our hypothesis that luminal chemicals/nutrients enhance the duodenal mucosal defenses partly via GLP-2 release. Luminal chemicals activate GPCRs expressed on the apical membrane of the enteroendocrine cell, which secretes gut hormones including GLP-2. GLP-2 may stimulate duodenal HCO3– secretion via vasoactive intestinal peptide (VIP) and nitric oxide (NO) pathways. Since GLP-2 is intestinotropic, the stimulated GLP-2 release may enhance mucosal repair via growth factor, such as epidermal growth factor (EGF) and insulin-like growth factor-1 (IGF-1).
Duodenal chemosensing has been implicated in the pathophysiology of functional dyspepsia [69]. Many clinical studies have related abnormal chemosensing to dyspeptic symptoms. The strategy includes the increased stimulus intensity (increased acid secretion or decreased HCO3– secretion), increased expression of chemosensors (epithelial or afferent nerve endings), hypersensitivity of chemosensors (sensitization), and functional modulation of chemosensors (mucosal mediator release). Nevertheless, a recent pilot study of real-time pH monitoring using a wireless pH meter has demonstrated that duodenal acidification is implicated in the onset of epigastric pain in healthy subjects [70], suggesting that duodenal chemosensing may control epigastric sensation via neurohormonal pathways [71]. Studying the physiological roles of luminal chemosensing may help to understand the pathophysiology of dyspeptic symptoms.
In conclusion, the upper GI mucosa ‘tastes’ luminal chemicals such as H+, CO2, amino acids, especially L-Glu, and Ca2+, and enhances mucosal defense mechanisms through specific signaling cascades, including epithelial ion transporters, enzymes and receptors, and capsaicin-sensitive afferent nerves and the COX pathway. The result is the protection of the duodenal mucosa from acid injury. Understanding luminal chemosensory mechanisms may help to identify novel molecular targets for treating and preventing mucosal injury, metabolic disorder and abnormal visceral sensation.
Disclosure Statement
No conflicts of interest to disclose.
Acknowledgements
We thank Drs. Misa Mizumori, Maggie Ham, Chikako Watanabe, Takanari Nakano, Joonho Wang and Takuya Inoue for their research contributions. Supported by a research grant from Ajinomoto Inc., Japan (Y.A.), Investigator-Sponsored Study Program of AstraZeneca IRUSESOM0424 (Y.A.), Department of Veterans Affairs Merit Review Award (J.K.), and NIH-NIDDK R01 DK54221 (J.D.K.).
References
- 1.Akiba Y, Kaunitz JD. Luminal chemosensing and upper gastrointestinal mucosal defenses. Am J Clin Nutr. 2009;90:826S–831S. doi: 10.3945/ajcn.2009.27462U. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Akiba Y, Nakamura M, Nagata H, Kaunitz JD, Ishii H. Acid-sensing pathways in rat gastrointestinal mucosa. J Gastroenterol. 2002;37:133–138. doi: 10.1007/BF03326432. [DOI] [PubMed] [Google Scholar]
- 3.Andersson S. Inhibitory effects of hydrochloric acid in the duodenum on gastrin-stimulated gastric secretion in Heidenhain pouch dogs. Acta Physiol Scand. 1960;50:105–112. doi: 10.1111/j.1748-1716.1960.tb02080.x. [DOI] [PubMed] [Google Scholar]
- 4.Kaunitz JD, Akiba Y. Acid-sensing protective mechanisms of duodenum. J Physiol Pharmacol. 2003;54:19–26. [PubMed] [Google Scholar]
- 5.Kaunitz JD, Akiba Y. Duodenal carbonic anhydrase: mucosal protection, luminal chemosensing, and gastric acid disposal. Keio J Med. 2006;55:96–106. doi: 10.2302/kjm.55.96. [DOI] [PubMed] [Google Scholar]
- 6.Rune SJ, Henriksen FW. Carbon dioxide tensions in the proximal part of the canine gastrointestinal tract. Gastroenterology. 1969;56:758–762. [PubMed] [Google Scholar]
- 7.Sugai N, Okamura H, Tsunoda R. Histochemical localization of carbonic anhydrase in the rat duodenal epithelium. Fukushima J Med Sci. 1994;40:103–117. [PubMed] [Google Scholar]
- 8.Mizumori M, Meyerowitz J, Takeuchi T, Lim S, Lee P, Supuran CT, Guth PH, Engel E, Kaunitz JD, Akiba Y. Epithelial carbonic anhydrases facilitate PCO2 and pH regulation in rat duodenal mucosa. J Physiol. 2006;573:827–842. doi: 10.1113/jphysiol.2006.107581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Akiba Y, Ghayouri S, Takeuchi T, Mizumori M, Guth PH, Engel E, Swenson ER, Kaunitz JD. Carbonic anhydrases and mucosal vanilloid receptors help mediate the hyperemic response to luminal CO2 in rat duodenum. Gastroenterology. 2006;131:142–152. doi: 10.1053/j.gastro.2006.04.018. [DOI] [PubMed] [Google Scholar]
- 10.Gamble JL, Ross SG. The factors in the dehydration following pyloric obstruction. J Clin Invest. 1925;1:403–423. doi: 10.1172/JCI100021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rune SJ. The metabolic alkalosis following aspiration of gastric acid secretion. Scand J Clin Lab Invest. 1965;17:305–310. doi: 10.3109/00365516509077055. [DOI] [PubMed] [Google Scholar]
- 12.Sasaki Y, Aihara E, Ohashi Y, Okuda S, Takasuka H, Takahashi K, Takeuchi K. Stimulation by sparkling water of gastroduodenal HCO3– secretion in rats. Med Sci Monit. 2009;15:BR349–BR356. [PubMed] [Google Scholar]
- 13.Sjöblom M, Singh AK, Zheng W, Wang J, Tuo BG, Krabbenhoft A, Riederer B, Gros G, Seidler U. Duodenal acidity ‘sensing' but not epithelial HCO3– supply is critically dependent on carbonic anhydrase II expression. Proc Natl Acad Sci USA. 2009;106:13094–13099. doi: 10.1073/pnas.0901488106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ludwig MG, Vanek M, Guerini D, Gasser JA, Jones CE, Junker U, Hofstetter H, Wolf RM, Seuwen K. Proton-sensing G-protein-coupled receptors. Nature. 2003;425:93–98. doi: 10.1038/nature01905. [DOI] [PubMed] [Google Scholar]
- 15.Im DS. Two ligands for a GPCR, proton vs. lysolipid. Acta Pharmacol Sin. 2005;26:1435–1441. doi: 10.1111/j.1745-7254.2005.00237.x. [DOI] [PubMed] [Google Scholar]
- 16.Im DS. New intercellular lipid mediators and their GPCRs: an update. Prostaglandins Other Lipid Mediat. 2009;89:53–56. doi: 10.1016/j.prostaglandins.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 17.Huang CW, Tzeng JN, Chen YJ, Tsai WF, Chen CC, Sun WH. Nociceptors of dorsal root ganglion express proton-sensing G-protein-coupled receptors. Mol Cell Neurosci. 2007;36:195–210. doi: 10.1016/j.mcn.2007.06.010. [DOI] [PubMed] [Google Scholar]
- 18.Yang LV, Radu CG, Roy M, Lee S, McLaughlin J, Teitell MA, Iruela-Arispe ML, Witte ON. Vascular abnormalities in mice deficient for the G-protein-coupled receptor GPR4 that functions as a pH sensor. Mol Cell Biol. 2007;27:1334–1347. doi: 10.1128/MCB.01909-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mogi C, Tobo M, Tomura H, Murata N, He XD, Sato K, Kimura T, Ishizuka T, Sasaki T, Sato T, Kihara Y, Ishii S, Harada A, Okajima F. Involvement of proton-sensing TDAG8 in extracellular acidification-induced inhibition of proinflammatory cytokine production in peritoneal macrophages. J Immunol. 2009;182:3243–3251. doi: 10.4049/jimmunol.0803466. [DOI] [PubMed] [Google Scholar]
- 20.Akiba Y, Mizumori M, Guth PH, Engel E, Kaunitz JD. Duodenal brush border intestinal alkaline phosphatase activity affects bicarbonate secretion in rats. Am J Physiol Gastrointest Liver Physiol. 2007;293:G1223–G1233. doi: 10.1152/ajpgi.00313.2007. [DOI] [PubMed] [Google Scholar]
- 21.Mizumori M, Ham M, Guth PH, Engel E, Kaunitz JD, Akiba Y. Intestinal alkaline phosphatase regulates protective surface microclimate pH in rat duodenum. J Physiol. 2009;587:3651–3663. doi: 10.1113/jphysiol.2009.172270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ham M, Mizumori M, Watanabe C, Wang J, Inoue T, Nakano T, Guth PH, Engel E, Kaunitz JD, Akiba Y. Endogenous luminal surface adenosine signaling regulates duodenal bicarbonate secretion in rats. J Pharmacol Exp Ther. 2010;335:607–613. doi: 10.1124/jpet.110.171520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kaunitz JD, Akiba Y. Purinergic regulation of duodenal surface pH and ATP concentration: implications for mucosal defence, lipid uptake and cystic fibrosis. Acta Physiol (Oxf) 2011;201:109–116. doi: 10.1111/j.1748-1716.2010.02156.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Akiba Y, Mizumori M, Kuo M, Ham M, Guth PH, Engel E, Kaunitz JD. CO2 chemosensing in rat oesophagus. Gut. 2008;57:1654–1664. doi: 10.1136/gut.2007.144378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chandrashekar J, Yarmolinsky D, von BL, Oka Y, Sly W, Ryba NJ, Zuker CS. The taste of carbonation. Science. 2009;326:443–445. doi: 10.1126/science.1174601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goo T, Akiba Y, Kaunitz JD. Mechanisms of intragastric pH sensing. Curr Gastroenterol Rep. 2010;12:465–470. doi: 10.1007/s11894-010-0147-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Buchan AM, Squires PE, Ring M, Meloche RM. Mechanism of action of the calcium-sensing receptor in human antral gastrin cells. Gastroenterology. 2001;120:1128–1139. doi: 10.1053/gast.2001.23246. [DOI] [PubMed] [Google Scholar]
- 28.Quinn SJ, Bai M, Brown EM. pH sensing by the calcium-sensing receptor. J Biol Chem. 2004;279:37241–37249. doi: 10.1074/jbc.M404520200. [DOI] [PubMed] [Google Scholar]
- 29.Busque SM, Kerstetter JE, Geibel JP, Insogna K. L-type amino acids stimulate gastric acid secretion by activation of the calcium-sensing receptor in parietal cells. Am J Physiol Gastrointest Liver Physiol. 2005;289:G664–G669. doi: 10.1152/ajpgi.00096.2005. [DOI] [PubMed] [Google Scholar]
- 30.Feng J, Lu M, Anthony S, Petersen CD, Wank SA. The calcium-sensing receptor mediates meal stimulated gastrin secretion. Gastroenterology. 2007;132:A101. [Google Scholar]
- 31.Schicho R, Florian W, Liebmann I, Holzer P, Lippe IT. Increased expression of TRPV1 receptor in dorsal root ganglia by acid insult of the rat gastric mucosa. Eur J Neurosci. 2004;19:1811–1818. doi: 10.1111/j.1460-9568.2004.03290.x. [DOI] [PubMed] [Google Scholar]
- 32.Holzer P. Neural emergency system in the stomach. Gastroenterology. 1998;114:823–839. doi: 10.1016/s0016-5085(98)70597-9. [DOI] [PubMed] [Google Scholar]
- 33.Lindemann B. Receptors and transduction in taste. Nature. 2001;413:219–225. doi: 10.1038/35093032. [DOI] [PubMed] [Google Scholar]
- 34.Dyer J, Salmon KS, Zibrik L, Shirazi-Beechey SP. Expression of sweet taste receptors of the T1R family in the intestinal tract and enteroendocrine cells. Biochem Soc Trans. 2005;33:302–305. doi: 10.1042/BST0330302. [DOI] [PubMed] [Google Scholar]
- 35.Margolskee RF, Dyer J, Kokrashvili Z, Salmon KS, Ilegems E, Daly K, Maillet EL, Ninomiya Y, Mosinger B, Shirazi-Beechey SP. T1R3 and gustducin in gut sense sugars to regulate expression of Na+-glucose cotransporter 1. Proc Natl Acad Sci USA. 2007;104:15075–15080. doi: 10.1073/pnas.0706678104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mace OJ, Affleck J, Patel N, Kellett GL. Sweet taste receptors in rat small intestine stimulate glucose absorption through apical GLUT2. J Physiol. 2007;582:379–392. doi: 10.1113/jphysiol.2007.130906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wu SV, Rozengurt N, Yang M, Young SH, Sinnett-Smith J, Rozengurt E. Expression of bitter taste receptors of the T2R family in the gastrointestinal tract and enteroendocrine STC-1 cells. Proc Natl Acad Sci USA. 2002;99:2392–2397. doi: 10.1073/pnas.042617699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Raybould HE. Nutrient tasting and signaling mechanisms in the gut. I. Sensing of lipid by the intestinal mucosa. Am J Physiol. 1999;277:G751–G755. doi: 10.1152/ajpgi.1999.277.4.G751. [DOI] [PubMed] [Google Scholar]
- 39.Rozengurt E. Taste receptors in the gastrointestinal tract. I. Bitter taste receptors and α-gustducin in the mammalian gut. Am J Physiol Gastrointest Liver Physiol. 2006;291:G171–G177. doi: 10.1152/ajpgi.00073.2006. [DOI] [PubMed] [Google Scholar]
- 40.Nelson G, Chandrashekar J, Hoon MA, Feng L, Zhao G, Ryba NJ, Zuker CS. An amino-acid taste receptor. Nature. 2002;416:199–202. doi: 10.1038/nature726. [DOI] [PubMed] [Google Scholar]
- 41.Zhao GQ, Zhang Y, Hoon MA, Chandrashekar J, Erlenbach I, Ryba NJ, Zuker CS. The receptors for mammalian sweet and umami taste. Cell. 2003;115:255–266. doi: 10.1016/s0092-8674(03)00844-4. [DOI] [PubMed] [Google Scholar]
- 42.Chaudhari N, Landin AM, Roper SD. A metabotropic glutamate receptor variant functions as a taste receptor. Nat Neurosci. 2000;3:113–119. doi: 10.1038/72053. [DOI] [PubMed] [Google Scholar]
- 43.Toyono T, Seta Y, Kataoka S, Kawano S, Shigemoto R, Toyoshima K. Expression of metabotropic glutamate receptor group I in rat gustatory papillae. Cell Tissue Res. 2003;313:29–35. doi: 10.1007/s00441-003-0740-2. [DOI] [PubMed] [Google Scholar]
- 44.San Gabriel AM, Maekawa T, Uneyama H, Yoshie S, Torii K. mGluR1 in the fundic glands of rat stomach. FEBS Lett. 2007;581:1119–1123. doi: 10.1016/j.febslet.2007.02.016. [DOI] [PubMed] [Google Scholar]
- 45.Chattopadhyay N, Cheng I, Rogers K, Riccardi D, Hall A, Diaz R, Hebert SC, Soybel DI, Brown EM. Identification and localization of extracellular Ca2+-sensing receptor in rat intestine. Am J Physiol. 1998;274:G122–G130. doi: 10.1152/ajpgi.1998.274.1.G122. [DOI] [PubMed] [Google Scholar]
- 46.Uneyama H, Niijima A, San GA, Torii K. Luminal amino acid sensing in the rat gastric mucosa. Am J Physiol Gastrointest Liver Physiol. 2006;291:G1163–G1170. doi: 10.1152/ajpgi.00587.2005. [DOI] [PubMed] [Google Scholar]
- 47.Akiba Y, Kaunitz JD. Luminal chemosensing in the duodenal mucosa. Acta Physiol (Oxf) 2011;201:77–84. doi: 10.1111/j.1748-1716.2010.02149.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Akiba Y, Watanabe C, Mizumori M, Kaunitz JD. Luminal L-glutamate enhances duodenal mucosal defense mechanisms via multiple glutamate receptors in rats. Am J Physiol Gastrointest Liver Physiol. 2009;297:G781–G791. doi: 10.1152/ajpgi.90605.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Akiba Y, Furukawa O, Guth PH, Engel E, Nastaskin I, Sassani P, Dukkipatis R, Pushkin A, Kurtz I, Kaunitz JD. Cellular bicarbonate protects rat duodenal mucosa from acid-induced injury. J Clin Invest. 2001;108:1807–1816. doi: 10.1172/JCI12218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sato M, Yamashita S, Ogawa H. Potentiation of gustatory response to monosodium glutamate in rat chorda tympani fibers by addition of 5′-ribonucleotides. Jpn J Physiol. 1970;20:444–464. doi: 10.2170/jjphysiol.20.444. [DOI] [PubMed] [Google Scholar]
- 51.Jang HJ, Kokrashvili Z, Theodorakis MJ, Carlson OD, Kim BJ, Zhou J, Kim HH, Xu X, Chan SL, Juhaszova M, Bernier M, Mosinger B, Margolskee RF, Egan JM. Gut-expressed gustducin and taste receptors regulate secretion of glucagon-like peptide-1. Proc Natl Acad Sci USA. 2007;104:15069–15074. doi: 10.1073/pnas.0706890104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bezencon C, le Coutre J, Damak S. Taste-signaling proteins are coexpressed in solitary intestinal epithelial cells. Chem Senses. 2007;32:41–49. doi: 10.1093/chemse/bjl034. [DOI] [PubMed] [Google Scholar]
- 53.Mace OJ, Lister N, Morgan E, Shepherd E, Affleck J, Helliwell P, Bronk JR, Kellett GL, Meredith D, Boyd R, Pieri M, Bailey PD, Pettcrew R, Foley D. An energy supply network of nutrient absorption coordinated by calcium and T1R taste receptors in rat small intestine. J Physiol. 2009;587:195–210. doi: 10.1113/jphysiol.2008.159616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Adibi SA, Mercer DW. Protein digestion in human intestine as reflected in luminal, mucosal, and plasma amino acid concentrations after meals. J Clin Invest. 1973;52:1586–1594. doi: 10.1172/JCI107335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Marcus CS, Lengemann FW. Absorption of Ca45 and Sr85 from solid and liquid food at various levels of the alimentary tract of the rat. J Nutr. 1962;77:155–160. doi: 10.1093/jn/77.2.155. [DOI] [PubMed] [Google Scholar]
- 56.Bronner F. Recent developments in intestinal calcium absorption. Nutr Rev. 2009;67:109–113. doi: 10.1111/j.1753-4887.2008.00147.x. [DOI] [PubMed] [Google Scholar]
- 57.Balesaria S, Sangha S, Walters JR. Human duodenum responses to vitamin D metabolites of TRPV6 and other genes involved in calcium absorption. Am J Physiol Gastrointest Liver Physiol. 2009;297:G1193–G1197. doi: 10.1152/ajpgi.00237.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Barley NF, Howard A, O'Callaghan D, Legon S, Walters JR. Epithelial calcium transporter expression in human duodenum. Am J Physiol Gastrointest Liver Physiol. 2001;280:G285–G290. doi: 10.1152/ajpgi.2001.280.2.G285. [DOI] [PubMed] [Google Scholar]
- 59.Engelstoft MS, Egerod KL, Holst B, Schwartz TW. A gut feeling for obesity: 7TM sensors on enteroendocrine cells. Cell Metab. 2008;8:447–449. doi: 10.1016/j.cmet.2008.11.004. [DOI] [PubMed] [Google Scholar]
- 60.Reimann F, Habib AM, Tolhurst G, Parker HE, Rogers GJ, Gribble FM. Glucose sensing in L cells: a primary cell study. Cell Metab. 2008;8:532–539. doi: 10.1016/j.cmet.2008.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hirasawa A, Tsumaya K, Awaji T, Katsuma S, Adachi T, Yamada M, Sugimoto Y, Miyazaki S, Tsujimoto G. Free fatty acids regulate gut incretin glucagon-like peptide-1 secretion through GPR120. Nat Med. 2005;11:90–94. doi: 10.1038/nm1168. [DOI] [PubMed] [Google Scholar]
- 62.Samuel BS, Shaito A, Motoike T, Rey FE, Backhed F, Manchester JK, Hammer RE, Williams SC, Crowley J, Yanagisawa M, Gordon JI. Effects of the gut microbiota on host adiposity are modulated by the short-chain fatty-acid binding G-protein-coupled receptor, Gpr41. Proc Natl Acad Sci USA. 2008;105:16767–16772. doi: 10.1073/pnas.0808567105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Liou AP, Lu X, Sei Y, Zhao X, Pechhold S, Carrero RJ, Raybould HE, Wank S. The G-protein-coupled receptor GPR40 directly mediates long-chain fatty acid-induced secretion of cholecystokinin. Gastroenterology. 2010 doi: 10.1053/j.gastro.2010.10.012. (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Thomas C, Gioiello A, Noriega L, Strehle A, Oury J, Rizzo G, Macchiarulo A, Yamamoto H, Mataki C, Pruzanski M, Pellicciari R, Auwerx J, Schoonjans K. TGR5-mediated bile acid sensing controls glucose homeostasis. Cell Metab. 2009;10:167–177. doi: 10.1016/j.cmet.2009.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Baldassano S, Liu S, Qu MH, Mule F, Wood JD. Glucagon-like peptide-2 modulates neurally-evoked mucosal chloride secretion in guinea pig small intestine in vitro. Am J Physiol Gastrointest Liver Physiol. 2009;297:G800–G805. doi: 10.1152/ajpgi.00170.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tsai CH, Hill M, Asa SL, Brubaker PL, Drucker DJ. Intestinal growth-promoting properties of glucagon-like peptide-2 in mice. Am J Physiol. 1997;273:E77–E84. doi: 10.1152/ajpendo.1997.273.1.E77. [DOI] [PubMed] [Google Scholar]
- 67.Wang JH, Akiba Y, Engel E, Guth PH, Kaunitz JD. Umami receptor activation increases duodenal bicarbonate secretion via GLP-2 release in rats. Gastroenterology. 2010;138:S405. doi: 10.1124/jpet.111.184788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Dubé PE, Brubaker PL. Frontiers in glucagon-like peptide-2: multiple actions, multiple mediators. Am J Physiol Endocrinol Metab. 2007;293:E460–E465. doi: 10.1152/ajpendo.00149.2007. [DOI] [PubMed] [Google Scholar]
- 69.Van Boxel OS, Ter Linde JJ, Siersema PD, Smout AJ. Role of chemical stimulation of the duodenum in dyspeptic symptom generation. Am J Gastroenterol. 2010;105:803–811. doi: 10.1038/ajg.2010.100. [DOI] [PubMed] [Google Scholar]
- 70.Tanimura T, Adachi K, Furuta K, Ohara S, Morita T, Koshino K, Miki M, Kinoshita Y. Usefulness of catheterless radiotelemetry pH monitoring system to examine the relationship between duodenal acidity and upper-GI symptoms. J Gastroenterol Hepatol. 2011;26:98–103. doi: 10.1111/j.1440-1746.2010.06468.x. [DOI] [PubMed] [Google Scholar]
- 71.Akiba Y, Kaunitz JD. Duodenal chemosensing: master control for epigastric sensation? J Gastroenterol Hepatol. 2011;26:6–7. doi: 10.1111/j.1440-1746.2010.06580.x. [DOI] [PubMed] [Google Scholar]