Abstract
Introduction:
The aim of this study was to investigate changes in the relative proportion of hardcore smokers (HCS) in Norway for the years 1996–2009.
Methods:
Data were derived from Statistics Norway’s annually cross-sectional representative samples of the adult population. The total sample size of smokers each year was between 250 and 500. The outcome measure was HCS, defined by their intention not to quit smoking and absence of attempts to quit during the last 12 months. Logistic regression analysis was conducted to estimate the association between time (survey year) and the number of HCS.
Results:
We identified three groups of smokers: occasional smokers, daily non-HCS, and HCS. The relative proportion of HCS declined in the period 1996–2009, from 30% to 23%. A model adjusted for gender, age, educational level, and the use of snus (smokeless tobacco) showed the same downward trend.
Conclusions:
Within this sample of Norwegian smokers, the relative share of HCS is not increasing. This knowledge is important for tobacco prevention policy. The result does not support a hardening hypothesis regarding changes in the size of the group of HCS. Further analysis is needed to investigate individual resistance to smoking cessation.
Introduction
Cigarette smoking is declining in Norway, a trend shown both in population surveys and official sales statistics of smoking tobacco products (M. Lund & Lindbak, 2007; Norwegian Institute for Alcohol and Drug Research, 2010). Daily smoking has dropped continually since 1973 among men and since 2000 among women. A gender convergence in daily smoking occurred in the late 1990s and has been present since (Norwegian Directorate of Health, 2010). The amount of smoking tobacco consumed annually per adult decreased from 2 to 1.5 kg for men and from 1.6 to 1.3 kg for women in the period 1996–2007 (K. E. Lund, Lund, & Bryhni, 2009). From 1996 to 2009, daily smoking among 16–24 years dropped from 30% to 15% (Statistics Norway, 2007). However, in the adult population, there has been no significant decline in smoking rates during the most recent period, causing speculation that a smoking prevalence plateau has been reached.
The Norwegian Tobacco Act came into force in 1975, with the most important regulations being a ban on tobacco advertising and age restrictions for buying tobacco. Since then, several tobacco control measures have been introduced. At present, regulatory restrictions include an age limit of 18 years for purchasing tobacco, warning labels on tobacco products, a ban on smoking in bars and restaurants from 2004, and the requirement for all retailers to put tobacco products out of sight for customers from 2010. Norway is considered to have a strict tobacco prevention policy, ranking as the fourth country on a European tobacco control scale (Joossens & Raw, 2006, 2007). However, in spite of having a strict tobacco prevention policy, 30% of Norwegian adults still smoke daily or occasionally.
The concept of hardcore smokers (HCS) and the hardening hypothesis are essential in this study. HCS refer to a group of smokers who probably would not quit smoking. Studies that have analyzed HCS at an individual level have found that HCS are distinct from other smokers. They are more likely to be male (Emery, Gilpin, Ake, Farkas, & Pierce, 2000; Jarvis, Wardle, Waller, & Owen, 2003; MacIntosh & Coleman, 2006), to be older (Emery et al., 2000; Jarvis et al., 2003), and to have a low level of education and income (Augustson & Marcus, 2004; Emery et al., 2000; Ferketich et al., 2009; Jarvis et al., 2003). The size of the HCS group has also been addressed. HCS constitute 5% of Californian smokers (Emery et al., 2000), 13.7% of all U.S. smokers (Augustson & Marcus, 2004), and 16% of smokers in England (Jarvis et al., 2003). HCS have some similarities with so-called precontemplators in the Transtheoretical Model, which are defined as smokers with no quit intention during the next six months (Velicer Rossi, Prochaska, & DiClemente, 1996). About 65% of the remaining smokers in Europe and United States are precontemplators (Meyer, Rumpf, Schumann, Hapke, & John, 2004). Early smoking onset, high consumption of cigarettes per day, and prolonged smoking are other characteristics of HCS, factors that could indicate high nicotine dependence among this group (Augustson & Marcus, 2004). Studies using Fagerström Test for Nicotine Dependence (FTND) found higher FTND scores among smokers not willing to quit compared with other smokers (Haukkala, Laaksonen, & Uutela, 2001). A higher proportion of HCS smoke their first cigarette within 30 min after awakening compared with other smokers (Emery et al., 2000).
The association between nicotine dependence and smoking cessation has been widely addressed in tobacco research. A selection hypothesis has been introduced, stating that smokers with low nicotine dependence level quit at a higher speed, leaving behind a group of smokers who are highly nicotine dependent (Hughes, 1993). The idea that as smoking prevalence in a society decreases, the remaining smokers will become more hardcore, is referred to as the “hardening hypothesis” (Warner & Burns, 2003). One study supporting the hardening hypothesis compared the prevalence of smoking in different countries with the subsequent level of nicotine dependence in the countries (Fagerstrom & Furberg, 2008). This study found an inverse relationship between FTND scores and smoking prevalence across countries. The finding that countries with a low prevalence of smoking had high scores on the nicotine dependence scale was interpreted as a result of higher smoking cessation activity among the low-dependent smokers. Other studies giving support to the hardening hypothesis investigated smoking cessation success in clinical settings and found lower success rates over time in both interventions using pharmacotherapy and behavioral therapy as smoking cessation aids (Irvin & Brandon, 2000; Irvin, Hendricks, & Brandon, 2003).
However, other studies investigating the hardening hypothesis have not supported the hypothesis. In the monograph “Those who continue to smoke,” the overall conclusion was that hardening among the remaining smokers in the United States is probably not the case (National Cancer Institute, 2003). This conclusion is supported by proponents of a softening hypothesis, based on the idea that tobacco intervention at a population level would influence all smokers (Chaiton, Cohen, & Frank, 2008). One premise for the nicotine dependence explanation to be true is the need for replacement of new highly nicotine-dependent smokers to maintain a high nicotine dependence level on average. This situation is not likely to occur since most new smokers consist of both high- and low-dependent smokers (Warner & Burns, 2003).
The hardening hypothesis focuses on nicotine dependence as an explanation, but psychosocial factors have also been outlined as important factors for a potential hardening of the remaining smoking population (Hughes, 2003). Accumulation of other health risk factors such as mental illness or accumulation of unhealthy lifestyle factors could make it harder for smokers to quit (Haukkala et al., 2001; Lasser et al., 2000). A recently published study from Australia found that psychological distress and social disadvantage were more common among smokers than among nonsmokers, but there was no evidence that this relationship was getting stronger among smokers over time (Mathews, Hall, & Gartner, 2010). Other explanations for a potential hardening have been related to changes in the social composition of the remaining smokers, where a high proportion of smokers with lower socioeconomic status is expected to have a harder time quitting (Warner & Burns, 2003).
There is no established definition of HCS (Costa et al., 2010), but one often cited definition is “a daily, long-term smoker who is unable or unwilling to quit and who is likely to remain so even when possessing extensive knowledge about the hazards of smoking and when confronting substantial social disapprobation of smoking” (Warner & Burns, 2003). The definition of HCS used in our study relates both to the “unwillingness” and the “unableness” of Warner and Burn’s construct of HCS. The absence of recent quit attempts, lack of intention to quit in next six months, and a belief in persistent smoking in five years could not only be related to an unwillingness to quit smoking but might also be based on the smokers belief that quitting smoking most probably would fail based on their experiences and/or low self-efficacy. The definition used does not cover those who are “unable” to quit due to nicotine dependence or other individual or social factors that could reflect a smoker’s incapability toward smoking cessation. The aim of the study was to investigate relative changes in the proportion of HCS in the population of smokers in the time period 1996–2009 in Norway. The relative size of HCS over time was used as an indication of a possible hardening of the remaining population of smokers.
Methods
Samples and Procedures
We used data from annual cross-sectional surveys of tobacco behavior, comprising a representative sample of the adult Norwegian population (16+ years). Data were collected by Statistics Norway and the Norwegian Directorate of Health, and samples were drawn from Statistics Norway’s own population database, which is updated every month with the National Population Register, a register that covers almost 100% of the Norwegian population. The samples were adjusted for gender and age in accordance with the population numbers for each survey year. Smoking behavior was one of the several topics in the surveys, and correspondence between the gross and the net samples for the variables related to smoking is not known. The data were collected from a combination of face-to-face and telephone interviews from 1996 to 2000. From 2001, all data have been collected by telephone interviews. The original annual sample was N = 2,000 minus a small sample each year which was not eligible due to death or emigration (varied between 13 and 32 respondents). The response rate varied from 56.5% in 2000 to 73% in 2002 (Table 1). The wordings of the questions for the variables used in this study were identical for every survey year. The study sample was restricted to daily smokers 25–74 years. Respondents below the age of 25 were excluded because they may still be in a smoking initiation phase, a condition taken into consideration in other studies of HCS (Augustson & Marcus, 2004; Emery et al., 2000).
Table 1.
Sample Size 25–74 Years, Response Rate, Numbers and Prevalence of Daily Hardcore Smokers (HCS), Daily Non-Hardcore Smokers, and Occasional Smokers by Survey Year
| Survey year | N, 25–74 years | Response rate, % (total sample) | Number and prevalence (%) of daily HCS | Number and prevalence (%) of daily non-HCS | Number and prevalence (%) of occasional smokers |
| 1996 | 1,112 | 68 | 155 (14) | 233 (21) | 119 (11) |
| 1997 | 1,105 | 69 | 171 (16) | 215 (20) | 107 (10) |
| 1998 | 1,091 | 67 | 170 (16) | 196 (18) | 88 (8) |
| 1999 | 948 | 59 | 146 (15) | 162 (17) | 99 (11) |
| 2000 | 900 | 57 | 109 (12) | 167 (19) | 81 (9) |
| 2001 | 1,017 | 64 | 135 (13) | 194 (19) | 102 (10) |
| 2002 | 1,175 | 73 | 138 (12) | 206 (18) | 93 (8) |
| 2003 | 1,054 | 66 | 97 (9) | 195 (19) | 91 (9) |
| 2004 | 1,062 | 68 | 85 (8) | 190 (18) | 86 (8) |
| 2005 | 986 | 65 | 55 (7) | 164 (17) | 82 (8) |
| 2006 | 980 | 62 | 92 (9) | 147 (15) | 64 (7) |
| 2007 | 1,029 | 63 | 73 (7) | 165 (16) | 82 (8) |
| 2008 | 954 | 57 | 67 (7) | 127 (13) | 64 (7) |
| 2009 | 977 | 58 | 54 (6) | 145 (15) | 55 (6) |
| Total | 14,390 | 1,547 (11) | 2,506 (18) | 1,213 (8) |
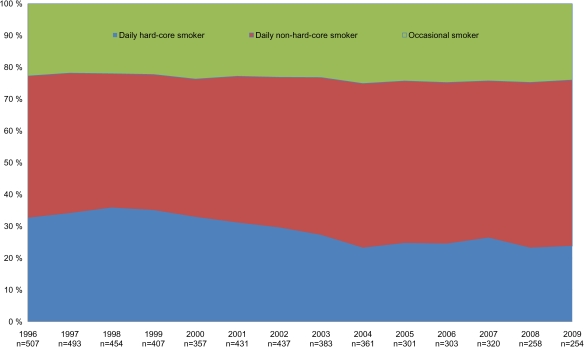
Measures
We measured smoking status in two steps. The first question was: “Do you sometimes smoke?” Those who answered yes were then asked: “Do you smoke daily or occasionally?” All daily smokers were split into two separate groups. The HCS group was defined by using three different questions about smoking intention and previous attempts to quit. The first question was: “Are you considering to quit during the next six months?” The second question covered smokers’ beliefs about future smoking: “Try to predict your smoking status in five years from now. Which statement fits your beliefs best?” Four answers were available: (a) “I will definitely be a daily smoker,” (b) “I will probably be a daily smoker,” (c) “I will probably not be a daily smoker,” and (d) “I will definitely not be a daily smoker.” The third question was: “Have you tried to quit smoking during the latest 12 months?” All daily smokers with no quit attempt during the previous year, no intention to quit during the next six months, and a belief in continued smoking status in five-year time (Answers 1 and 2, including those who answered “don’t know” regarding future smoking) were defined as daily HCS. All other daily smokers were defined as daily non-HCS. The third group was defined as occasional smokers (Figure 1). In the analysis shown in Table 2, non-HCS and occasional smokers were merged as all other smokers.
Figure 1.
Relative share of daily hardcore smokers (HCS), daily non-HCS, and occasional smokers in the population of smokers, 25–74 years. 1996–2009. Three years moving average.
Table 2.
Crude OR and AOR with 95% CI for Being a Daily Hardcore Smoker by Survey Year, Gender, Age, Education, and Snus Use
| Predictor variables | Daily hardcore smoker vs. all other smokers |
||
| n/N | OR (95% CI) | AOR (95% CI) | |
| Gender | |||
| Female | 736/2,591 | 1.00 | 1.00 (ref.) |
| Male | 811/2,675 | 1.10 (0.97–1.24) | 1.16 (1.02–1.31) |
| Age group, years | |||
| 25–38 | 432/1,941 | 1.00 | 1.00 |
| 39–52 | 552/1,916 | 1.41 (1.22–1.64) | 1.39 (1.19–1.61) |
| 53–74 | 563/1,409 | 2.33 (2.00–2.70) | 2.21 (1.89–2.58) |
| Education level | |||
| High | 204/1,100 | 1.00 | 1.00 (ref.) |
| Low | 1,317/4,051 | 2.12 (1.79–2.50) | 2.01 (1.70–2.38) |
| Use snus daily or occasionally | |||
| No | 1,479/4,864 | 1.00 | 1.00 |
| Yes | 68/397 | 0.47 (0.36–0.62) | 0.54 (0.40–0.72) |
| Survey year | |||
| 1996/1997 | 326/1,000 | 1.00 | 1.00 (ref.) |
| 1998/1999 | 316/861 | 1.20 (0.99–1.45) | 1.25 (1.02–1.52) |
| 2000/2001 | 244/788 | 0.93 (0.76–1.13) | 0.92 (0.75–1.13) |
| 2002/2003 | 235/820 | 0.83 (0.70–1.02) | 0.81 (0.66–1.00) |
| 2004/2005 | 140/662 | 0.55 (0.44–0.70) | 0.55 (0.43–0.70) |
| 2006/2007 | 165/623 | 0.75 (0.60–0.93) | 0.71 (0.57–0.89) |
| 2008/2009 | 121/512 | 0.64 (0.50–0.82) | 0.59 (0.40–0.72) |
| Survey year (1–7) | 0.90 (0.88–0.93) | ||
Note. Daily and occasional smokers aged 25–74 years; N = 5,266. AOR = adjusted odds ratio; OR = odds ratio; n = number of hardcore smokers in each category; N = total number in the category.
The main independent variable was survey year, as a measure of time. In order to aid the presentation of the results, survey years were pooled in pairs and used as a categorical variable in the logistic regression analysis. We made adjustments for gender, age, and education since these variables were considered to be confounding variables based on earlier research on HCS. We also included use of smokeless tobacco (snus) as an independent variable to detect possible association between hardcore smoking and double use of tobacco. Age was grouped by using the cutoff point of three equal groups. We dichotomized information about highest completed education into higher education, which refers to completed university or college education (ranging from minimum 14 years in school), and lower education, which refers to completed primary or secondary school education. Those without any formal education were categorized as lower educated (n = 12).
Data Analysis
We analyzed the data in two ways. First, we used three-year moving averages to present the relative proportion of HCS, daily non-HCS, and occasional smokers in the population of all smokers for the years 1996–2009 (Figure 1). Second, we used logistic regression analysis to estimate the association between HCS and survey years, with adjustments for gender, age, educational level, and use of snus. The analysis shows crude odds ratio (OR) and adjusted odds ratios for hardcore smoking (Table 2). In the multivariate analyses, we entered all the independent variables into the model simultaneously. We tested all the independent variables for possible interaction with survey year. The interaction terms are not presented in the table, as there was no evidence of interaction with survey years. We calculated all the OR with a 95% CI.
Results
The percentage of daily smokers who reported no to quit attempt last year was 79.0%, 57.2% reported no quit intention next six months, and 48.7% stated a future belief in continued smoking. Those daily smokers who fulfilled all the three criteria defining HCS comprise 29.4% of the total sample of smokers for the years 1996–2009 (Table 1). The relative size of the HCS group declined in the study period 1996–2009 (Figure 1). At the beginning of the survey period, from 1996 until 2000, HCS constituted approximately 30% of the population of smokers, with a peak in 1998. After this period, the proportion of HCS decreased to 23% in 2004, the lowest observed level. After 2004, the percentage of HCS has been stable at 24%–25%.
The downward trend in hardcore smoking was confirmed in the logistic regression analysis (Table 2). We used 1996/1997 as the reference category for calculating the OR for being a HCS for the following survey years. We calculated crude ORs between HCS and years. This showed a steady decline in the ORs from 2000/2001. There was a significant increase in OR for hardcore smoking from the reference years to the next years 1998/1999, reflecting the peak observed in Figure 1. The crude OR was only significant for the years 2004/2005, 2006/2007, and 2008/2009 when compared with the reference years 1996/1997. Using survey year as a continuous variable (seven measure points) gave a significant downward trend. The multivariate model adjusted for gender, age, education, and snus use gave approximately the same OR for being a HCS as the bivariate analysis. No significant interaction terms were detected between survey year and the confounding variables gender, age, educational level, or snus. Increasing age, being male, and having low educational level showed higher ORs for being a HCS (Table 2).
Discussion
In the present study, we have shown that there is a downward trend in HCS relatively to other smokers in the period 1996–2009. Daily smokers who have no intention to quit in both the short term and the long term and who have made no attempts to quit have become more and more rare during the survey period. In this study, 24% of all smokers were categorized as HCS in 2009. This estimate of HCS is different from the estimates in England in 1994–1997 (16%) and in a national U.S. sample from 1998 to 1999 (13.7%; Augustson & Marcus, 2004; Jarvis et al., 2003). One possible reason is differences in the definition of HCS. The definition used in this study does not include prolonged smoking during the last five years or daily cigarette consumption.
The results from this study do not support a hardening hypothesis, if hardening is defined as increased unwillingness or unableness of the remaining smokers to quit smoking. An alternate hypothesis of softening rather than hardening has been highlighted, based on upstream tobacco prevention policies that influence the whole population of smokers (Chaiton et al., 2008). By using Geoffrey Rose’s epidemiological perspective of the “curve shift” (Rose, 2001), the potential of population tobacco control intervention to move all smokers in a “smoking cessation direction” is highlighted. An increasing proportion of cessation prone smokers, as found in this study, could be interpreted as a result of intensified tobacco control interventions. One U.S. study comparing state-level prevalence with smoking cessation found higher cessation activity in states where smoking prevalence was the lowest (Burns, Major, Anderson, & Vaughn, 2003).
Several tobacco control interventions have taken place in Norway during the study period, especially in the second half of the period. Several antismoking media campaigns were launched between 2003 and 2006 with high awareness rates (K. E. Lund, 2009). Antismoking media campaigns are designed to influence beliefs, attitudes, and behavior, and there is strong evidence for their benefits in tobacco control (Wakefield, Loken, & Hornik, 2010). Media campaigns have the potential to influence norms regarding smoking, and an unfavorable climate for smoking makes smokers more willing to quit (Kim & Shanahan, 2003). On June 1, 2004, Norway implemented a total ban on smoking in bars and restaurants. Before the implementation, a media campaign drew attention to nonsmokers’ rights and employees’ protection from passive smoking. A drop in the relative proportion of HCS was observed a few months after the ban was implemented, as shown in Figure 1. A separate analysis was performed (not shown) to detect whether the drop in the percentage of HCS was to be found mainly from changes in intention to quit smoking in the next six months, changes in quit attempts last year or changes in the smokers belief about own future smoking. The results revealed that the drop in 2004 was due to increased smoking cessation attempts. Results from Scotland also support the hypothesis that a ban on smoking may influence intention to quit through changing social norms (Brown, Moodie, & Hastings, 2009).
Warner and Burns (2003) define the hardening hypothesis as an average decrease in the ability to quit smoking, and they point out that a sizeable group of HCS may be identified without finding evidence for hardening. Studies on HCS published to date have measured the size of the group at a single point in time. To our knowledge, this is the first study identifying HCS and the relative proportion of this group over time. It is expected that a decreasing relative proportion of HCS over time would influence the average desire to quit in the population of daily smokers. But whether the downward trend in HCS influences the ability to quit among the remaining smokers on average is unknown.
Some proponents of the hardening hypothesis emphasize nicotine dependence as the root cause for the hardening mechanism (Fagerstrom & Furberg, 2008), but measures of nicotine dependence have also shown diverging results for predicting successful smoking cessation. Higher cessation reports are found among those with a low score and a high score on the Heaviness of Smoking Index compared with medium scores (Chaiton, Cohen, McDonald, & Bondy, 2007). An alternative understanding of the hardening hypothesis could be that remaining smokers are more nicotine dependent now because of dual or triple use of nicotine products, like smokeless tobacco (snus) and/or nicotine replacement therapy in combination with cigarette smoking. The prevalence of double use of tobacco is reported to be low in Norway, 4.5% of the adult population (Norwegian Directorate of Health, 2010). The logistic regression analysis in this study showed that the OR for being HCS was significantly lower for those who use snus daily or occasionally, indicating that dual use is not a HCS phenomenon.
Other explanations of the hardening hypothesis highlight changes in the social composition of the remaining population of smokers. These changes may mean that it is harder to quit today than previously (Warner & Burns, 2003). One such factor is the strong association between smoking and low socioeconomic position found in Northern Europe, including Norway (K. E. Lund & Lund, 2005; M. Lund & Lund, 2005; Schaap, van Agt, & Kunst, 2008). In this study, we found higher odds for being a HCS among smokers with a low level of education but no indication for an increasing association over time (no significant interaction between education and survey year). Low education or socioeconomic position is associated with lower smoking success rates (Gilman, Abrams, & Buka, 2003; Kotz & West, 2009; Reid, Hammond, & Driezen, 2010). Explanations for these differences may be found in the experience of socioeconomic hardship and deprivation (Layte & Whelan, 2009).
Preventing smoking behavior by using population intervention strategies could also have some unintended consequences with relevance for the hardening versus softening debate. Repeated exposure of an antismoking message over a long time could desensitize smokers and lead to a boomerang effect where the target group react in the opposite way to the intended response (Hyunyi & Salmon, 2007). Recent studies have focused on the increasing social denormalization of smoking, which is defined as strategies that seeks to change the norms around using tobacco, making tobacco use an abnormal behavior (Hammond, Fong, Zanna, Thrasher, & Borland, 2006). Negative consequences of denormalization have been outlined, such as increased social stigma toward smokers (Stuber, Galea, & Link, 2008) and that increasing stigma would exacerbate the existing social inequality in smoking (Bell, Salmon, Bowers, Bell, & McCullough, 2010). Such a boomerang effect could result in an increasing relative proportion of HCS over time and/or hide a hardening effect among remaining smokers by increasing psychological reactance and hostility toward changing their smoking behavior.
Strengths and Limitations of the Study
The strength of this study was the sample’s representativeness for the adult population in Norway. Another unique possibility with these data was the ability to define HCS for 14 separate survey years and to observe the development of the group over time. In this study, we have used a somewhat different definition of HCS than earlier published studies on this subject. We find the inclusion of future belief about smoking as strengthening the concept of HCS. The study’s limitations are first of all the lack of a valid measure of nicotine dependence. FTND scores are only available from the survey year 2005 and onwards and were therefore not included in this study. The association between HCS and nicotine dependence has been highlighted in other studies (Emery et al., 2000). The second limitation deals with the tendency of decreasing response rate by time. Even though the latest surveys response at 58% is considered acceptable, we lack information about the nonresponse group. Nonresponse bias regarding smoking status is not known. The only available nonresponse analysis is on known variables as gender, age, and region (Statistics Norway, 2007). Social desirability bias is also a possibility, where smokers exaggerate their intention to quit, conforming to the no-smoking norm. If such a mechanism is present, it would lead to an underestimation of HCS. At last, the decreasing pool of smokers over time gives small number of cases and limits the possibility for detailed analysis.
Funding
The present study was supported by the Research Program on Public Health (FOLKEHELSE) of the Research Council of Norway, project no.190443 “Tobacco and the social inequality gap,” and from Norwegian Institute for Alcohol and Drug Research.
Declaration of Interests
None declared.
Acknowledgments
Thanks to the Norwegian Directorate for Health for initiating the survey, Statistics Norway for collecting them, and Norwegian Social Science Data Service for making data available. Neither of the institutes above is responsible for the analysis or interpretations in this article.
References
- Augustson EM, Marcus SE. Use of the Current Population Survey to characterize subpopulations of continued smokers: A national perspective on the “hardcore” smoker phenomenon. Nicotine & Tobacco Research. 2004;6:621–629. doi: 10.1080/14622200410001727876. doi:10.1080/14622200410001727876. [DOI] [PubMed] [Google Scholar]
- Bell K, Salmon A, Bowers M, Bell J, McCullough L. Smoking, stigma and tobacco denormalization: Further reflections on the use of stigma as a public health tool. A commentary on Social Science & Medicine's stigma, prejudice, discrimination and health special issue (67: 3) Social Science & Medicine. 2010;70:795–799. doi: 10.1016/j.socscimed.2009.09.060. doi:10.1016/j.socscimed.2009.09.060. [DOI] [PubMed] [Google Scholar]
- Brown A, Moodie C, Hastings G. A longitudinal study of policy effect (smoke-free legislation) on smoking norms: ITC Scotland/United Kingdom. Nicotine & Tobacco Research. 2009;11:924–932. doi: 10.1093/ntr/ntp087. doi:10.1093/ntr/ntp087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns D, Major J, Anderson C, Vaughn J. Changes in cross-sectional measures of cessation, numbers of cigarettes smoked per day, and time to first cigarette-California and national data. 2003. (Monograph No. 15) Those Who Continue to Smoke. Is Achieving Abstinence Harder and Do We Need to Change Our Interventions? U.S. Department of Health and Human Services, National Institute of Health, National Cancer Institute. [Google Scholar]
- Chaiton MO, Cohen JE, Frank J. Population health and the hard core smoker. Journal of public health policy. 2008;29:307–318. doi: 10.1057/jphp.2008.14. doi:10.1057/jphp.2008.14Article. [DOI] [PubMed] [Google Scholar]
- Chaiton MO, Cohen JE, McDonald PW, Bondy SJ. The heaviness of smoking index as a predictor of smoking cessation in Canada. Addictive Behaviors. 2007;32:1031–1042. doi: 10.1016/j.addbeh.2006.07.008. doi:10.1016/j.addbeh.2006.07.008. [DOI] [PubMed] [Google Scholar]
- Costa ML, Cohen JE, Chaiton MO, Ip D, McDonald P, Ferrence R. “Hardcore” definitions and their application to a population-based sample of smokers. Nicotine & Tobacco Research. 2010;12:860–864. doi: 10.1093/ntr/ntq103. doi:10.1093/ntr/ntq103. [DOI] [PubMed] [Google Scholar]
- Emery S, Gilpin EA, Ake C, Farkas AJ, Pierce JP. Characterizing and identifying “hard-core” smokers: Implications for further reducing smoking prevalence. American Journal of Public Health. 2000;90:387–394. doi: 10.2105/ajph.90.3.387. doi:10.2105/AJPH.90.3.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fagerstrom KO, Furberg H. A comparison of the Fagerstrom Test for Nicotine Dependence and smoking prevalence across countries. Addiction. 2008;103:841–845. doi: 10.1111/j.1360-0443.2008.02190.x. doi:10.1111/j.1360-0443.2008.02190.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferketich AK, Gallus S, Colombo P, Pacifici R, Zuccaro P, La Vecchia C. Hardcore smoking among Italian men and women. European Journal of Cancer Prevention. 2009;18:100–105. doi: 10.1097/CEJ.0b013e32830c8d98. doi:10.1097/CEJ.0b013e32830c8d98. [DOI] [PubMed] [Google Scholar]
- Gilman SE, Abrams DB, Buka SL. Socioeconomic status over the life course and stages of cigarette use: Initiation, regular use, and cessation. Journal of Epidemiology and Community Health. 2003;57:802–808. doi: 10.1136/jech.57.10.802. doi:10.1136./jech.57.10.802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammond D, Fong GT, Zanna MP, Thrasher JF, Borland R. Tobacco denormalization and industry beliefs among smokers from four countries. [Article] American Journal of Preventive Medicine. 2006;31:225–232. doi: 10.1016/j.amepre.2006.04.004. doi:10.1016/j.amepre.2006.04.004. [DOI] [PubMed] [Google Scholar]
- Haukkala A, Laaksonen M, Uutela A. Smokers who do not want to quit smoking—Is consonant smoking related to lifestyle and socioeconomic factors? Scandinavian Journal of Public Health. 2001;29:226–232. doi:10.1177/14034948010290031401. [PubMed] [Google Scholar]
- Hughes JR. Pharmacotherapy for smoking cessation: Unvalidated assumptions, anomalies, and suggestions for future research. Journal of Consulting and Clinical Psychology. 1993;61:751–760. doi: 10.1037//0022-006x.61.5.751. doi:10.1037/0022-006x.61.5.751. [DOI] [PubMed] [Google Scholar]
- Hughes JR. The case for hardening of the target. 2003. (Monograph No. 15)Those Who Continue to Smoke. Is Achieving Abstinence Harder and Do We Need to Change Our Interventions? U.S. Department of Health and Human Services, National Institute of Health, National Cancer Institute. Retrieved from http://cancercontrol.cancer.gov/tcrb/monographs/15/monograph15-front.pdf. [Google Scholar]
- Hyunyi C, Salmon CT. Unintended effects of health communication campaigns. Journal of Communication. 2007;57:293–317. doi:10.1111/j.1460-2466.2007.00344.x. [Google Scholar]
- Irvin JE, Brandon TH. The increasing recalcitrance of smokers in clinical trials. Nicotine & Tobacco Research. 2000;2:79–84. doi: 10.1080/14622200050011330. doi:10.1080/14622200050011330. [DOI] [PubMed] [Google Scholar]
- Irvin JE, Hendricks PS, Brandon TH. The increasing recalcitrance of smokers in clinical trials II: Pharmacotherapy trials. Nicotine & Tobacco Research. 2003;5:27–35. doi: 10.1080/1462220031000070534. doi:10.1080/1462220031000070534. [DOI] [PubMed] [Google Scholar]
- Jarvis MJ, Wardle J, Waller J, Owen L. Prevalence of hardcore smoking in England, and associated attitudes and beliefs: Cross sectional study. British Medical Journal. 2003;326:1061. doi: 10.1136/bmj.326.7398.1061. doi:10.1136/bmj.326.7398.1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joossens L, Raw M. The Tobacco Control Scale: A new scale to measure country activity. Tobacco Control. 2006;15:247–253. doi: 10.1136/tc.2005.015347. doi:10.1136/tc.2005.015347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joossens L, Raw M. Progress in tobacco control in 30 European countries, 2005–2007. 2007, October. Paper presented at the 4th European conference Tobacco or Health, Basel, Switzerland. [Google Scholar]
- Kim SH, Shanahan J. Stigmatizing smokers: Public sentiment toward cigarette smoking and its relationship to smoking behaviors. Journal of Health Communication. 2003;8:343–367. doi: 10.1080/10810730305723. doi:10.1080/10810730390223371. [DOI] [PubMed] [Google Scholar]
- Kotz D, West R. Explaining the social gradient in smoking cessation: It's not in the trying, but in the succeeding. Tobacco Control. 2009;18:43–46. doi: 10.1136/tc.2008.025981. doi:10.1136/tc.2008.025981. [DOI] [PubMed] [Google Scholar]
- Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness: A population-based prevalence study. Journal of the American Medical Association. 2000;284:2606–2610. doi: 10.1001/jama.284.20.2606. doi:10.1001/jama.284.20.2606. [DOI] [PubMed] [Google Scholar]
- Layte R, Whelan CT. Explaining social class inequalities in smoking: The role of education, self-efficacy, and deprivation. European Sociological Review. 2009;25:399–410. doi:10.1093/Esr/Jcn022. [Google Scholar]
- Lund KE. Tobacco-free society or tobacco harm reduction? Which objective is best for the remaining smokers in Scandinavia? Oslo, Norway: Norwegian Institute for Alcohol and Drug Research, SIRUS; 2009. SIRUS report. Retrieved from http://www.sirus.no/filestore/Import_vedlegg/sirusrap.6.09.eng.pdf. [Google Scholar]
- Lund KE, Lund M. Røyking og sosial ulikhet. Journal of the Norwegian Medical Association. 2005;125:560–563. [PubMed] [Google Scholar]
- Lund KE, Lund M, Bryhni A. Tobacco consumption among men and women 1927–2007. Journal of the Norwegian Medical Association. 2009;129:1871–1874. doi: 10.4045/tidsskr.08.0248. doi:10.4045/tidsskr.08.0248. [DOI] [PubMed] [Google Scholar]
- Lund M, Lindbak R. Norwegian tobacco statistics 1973–2006. Oslo, Norway: Norwegian Institute for Alcohol and Drug Research, SIRUS; 2007. SIRUS skrifter. Retrieved from http://www.sirus.no/filestore/Import_vedlegg/sirusskrifter3.07.pdf. [Google Scholar]
- Lund M, Lund KE. Sosiale ulikheter og røykeslutt blant voksne. Journal of the Norwegian Medical Association. 2005;125:564–568. [PubMed] [Google Scholar]
- MacIntosh H, Coleman T. Characteristics and prevalence of hardcore smokers attending UK general practitioners. BMC Family Practice. 2006;7:24. doi: 10.1186/1471-2296-7-24. doi:10.1186/1471-2296-7-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathews R, Hall WD, Gartner CE. Is there evidence of “hardening” among Australian smokers between 1997 and 2007? Analyses of the Australian National Surveys of Mental Health and Well-Being. Australian and New Zealand Journal of Psychiatry. 2010;44:1132–1136. doi: 10.3109/00048674.2010.520116. doi:10.3109/00048674.2010.520116. [DOI] [PubMed] [Google Scholar]
- Meyer C, Rumpf HJ, Schumann A, Hapke U, John U. Subtyping general population smokers not intending to quit by stages to reduce smoking. Nicotine & Tobacco Research. 2004;6:1043–1050. doi: 10.1080/14622200412331324866. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute. Those who continue to smoke. Is achieving abstinence harder and do we need to change our interventions? Bethesda, MD: US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Cancer Institute; 2003. [Google Scholar]
- Norwegian Directorate of Health. Tal om tobakk 1973–2009 [Tobacco statistics 1973–2009] 2010. Retrieved from http://www.helsedirektoratet.no/vp/multimedia/archive/00318/Tal_om_tobakk_1973__318239a.pdf. [Google Scholar]
- Norwegian Institute for Alcohol and Drug Research. Alcohol and drugs in Norway. 2010. Retrieved from Oslo.http://www.sirus.no/filestore/Automatisk_opprettede_filer/Rusmidler_i_Norge_2010_NO.pdf. [Google Scholar]
- Reid JM, Hammond DP, Driezen PM. Socio-economic status and smoking in Canada, 1999–2006: Has there been any progress on disparities in tobacco use ? Canadian Journal of Public Health. 2010;101:73. doi: 10.1007/BF03405567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose G. Sick individuals and sick populations. International Journal of Epidemiology. 2001;30:427–432. doi: 10.1093/ije/30.3.427. [DOI] [PubMed] [Google Scholar]
- Schaap MM, van Agt HM, Kunst AE. Identification of socioeconomic groups at increased risk for smoking in European countries: Looking beyond educational level. Nicotine & Tobacco Research. 2008;10:359–369. doi: 10.1080/14622200701825098. doi:10.1080/14622200701825098. [DOI] [PubMed] [Google Scholar]
- Statistics Norway. Reise- og ferievaneundersøkelsen 2006. Dokumentasjonsrapport [Documentation report] Notat. Oslo, Norway: Author; 2007. [Google Scholar]
- Stuber J, Galea S, Link BG. Smoking and the emergence of a stigmatized social status. Social Science & Medicine. 2008;67:420–430. doi: 10.1016/j.socscimed.2008.03.010. doi:10.1016/j.socscimed.2008.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velicer WF, Rossi JS, Prochaska JO, DiClemente CC. A criterion measurement model for health behavior change. Addictive Behaviors. 1996;21:555–584. doi: 10.1016/0306-4603(95)00083-6. doi:10.1016/0306-4603(95)00083-6. [DOI] [PubMed] [Google Scholar]
- Wakefield MA, Loken B, Hornik RC. Use of mass media campaigns to change health behaviour. The Lancet. 2010;376:1261–1271. doi: 10.1016/S0140-6736(10)60809-4. doi:10.1016/s0140-6736(10)60809-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner KE, Burns DM. Hardening and the hard-core smoker: Concepts, evidence, and implications. Nicotine & Tobacco Research. 2003;5:37–48. doi: 10.1080/1462220021000060428. doi:10.1080/14622220021000060428. [DOI] [PubMed] [Google Scholar]