Abstract
BACKGROUND:
Pruritus is one of the commonest problems in patients with end-stage renal failure undergoing hemodialysis. Pruritus is an irritating symptom which can directly affect the life quality of patients with chronic renal failure. However, available treatments have failed to relieve the symptom and kidney transplant remains the definite treatment of the problem. A recently proposed treatment for pruritus is the use of complementary medicine. Thus, the aim of this research is to study the effect of aromatherapy on pruritus relief in hemodialysis patients.
METHODS:
The study is a pre- and post-clinical trial, carried out in dialysis centers of Isfahan University of Medical Sciences in 2009. Sample was performed using convenient sampling method and the participants were selected from among the patient who received hemodialysis three times a week for 3-5 hours and had pruritus scores above 3. All the participants received seven minutes of hand massage in the non-fistulated hand with 3-5 ml of lavender, mint, and tea tree oils at 5% concentration for six sessions (two weeks). The data of the study were analyzed using descriptive and inferential statistics by SPSS software, version 16.
RESULTS:
Twenty patients with end-stage renal failure who had pruritus fulfilled the course of the study. Data analysis indicated that aromatherapy significantly relieved pruritus (p < 0.05).
CONCLUSIONS:
Aromatherapy can significantly relieve pruritus in hemodialysis patients.
KEY WORDS: Aromatherapy, pruritus, hemodialysis
Pruritus and skin dryness are currently the main cutaneous presentations of kidney disease patients undergoing hemodialysis.1 According to various studies, severe and obvious pruritus affects 15-49% of patients with chronic renal failure and 50-90% of patients under hemodialysis. The symptoms are more frequent in patients under hemodialysis than in those under peritoneal dialysis (42% vs. 32%).2 In Iran, a study has reported the prevalence of pruritus in 167 hemodialysis patients to be 41.9%, in which 37.1%, 11.4%, and 51.4% reported severe, moderate, and mild pruritus, respectively.3 In such patients, physical and mental ability as well as sleep quality are impaired by pruritus, hence the interference in life quality of the patient. Furthermore, an increase in mortality in patients with pruritus has been reported in some studies.4
Since the physiopathology of pruritus in chronic renal failure patients is unknown and different hypotheses have been proposed in this respect,5 several treatments have been employed for pruritus relief, including intravenous lidocaine or heparin injection, oral administration of cholestyramine, active charcoal, low-protein diet, magnesium-free dialysis, electrical needle stimulation, parathyroidectomy, and UV treatment.6 Moreover, dialysis has slight effect on pruritus of such patients3 and kidney transplant is considered the definite treatment.6
One of the treatments of the problem is complementary medicine. Such treatments have currently attracted great attention7 and many of them are used for patients with kidney diseases. Among these treatments, one can mention touch-therapy, consultation strategies, massage therapy, game therapy, and music therapy.8 Aromatherapy is also one of these complementary medicine methods increasingly used in the 21st century.9 Many of the effects of essential oils used in aromatherapy have been reported in animal experiments, including relaxation, anti-inflammation, analgesia, disinfection, anti-oxidation, and decreasing the blood urea level. Although there is an increasing inclination toward employing aromatherapy, the real effect of aromatherapy on uremic pruritus in patients with chronic kidney failure is not well established.6
Moreover, the studies performed in other fields have reported controversial findings. For instance, in a study by Atashzadeh et al, the effect of perfume therapy and massage on pain intensity in multiple sclerosis patients in Tehran was investigated. It was demonstrated that both perfume therapy and massage had considerable effect on pain intensity and the effect of massaging with menthol (containing peppermint essence) was greater than that with sweet almond oil.10 On the other hand, a study by Pazandeh et al, on the effect of aromatherapy with chamomile on the pain of episiotomy showed that chamomile essence has no effect in reducing the episiotomy pain.11 Thus, the researcher performed this study to evaluate the effect of aromatherapy in relieving pruritus in patients undergoing hemodialysis in hospitals affiliated with Isfahan University of Medical Sciences in 2009. The objective of the study was to determine and compare pruritus scores before and after aromatherapy in the patients.
Methods
This study is a pre- and post- quasi-experimental clinical trial carried out in 2009 in dialysis centers affiliated with Isfahan University of Medical Sciences. All patients with pruritus who underwent hemodialysis three times a week for 3-5 hours in each session participated in this study. We used convenient sampling method. The following inclusion criteria were considered. All patients above 18 years old who had undergone hemodialysis for more than three months with bicarbonate solution using polysulfane filters, had pruritus during the past two weeks before sampling, had not used any pruritus relieving medication before and during sampling, had no dermatological problem other than uremic pruritus, and had phosphate serum levels less than 6 mg/dl, and parathormone serum levels less than 600 pg/ml entered the study. If a patient underwent kidney transplant, exhibited allergic reaction to the aromatic oil, or was prescribed to undergo fistulation, he/she would be excluded from the study.
After receiving informed consent in the midweek hemodialysis session, a 5 ml sample was taken from each patient's fistula to control physiological parameters (phosphorus, parathormone, calcium, blood urea nitrogen, creatinine, alkaline phosphatase, hemoglobin, and hematocrit). Then, skin dryness was recorded according to the scale in which 0 indicated lack of dryness and 3 indicated severe dryness of the skin.3 Moreover, the pruritus was scored according to the severity, site, and frequency of itching. Pruritus severity scores ranged from 0 to 4, site scores were 1 and 2, and pruritus frequency scores ranged from 0 to 3. The range of overall scores was 0-9, in which 9 indicated the most severe case.7 In this study, we defined pruritus as having a score of three and above in the scale mentioned above. The validity of the pruritus scale has been established by Bujaro et al,6 and the validity of skin dryness scale in Akhiani et al.3
All the participants had a skin test before undergoing massage with the oil to make sure they were not allergic to the oil. Non-allergic participants received seven minutes of massage in 12 steps in all hemodialysis sessions for two weeks, using mint, lavender, and tea tree oils diluted to 5% in sweet almond oil.7 The pruritus scores were evaluated at the end of the treatment.
We analyzed the data using descriptive statistics (mean, standard deviation, frequency, and percentage) and inferential statistics (paired t-test) by SPSS software, version 16.
Results
Out of the 24 participants, four left the study; two because of complaint about the oil odor, one because of having incontinence with the greasy sensation, and one because of not following up with the dialysis. The mean age of the participants was 50.75 ± 18.02, and 60% of the participants were male. The most common underlying diseases were diabetes (40%), hypertension (20%), and glomerulonephritis (5%). As regards skin dryness, 65% had mild dryness, 5% had moderate dryness, and none exhibited severe dryness. The mean duration of treatment with dialysis in the participants was 47.15 ± 43.48 months. The mean values for the physiological parameters were as follows: calcium 8.37 ± 1.06 mg/dl, alkaline phosphatase 455.30 ± 380.63 mg/dl, blood urea nitrogen 60.80 ± 22.28, creatinine 7.83 ± 3.20 mg/dl, Hb 10.2 ± 1.9 mg/dl, and hematocrit 31.9 ± 5.6%.
The average of pruritus score before the intervention was 7.40 (1.18) which after intervention received 5.85 (1.69) and paired t-test showed that there was a significant difference between average of pruritus scores before and after the study (t = 5.43, p < 0.001) (Diagram 1).
Diagram 1.
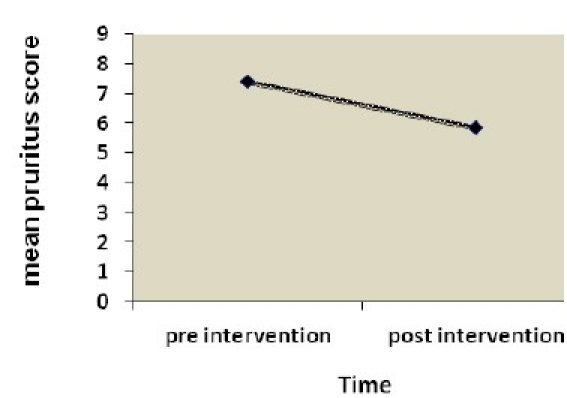
comparison of mean pruritus score before and after the intervention
Discussion
The findings of the present study showed that pruritus score had been decreased after the aromatherapy in subjects under study in comparison with their past and in a study by Ujaro et al, the average pruritus scores were 5.69 (1.25) and 2.69 (1.03) before and after the aromatherapy respectively and there was a significant difference before and after the study (p = 0.01).7 In a study by Khalili.et.al, the application of some antihistamine medicines have been effective to control uremic pruritus such as hydroxyzine and chlorpheniramine so that average pruritus score was 25 before the beginning of hydroxyzine medicine and two weeks later, after the treatment declined to 17 and the difference of average pruritus score has been significant before and after taking medicine (p < 0.001). Average pruritus score was 20 before the beginning of chlorpheniramine and it declined to 15, two weeks after the treatment and reduction of itchy intensity was significant after taking this medicine (p < 0.001).5
Makhlough.et.al, showed that taking capsaicin was effective in itchy relief so that pruritus score was 10.9 (6.3) before taking the medicine and in successive weeks it was 6.4 (3.9) at the first week, 4.7 (3.1) at the second week, 3.2 (2.9) at the third week and 2.55 (2.5) at the fourth week and there was a significant difference in successive weeks statistically (p = 0.001).12 Since capsaicin stimulated C neural fibers and discharged them from P substance which was a neural bond of pain and pruritus, so it stops pruritus and pain several days after the beginning of the treatment12 and according to the similar effect of massaging in decreasing or controlling the pain and also sedative massaging on neural system7,9 and also the effect of aromatherapy on secretion of neurotransmitters such as encephalin and endorphins13 and influence of linalil acetate in lavender on depression of central neural system, the above mentioned study was used in order to support the present study.7 In his study, Imura.et.al found that massaging with aromatic oil decreased the anxiety, depression, fatigue and confusion in mothers under study.14 Wilkinson et al, showed in their research that massaging with aromatic oils, as compared to conventional care leads to a significant decrease in anxiety and depression of patients only for two weeks after the end of the intervention, and there was no significant difference in anxiety and depression in the follow-up up to ten weeks after the end of the intervention.15 Halm showed in his systematic study that anxiety and depression had decreased in three out of five papers and pain in one out of five papers.16 Moreover, Wilcock et al, evaluated the effect of massage with aromatic oil in cancer patients and found that no significant difference existed between the experiment and control groups in terms of affect, life quality, and physical symptoms.17 Therefore, since psychological factors can affect the perception of pruritus18,19 and considering the similar pattern of neuronal sensitization in pruritus and chronic pain,20 we used the studies on chronic pain to support or reject the results of the study. Several studies support the effectiveness of aromatherapy in contrast to a limited number rejecting it. Thus, it can be concluded that aromatherapy can, directly or indirectly, relieve pruritus. Also, regarding the findings of the present study, one can conclude that aromatherapy can significantly reduce pruritus in patients undergoing hemodialysis. However, generalization and application of this method still lies dependent upon more accurate and more comprehensive studies in the field. Further studies with larger sample sizes and longer follow-up periods (at least four weeks) are required to make the findings generalizable to the population.
The authors declare no conflict of interest in this study.
Acknowledgments
We would like to express our gratitude to all the patients participating in this study and all the personnel in the dialysis centers affiliated with Isfahan University of Medical Sciences, who cooperated with us in carrying out this research.
References
- 1.Andersson RG, Quirk C, Sullivan J, Anderson CD. Cutaneous manifestations of internal disease. Drug Discovery Today: Disease Mechanisms. 2008;5(1):e113–e123. [Google Scholar]
- 2.Kurban MS, Boueiz A, Kibbi AG. Cutaneous manifestations of chronic kidney disease. Clin Dermatol. 2008;26(3):255–64. doi: 10.1016/j.clindermatol.2007.10.017. [DOI] [PubMed] [Google Scholar]
- 3.Akhyani M, Ganji MR, Samadi N, Khamesan B, Daneshpazhooh M. Pruritus in hemodialysis patients. BMC Dermatol. 2005;5:7. doi: 10.1186/1471-5945-5-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Melo NC, Elias RM, Castro MC, Romao JE, Abensur H. Pruritus in hemodialysis patients: the problem remains. Hemodial Int. 2009;13(1):38–42. doi: 10.1111/j.1542-4758.2009.00346.x. [DOI] [PubMed] [Google Scholar]
- 5.Khalili H, Dashti S, Ahmed Pur P, Haji Babaei M, Abdollahi F. Comparison of the efficacy of drugs in patients with chronic renal failure itching. Tehran University of Medical Sciences Journal. 2006;64(4):36–42. [Google Scholar]
- 6.Ro YJ, Ha HC, Kim CG, Yeom HA. The effects of aromatherapy on pruritus in patients undergoing hemodialysis. (256).Dermatol Nurs. 2002;14(4):231–8. [PubMed] [Google Scholar]
- 7.Nurse's handbook of alternative and complementary therapies. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 2003. Lippincott Williams & Wilkins. [Google Scholar]
- 8.Terrill B. Melbourne: Ausmed Publications; 2002. Renal Nursing: A Practical Approach. [Google Scholar]
- 9.Shutes J, Weaver C. 1st ed. New Jersey: Pearson; 2007. Aromatherapy for Bodyworkers. [Google Scholar]
- 10.Atash Zedeh Shourideh F, Mohammadei SH, Abed Saeedi ZH, Alavi Majd H, Salehi Sormaghie MH. Compared the effect of aroma therapy and massage on pain in patients with multiple sclerosis. Journal of Nursing and Midwifery, Shahid Beheshti. 2007;17(58):28–32. [Google Scholar]
- 11.Pazndeh F, Savadzadeh S, Mojab F, Alavi Majd H. Effect of chamomile essential oil aromatherapy with episiotomy pain”. Journal of School Shahid Beheshti Nursing and Midwifery. 2008;18(62):5–12. [Google Scholar]
- 12.Makhlough A, Ala SH, Haj Heydari Z, Kashi Z, Barry AR, Barry Z. Effect of ointment Kapsaysyn Kapsyan {0.03} percent in treatment of pruritus in hemodialysis patients. Journal of Mazandaran Medical Science. 2009;19(69):7–13. [Google Scholar]
- 13.Potts J. Aromatherapy in nursing practice. Aust Nurs J. 2009;16(11):55. [PubMed] [Google Scholar]
- 14.Imura M, Misao H, Ushijima H. The psychological effects of aromatherapy-massage in healthy postpartum mothers. J Midwifery Womens Health. 2006;51(2):e21–e27. doi: 10.1016/j.jmwh.2005.08.009. [DOI] [PubMed] [Google Scholar]
- 15.Wilkinson SM, Love SB, Westcombe AM, Gambles MA, Burgess CC, Cargill A, et al. Effectiveness of aromatherapy massage in the management of anxiety and depression in patients with cancer: a multicenter randomized controlled trial. J Clin Oncol. 2007;25(5):532–9. doi: 10.1200/JCO.2006.08.9987. [DOI] [PubMed] [Google Scholar]
- 16.Halm MA. Essential oils for management of symptoms in critically ill patients. Am J Crit Care. 2008;17(2):160–3. [PubMed] [Google Scholar]
- 17.Wilcock A, Manderson C, Weller R, Walker G, Carr D, Carey AM, et al. Does aromatherapy massage benefit patients with cancer attending a specialist palliative care day centre? Palliat Med. 2004;18(4):287–90. doi: 10.1191/0269216304pm895oa. [DOI] [PubMed] [Google Scholar]
- 18.Yosipovitch G. 1st ed. New York: CRC Press; 2004. Itch: basic mechanisms and therapy. [Google Scholar]
- 19.Lugton J, McIntyre R. 1st ed. New York: Elsevier Health Sciences; 2005. Palliative care: the nursing role. [Google Scholar]
- 20.Schmelz M. Itch and pain. Neuroscience & Biobehavioral Reviews. 2010;34(2):171–6. doi: 10.1016/j.neubiorev.2008.12.004. [DOI] [PubMed] [Google Scholar]


