Abstract
BACKGROUND:
One of the biggest problem today that most developing countries are faced with is the uncontrolled population growth; a serious threat to the international community. One of the most accessible contraceptive methods is the hormonal methods in which low-dose estrogen (LD) combined pills are considered as the most common among them. The most important reason for discontinuation of the combination pills is the side effects and following the discontinuation, it can lead to unwanted pregnancy. Promotion of more new methods and providing better methods with lesser side effects can be an important step towards solving some of the problems and increasing the usage percentages of contraceptive methods. This study therefore aimed to compare the effects of Yasmin and LD on menstrual cycle changes.
METHODS:
In this clinical trial study, 60 women referred to the Family Planning Health Center of Isfahan in 2008 were studied that finally after the sample loss, 27 and 24 samples were placed in Yasmin and LD groups, respectively. A questionnaire was used in order to collect the data. Content validity test and re-test also were used to confirm the validity and reliability of the questionnaire. To analyze the data, SPSS software and descriptive and inferential statistical methods were used.
RESULTS:
The results of this study indicated that the bleeding rate in the Yasmin group within the next six month compared to taking them before was significantly lower than that in LD group (p = 0.02); but there was no significant difference in terms of menstrual bleeding duration and the two menstruation interval between the two groups (p = 0.2). There was no significant difference between the Yasmin and LD groups in terms of delay in menstruation and dysmenorrheal. Spotting rate significantly was higher in Yasmin group than that in LD group (p = 0.02). There was a significant reduction in terms of bleeding rate changes and menstrual bleeding duration in both Yasmin and LD group at the following next six months in comparison with before the consumption (p < 0.05).
CONCLUSIONS:
According to the results obtained, the oral combination of Yasmin pills has fewer side effects than LD pills. Therefore, it is recommended to start using Yasmin pill in the family planning units in Iran.
KEY WORDS: LD, side effects, contraceptive pill, Yasmin
Family planning together with intervention in women reproductive cycle would help them to control the number and the gap between pregnancies and the population growth. This plan was seriously followed in Iran since 1989 and as a result, according to the statistics of the National Investigation (Population and health characteristics) the 2.3% population growth rate in 1986 was reduced to 1.58% in 2000; and according to the reported statistics by the National Research (New Monitoring and Assessment System, 2005) it encouraged 78.9% of people to use contraception methods in 2005 Up to 2001, the average use of these methods was 60% worldwide while it was 73% in Iran.1
According to the statistics, the rate of unwanted pregnancies in Iran reached 31.1% in 2000 which differed in various areas of Iran. Studies showed it occurred in 38and 35% of pregnancies in Tehran and Isfahan, respectively2 which was caused by failing to use contraception methods as an important reason and then not using the effective contraceptives.3
One of the family planning activities in Iran is extensive and varied work to prepare and provide the contraceptive tools. It could be expressed that 93 million women around the world are using oral combination pills as contraceptives.4 Despite its low failure rate and considerable benefits, many women experience its short and long term outcomes and side effects. The side effects of combined pills include spotting, menstrual irregularities, nausea, headaches, painful breasts and weight loss and gain. The majority of the contraceptive pills contain estrogen and progesterone that is the reason they are called combination pills. One of the oral combined contraceptives is LD which contains 30 mcg ethinyl estradiol and 150 mcg levonorgestrel. New hormonal oral contraceptives are Yasmin medication which contains 30 mcg ethinyl estradiol and 3 mg drospirenone (spironolactone analogue and anti-androgen and anti-mineralocorticosteroids).5
One of the side effects of combined oral contraceptives is sudden and unexpected bleeding which can be due to forgetting to consume the contraceptives. The amount of bleeding varies from 10-30% at the first few months to 10% at the third month. Spotting between menstruations reduces after the first 2-3 months. Irregular consumption of the pills and taking anti-rifampin and anti-epilepsy drugs, forgetting, pregnancy, poor oral absorption due to drug interactions, vomiting 2 hours after taking the pill or severe diarrhea could be reasons of the sudden bleeding.6–9 There is no evidence proving that sudden and unexpected bleeding is due to reduction of the pills efficacy. The other side effect associated with taking combined pills is amenorrhea after taking the pill with the rate of 7-8% which increase by duration of consumption and probably would be decreased to 5% after many years of consumption. One of the beneficial effects of oral contraceptives is dysmenorrhea reduction, menorrhagia and PMS (premenstrual syndrome) reduction and the bleeding control. The positive note in taking the combination pills is that 90% of the consumers have normal bleeding pattern.6–10 The study of Suthipongse also indicated that amount of blood loss during menstruation in the group containing 30 mcg ethinyl estradiol, and 150 mcg levonorgestrel was more than that in the group containing 30 mcg ethinyl estradiol and 3 mg drospirenone. While, in terms of menstrual bleeding duration, despite both groups causing reduction of menstrual period but no significant difference was observed between the two groups.11 The study of Sulak also showed that the combination containing drospirenone was more beneficial in reducing menstrual symptoms than the second and third generations of progestins (such as desogestrel or levonorgestrel).10 This study aimed to evaluate the effects of Yasmin and LD as contraceptives on the menstrual cycle changes.
Methods
This was a clinical trial study. Women aged between 18 to 35 years old who referred to family planning health care centers in Isfahan participated in this study. The study started at 2009.7.25 to 2010.3.6 so that the samples took Yasmin or LD for six months. The inclusion criteria included women aged between 18 to 35 years old, with regular menstrual cycle, having no menstrual disorders such as menorrhagia and spotting before taking the pills, having not used norplant in at least 6 cycles prior to the study and injectable hormones in at least 3 cycles prior to the study, no contraindications from the use of combination pills and no endocrine disorders, passing at least 3 regular cycles from their labor or abortion and not breastfeeding. The exclusion criteria also included taking medications which affect the pill's metabolism, incidence of a disease during the study so that the study subject was contraindicated to take hormonal medications and or the study subjects’ dissatisfaction to continue the method and tending to withdrawal from the study.
The health care centers were chosen on a random cluster selection from the 1st and the 2nd Isfahan health care centre networks and the samples were selected by simple random sampling. Thereafter, each of the samples randomly and based on random numbers table were placed in the two Yasmin and LD groups. According to consultation and conscious selection of the methods by the subject, some predetermined packs containing the type of the pills (Yasmin or LD) they had to take, were given to the study samples. Provided that one of the samples refused to take the medicine which was assigned for her, she would have excluded from the study. The data collection tool included a questionnaire and it was performed through interview at three phases, before start taking the pills, in 3 and 6 months during the pills consumption. In order to determine the reliability, the mentioned questionnaire was given to 10 subjects who had just completed the menstrual cycle (who were excluded from the study after sampling). Again within two weeks, the questionnaire was completed by the same subjects. Then, coefficient correlation was calculated through a re-test which obtained the result of 80%. Validity of the two parts questionnaire was confirmed by several Faculty members of School of Nursing and Midwifery, Gynecologists and Isfahan Health Center Authorities. The first part included questions about demographic information, fertility and the second part was about the side effect of using pills such as menstrual cycle changes (bleeding volume, menstrual duration, the gap between the two menstrual cycles, spotting and unexpected bleeding and delay in menstruation and dysmenorrhea). The criteria to measure volume of the menstrual bleeding was according to the stained pads by the menstrual blood which was considered as follows: low bleeding, i.e., 1.4 of the pad stained with blood equal to 6.2 cc, moderate bleeding, i.e., 2.4 of the pad stained with blood equal to 12.5 cc, severe bleeding, i.e., 4.4 of the pad stained with blood equal to 25 cc. Considering that 1 pad can approximately keeps 25 ml of the menstrual blood, the amount of blood lost was calculated. The pills should have been taken from the first day to the fifth day of menstrual; preferably started at the first day for 21 days and again after seven days of taking the last pills the next pack should have been started and this process was continued for six months. The information about the pills’ side effects was collected through questionnaire and interview. The sample size was contained of 25 subjects in each group by confidence coefficient of 95% which due to a probable loss, 5 other subjects were added to each group and finally the samples reached to 60 subjects; 30 in the Yasmin consumers and 30 in the LD consumers. At the end of the study, the following subjects left the study: in Yasmin group, 1 subject due to frequent spotting, 1 subject due to severe nausea, headaches and dizziness, 1 subject due to severe bleeding and prescriptions of the physician; in LD group, 1 subject due to pregnancy, 2 subjects due to severe headache and 2 subjects due to nausea and vomiting and 1 subjects due to dissatisfaction of her husband discontinued the method. At the end, 27 and 24 subjects were studied in the Yasmin and LD groups, respectively. The data were analyzed using SPSS software, version 10, descriptive statistics (mean, standard deviation, minimum, maximum) and analysis (chi-square, independent t-test, ANOVA with repeated observations).
Results
The mean age of the women in Yasmin and LD group was 29.07 and 29.2 years, respectively. In terms of education, the highest frequency (54.2%) in the LD group was related to under the high school graduates and in Yasmin group, the highest frequency (40.7) was related to the academic educational level. It should be noted that among these subjects, those who had academic education, after providing consultant and advice, they tended more to use the new methods, whereas the subjects with lower educational level refused to accept the new methods.
Independent t-test, in terms of the mean menstrual bleeding at three times, showed that the mean menstrual bleeding in 3 and 6 months after the intervention in Yasmin group significantly was lower than that in the LD group (p < 0.05); ANOVA with repeated observations also showed that the mean menstrual bleeding was significantly reduced in the Yasmin group in 3 and 6 months after taking the pills (p < 0.001) and in the LD group in 6 months after taking the pills compared to the previous consumption of the same pills (p < 0.003).
The finding of Table 1 shows that the mean menstrual bleeding was reduced in 3 and 6 months after the intervention in both groups and this reduction was greater in Yasmin group, but there was no significant difference (p > 0.05). ANOVA with repeated observations in each group showed that the mean menstrual bleeding in Yasmin group with (p = 0.011) and LD group with (p = 0.02) indicated a significant difference during 3 and 6 months after the intervention compared to that before. Independent t-test showed that there was no significant difference between the interval times of menstruation in three cycles in two Yasmin and LD groups (p > 0.05).
Table 1.
Comparison of the mean duration of menstrual bleeding in three different times in Yasmin and LD groups
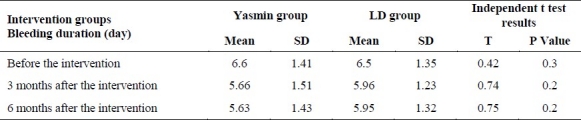
Table 2 indicates that the most frequency of spotting was in Yasmin group (29.6%) and the lowest frequency was related to the LD consumers (8.3%). The present study showed that spotting rate in the first 3-months in both groups was higher than that of the second 3-months. Fisher's exact test showed that spotting and inter-cycle bleeding significantly was higher in Yasmin group than that in LD group (p = 0.02). In this study, 8 out of 27 subjects in Yasmin group and 2 out of 24 subjects in LD group experienced spotting and inter-cycle bleeding.
Table 2.
Comparison the frequency distribution of spotting and Inter-cycle bleeding (inter-menstrual) in Yasmin and LD groups
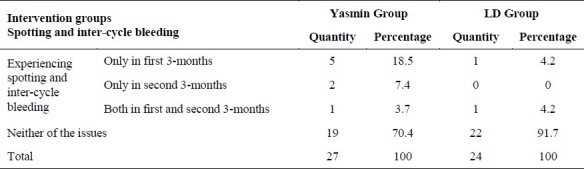
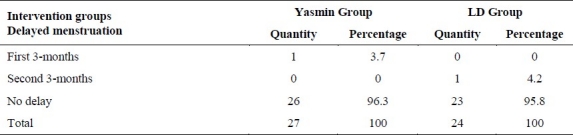
Table 3 shows that frequency of delay in the menstruation in Yasmin group and LD group was 3.7% and 4.2%, respectively. Fisher's exact test showed that delay in the menstruation in both groups had no significant difference (p = 0.3).
Table 3.
Comparison the frequency distribution of delayed menstruation (amenorrhea) in Yasmin and LD groups
Chi-square test showed that the distribution of dysmenorrhea had no significant difference in Yasmin and LD groups (p = 0.19). The most dysmenorrhea improvement was related to Yasmin group at 51.9%; so that 14 out of 27 subjects mentioned dysmenorrhea improvement in Yasmin group, whereas this amount was reported as 8 out of 24 subjects in LD group.
Discussion
According to the results of the present study, reduction of the hemorrhage rate was occurred in the two groups which was significantly higher in Yasmin group than that in LD group. Study findings of Suthipongse indicated that blood loss in the group containing levonorgestrel was higher than that in the group containing drospirenone.11 Diana Mansour also in her study found that oral contraceptives could reduce the bleeding during the menstrual cycle by 43%.12 Time intervals between the menstrual bleeding can be easily identified, but measuring the rate of the menstrual blood loss is more difficult. The association between the actual and subjective rate of bleeding is relatively weak. Furthermore, women's complaints about severe menstrual bleeding are more associated with the bleeding interaction in their daily performances than the actual bleeding rate.6 Only 80-90 percent of women have normal bleeding, i.e., > 80 ml.7 Janatannavak also stated that half of the women, who have thought they had heavy bleeding, in fact had bleeding less than 80 ml.8 According to the results of the recent study and other studies, the new third-generation combination pills especially those with anti-androgen properties such as Yasmin and dienogest are more effective in reducing the bleeding severity.
Results of the present study showed that the mean duration of menstrual bleeding reduction was higher in Yasmin group but no significant difference was observed between the two groups. Suthipongse's study regarding this showed that reduction in the mean menstrual duration was higher in the group containing drospirenone and it was indicated that there was no significant difference in the mean duration of the cycle in both groups.11
Suthipongse study results about interval between menstruation indicated that the majority of the subjects in both groups containing levonorgestrel and drospirenone had a menstrual cycle length between 26 to 29 days.11 In the present study, although the group containing drospirenone showed longer interval between the two menstruations than that in the group containing levonorgestrel, the difference between the two groups statistically was not significant (p > 0.05).
The results of the present study showed that the mean changes in the bleeding rate in Yasmin group in 3 and 6 months after the intervention (p < 0.001) and in LD group in 6 months after the intervention was significantly lower in comparison with before the intervention (p < 0.003). Study of Endrikat showed that by taking Yasmin, the percentage of women who had mild bleeding during the menstruation increased from 8.1% at the beginning of consumption to 34.9% after the sixth cycle of consumption. While, the percentage of women who had severe bleeding during the menstruation, significantly decreased from 22.7% to 0.9%.13 This study indicated that taking Yasmin decreased the percentage of women with severe menstrual bleeding and the blood loss rate had a significant reduction from the beginning of consumption compared to the sixth cycle. Bachmann also indicated that by taking low-dose combined oral contraceptives, the severity of menstrual bleeding was seen from spotting range to normal bleeding in more than 88% of the subjects.14
Recent studies have shown that the mean changes in duration of menstrual bleeding in Yasmin and LD group in 3 and 6 months after the intervention had a significant reduction in comparison with before the intervention. Sanders showed that before taking Ortho-cyclen and Tri-cyclen, 1% of women reported light bleeding, 55% moderate bleeding and 40% very heavy bleeding. When the subjects were asked about the effect of pills on bleeding rate, most of them reported the bleeding rate had been lighter or shorter.15
The present study showed that spotting and inter-cycle bleeding in Yasmin group significantly was higher than that in LD group (p = 0.02). According to Suthipongse's study, spotting and unexpected bleeding rate in the group containing drospirenone reported as 30.7%. The high rate of spotting and bleeding perhaps was caused because for most women, it was their first time to take the pill.11 Parsey in his study stated that at least 30% of women had intercycle bleeding during the first and second cycles of taking Yasmin. The most spotting rate happens at the beginning of taking pills and during the first 3-month particularly at the first month of taking combined contraceptives especially before the body adjust itself to the pills.16 Moreover, Berenson believed inter-cycle bleeding would happen if they forget to take a pill or take them later than the required time.11
The present study indicated that the frequency of delay in menstruation in Yasmin group (3.7%) and LD group (4.2) was similar; therefore, delay in menstruation in both groups showed no significant difference (p = 0.3). The study of Parsey also showed that during 13 cycles of taking Yasmin, amenorrhea averagely was occurred in 3.2% of women. This rate was reported 3.6% until the sixth cycle of consumption.16 Suthipongse in his study observed no cases of amenorrhea in the groups containing levonorgestrel and drospirenone.11
The authors declare no conflict of interest in this study.
References
- 1.Mehdi Zadeh Z. Isfahan: School of Nursing Midwifery, Isfahan University; 2009. Relationship between sexual function with common contraceptive methods in couples referred to the Isfahan Health Mrakzbhdashty year 2008, [MSc Thesis] [Google Scholar]
- 2.Saghafi Z. Isfahan: School of Nursing Midwifery, Isfahan University; 2004. Unwanted pregnancy, [MSc Thesis] [Google Scholar]
- 3.Kasmaei P, Atr Kareroshan Z. Prevalence and factors correlated with unwanted pregnancies. Guilan University of Medical Sciences. 2003;12(48):61–6. [Google Scholar]
- 4.Crosignani PG, Nappi C, Ronsini S, Bruni V, Marelli S, Sonnino D. Satisfaction and compliance in hormonal contraception: the result of a multicentre clinical study on women's experience with the ethinylestradiol/norelgestromin contraceptive patch in Italy. BMC Womens Health. 2009;9:18. doi: 10.1186/1472-6874-9-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reza Soltanei P, Parsaei S. Tehran: Sanjesh Publication; 2008. Motherhood and childhood health. [Google Scholar]
- 6.Aspirof LA, Feritiz M. Clinical Endocrinology and infertility in women Aspirof. In: Ghazi Jahanei B, Mohajerani S, translators. Tehran: Sanjesh Publication; 2005. [Google Scholar]
- 7.Campbell S, Monga A. London: Arnold; 2000. Gynaecology by Ten Teachers; p. 50. [Google Scholar]
- 8.Janatannavak BE. Novak Gynecology. In: Farhang Beygvand SH, Faridian D, Alaei M, translators. Tehran: Golban Publication; 2002. p. 178. [Google Scholar]
- 9.Biswasa J, Manna M, Webberle H. Oral contraception. Obstetrics, Gynaecology & Reproductive Medicine. 2008;18(2):317–23. [Google Scholar]
- 10.Sulak PJ, Kuehl TJ, Coffee A, Willis S. Prospective analysis of occurrence and management of breakthrough bleeding during an extended oral contraceptive regimen. Am J Obstet Gynecol. 2006;195(4):935–41. doi: 10.1016/j.ajog.2006.02.048. [DOI] [PubMed] [Google Scholar]
- 11.Suthipongse W, Taneepanichskul S. An open-label randomized comparative study of oral contraceptives between medications containing 3 mg drospirenone/30 microg ethinylestradiol and 150 microg levonogestrel/30 microg ethinylestradiol in Thai women. Contraception. 2004;69(1):23–6. doi: 10.1016/j.contraception.2003.08.014. [DOI] [PubMed] [Google Scholar]
- 12.Mansour D. Experiences with Yasmin: the acceptability of a novel oral contraceptive and its effect on well-being. Eur J Contracept Reprod Health Care. 2002;(Suppl 3):35–41. [PubMed] [Google Scholar]
- 13.Endrikat JS, Milchev NP, Kapamadzija A, Georgievska J, Gerlinger C, Schmidt W, et al. Bleeding pattern, tolerance and patient satisfaction with a drospirenone-containing oral contraceptive evaluated in 3488 women in Europe, the Middle East and Canada. Contraception. 2009;79(6):428–32. doi: 10.1016/j.contraception.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 14.Bachmann G, Sulak PJ, Sampson-Landers C, Benda N, Marr J. Efficacy and safety of a low-dose 24-day combined oral contraceptive containing 20 micrograms ethinylestradiol and 3 mg drospirenone. Contraception. 2004;70(3):191–8. doi: 10.1016/j.contraception.2004.05.013. [DOI] [PubMed] [Google Scholar]
- 15.Sanders SA, Graham CA, Bass JL, Bancroft J. A prospective study of the effects of oral contraceptives on sexuality and well-being and their relationship to discontinuation. Contraception. 2001;64(1):51–8. doi: 10.1016/s0010-7824(01)00218-9. [DOI] [PubMed] [Google Scholar]
- 16.Parsey KS, Pong A. An open-label, multicenter study to evaluate Yasmin, a low-dose combination oral contraceptive containing drospirenone, a new progestogen. Contraception. 2000;61(2):105–11. doi: 10.1016/s0010-7824(00)00083-4. [DOI] [PubMed] [Google Scholar]


