Abstract
BACKGROUND:
Oxytocin is the most consumed medication in modern midwifery. The consumption of oxytocin in inducing and strengthening delivery in delivery wards requires an efficient method for making use of this medication with maximum effect and minimum side effects. In this regard, this study has been conducted aiming at comparing the effect of two methods of prescribing oxytocin in inducing delivery on the duration of stages.
METHODS:
The present study is of a clinical trial kind with three-blinded parties which was conducted in 2010 on 120 research volunteers who had the inclusion criteria. The samples were randomly assigned into two groups of control and experiment. The data collection means consisted of a questionnaire and a checklist. In order to analyze the data, the SPSS software, version 17, Student T-test and Chi-square test were used.
RESULTS:
There was no statistically significant difference between two groups regarding the duration of the first and the first stages and the active phase. The duration of the third stage of delivery was shorter than the group which had stopped using oxytocin at the active phase. There has been no significant difference between the mean of oxytocin dosage from the initiation of the delivery induction till the active phase. The mean of oxytocin dosage has been significantly different between two groups during all stages of delivery so much so that this rate has been lower in the experiment group.
CONCLUSIONS:
The results of the data analysis show that the continuation of oxytocin after the active phase not only does not have any advantage regarding the shortening of duration of stages and its cutting but also it leads to a decrease in the consumption dosage of oxytocin in the active phase and the second stage of delivery and on the other hand leads to a decrease in the side effects of the medication on mother and infant.
KEY WORDS: Oxytocin, delivery induction, delivery stages, intensified contractions
By attending to this point that women's health is one of the important indicators of hygienic cares in the national level and also the number of women at pregnancy age forms a large and effective amount of population in the society,1 the direction of a labor must be towards assuring the maternal and neonatal health, diagnosing abnormal findings, and reducing pain and duration of labor, all of which being at the top priority for an expert or a mid-wife.2 One of the actions that is done for reducing the rate of death among mothers and infants during high risk pregnancies is labor induction. The need for labor induction is made clear for any reason that the continuation of pregnancy jeopardizes the maternal and neonatal health.1
Nowadays, rush had overshadowed every aspect of our daily activities and even doctors and nurses’ clinical decisions are not excluded from this fact, so much so that it has led to an increase in the rate of optional induction and strengthening labor cramps by the using oxytocin. Oxytocin is the mostly consumed medicine in modern midwifery1 to the extent that it has confronted us with a population under induction and we ought to wait for its long-term consequences.3
According to the National Center for Health Statistics, the rate of annual induction and strengthening of labor cramps is growing and it has reached from nearly 20 percent in 1989 to 25 percent in 2002 in the USA. Labor induction can be in form of medicine, surgery, or a mixture of both. The commonest method of induction is the use of oxytocin and the opening of the amnion membrane.4
This medicine recuperates most of the delayed labor effects and the post-labor bleedings. Due to rampant and incautious usage, oxytocin has been considered as a high alert medicine in 2007 and it has been added to the 18 medicines which need special safety measures at the time of prescription.5 However, Vicknord got the Nobel Prize in Chemistry in 1950 for discovering the structure of this medicine and in 2000, the American Women's Midwifery Association announced that 50 percent of Forensics Medicine's meetings has been about the issues and problems regarding pregnancy and labor related to oxytocin or its side effects such as intensified cramps, uterine rupture and uterine inertia after labor.6 This issue has compelled the researchers to adopt policies for assuring the maternal and neonatal safety against this medicine. One of these policies is the reduction of dosage and duration of usage of oxytocin. Lots of studies have been conducted about the dosage and duration of oxytocin infusion. Of course, no special study has been observed inside the country among the present researches in this respect which could be pointed out to. Only, the clinical experiences indicate the rampant usage of this medicine and its harmful effects in the Women, Midwifery and Health System Sector.
Studies have shown that activity of oxytocin receptors which is out of GP (G Protein-coupled receptors) paired protein are under the effect of the time during which oxytocin gets infused. Robinson showed through a study in 2002 that after 4.2 hours that myocytes are placed next to oxytocin, they lose 50 percent of their activity.7 Phaneuf et al also showed that continuing the use of oxytocin negatively stimulates its receptors in laboratory.8
All these studies have led to a higher attention to the duration of oxytocin in labor.
In 2004, Daniel-Spiegel et al9 conducted a research by posing this question: “how long should oxytocin be continued after labor induction”? He showed that if oxytocin is not used after the initiation of the active phase of labor, not only it won’t cause the lengthening of labor stages also it reduces the intensified cramps. These researches have been conducted to address a question that midwifery references have not alluded to and on the other hand, the little number of samples, considering labor induction and strengthening of labor cramps and lack of attention to the number of labors are among the limitations of Spiegel's study and all these factors compelled us to invest on a more precise study aiming at “the identification of two administration methods of oxytocin in labor inducing on labor stages duration”.
Methods
The present study was a triple blind clinical trial, conducted after getting a license from the Ethics Committee of Isfahan University of Medical Sciences from 17.4.2009 till 19.9.2009 on 120 individuals who had inclusion criteria in labor departments of Dr. Beheshti and Dr. Shariati hospitals. The sampling was random for which the Table of random numbers and closed envelopes were used. 120 proper envelopes were provided and were divided into 2 groups of 60. Each envelop was selected randomly for administering induction in each sample and it was left closed on the file till the initiation of intervention.
Number of samples according to the following formula was 60:
N = [Z1-a/2 + Z1-β]2 [δ2 + δ2] / d2 = [1.96+ 1.28]2 [1+1] / (0.75)2 = 60
By considering the maximum amount for the proportion of subcategories in the population with a 0.05 error and confidence of 95 percent, 120 individuals were attained. The duration of the first stage of delivery was the variable on the basis of which the number of samples has been defined.
The inclusion criteria included completed consent form, gestational age over full 36 weeks, written prescription of induction from the physician, age over 18 or under 35 years old, correct heart beat pattern, single-fetus pregnancy by vertex presentation and anterior oxiput, bishop score of the uterine entrance above 5, not using any medicine but routine medications (painkillers and antibiotics), not using prostaglandins and other induction methods, absence of placenta abruption, and body mass index less than 26 prior to pregnancy. In case of having any hypertonic contraction before the initiation of intervention or during administering the induction (by intensified contraction we mean 5 times or more incidence of contraction within 10 minutes), fetal distress before the initiation of intervention, allergy to medicine, and in case that after the active phase, the contraction weakened and the progression rate of dilation was less than 0.5 centimeters in an hour, the participating individual was excluded from the study.
The participants in this study received induced labor in the same way as it was described above after initial evaluations; so that 5 units of oxytocin was solved in 500 cc ringer serum and was injected. Besides, a 5 percent sugar serum through an interface was considered to prevent the reduction of body fluids and the blood sugar. Therefore, the volunteering individual received 120 cc liquid in an hour. The induction started with 6 mili-units/ minute and 6 mili-units were added, every 30 minutes till the effective labor contraction flourished. After the active phase (dilation of 4 cm and 80 percent effacement or dilatation of 5 cm without considering dilatation), the envelopes were opened by the shift supervisor and the ringer serum were totally changed according to the placement of the volunteer in each group. For the first group which is the control group, 500 cc ringer serum with 5 units of infusion oxytocin and for the experiment group, one ringer serum without oxytocin was injected. The serums were regulated with the previous speed. The shift supervisor had tagged his intended code on the ringer according to the type of the group and only he was aware of the contents of the serums. After this, the researcher observed, examined and recorded the intended data like the previous order. The means of data collection in this study was a questionnaire alongside a checklist. In order to define the scientific validity of the collected means, the content validity method was used. In other words, following the study of all the reliable references in this regard, a checklist was provided and it was then evaluated by virtue of content quality and assessed by a group of faculty members of Isfahan University of Medical Sciences. All the stages of research were conducted by the researcher and two experienced interviewers in a manner that through three scientific sessions, all the diagnosis criteria and the methodology were homogenized between the researcher and the interviewers and the performance of the interviewers was randomly evaluated by the researcher during the study.
All routine cares were followed similarly for all the volunteers. In both groups, the third stage of labor was controlled by 1 liter of ringer with 20 units of oxytocin. Among the 120 participants, 5 individuals from the control group and 5 individuals from the experiment group exited from the study due to lack of progression. 110 individuals’ data were analyzed by the SPSS software, version 17 via student t-test and chi-square test.
In order to describe the data related to individuals in this study, the descriptive analytical techniques for quantitative variables and frequency percentage for qualitative variables were applied. Luann teat was used to attain normal distribution in quantitative variables and variance equation. In order to compare the mean of quantitative variables in different groups, the student t-test and for comparing the frequency distribution of some of the data, the chi-square test was used. The level of significance was considered 0.05.
Results
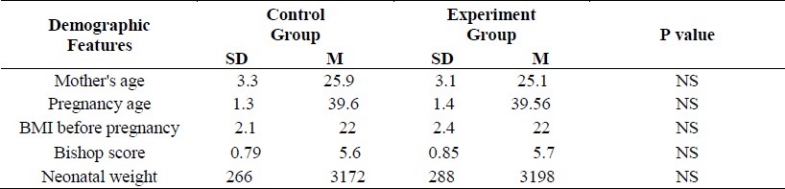
There was no significant difference between the control and the experiment groups with regard to demographic features such as age, body mass index before pregnancy, weight of infant, bishop score, the volume of distributed fluids till the active phase of labor, age of pregnancy, and number of parity. The frequency rate of the reasons for induction did not have any significant difference in the two groups (p > 0.05) (Table 1).
Table 1.
Comparison of demographic features between control and experiment groups
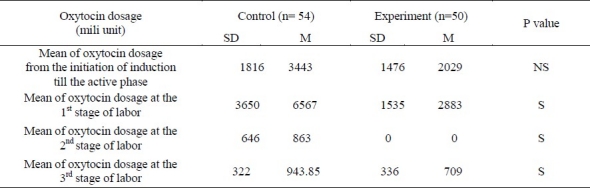
Considering the goal mentioned in the introduction, the results showed that the mean of the first stage (p > 0.05, t = 1.13) and the second stage (p > 0.05, t = 0.62) between the two groups did not have any statistically significant difference (Table 2). But, the mean duration of the third stage had a significant difference between the two groups (p < 0.05, t = 2.25) so that the duration of this stage was shorter in the group that did not receive oxytocin after the active phase. The mean oxytocin dosage at the first, second and the third stages of labor had a significant difference in a way that this amount was lower in the group that did not receive oxytocin after the active stage (the experiment group) than in the group received oxytocin till the end of the second stage of labor (the control group, p < 0.001) (Table 3).
Table 2.
Comparison of duration of labor stages between control and experiment groups
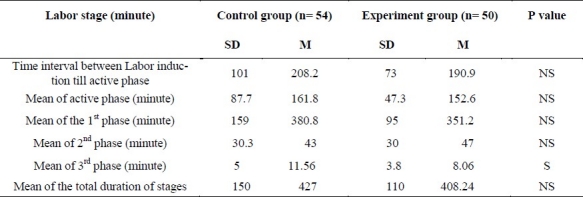
Table 3.
Mean of dosage of oxytocin in different labor stages
Discussion
Although the industrial oxytocin is the most common used medicine in modern midwifery, there are different viewpoints regarding its prescription and wide ranges have been proposed regarding the amount of consumption and time intervals required for increasing the amount of the medicine.
In this study, there was no significant difference in comparing the mean duration of the first, second and labor stages between the two groups. But, the mean duration of the third stage had a significant difference between the two groups (P < 0.05), so that the duration of this stage was shorter in the group that did not receive oxytocin after the active phase. The shortening of this stage can lead to a reduction in the effects of this stage.
Up to now, two studies have been done in 2004 and 2007 by Daniel-Spiegel et al and Ustunyurt et al respectively9,10 which showed the effects of stopping the oxytocin after the initiation of the active phase on induction. Daniel-Spiegel et al showed through a study in 2004 on 104 aid seekers that even the duration of labor decreased in a group which did not receive oxytocin and the frequency of cesarean and intensified cramps also decreased and hence, the author concluded that the infusion of oxytocin can be stopped after the initiation of the active stage without having any effect on the duration of labor.
In Ustunyurt et al's study in 2007, no significant difference was seen between the duration of labor stages in the two groups despite the fact that the duration of labor stages had seemingly shortened in the group that received oxytocin.
This study and other previously done studies have shown that if oxytocin is stopped after the initiation of induction and after reaching the active labor phase, it will not have any effects on labor stages; in other words, it will not lead to the lengthening or stopping the cramps. Thus, it can be stated that the labor induction procedure can be changed into a physiological procedure by this method and in countries in which the 1:1 proportion of midwife to patient under induction cannot be observed, the intensive cares for controlling the medicine during prescription can be decreased.
With regard to the usage dosage of oxytocin, there was also a significant difference between the two groups in Spiegel and Steinhart's studies and the present research so that the usage dosage of the oxytocin was lower in a group that did not receive oxytocin after the active phase of labor compared to the group that received oxytocin till the end of labor. Still, some studies have pointed out to the long-term effects of oxytocin on infants whose mothers had used oxytocin for induction of their labor. For example, Katherine Kurt (2008) found a significant difference in her study between the hyperactivity of children and their mothers’ induction of labor with oxytocin.3 She found that labor induction by oxytocin and the time within which the help seeker has been under labor induction with oxytocin and also the dosage of the taken medicine are 3 important factors with relation to this disorder (p < 0.001, relation amount: 70 %). By attending to this fact that this medicine was categorized in 2007 among a high-alert medicines, and new reports are released about its probable long-term effects, it is better to use the instructions that lead to the reduction of oxytocin usage during induction so that its side effects are lowered which can finally result in providing security for the pregnant woman and her infant during labor.
It was made clear in this study that stopping oxytocin after the active phase in inducing labor not only does not have any effects on labor stages also it can change the labor induction procedure into a physiological procedure which in itself leads to a decrease in the number of more human personnel for providing required intensive cares. This issue can have a significant effect on decreasing the deaths caused by a lack of human personnel or the medical and midwifery errors, especially in countries in which the proportion of midwife to patient is more than 1:2. On the other hand, by using instructions that lead to the reduction of using oxytocin during the induction, its probable long-term effects in future could be decreased. Nonetheless, in order to verify this issue, additional studies with more samples are needed.
The authors declare no conflict of interest in this study.
Acknowledgments
Thanks to Dr. Elham Zarean, Midwifery Specialist, Dr. Sadeghi, Women and Midwifery Specialist, Dr. Tahereh Nasr Isfahani, Teriza Basirat, B.S in Midwifery, Maryam Doudangeh, B.S in Midwifery, Gholam Hossein Dehghani, Shariati Hospital supervisor, residents and interns at Shahid Beheshti Hospital, authorities at Shariati and Beheshti Hospitals.
References
- 1.Canningham L, Bloom H. In: Pregnancy and childbirth Williams. Ghazei Jahan B, Aghsa Malek M, translators. Tehran: Golban Publication; 2005. p. 11. Pregnancy and childbirth Williams Trans Ghazei Jahan B, Aghsa Malek M Tehran: Golban Publication; 2005 p 11. [Google Scholar]
- 2.Littleton LY, Engebretson J. Maternal, neonatal, and women's health nursing. New York: Cengage Learning; 2004. [Google Scholar]
- 3.Kurth CL. The relationship between AD/HD and perinatal (oxytocin) Pitocin induction: Risk for developmental adversity? Northcentral University [Online] 2008. Available from: URL: http://gradworks.umi.com/33/10/3310167.html/
- 4.Durodola A, Kuti O, Orji EO, Ogunniyi SO. Rate of increase in oxytocin dose on the outcome of labor induction. Int J Gynaecol Obstet. 2005;90(2):107–11. doi: 10.1016/j.ijgo.2005.04.010. [DOI] [PubMed] [Google Scholar]
- 5.Simpson KR, Knox GE. Oxytocin as a high-alert medication: implications for perinatal patient safety. MCN Am J Matern Child Nurs. 2009;34(1):8–15. doi: 10.1097/01.NMC.0000343859.62828.ee. [DOI] [PubMed] [Google Scholar]
- 6.Clayworth S. The nurse's role during oxytocin administration. MCN Am J Matern Child Nurs. 2000;25(2):80–4. doi: 10.1097/00005721-200003000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Robinson CJ, Schuman R. South Carolina OB-GYN Associates [Online] 2003. pp. 479–502. Available from: URL: www.scobgyn.com/
- 8.Phaneuf S, Rodriguez LB, TambyRaja RL, MacKenzie IZ, Lopez BA. Loss of myometrial oxytocin receptors during oxytocin-induced and oxytocin-augmented labour. J Reprod Fertil. 2000;120(1):91–7. doi: 10.1530/jrf.0.1200091. [DOI] [PubMed] [Google Scholar]
- 9.Daniel-Spiegel E, Weiner Z, Ben Shlomo I, Shalev E. For how long should oxytocin be continued during induction of labour? BJOG. 2004;111(4):331–4. doi: 10.1111/j.1471-0528.2004.00096.x. [DOI] [PubMed] [Google Scholar]
- 10.Ustunyurt E, Ugur M, Ustunyurt BO, Iskender TC, Ozkan O, Mollamahmutoglu L. Prospective randomized study of oxytocin discontinuation after the active stage of labor is established. J Obstet Gynaecol Res. 2007;33(6):799–803. doi: 10.1111/j.1447-0756.2007.00659.x. [DOI] [PubMed] [Google Scholar]


