Abstract
For Ebola virus (EBOV), 4 different species are known: Zaire, Sudan, Côte d’Ivoire, and Reston ebolavirus. The newly discovered Bundibugyo ebolavirus has been proposed as a 5th species. So far, no cross-neutralization among EBOV species has been described, aggravating progress toward cross-species protective vaccines. With the use of recombinant vesicular stomatitis virus (rVSV)–based vaccines, guinea pigs could be protected against Zaire ebolavirus (ZEBOV) infection only when immunized with a vector expressing the homologous, but not a heterologous, EBOV glycoprotein (GP). However, infection of guinea pigs with nonadapted wild-type strains of the different species resulted in full protection of all animals against subsequent challenge with guinea pig–adapted ZEBOV, showing that cross-species protection is possible. New vectors were generated that contain EBOV viral protein 40 (VP40) or EBOV nucleoprotein (NP) as a second antigen expressed by the same rVSV vector that encodes the heterologous GP. After applying a 2-dose immunization approach, we observed an improved cross-protection rate, with 5 of 6 guinea pigs surviving the lethal ZEBOV challenge if vaccinated with rVSV-expressing SEBOV-GP and -VP40. Our data demonstrate that cross-protection between the EBOV species can be achieved, although EBOV-GP alone cannot induce the required immune response.
In the preceding 3 decades, 4 different Ebola virus (EBOV) species have been identified: Zaire ebolavirus (ZEBOV), Sudan ebolavirus (SEBOV), Côte d’Ivoire ebolavirus (CIEBOV), and Reston ebolavirus (REBOV) [1]. The newly discovered Bundibugyo ebolavirus (BEBOV) has been proposed as the fifth EBOV species [2]. ZEBOV is the most pathogenic species, with a case-fatality rate of up to 90%, followed by SEBOV with about 50% and the newest member BEBOV with about 25% [1, 2]. CIEBOV and REBOV have not yet been associated with fatal human cases, but have been shown to be lethal in nonhuman primates [3–5]. ZEBOV, SEBOV, and BEBOV are important public health concerns in Central Africa where their endemic areas overlap [1, 2]. Despite serological cross-reactivity, there are no reports of cross-protective immune responses among the species, which has impeded the development of EBOV countermeasures [1].
Although EBOV and Ebola hemorrhagic fever have been studied extensively, today there is neither a licensed vaccine nor treatment available. However, over the last few years enormous progress has been made in developing experimental vaccines and postexposure treatment schemes using several different approaches: small interfering RNA, phosphorodiamidate morpholino oligomers, DNA vaccination, virus-like particles (VLPs), Venezuelan equine encephalitis virus replicons (VEEV RPs), replication incompetent adenovirus serotype 5 vectors, replication-deficient EBOV, and replication competent viral platforms (human parainfluenzavirus 3 [HPIV3] and recombinant vesicular stomatitis virus [rVSV]) [6–8].
Currently, among the most-promising strategies is the rVSV-based vaccine, which expresses the EBOV glycoprotein (GP) as the immunogen [9, 10]. Its protective efficacy has been demonstrated in 3 relevant EBOV animal models [11], including immunocompromised nonhuman primates [12]. The value of rVSV in postexposure treatment against lethal challenge with EBOV or Marburg virus has also been successfully evaluated in nonhuman primate models [13–15], and recently an rVSV-based vaccine was administered to a laboratory worker following exposure to ZEBOV [16]. Despite promising protective efficacy against homologous challenge, a single-injection vaccine has not demonstrated cross-protective value against heterologous challenge with viruses from a different genus or species [6]. Cross-protection in nonhuman primates was previously observed in 2 survivors of a CIEBOV infection that subsequently also survived infection with SEBOV (strain Gulu) or ZEBOV (strain Kikwit) [17]. In contrast, nonhuman primates that were immunized with rVSV-expressing ZEBOV-GP were protected against a ZEBOV challenge but not against a subsequent SEBOV infection [18]. In a first attempt to achieve cross-protection with the rVSV vaccine, viruses expressing different GPs as immunogens were successfully administered as a blended vaccine approach and resulted in complete protection against challenge with the individual homologous virus and CIEBOV, a heterologous virus [17]. Recently, a report by Hensley and colleagues showed cross-protective immunity against BEBOV elicited using an adenovirus-based prime/boost vaccination approach with SEBOV-GP and ZEBOV-GP as antigens [19]. However, a single cross-protective vaccine against all human pathogenic filoviruses in Central Africa would clearly be the most desirable approach.
In this study, we have evaluated the cross-protective potential of second-generation rVSV vectors expressing different EBOV immunogens, or combinations of immunogens, in rodent models. We found that GP is sufficient to provide cross-protective efficacy in the mouse but not in the guinea pig model. Cross-species protection in the guinea pig model could be achieved only through a 2-dose vaccination scheme using a dual rVSV expression vector encoding SEBOV-GP and SEBOV viral protein 40 (VP40). The success of this approach might be partially explained by the generation of SEBOV-like particles, which are a byproduct of the newly designed immunization vector. This new vaccine is a promising candidate for testing in nonhuman primates.
MATERIALS AND METHODS
Cell Culture and EBOV Propagation
293T and Vero cell lines were obtained from ATCC and cultured in Dulbecco’s modified Eagle’s medium (DMEM; Sigma) supplemented with 10% fetal bovine serum (FBS), penicillin/streptomycin, and l-glutamine in a 37°C incubator, 5% CO2. CIEBOV, REBOV (strain Pennsylvania), SEBOV (strain Boniface), and ZEBOV (strain Mayinga) as well as the guinea pig–adapted and mouse-adapted variants of ZEBOV (GPA-ZEBOV and MA-ZEBOV, respectively) [20, 21] and ZEBOV-expressing green fluorescent protein (ZEBOV-GFP) [22] were propagated in Vero cells. The supernatants were cleared of cell debris by centrifugation at 1500 × g for 10 minutes, aliquoted, and stored in liquid nitrogen. Viral titers were determined by conducting immunoplaque assays. All infectious work with EBOV was performed in the biosafety level 4 laboratories at the National Microbiology Laboratory (NML) of the Public Health Agency of Canada (PHAC) or the Integrated Research Facility (IRF) of the Rocky Mountain Laboratories (RML), Division of Intramural Research (DIR), National Institute of Allergy and Infectious Diseases (NIAID), National Institutes of Health (NIH).
VSV Plasmid Construction and Virus Rescue
We generated pATX-VSVΔG-XN2 by cloning the previously described VSV-backbone (kindly provided by J. Rose, Yale University) [9, 10] into pATX-MCS using the restriction enzymes NotI and SpeI. Additionally, polymerase chain reaction (PCR) mutagenesis was performed to create Mlu I and Avr II restriction enzyme sites flanking VSV-G (Figure 1A). The final vector contains 2 transcription units allowing the insertion of EBOV-GP, as well as an additional antigen downstream of GP, in the VSV genome (Figure 1A). All EBOV genes were PCR-amplified with the appropriate oligonucleotides, inserted into pATX-VSVΔG-XN2 via the MluI and AvrII or XhoI and NheI restriction sites and the resulting vectors were confirmed by sequencing. Helper plasmids encoding T7 polymerase, VSV polymerase (L), VSV nucleoprotein (N) and VSV phosphoprotein (P) have been described elsewhere [9, 10]. For virus recovery, a coculture of Vero and 293T cells was cotransfected with pATX-VSVΔG-XN2 encoding the respective antigen(s), as well as the 4 helper plasmids, using Lipofectamine 2000 (Life Technologies). Seventy-two hours after transfection, the supernatant was transferred onto fresh Vero cells. Cytopathic effect (CPE) and, therefore, rVSV replication could be detected 24–72 hours later. For larger virus preparations, Vero cells were infected with the initially rescued rVSV at a 1:1000 dilution and harvested when about 70% of the cells showed CPE. The supernatant was then cleared of cell debris by centrifugation at 1500 × g for 10 minutes, aliquoted, and stored at −80°C. All recovered viruses were characterized by reverse-transcription polymerase chain reaction (RT-PCR) and Western blot analysis for EBOV antigen expression with antibodies kindly provided by A. Takada (Hokkaido University, Japan) and Y. Kawaoka (University of Wisconsin, Madison). Viral titers were determined by performing conventional plaque assays.
Figure 1.
Recombinant vesicular stomatitis virus vector development, antigen expression, and virus-like particle formation. A, Illustration of the newly designed single or dual recombinant vesicular stomatitis virus (rVSV) vectors encoding different Ebola virus (EBOV) antigens. The vesicular stomatitis virus glycoprotein (VSV-G) gene was excised using Mlu I and Avr II digestion. The first antigen was cloned into the genome backbone using the same restriction enzymes used to delete the VSV-G gene. The second antigen was inserted downstream of the VSV-G gene as an additional transcriptional unit using the restriction enzymes Xho I and Nhe I. B, Expression of foreign antigens. Western blot analysis was performed on cell lysates and supernatant of rVSVwt/S-NP–, rVSV-S-GP/VP40–, or rVSVwt/S-VP24–infected Vero cells. Expression of the EBOV antigens was detected using monoclonal antibodies directed against the nucleoprotein (NP), viral protein 40 (VP40), or viral protein 24 (VP24). C, Release of recombinant viral particles and virus-like particles. Supernatants of cells infected with rVSVwt/S-VP40 (top) and rVSV-S-GP/VP40 (bottom) were purified through a 20% sucrose cushion and analyzed by electron microscopy for production of rVSV particles (bullet-shape smaller particles) and Sudan ebolavirus (SEBOV)–like particles (long filamentous particles; indicated by arrow).
Electron Microscopy
rVSVs were concentrated by centrifugation through a 20% sucrose cushion and fixed in 2.5% glutaraldehyde and 4% paraformaldehyde in a 0.1 M sodium cacodylate buffer. Samples of 5 μL were spotted on 200 mesh formvar-coated copper grids (Electron Microscopy Sciences) for 5 minutes. After excess liquid was blotted, the grids were stained with 1% aqueous uranyl acetate (UA) for 5 minutes and viewed on a Tecnai BioTwin Spirit transmission electron microscope (TEM; FEI) at 120 kV. Digital images were acquired with a Hamamatsu XR-100 digital camera system (Advanced Microscopy Techniques).
Animal Experiments
Female BALB/c mice (6 weeks of age) as well as female Hartley guinea pigs (about 250 g) were obtained from Charles River Laboratories and housed in HEPA-filtered microisolator cage systems. Animals were vaccinated intraperitoneally with a single dose of 1 × 104 plaque-forming units (PFU) to mice or 2 × 105 PFU to guinea pigs of rVSV. Mice were infected 21 days after vaccination with 1000 median lethal dose (LD50) of MA-ZEBOV [21]. Blood samples were collected from anesthetized guinea pigs, using an anterior vena cava bleeding technique, 21 days after vaccination. Animals were subsequently challenged with 1000 LD50 of GPA-ZEBOV [20] or boosted with the same dose of rVSV and challenged 3 weeks later. All animals were weighed daily and monitored for signs of illness. On necropsy days, guinea pigs and mice were anesthetized, bled, and euthanized with an overdose of isoflurane before liver and spleen samples were taken. Surviving animals were sacrificed 3 weeks after challenge, and serum was collected for antibody titrations. All animal work was approved by the Institutional Animal Care and Use Committees and performed following the guidelines of the Canadian Council on Animal Care and the Association for Assessment and Accreditation of Laboratory Animal Care, International by certified staff in approved facilities.
Quantitative Real-time RT-PCR
RNA from blood was isolated using the QIAmp viral Mini RNA kit (QIAGEN); RNA from liver and spleen samples was prepared using the RNeasy Mini kit (QIAGEN). All quantitative real-time RT-PCRs were performed using the QIAquick 1-step Rotorgene kit (QIAGEN). The ZEBOV specific primers and probe were based on the nucleoprotein (NP; bp 2661–2721, GenBank accession number AF086833). Real-time RT-PCRs were performed on a Rotor-Gene 6000 machine, and data were analyzed using the Rotor-Gene 6000 Series software (QIAGEN).
Humoral Immune Responses in Guinea Pigs
Antigens for the enzyme-linked immunosorbent assay (ELISA) were produced as described below. EBOV-GP and VSV-G open reading frames lacking the transmembrane domain (ΔTM) but encoding a histidine tag at the C-terminus were cloned into pCAGGS, expressed in 293T cells, and purified as reported by Nakayama et al [23]. SEBOV-like particles were produced by transfection of 293T cells with a SEBOV-VP40 expression plasmid. After 48 hours, the supernatant containing VP40-VLPs was harvested. The VLPs were then purified through a 20% sucrose cushion and treated with 0.05% Triton X-100 in phosphate-buffered saline (PBS) prior to storage at −80°C. Guinea pig sera were inactivated by γ-irradiation (5 MRad). ELISA with SEBOV-GPΔTM was performed as described previously [23]. VLPs were used as ELISA antigen in a 1:100 dilution.
Neutralization Assay
Neutralizing antibody titers were determined by performing focus reduction neutralization titration assays (FRNT). Vero cells were seeded into 96-well plates to generate a confluent monolayer on the day of infection. Serum dilutions were prepared in PBS and 10 μL were incubated with 100 focus-forming units (FFU) of ZEBOV-GFP [22] in a total volume of 20 μL. After 30 min at 37°C, the media was removed from cells, the serum-virus mixture was added, and samples were incubated for 60 minutes at 37°C. Then the mixture was removed from the cells, and 100 μL of 1.2% carboxymethylcellulose-MEM was added per well and left for 4 days at 37°C. The neutralizing antibody titer of a serum sample was considered positive at a dilution showing a >80% reduction (FRNT 80) in GFP-foci compared with the control without serum.
RESULTS
Generation of rVSV Vectors Capable of Expressing 1 or 2 EBOV Immunogens
To address cross-protective efficacy of the rVSV vectors expressing EBOV-GP as the immunogen, we generated a new VSV full-length genome plasmid designated pATX-VSVΔG-XN2 (Figure 1A). The VSV-G gene in the plasmid was deleted through Mlu I and Avr II digestion and replaced with EBOV-GP open reading frames cloned individually into the Mlu I and Avr II sites (Figure 1A). In addition, this vector contained a second insertion site (Xho I and Nhe I) in the VSV genome that could be used to add a second EBOV gene: NP, VP40, or VP24 (Figure 1A). Initially, we used this new vector to generate single GP-expressing rVSVs representative of each EBOV species, BEBOV, CIEBOV, REBOV, SEBOV, and ZEBOV (rVSV-B-GP, rVSV-CI-GP, rVSV-R-GP, rVSV-S-GP, and rVSV-Z-GP, respectively) (Figure 1A). All rVSVs were rescued following cotransfection of the recombinant full-length genome plasmid with expression plasmids encoding the T7 polymerase, VSV-N, VSV-P, and VSV-L. EBOV-GP expression and rVSV particle formation were analyzed by electron microscopy and Western blot (Figure 1B and C).
rVSV Vaccine Vectors Expressing Different EBOV-GPs Confer Cross-Protective Immunity in Mice
We evaluated the cross-protective potential of the rVSV vaccine vectors expressing EBOV-GPs as a single antigen by immunizing groups of mice with a single intraperitoneal dose of DMEM (control), rVSV wild-type (rVSVwt), or the different rVSV vaccines (1 × 104 PFU). At 3 weeks after immunization, all mice were challenged with a lethal dose of MA-ZEBOV (1000 LD50) and monitored daily for weight loss and signs of disease. Most control and rVSVwt immunized mice succumbed to infection as expected between day 5 and 7 [21, 24], but 20% of these animals survived after developing severe disease signs (Table 1), a phenomenon that we occasionally observe in this challenge model (unpublished data). All mice vaccinated with the heterologous rVSV-CI-GP or rVSV-R-GP or the homologous rVSV-Z-GP remained asymptomatic and were protected from lethal MA-ZEBOV challenge (Table 1). Interestingly, only 15 of 20 animals immunized with rVSV-S Boniface-GP survived the challenge (Table 1), demonstrating that this recombinant virus is less potent in inducing a cross-protective immune response to ZEBOV. Furthermore, we examined and compared viral RNA (vRNA) levels in the blood of infected animals on day 5 postchallenge using quantitative real-time RT-PCR. We were unable to detect challenge virus RNA in the blood samples from mice vaccinated with the homologous rVSV-Z-GP vector, whereas all other animals developed viremia (Figure 2). Notably, only animals with vRNA levels greater than 2 × 107 genome equivalents per 1 mL blood developed disease and succumbed to infection (Figure 2).
Table 1.
Recombinant Vesicular Stomatitis Virus Ebola Virus Glycoprotein Cross-Protective Efficacy in Rodent Models
| Mice MA-ZEBOV | Guinea Pigs GPA-ZEBOV | |||
| Vaccine | survival (n survival/n total) | Time to death (d) | Survival (n survival/n total) | Time to death (d) |
| Control | 4/21 | 6.5 ± 1.5 | 0/6 | 7.3 ± 0.5 |
| rVSVwt | 5/21 | 5.6 ± 1.6 | 0/6 | 7.0 ± 0 |
| rVSV-B-GP | n.d. | n.a. | 1/6 | 9.4 ± 3.1 |
| rVSV-CI-GP | 22/22 | n.a. | 1/6 | 9.4 ± 2.3 |
| rVSV-R-GP | 20/20 | n.a. | 1/6 | 9.2 ± 2.5 |
| rVSV-S Boniface-GP | 15/20 | 6.8 ± 0.4 | 0/6 | 7.7 ± 0.5 |
| rVSV-S Gulu-GP | n.d. | n.a. | 0/6 | 7.8 ± 0.4 |
| rVSV-Z Mayinga-GP | 20/20 | n.a. | 6/6 | n.d. |
| rVSV-Z Kikwit-GP | n.a. | n.a. | 4/4 | n.a. |
NOTE. B = Bundibugyo ebolavirus (BEBOV); CI = Côte d'Ivoire ebolavirus (CIEBOV); GP = glycoprotein; GPA = guinea pig–adapted; MA - mouse-adapted; rVSV = recombinant vesicular stomatitis virus; R = Reston ebolavirus (REBOV); S = Sudan ebolavirus (SEBOV); wt = wild-type; Z = Zaire ebolavirus (ZEBOV); n.a., not applicable; n.d., not done.
Figure 2.
Detection of mouse-adapted Zaire ebolavirus (MA-ZEBOV) genome equivalents in mice immunized with recombinant vesicular stomatitis virus (rVSV) vectors expressing different Ebola virus glycoproteins (EBOV-GPs). Mice (n = 5) were vaccinated with a single dose of rVSV vectors and challenged 3 weeks later with 1000 median lethal dose (LD50) of MA-ZEBOV. Animals were killed 5 days postchallenge, blood samples were collected, and RNA was extracted. Quantitative real-time reverse-transcriptase polymerase chain reaction (RT-PCR) data are shown as genome equivalents per 1 mL blood. Error bars represent the standard error of the mean.
rVSV Vaccine Vectors Expressing EBOV-GPs Do Not Confer Cross-Protective Immunity in Guinea Pigs
As a next step, we determined cross-protection in the more stringent guinea pig model for ZEBOV [11]. Given the reduced cross-protection with the rVSV-S Boniface-GP, derived from the Boniface strain isolated in 1976, we also included a rVSV-S Gulu-GP, representing a distinct SEBOV strain isolated in 2000 [1, 25]. In addition, we also added rVSV-Z Kikwit-GP, representing a more recent strain of ZEBOV [1, 25]. Guinea pigs were immunized intraperitoneally with 2 × 105 PFU of the respective rVSV vaccine vectors (Table 1), rVSVwt or DMEM (control) and challenged 3 weeks later with a lethal dose of GPA-ZEBOV (1000 LD50). All control and rVSVwt-immunized guinea pigs succumbed to infection between days 7 and 8, whereas rVSV-Z Mayinga-GP and rVSV-Z Kikwit-GP vaccinated animals survived the homologous challenge without signs of illness (Table 1). In contrast, animals vaccinated with rVSV vectors expressing heterologous BEBOV-GP, CIEBOV-GP, or REBOV-GP developed severe disease and 5 of 6 (83%) animals in each group succumbed to infection between days 8 and 13 (Table 1). Interestingly, rVSV vectors expressing SEBOV-GPs did not induce any cross-protective immune responses and disease progression in vaccinated animals was similar to that in control animals (Table 1). These results demonstrate that the EBOV-GP is not sufficient to elicit effective cross-species protective immunity in the guinea pig model.
EBOV Infection Confers Cross-Species Protection in Guinea Pigs
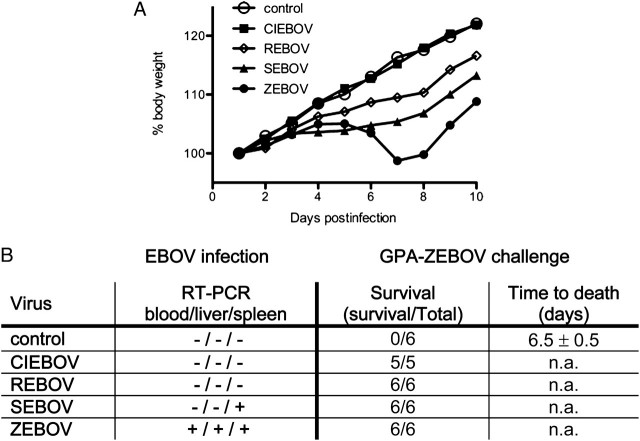
Cross-protection among different EBOV species has been demonstrated in the mouse model [26] and to test whether this can also be achieved in the guinea pig model, groups of 6 animals were infected intraperitoneally with 2 × 105 FFU of wild-type ZEBOV, SEBOV, CIEBOV, or REBOV and monitored daily for weight loss and signs of illness. None of the wild-type (non–rodent-adapted) EBOV-infected animals developed signs of disease, but compared with control animals (DMEM-treated), a reduced weight gain was noticed in all groups with the exception of the CIEBOV-infected animals, indicating virus replication in these animals (Figure 3A). The ZEBOV-infected animals were the only ones with weight loss over several days, an observation that might explain the success in adapting this EBOV species to uniform lethality in guinea pigs (Figure 3A) [20, 27], which has not been reported for any other EBOV species. To monitor virus replication, liver, spleen, and blood samples from infected animals were taken on day 5 postinfection, and RNA levels were analyzed using quantitative real-time RT-PCR. EBOV-specific RNA could be detected only in SEBOV (strain Boniface)– and ZEBOV (strain Mayinga)–infected animals, indicating virus replication (Figure 3B). However, virus isolation was positive only from liver and spleen of ZEBOV-infected guinea pigs (data not shown). At 3 weeks after the initial infection, all animals were challenged with a lethal dose of GPA-ZEBOV (1000 LD50). Although the control animals succumbed to infection, all other guinea pigs were completely protected against disease and survived (Figure 3B). This demonstrates that cross-species protection can be achieved in the guinea pig model but most likely requires additional EBOV immunogens, not only GP.
Figure 3.
Ebola virus infection induces cross-protective immunity against heterologous lethal challenge in guinea pigs. Guinea pigs (n = 6) were infected with Dulbecco’s modified Eagle’s medium (DMEM; control) or nonadapted viruses representing the different Ebola virus (EBOV) species and monitored daily for weight loss (A). In addition, we analyzed the presence of viral RNA in blood, liver, and spleen at day 5 postinfection (B). Survival was monitored following guinea pig–adapted Zaire ebolavirus (GPA-ZEBOV) challenge (B). +, RT-PCR positive; −, RT-PCR negative; n.a., not applicable.
Blended and Dual rVSV-SEBOV Vaccine Vectors Do Not Confer Cross-Protection in the Guinea Pig Model After a Single Vaccination
The complete lack of cross-protection with SEBOV-GP in guinea pigs (Table 1) provided a suitable background for identifying important cross-protective immunogens. A new set of dual foreign gene–expressing rVSV vectors was generated encoding SEBOV (strain Boniface) NP, SEBOV-VP40 or SEBOV-VP24 as a second immunogen in combination with either SEBOV-GP or VSV-G (VSVwt) (Figure 1A; Table 2). Virus particle formation and foreign gene expression were confirmed by electron microscopy and Western blot analysis (Figure 1B and C). rVSVs expressing VP40 were of particular interest because they possess the ability to release SEBOV-like particles from the rVSV-infected cells (Figure 1C, arrows). Guinea pigs were immunized intraperitoneally once with 2 × 105 PFU of vaccine in the combinations outlined in Table 2. Animals were challenged 3 weeks later with 1000 LD50 of GPA-ZEBOV and monitored daily for weight loss and signs of illness. None of the antigen combinations tested resulted in a significant increase in survival, although with GP and VP40 present as antigens, 2 of 6 guinea pigs survived the lethal challenge (Table 2).
Table 2.
Cross-Protective Potential of Different Ebola Virus Immunogen Combinations in Guinea Pigs
| GPA-ZEBOV | ||
| Immunogen(s) | Survival (n survival/n total) | Time to death (d) |
| rVSVwt | 0/8 | 7.8 ± 1.0 |
| rVSV-Z-GP | 8/8 | n.a. |
| rVSV-S-GP | 1/6 | 7.8 ± 0.8 |
| rVSVwt/S-NP | 0/6 | 6.3 ± 0.5 |
| rVSVwt/S-VP40 | 0/6 | 7.5 ± 0.5 |
| rVSV-S-GP/NP | 1/6 | 9.0 ± 2.3 |
| rVSV-S-GP/VP40 | 1/6 | 8.6 ± 1.3 |
| rVSV-S-GP/NP + rVSVwt/S-VP24 | 0/6 | 7.2 ± 0.4 |
| rVSV-S-GP/NP + rVSV-S-GP/VP40 | 2/6 | 7.0 ± 0.8 |
| rVSV-S-GP/VP40 + rVSVwt/S-VP24 | 2/6 | 7.5 ± 1.3 |
| rVSV-S-GP/NP + rVSV-S-GP/VP40 + rVSVwt/S-VP24 | 1/6 | 7.8 ± 1.6 |
NOTE. GP, glycoprotein; GPA-ZEBOV, guinea pig–adapted Zaire ebolavirus; NP 5 nucleoprotein; rVSV, recombinant vesicular stomatitis virus; S, SEBOV Boniface; VP24, viral protein 24; VP40, viral protein 40; wt, wild-type; Z, ZEBOV Mayinga; n.a., not applicable.
A 2-Dose Regime of Selected rVSV-SEBOV Vaccine Vectors Confers Cross-Species Protection in the Guinea Pig Model
To determine if protection could be improved with a 2-dose immunization approach, we tested different combinations of single or dual antigen expressing rVSV-SEBOV vectors for cross-species protection in guinea pigs. The 2 vaccine doses (2 × 105 PFU per dose, intraperitoneally) were administered 3 weeks apart, and animals were challenged 21 days after the second immunization with a lethal dose of GPA-ZEBOV (1000 LD50). Only 1 of 6 animals vaccinated with rVSV-S-GP/VP40 succumbed to infection, whereas all other animals in this group were completely protected against disease (Figure 4). Interestingly, when SEBOV-NP was present as an immunogen weight loss in animals was increased and cross-species protection was reduced (Figure 4). Analysis of antibody levels in the serum of rVSV-S-GP/VP40–vaccinated guinea pigs demonstrated an increased level of immunoglobulin G (IgG) antibodies against both immunogens following the second vaccination (Figure 5A). IgG antibody titers did not increase after challenge (Figure 5A; day 66), indicating a lack of virus replication in the protected animals. The sera were further tested in neutralization assays against ZEBOV but did not show any neutralizing ability (Figure 5B, upper part). In contrast, sera collected from guinea pigs immunized with the homologous rVSV-Z-GP showed FRNT80 titers of up to 1:80 (Figure 5B, bottom part).
Figure 4.
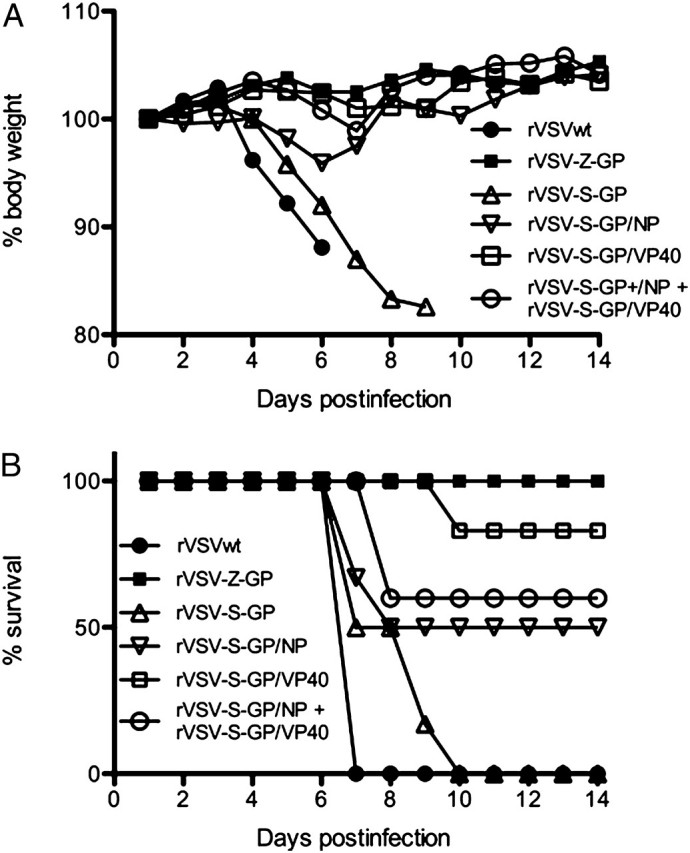
Cross-species protection following a 2-dose vaccination regime using a dual recombinant vesicular stomatitis virus (rVSV) vector expressing Sudan ebolavirus antigens. Guinea pigs (n = 6) were vaccinated twice (day 0, day 21) with the indicated rVSV vaccine vectors and challenged 42 days after the initial immunization with 1000 median lethal dose (LD50) of guinea pig–adapted Zaire ebolavirus. Animals were monitored for weight loss (A) and survival (B).
Figure 5.
Humoral immune responses following vaccination with rVSV-S-GP/VP40. Guinea pigs were vaccinated twice (day 0, day 21) with the indicated recombinant vesicular stomatitis virus (rVSV) vaccine vectors and challenged 42 days after the initial immunization with 1000 median lethal dose (LD50) of guinea pig–adapted Zaire ebolavirus (GPA-ZEBOV). Humoral immune responses to vaccination were analyzed on day 21 (prior to second immunization), day 42 (prior to challenge), and day 66 (convalescence) using (A) enzyme-linked immunosorbent assay (ELISA) and (B) focus reduction neutralization titration assay (FRNT). A, Sudan ebolavirus glycoprotein (SEBOV-GP)–specific antibodies were detected using purified recombinant expressed SEBOV-GPΔTM. Viral protein 40 (VP40)–specific antibodies were detected using SEBOV-VP40 virus-like particles (VLPs). Error bars represent the standard error of the mean (SEM; n = 6). B, FRNT assay was performed to detect neutralizing antibodies against Zaire ebolavirus (ZEBOV) in the sera of rVSV-S-GP/VP40 (top; n = 6) and rVSV-Z-GP (bottom; n = 2) immunized guinea pigs. Error bars represent SEM.
DISCUSSION
The presented study demonstrates that a 2-dose vaccination approach with rVSV-S-GP/VP40 can protect guinea pigs from a lethal challenge with heterologous ZEBOV (Figure 4). Until now, only blended vaccine approaches with rVSVs or complex adenoviral vectors using a prime/boost strategy have been shown to induce cross-species protective immunity in the nonhuman primate model [17, 19, 28]. Our goal was to develop 1 single-dose rVSV vaccine vector inducing a cross-species protective immune response against all African EBOVs. In a first experiment, the well-characterized rVSV-Z-GP vaccine [6], as well as rVSVs expressing either BEBOV-GP, CIEBOV-GP, REBOV-GP, or SEBOV-GP were tested in mice and guinea pigs (Table 1). The main observations were that (i) the ZEBOV mouse model possesses less predictive value regarding vaccine efficacy than the guinea pig model, and (ii) EBOV-GP as a single antigen is not sufficient to induce cross-species protective immune responses in guinea pigs. The guinea pig model was appropriate for cross-protection studies because animals infected with non–rodent-adapted CIEBOV, REBOV, or SEBOV (strain Boniface) were completely protected against a lethal GPA-ZEBOV challenge (Figure 3). This is different from past nonhuman primate studies that have shown little cross-species protection [17, 18].
Further rVSV vector development was then based on the rVSV-SEBOV Boniface-GP backbone, which displayed the lowest cross-species protective potential in the guinea pig model (Table 1). SEBOV Boniface–NP, SEBOV Boniface–VP40 and SEBOV Boniface–VP24 were chosen as additional antigens in the vaccine (Figure 1A) because they have been shown to be immunogenic [28–34], and are most abundantly present in viral particles [25]. Analysis of several antigen combinations for cross-species protective immunity in the ZEBOV guinea pig model (Table 2) demonstrated that for a single-dose immunization strategy with rVSV vectors at least three EBOV immunogens need to be present, including GP and VP40. The expression level of the second antigen in the rVSV vectors was lower than that for GP (data not shown), presumably because it was encoded further downstream in the rVSV genome (Figure 1A) [35]. Notably, VP40 expression resulted in the release of EBOV-like particles into the supernatant of rVSV-S-GP/VP40 or rVSVwt/S-VP40-infected cells (Figure 1C). It has been estimated that >3500 VP40 molecules are required to form an EBOV particle [25], which explains the low number of eVLPs found in supernatants of rVSV-infected cells (Figure 1C), which mainly released rVSV particles. For future studies, VP40 will be moved further upstream in the rVSV genome to increase expression and facilitate enhanced eVLP formation. Such eVLPs are immunogenic and have been studied as a possible vaccine candidate [29, 36, 37]. Thus the rVSV vaccine encoding GP/VP40 and leading to release of rVSV particles as well as eVLPs from infected cells appears to be very potent, combining the features of 2 vaccine approaches and 2 immunogens.
Interestingly, although EBOV-NP has shown potent immunogenic properties in other vaccine platforms, such as VLPs [29] or adenoviral vectors [28, 32, 34, 38], in the presented rVSV studies its expression slightly decreased vaccine efficacy (Figure 4) with rVSVwt/S-NP–immunized guinea pigs starting to succumb to GPA-ZEBOV infection sooner than control vaccinated animals (Table 2). Sullivan and colleagues made a similar observation in nonhuman primates, where the inclusion of ZEBOV-NP in the adenovirus-based vaccine diminished survival [33]. Furthermore, ZEBOV-NP as the single antigen in the background of the VEEV RP vaccine platform was not protective in homologous challenge studies in nonhuman primates [31], suggesting that NP’s immunogenicity is not sufficient to elicit a strong protective immune response.
As expected, IgG levels specific for both immunogens were increased after administering 2 vaccine doses (Figure 5A) and seem to contribute to the increased survival rate (33%–83%) (Table 2, Figure 4). Although without passive serum transfer experiments and the analysis of T-cell responses the importance of antigen specific IgGs for protection remains unconfirmed.
In summary, we have provided evidence that cross-species protection between at least the 2 most clinically significant African EBOV species, ZEBOV and SEBOV, can be achieved in the ZEBOV guinea pig model using a 2-dose immunization strategy with a single rVSV vector expressing SEBOV-VP40 and SEBOV-GP. Future studies will determine if a combination of immunogens from different EBOV species, as well as an increased expression level of the respective antigens, will enhance cross-species protective immunity.
Funding
This work was supported by the Intramural Research Program of the National Institutes of Health (NIH), the Public Health Agency of Canada and the Department of Health and Human Services (grant U01 AI082197 to Thomas W. Geisbert). A. M. and A. G. were funded by the Natural Science and Engineering Council of Canada (NSERC).
Acknowledgments
We are grateful to Ayato Takada (Hokkaido University, Japan) for providing plasmids and antibodies for EBOV-GP and EBOV-NP. We thank Yoshihiro Kawaoka (University of Wisconsin, Madison) for providing antibodies for ZEBOV-VP24 and ZEBOV-VP40. Doug Brining, Rachel LaCasse, Kathleen Meuchel, Sandra Skorupa, Emmie de Wit, Jessica Levine, and Barry Rockx helped with animal work at the Rocky Mountain Laboratories (RML), Division of Intramural Research (DIR), National Institute of Allergy and Infectious Diseases (NIAID), National Institute of Health (NIH), Hamilton, MT. Friederike Feldmann, Shane Jones, Jim Strong, and Jason Gren helped with the mouse and guinea pig work at the National Microbiology Laboratory, Public Health Agency of Canada in Winnipeg, Canada. We thank John Rose (Yale University) for kindly providing us with the VSV reverse-genetics system. The authors show gratitude to Vinod Nair, RML, DIR, NIAID, NIH, Hamilton, MT, for electron microscopy.
Opinions, interpretations, conclusions, and recommendations are those of the authors and are not necessarily endorsed by the NIH or PHAC.
References
- 1.Sanchez A, Geisbert TW, Feldmann H. Filoviridae: Marburg and Ebola viruses. In: Knipe DM, Howley PM, editors. Fields virology. Philadelphia, PA: Lippincott Williams & Wilkins; 2006. pp. 1409–48. [Google Scholar]
- 2.Towner JS, Sealy TK, Khristova ML, et al. Newly discovered Ebola virus associated with hemorrhagic fever outbreak in Uganda. PLoS Pathog. 2008;4:e1000212. doi: 10.1371/journal.ppat.1000212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Le Guenno B, Formenty P, Wyers M, Gounon P, Walker F, Boesch C. Isolation and partial characterisation of a new strain of Ebola virus. Lancet. 1995;345:1271–4. doi: 10.1016/s0140-6736(95)90925-7. [DOI] [PubMed] [Google Scholar]
- 4.Geisbert TW, Jahrling PB, Hanes MA, Zack PM. Association of Ebola-related Reston virus particles and antigen with tissue lesions of monkeys imported to the United States. J Comp Pathol. 1992;106:137–52. doi: 10.1016/0021-9975(92)90043-t. [DOI] [PubMed] [Google Scholar]
- 5.Rollin PE, Williams RJ, Bressler DS, et al. Ebola (subtype Reston) virus among quarantined nonhuman primates recently imported from the Philippines to the United States. J Infect Dis. 1999;179:S108–14. doi: 10.1086/514303. [DOI] [PubMed] [Google Scholar]
- 6.Geisbert TW, Bausch DG, Feldmann H. Prospects for immunisation against Marburg and Ebola viruses. Rev Med Virol. 2010;20:344–57. doi: 10.1002/rmv.661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Falzarano D, Geisbert TW, Feldmann H. Progress in filovirus vaccine development: Evaluating the potential for clinical use. Expert Rev Vaccines. 2011;10:63–77. doi: 10.1586/erv.10.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sullivan NJ, Martin JE, Graham BS, Nabel GJ. Correlates of protective immunity for Ebola vaccines: Implications for regulatory approval by the animal rule. Nat Rev Microbiol. 2009;7:393–400. doi: 10.1038/nrmicro2129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schnell MJ, Buonocore L, Kretzschmar E, Johnson E, Rose JK. Foreign glycoproteins expressed from recombinant vesicular stomatitis viruses are incorporated efficiently into virus particles. Proc Natl Acad Sci U S A. 1996;93:11359–65. doi: 10.1073/pnas.93.21.11359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garbutt M, Liebscher R, Wahl-Jensen V, et al. Properties of replication-competent vesicular stomatitis virus vectors expressing glycoproteins of filoviruses and arenaviruses. J Virol. 2004;78:5458–65. doi: 10.1128/JVI.78.10.5458-5465.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bente D, Gren J, Strong JE, Feldmann H. Disease modeling for Ebola and Marburg viruses. Dis Model Mech. 2009;2:12–7. doi: 10.1242/dmm.000471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Geisbert TW, Daddario-Dicaprio KM, Lewis MG, et al. Vesicular stomatitis virus-based Ebola vaccine is well-tolerated and protects immunocompromised nonhuman primates. PLoS Pathog. 2008;4:e1000225. doi: 10.1371/journal.ppat.1000225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Feldmann H, Jones SM, Daddario-DiCaprio KM, et al. Effective post-exposure treatment of Ebola infection. PLoS Pathog. 2007;3:e2. doi: 10.1371/journal.ppat.0030002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Geisbert TW, Hensley LE, Geisbert JB, et al. Postexposure treatment of Marburg virus infection. Emerg Infect Dis. 2010;16:1119–22. doi: 10.3201/eid1607.100159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Geisbert TW, Daddario-DiCaprio KM, Williams KJ, et al. Recombinant vesicular stomatitis virus vector mediates postexposure protection against Sudan Ebola hemorrhagic fever in nonhuman primates. J Virol. 2008;82:5664–8. doi: 10.1128/JVI.00456-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tuffs A. Experimental vaccine may have saved Hamburg scientist from Ebola fever. BMJ. 2009;338:b1223. doi: 10.1136/bmj.b1223. [DOI] [PubMed] [Google Scholar]
- 17.Geisbert TW, Geisbert JB, Leung A, et al. Single-injection vaccine protects nonhuman primates against infection with Marburg virus and three species of Ebola virus. J Virol. 2009;83:7296–304. doi: 10.1128/JVI.00561-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jones SM, Feldmann H, Stroher U, et al. Live attenuated recombinant vaccine protects nonhuman primates against Ebola and Marburg viruses. Nat Med. 2005;11:786–90. doi: 10.1038/nm1258. [DOI] [PubMed] [Google Scholar]
- 19.Hensley LE, Mulangu S, Asiedu C, et al. Demonstration of cross-protective vaccine immunity against an emerging pathogenic Ebolavirus species. PLoS Pathog. 2010;6:e1000904. doi: 10.1371/journal.ppat.1000904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Connolly BM, Steele KE, Davis KJ, et al. Pathogenesis of experimental Ebola virus infection in guinea pigs. J Infect Dis. 1999;179:S203–17. doi: 10.1086/514305. [DOI] [PubMed] [Google Scholar]
- 21.Bray M, Davis K, Geisbert T, Schmaljohn C, Huggins J. A mouse model for evaluation of prophylaxis and therapy of Ebola hemorrhagic fever. J Infect Dis. 1999;179:S248–58. doi: 10.1086/514292. [DOI] [PubMed] [Google Scholar]
- 22.Ebihara H, Theriault S, Neumann G, et al. In vitro and in vivo characterization of recombinant Ebola viruses expressing enhanced green fluorescent protein. J Infect Dis. 2007;196:S313–22. doi: 10.1086/520590. [DOI] [PubMed] [Google Scholar]
- 23.Nakayama E, Yokoyama A, Miyamoto H, et al. Enzyme-linked immunosorbent assay for the detection of filovirus species-specific antibodies. Clin Vaccine Immunol. 2010;17:1723–8. doi: 10.1128/CVI.00170-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ebihara H, Takada A, Kobasa D, et al. Molecular determinants of Ebola virus virulence in mice. PLoS Pathog. 2006;2(7):e73. doi: 10.1371/journal.ppat.0020073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kuhn J. Filoviruses: A compendium of 40 years of epidemiological, clinical, and laboratory studies. In: Calisher C, editor. Vienna: SpringerWienNewYork; 2008. [PubMed] [Google Scholar]
- 26.Bray M. The role of the Type I interferon response in the resistance of mice to filovirus infection. J Gen Virol. 2001;82:1365–73. doi: 10.1099/0022-1317-82-6-1365. [DOI] [PubMed] [Google Scholar]
- 27.Bowen ET, Platt GS, Lloyd G, Raymond RT, Simpson DI. A comparative study of strains of Ebola virus isolated from southern Sudan and northern Zaire in 1976. J Med Virol. 1980;6:129–38. doi: 10.1002/jmv.1890060205. [DOI] [PubMed] [Google Scholar]
- 28.Swenson DL, Wang D, Luo M, et al. Vaccine to confer to nonhuman primates complete protection against multistrain Ebola and Marburg virus infections. Clin Vaccine Immunol. 2008;15:460–7. doi: 10.1128/CVI.00431-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Warfield KL, Swenson DL, Olinger GG, Kalina WV, Aman MJ, Bavari S. Ebola virus-like particle-based vaccine protects nonhuman primates against lethal Ebola virus challenge. J Infect Dis. 2007;196:S430–7. doi: 10.1086/520583. [DOI] [PubMed] [Google Scholar]
- 30.Bukreyev A, Rollin PE, Tate MK, et al. Successful topical respiratory tract immunization of primates against Ebola virus. J Virol. 2007;81:6379–88. doi: 10.1128/JVI.00105-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Geisbert TW, Pushko P, Anderson K, Smith J, Davis KJ, Jahrling PB. Evaluation in nonhuman primates of vaccines against Ebola virus. Emerg Infect Dis. 2002;8:503–7. doi: 10.3201/eid0805.010284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sullivan NJ, Geisbert TW, Geisbert JB, et al. Accelerated vaccination for Ebola virus haemorrhagic fever in non-human primates. Nature. 2003;424:681–4. doi: 10.1038/nature01876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sullivan NJ, Geisbert TW, Geisbert JB, et al. Immune protection of nonhuman primates against Ebola virus with single low-dose adenovirus vectors encoding modified GPs. PLoS Med. 2006;3:e177. doi: 10.1371/journal.pmed.0030177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pratt WD, Wang D, Nichols DK, et al. Protection of nonhuman primates against two species of Ebola virus infection with a single complex adenovirus vector. Clin Vaccine Immunol. 2010;17:572–81. doi: 10.1128/CVI.00467-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lichty BD, Power AT, Stojdl DF, Bell JC. Vesicular stomatitis virus: Re-inventing the bullet. Trends Mol Med. 2004;10:210–6. doi: 10.1016/j.molmed.2004.03.003. [DOI] [PubMed] [Google Scholar]
- 36.Warfield KL, Bosio CM, Welcher BC, et al. Ebola virus-like particles protect from lethal Ebola virus infection. Proc Natl Acad Sci U S A. 2003;100:15889–94. doi: 10.1073/pnas.2237038100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Swenson DL, Warfield KL, Negley DL, Schmaljohn A, Aman MJ, Bavari S. Virus-like particles exhibit potential as a pan-filovirus vaccine for both Ebola and Marburg viral infections. Vaccine. 2005;23:3033–42. doi: 10.1016/j.vaccine.2004.11.070. [DOI] [PubMed] [Google Scholar]
- 38.Sullivan NJ, Sanchez A, Rollin PE, Yang ZY, Nabel GJ. Development of a preventive vaccine for Ebola virus infection in primates. Nature. 2000;408:605–9. doi: 10.1038/35046108. [DOI] [PubMed] [Google Scholar]