Abstract
Background
There are limited data on substance use in South Africa. We describe patterns of substance use based on recent, nationally representative data.
Methods
Data were derived from the 2002 – 2004 South African Stress and Health (SASH) study. A nationally representative household probability sample of 4 351 adults was interviewed using the paper and pencil version of the World Health Organization Composite International Diagnostic Interview (CIDI). Data are reported for lifetime use, socio-demographic correlates of use, and age of cohort predicting lifetime use for four classes of drugs.
Results
The estimate for cumulative occurrence of alcohol use was 38.7%, of tobacco smoking 30.0%, of cannabis use 8.4%, of other drug use 2.0%, and of extra-medical psychoactive drug use 19.3%. There were statistically significant associations between male gender and alcohol, tobacco, cannabis and other drug use. Coloureds and whites were more likely than blacks to have used alcohol, tobacco and other drugs. Clear cohort variations existed in the age of initiation of drug use; these were most marked for other drugs and for extra-medical drug use. Use of all drug types was much more common in recent cohorts, with a similar cumulative incidence of tobacco, alcohol and cannabis use across age cohorts.
Conclusions
Epidemiological patterns of use for alcohol, tobacco, cannabis, other drugs and extra-medical drugs provide the first nationally representative data. New findings on race and exploratory data on time trends provide a foundation for future epidemiological work on drug use patterns across birth cohorts and population subgroups in South Africa.
During the apartheid years South Africa was relatively isolated from the rest of the world and substance use primarily revolved around locally produced substances, notably alcohol, tobacco and cannabis. During the 1990s and early 2000s South Africa went through major social and political transformation. During this period links and trade with the rest of the world opened. Law authorities, social services and service providers agree that substance-related problems have increased dramatically over the past 10 years. These include road traffic accidents, mental illness and, most worrying, violence and severe crime committed under the influence of substances.
Historically substance abuse data in South Africa have been limited. Until the late 1990s information came mostly from ad hoc cross-sectional studies, often conducted in a single location, and from information on police arrests and drug seizures, mortuaries and school surveys. This has since been supplemented by national surveys.1 Recently, several more reliable systems have been initiated, most notably the South African Community Epidemiology Network on Drug Use (SACENDU) project, which meets biannually to present and discuss information about substance abuse patterns.1 Alcohol is by far the major substance of abuse, while cannabis is still the most common illicit drug used, especially among youths attending treatment centres. Cape Town continues to experience a dramatic increase in the use of crystal methamphetamine (known as Tik), which has become the primary substance of abuse. Substance misuse is most prevalent among males, with trends suggesting roughly an 80/20% male/female split across the country. Whites appear to be the highest users of substances, followed by blacks, coloureds and Indians in Gauteng and Mpumalanga, while coloureds are the highest users, relative to other race groups, in Port Elizabeth and Cape Town. Black substance abusers far outnumber any other group in the East London area.2
Although systems such as SACENDU provide valuable information on substance abuse trends, there have been no systematic data available that are fully representative of the diverse South African population.
This paper aims to present: (i) cumulative incidence proportions of alcohol, tobacco, cannabis, other drugs (lysergic acid diethylamide (LSD), cocaine, heroin, opium, glue, any other drugs) and any extra-medical drug use for the population as a whole; and (ii) cumulative incidence proportions for major population subgroups, defined with reference to (a) year of birth, (b) gender, (c) race/ethnicity, and (d) the following characteristics (which may vary across time) as measured at the time of assessment: educational attainment, marital status, employment status, household income, assets owned by household, and location of residence (rural or urban).
Methods
Data were derived from the 2002 – 2004 South African Stress and Health (SASH) study. Briefly, SASH was an epidemiological survey of mental illness, and part of the World Health Organization (WHO)’s World Mental Health (WMH) 2000 initiative which sought to obtain population-based data on the prevalence and severity of psychiatric disorders, their demographic and psychosocial correlates, and the level of adequacy of mental health service utilisation.3
Study population
A sample of 4 351 adults aged 18 and older, drawn from a nationally representative, household probability sample, were interviewed. Households and hostel quarters were included. Sampled residences were stratified into 10 diverse household categories, including rural-commercial, agricultural, rural traditional subsistence areas, black townships, informal urban or peri-urban shack areas, coloured townships, Indian townships, general metropolitan residential areas, general large metropolitan residential areas and urban domestic servant accommodation. Within each of these strata, 600 households were listed from maps, census data or aerial photographs. A probability sample of households was selected and screened to determine eligibility. A singe adult respondent from each selected dwelling was drawn randomly using the Kish method.
Survey instrument
Fieldwork in SASH utilised the paper and pencil version of the WHO Composite International Diagnostic Interview Version 3.0 (WMH-CIDI 3.0). The CIDI is a fully structured interview used by trained lay interviewers and can generate diagnoses according to the ICD-10 (International Statistical Classification of Diseases and Related Health Problems, 10th revision) and DSM-IV (Diagnostic and Statistical Manual of Mental Disorders, 4th edition) diagnostic systems. The translation of the English version of the CIDI into six other South African languages (Afrikaans, Zulu, Xhosa, Northern Sotho, Southern Sotho and Tswana) used in the SASH study was carried out according to WHO recommendations of iterative back-translation procedures conducted by panels of bilingual and multilingual experts. Discrepancies found in the back-translation were resolved by an expert consensus panel.
Measures
Drug use
‘Extra-medical’ drug taking encompasses alcohol, tobacco and illegal drug use and the use of psychoactive prescription or over-the-counter (OTC) drug compounds, when used ‘to get high’ or for other reasons beyond the boundaries approved for legitimate prescribing and dispensing.4 Our primary response variable of interest is the cumulative occurrence of drug use, as observed through, and up to, the age of respondents born between 1927 and 1984 at the time of assessment. Evaluated in cross-section, this is a cumulative incidence proportion among cohort members who have survived to the age of assessment – i.e. the cumulative incidence proportion among survivors (CIPAS).5 These parameters were estimated for: (i) alcohol; (ii) tobacco; (iii) cannabis; (iv) other drugs; and (v) any extra-medical drug use (excluding tobacco and alcohol).
Alcohol use was defined as ever had a drink, and age of onset as the age at which the respondent had his or her first drink, and the age at which he or she started drinking at least 12 drinks a year. The response rate to the question of age of first drink was very low, with answers missing or refused for 62%. The combined number of respondents for the above questions was used to determine the prevalence of alcohol use.
Tobacco users were defined as those reporting smoking more than 100 cigarettes in their lifetime. Onset of use was defined as the age at which a respondent started smoking.
Cannabis use was defined as having ever used cannabis and its onset as at what age use commenced. Extra-medical drug use comprised the use of sedatives or tranquillisers, stimulants, analgesics or any other psychoactive over-the-counter compound. The age of onset was defined as the age at which the first of these drugs was used.
The category ‘other drugs’ included cocaine, LSD, heroin, opium, glue, or any other drug ever used during the respondent’s lifetime. Age of onset of use was defined as the age of first use.
Covariates
Covariates include three time-fixed variables: sex, race/ethnicity (black, white, coloured and Indian/Asian), and birth cohort. The birth cohorts were 1975 – 1986 (18 – 29 years at time of assessment), 1965 – 1974 (30 – 39 years), 1955 – 1964 (40 – 49 years), and 1912 – 1954 (≥50 years).
Time-varying covariates were studied, including: (i) completed level of education (grouped as none, Grades 1 – 7, Grades 8 – 11, Matric and Matric+ levels); (ii) marital status (married, previously married or not married); (iii) employment (employed or unemployed); and (iv) family income (zero, low, low average, high average and high). Similar to other WMH countries, our measure of income was calculated by dividing household income by the number of household members and defining four income categories. The two lowest quartiles of per capita income were called low income and low-average income. High average income was defined as income between one and two times the median per capita income and high income was defined as more than twice the median; (v) residence in an urban or rural area; (vi) asset index (we used an asset index based on 17 items reflecting individual and household wealth. This was based on household ownership of material goods (refrigerator/freezer, vacuum/floor cleaner, television, video cassette recorder, radio, microwave, and washing machine), ownership or use of other household resources (telephone, running water in the home, kitchen sink, flush toilet, automobile, domestic servant, and stove/hotplate) and financial activities participants engaged in (shopping at a supermarket, using financial services such as a bank account or credit card, and having an account at a retail store). This index has been shown to have excellent reliability (Cronbach’s alpha, 0.92). These measures of asset ownership were used to construct an aggregate asset score, which was categorised into categories for low, medium and high assets.6
Analysis methods
To account for the stratified multi-stage sample design, the data were weighted to adjust for differential probability of selection within households as a function of household size and clustering of the data, and for differential non-response. A post-stratification weight was also used to make the sample distribution comparable to the population distribution in the 2001 South African census for age, sex, and province. The weighting and geographical clustering of the data were taken into account by using the Taylor series linearisation method in the SUDAAN statistical package (Research Triangle Institute, Research Triangle Park, NC, USA). Logistic regression analysis was used to study socio-demographic correlates. Logistic regression coefficients and their design-corrected standard errors (SEs) were exponentiated and are reported here as odds ratios (ORs) and 95% confidence intervals (CIs). Statistical significance was consistently evaluated using 0.05 level two-sided tests.
Results
Sample characteristics
Table I presents frequency distributions for covariates and response variables. Unweighted sample sizes are followed by (weighted) estimated proportions and Taylor series linearisation derived SEs for the proportions. Aside from the unweighted sample frequencies, all results are based on conventional analytical methods for complex survey data.
Table I.
Description and summary of sample
| Unweighted (% (N)) | Weighted (%) | SE (%) | |
|---|---|---|---|
| Birth cohort | |||
| 1975 – 1986 (18 – 29 yrs) | 37.7 (1 640) | 39.1 | 1.0 |
| 1965 – 1974 (30 – 39 yrs) | 24.5 (1 066) | 22.1 | 0.8 |
| 1955 – 1964 (40 – 49 yrs) | 17.7 (768) | 18.1 | 0.8 |
| 1912 – 1954 (≥50 yrs) | 20.2 (877) | 20.7 | 0.7 |
| Gender | |||
| Male | 39.8 (1 733) | 46.3 | 1.0 |
| Female | 60.2 (2 618) | 53.7 | 1.0 |
| Race | |||
| Black | 76.2 (3 317) | 76.2 | 0.2 |
| White | 12.9 (563) | 10.4 | 0.9 |
| Coloured | 7.2 (311) | 10.0 | 0.1 |
| Indian/Asian | 3.7 (160) | 3.4 | 0.4 |
| Education | |||
| None | 7.7 (326) | 6.8 | 0.5 |
| Grade 1 – 7 | 20.9 (886) | 19.1 | 0.9 |
| Grade 8 – 11 | 34.7 (1 471) | 35.4 | 1.0 |
| Matric | 22.2 (939) | 23.5 | 0.9 |
| Matric+ | 14.6 (618) | 15.3 | 1.0 |
| Marital status | |||
| Currently married | 49.7 (2 135) | 50.6 | <0.1 |
| Previously married | 8.0 (343) | 6.5 | <0.1 |
| Never married | 42.4 (1 820) | 42.9 | <0.1 |
| Employment | |||
| Employed | 30.0 (1 306) | 31.0 | 1.3 |
| Unemployed | 70.0 (3 045) | 69.0 | 1.3 |
| Income | |||
| Zero | 14.5 (629) | 13.7 | 0.8 |
| Low | 30.5 (1 329) | 29.5 | 1.1 |
| Low average | 15.7 (683) | 15.4 | 0.8 |
| High average | 19.1 (830) | 19.6 | 1.0 |
| High | 20.2 (880) | 21.8 | 0.9 |
| Rural/urban residence | |||
| Rural | 42.2 (1 836) | 38.4 | 1.0 |
| Urban | 57.8 (2 515) | 61.6 | 1.0 |
| Asset index | |||
| Low | 41.9 (1 822) | 39.3 | 1.3 |
| Medium | 37.3 (1 623) | 37.4 | 1.2 |
| High | 20.8 (906) | 23.3 | 1.3 |
| Drug use | |||
| Alcohol | 35.2 (1 532) | 38.7 | 1.2 |
| Tobacco | 26.9 (1 169) | 30.0 | 1.1 |
| Cannabis | 6.6 (288) | 8.4 | 0.6 |
| Other drugs (cocaine, etc.) | 1.4 (59) | 2.0 | 0.4 |
| Any extra-medical drug use | 19.6 (807) | 19.3 | 1.5 |
The SE of a method of measurement or estimation is the estimated SD of the error in that method. Namely, it is the SD of the difference between the measured or estimated values and the true values. Notice that the true value is, by definition, unknown and this implies that the SE of an estimate is itself an estimated value.
More than half the sample was female, only 23.5% had completed high school, half was married and more than 60% lived in an urban setting. Slightly more than three-quarters was black, 69% were unemployed and 13.7% had no income at all. Use of alcohol was most common (38.7%), followed by tobacco (30%), extra-medical drugs (19.3%), cannabis (8.4%) and lastly other drugs (2%).
Cumulative occurrence of drug use across birth cohorts
Table II shows the estimated cumulative incidence proportions and ORs of cumulative occurrence. Alcohol was used by the majority of participants with the proportions using alcohol similar among younger birth cohorts (38.3% and 39.1%). These were slightly lower than estimates for the older 1955 – 1964 cohort (42.8%). The 1955 – 1964 birth cohort was 1.4 times more likely to report ever trying alcohol compared with the 1912 – 1954 cohort.
Table II.
Estimated cumulative occurrence of drug use by birth cohort, and estimates from discrete time survival analysis models
| Birth cohort | Alcohol
|
Tobacco
|
Cannabis
|
Other drugs (e.g. cocaine)
|
Extra-medical
|
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | SE | OR | 95% CI | % | SE | OR | 95% CI | % | SE | OR | 95% CI | % | SE | OR | 95% CI | % | SE | OR | 95% CI | |
| 1912 – 1954 | 35.3 | 2.3 | 1.0 | - | 33.7 | 2.2 | 1.0 | - | 5.9 | 1.3 | 1.0 | - | 1.0 | 0.5 | 1.0 | - | 16.6 | 2.6 | 1.0 | - |
| 1955 – 1964 | 42.8 | 2.8 | 1.4 | 1.1 – 1.7 | 33.4 | 2.9 | 1.0 | 0.8 – 1.3 | 6.9 | 1.2 | 1.2 | 0.6 – 2.2 | 1.5 | 0.7 | 1.6 | 0.6 – 3.9 | 17.1 | 1.8 | 1.0 | 0.7 – 1.6 |
| 1965 – 1974 | 39.1 | 1.8 | 1.2 | 0.9 – 1.5 | 28.6 | 1.7 | 0.8 | 0.6 – 1.0 | 8.0 | 1.3 | 1.4 | 0.8 – 2.5 | 2.9 | 0.6 | 3.1 | 1.0 – 9.9 | 21.9 | 2.2 | 1.4 | 0.9 – 2.2 |
| 1975 – 1986 | 38.3 | 1.8 | 1.1 | 0.9 – 1.4 | 27.3 | 1.3 | 0.7 | 0.6 – 1.0 | 10.6 | 1.0 | 1.9 | 1.2 – 3.0 | 2.3 | 0.6 | 2.5 | 0.8 – 8.2 | 20.3 | 1.8 | 1.3 | 0.9 – 1.8 |
| Total | 38.7 | 1.2 | 30.0 | 1.1 | 8.4 | 0.6 | 2.0 | 0.4 | 19.3 | 1.5 | ||||||||||
| p-value | 0.158 | 0.037 | 0.038 | 0.173 | 0.145 | |||||||||||||||
Estimated cumulative incidence proportions for cannabis were lowest for the oldest cohort, born 1912 – 1954 (5.9%). Larger proportions were observed in the most recent cohort, born 1975 – 1986: 10.6% of this cohort had become users by the time of the interview. The most recent cohort was 1.9 times more likely to report having tried cannabis compared with the oldest cohort (OR 1.9 compared with OR 1.0 for the 1912 – 1954 cohort, CI 1.2 – 3.0).
Although not statistically significant, the cumulative incidence proportions for other drugs, including cocaine, and extra-medical drug use were again slightly higher in the two more recent cohorts. Relatively high rates of extra-medical drug use were reported across age cohorts, ranging from a cumulative incidence of 16.6% to 20.3%.
Correlates of drug use
Table III presents estimated ORs for selected covariates (bivariate) and cumulative occurrence of drug use, and Table IV shows covariate-adjusted (multivariate) estimates of the strength of these associations. While trends showed an increase in the use of cannabis, other drugs and extra-medical drugs in younger age groups, this was only significant for cannabis use on bivariate analysis (Table III). While the same trends were observed on multivariate analysis, there were no significant associations between age and drug use (Table IV).
Table III.
Estimated strength of association between selected covariates and cumulative occurrence of drug use
| Alcohol
|
Tobacco
|
Cannabis
|
Other drugs (e.g. cocaine)
|
Extra-medical
|
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Age (yrs) | ||||||||||
| 18 – 29 | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - |
| 30 – 39 | 1.0 | 0.8 – 1.3 | 1.1 | 0.9 – 1.3 | 0.7 | 0.5 – 1.2 | 1.3 | 0.7 – 2.4 | 1.1 | 0.9 – 1.4 |
| 40 – 49 | 1.2 | 0.9 – 1.5 | 1.3 | 1.0 – 1.8 | 0.6 | 0.4 – 1.0 | 0.6 | 0.2 – 1.9 | 0.8 | 0.6 – 1.1 |
| ≥50 | 0.9 | 0.7 – 1.1 | 1.4 | 1.0 – 1.8 | 0.5 | 0.3 – 0.9 | 0.4 | 0.1 – 1.3 | 0.8 | 0.5 – 1.1 |
| Gender | ||||||||||
| Male | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - |
| Female | 0.3 | 0.2 – 0.3 | 0.2 | 0.1 – 0.2 | 0.1 | 0.1 – 0.2 | 0.2 | 0.1 – 0.5 | 1.0 | 0.8 – 1.1 |
| Race | ||||||||||
| Black | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - |
| White | 3.1 | 2.0 – 4.6 | 3.2 | 2.2 – 4.6 | 1.7 | 0.9 – 3.1 | 2.2 | 1.1 – 4.3 | 1.0 | 0.3 – 1.4 |
| Coloured | 2.6 | 1.9 – 3.5 | 3.4 | 2.8 – 4.2 | 2.7 | 1.9 – 3.8 | 3.9 | 1.6 – 9.8 | 0.7 | 0.4 – 2.3 |
| Indian/Asian | 0.9 | 0.6 – 1.4 | 1.7* | 1.1 – 2.7 | 0.6 | 0.4 – 1.1 | 0 | - | 0.6 | 0.3 – 1.1 |
| Education | ||||||||||
| None | 1.0 | - | 1.0 | - | 1.0 | - | 0 | - | 1.0 | - |
| Grade 1 – 7 | 1.0 | 0.7 – 1.4 | 0.8 | 0.6 – 1.2 | 1.1 | 0.5 – 2.3 | 1.0 | - | 1.3 | 0.8 – 2.1 |
| Grade 8 – 11 | 1.2 | 0.8 – 1.6 | 0.8 | 0.6 – 1.2 | 1.9 | 0.9 – 4.0 | 3.3 | 1.1 – 9.7 | 1.3 | 0.8 – 2.3 |
| Matric | 1.3 | 1.0 – 1.8 | 0.8 | 0.6 – 1.1 | 1.6 | 0.7 – 3.4 | 2.6 | 0.9 – 7.6 | 1.5 | 0.8 – 2.7 |
| Matric+ | 1.4 | 1.0 – 2.0 | 0.9 | 0.6 – 1.3 | 2.8 | 1.4 – 5.7 | 3.1 | 1.1 – 8.3 | 1.5 | 0.8 – 2.7 |
| Marital status | ||||||||||
| Currently married | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - |
| Previously married | 1.1 | 0.8 – 1.7 | 1.4 | 1.0 – 1.8 | 1.0 | 0.6 – 1.9 | 1.8 | 0.5 – 6.0 | 0.9 | 0.6 – 1.5 |
| Never married | 1.1 | 0.8 – 1.3 | 0.8 | 0.6 – 1.0 | 1.4 | 1.0 – 2.0 | 1.5 | 0.7 – 3.2 | 1.0 | 0.8 – 1.2 |
| Employment | ||||||||||
| Employed | 1.8 | 1.5 – 2.1 | 1.8 | 1.4 – 2.1 | 1.5 | 1.0 – 2.1 | 1.7 | 1.0 – 2.8 | 1.2 | 0.9 – 1.6 |
| Unemployed | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - |
| Income | ||||||||||
| None | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - |
| Low | 1.1 | 0.8 – 1.5 | 1.0 | 0.8 – 1.3 | 0.8 | 0.5 – 1.4 | 0.9 | 0.2 – 3.4 | 1.2 | 0.8 – 1.7 |
| Low average | 1.5 | 1.1 – 1.9 | 1.3 | 1.0 – 1.8 | 0.8 | 0.5 – 1.4 | 0.7 | 0.2 – 2.8 | 1.0 | 0.7 – 1.4 |
| High average | 1.4 | 1.0 – 1.9 | 1.3 | 1.0 – 1.8 | 1.3 | 0.8 – 2.1 | 0.7 | 0.2 – 1.8 | 1.1 | 0.7 – 1.6 |
| High | 1.2 | 0.9 – 1.6 | 1.3 | 1.0 – 1.7 | 1.3 | 0.9 – 2.1 | 0.3 | 0.1 – 1.9 | 1.1 | 0.8 – 1.6 |
| Urban/rural residence | ||||||||||
| Rural | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - |
| Urban | 1.5 | 1.3 – 1.9 | 1.3 | 1.1 – 1.7 | 2.2 | 1.7 – 2.9 | 2.5 | 1.2 – 5.0 | 1.3 | 0.9 – 1.7 |
| Asset index | ||||||||||
| Low | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - |
| Average | 1.6 | 1.4 – 1.8 | 1.2 | 1.0 – 1.5 | 1.7 | 1.2 – 2.6 | 1.4 | 0.8 – 2.6 | 1.4 | 1.0 – 1.8 |
| High | 2.2 | 1.7 – 2.8 | 1.8 | 1.4 – 2.4 | 2.0 | 1.3 – 3.3 | 1.7 | 0.6 – 4.7 | 1.1 | 0.7 – 1.7 |
p<0.05.
Table IV.
Covariate-adjusted estimates of strength of association between selected covariates and cumulative occurrence of drug use
| Alcohol
|
Tobacco
|
Cannabis
|
Other drugs (e.g. cocaine)
|
Extra-medical
|
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Age (yrs) | ||||||||||
| 18 – 29 | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - |
| 30 – 39 | 1.0 | 0.8 – 1.3 | 1.0 | 0.8 – 1.2 | 0.7 | 0.4 – 1.2 | 1.2 | 0.6 – 2.6 | 1.0 | 0.7 – 1.4 |
| 40 – 49 | 1.1 | 0.9 – 1.4 | 1.0 | 0.7 – 1.4 | 0.6 | 0.3 – 1.0 | 0.6 | 0.2 – 1.8 | 0.7 | 0.5 – 1.0 |
| ≥50 | 0.8 | 0.6 – 1.0 | 0.9 | 0.7 – 1.2 | 0.5 | 0.3 – 1.0 | 0.4 | 0.1 – 1.2 | 0.7 | 0.5 – 1.1 |
| Gender | ||||||||||
| Male | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - |
| Female | 0.2 | 0.2 – 0.3 | 0.1 | 0.1 – 0.1 | 0.1 | 0.1 – 0.2 | 0.2 | 0.1 – 0.5 | 1.0 | 0.8 – 1.2 |
| Race | ||||||||||
| Black | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - |
| White | 2.8 | 1.9 – 4.1 | 5.1 | 3.7 – 7.2 | 2.8 | 1.9 – 3.9 | 2.9 | 1.2 – 7.1 | 0.7 | 0.3 – 1.4 |
| Coloured | 3.9 | 2.0 – 7.5 | 5.3 | 3.0 – 9.5 | 1.5 | 0.7 – 3.2 | 8.4 | 2.6 – 26.7 | 0.9 | 0.4 – 2.2 |
| Indian/Asian | 1.0 | 0.6 – 1.8 | 2.7 | 1.6 – 4.5 | 0.6 | 0.3 – 1.2 | - | - | 0.5 | 0.3 – 1.0 |
| Education | ||||||||||
| None | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - |
| Grade 1 – 7 | 0.9 | 0.7 – 1.3 | 0.8 | 0.6 – 1.2 | 1.0 | 0.5 – 2.2 | - | - | 1.1 | 0.7 – 1.9 |
| Grade 8 – 11 | 0.8 | 0.6 – 1.2 | 0.7 | 0.5 – 1.0 | 1.3 | 0.6 – 3.0 | 2.5 | 0.9 – 6.7 | 1.1 | 0.7 – 1.9 |
| Matric | 0.8 | 0.5 – 1.0 | 0.5 | 0.3 – 0.9 | 0.9 | 0.4 – 2.0 | 1.9 | 0.6 – 6.1 | 1.2 | 0.7 – 2.1 |
| Matric+ | 0.6 | 0.4 – 0.9 | 0.4 | 0.3 – 0.8 | 1.5 | 0.7 – 3.6 | 2.3 | 0.7 – 7.5 | 1.2 | 0.6 – 2.3 |
| Marital status | ||||||||||
| Currently married | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - |
| Previously married | 1.5 | 1.0 – 2.1 | 2.1 | 1.5 – 2.9 | 1.7 | 0.8 – 3.4 | 3.2 | 0.9 – 13.0 | 1.0 | 0.6 – 1.7 |
| Never married | 1.1 | 0.9 – 1.4 | 0.8 | 0.6 – 1.0 | 1.0 | 0.7 – 1.6 | 1.1 | 0.6 – 2.1 | 0.8 | 0.6 – 1.1 |
| Employment | ||||||||||
| Unemployed | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - |
| Employed | 1.3 | 1.0 – 1.5 | 1.2 | 1.0 – 1.4 | 1.1 | 0.8 – 1.6 | 1.3 | 0.5 – 3.2 | 1.1 | 0.9 – 1.5 |
| Income | ||||||||||
| None | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - |
| Low | 1.0 | 0.7 – 1.5 | 1.1 | 0.8 – 1.4 | 0.8 | 0.5 – 1.3 | 1.0 | 0.3 – 2.9 | 1.2 | 0.8 – 1.7 |
| Low average | 1.2 | 0.9 – 1.6 | 1.2 | 0.9 – 1.6 | 0.6 | 0.4 – 1.1 | 0.5 | 0.2 – 1.7 | 1.0 | 0.7 – 1.4 |
| High average | 1.0 | 0.7 – 1.4 | 1.2 | 0.9 – 1.6 | 1.0 | 0.6 – 1.7 | 0.5 | 0.2 – 1.2 | 1.1 | 0.7 – 1.6 |
| High | 0.9 | 0.7 – 1.3 | 1.1 | 0.8 – 1.6 | 1.1 | 0.7 – 1.6 | 0.2* | 0.1 – 0.9 | 1.1 | 0.7 – 1.7 |
| Urban/rural residence | ||||||||||
| Rural | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - |
| Urban | 1.1 | 0.9 – 1.4 | 1.0 | 0.8 – 1.2 | 1.7 | 1.3 – 2.3 | 2.0 | 1.0 – 4.0 | 1.3 | 0.9 – 1.7 |
| Asset index | ||||||||||
| Low | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - | 1.0 | - |
| Average | 1.4 | 1.1 – 1.7 | 1.0 | 0.8 – 1.3 | 1.2 | 0.8 – 1.9 | 0.8 | 0.4 – 1.4 | 1.3 | 1.0 – 1.6 |
| High | 1.2 | 0.8 – 1.6 | 0.8 | 0.6 – 1.1 | 1.0 | 0.6 – 1.8 | 0.4 | 0.1 – 1.6 | 1.1 | 0.8 – 1.5 |
p<0.05.
On both bivariate and covariate estimates, gender was the most significant indicator of substance use – males were generally 8 – 9 times more likely than females to have become users of all drug types, except for extra-medical drugs.
On bivariate analysis, participants identified as black were less likely than whites and coloureds to be users of alcohol (OR 3.1 and 2.6), tobacco (OR 3.2 and 3.4) and other drugs (OR 2.2 and 3.9), and also less likely to have used tobacco than Indians/Asians (OR 1.7) (Table III). The association between race/ethnicity and alcohol use persisted, and became more robust in certain cases, on covariate-adjusted estimates. After adjustment for other demographic and socio-economic factors, coloureds were 3.9 times more likely to have tried alcohol, 5.3 times more likely to be smokers and 8.4 times more likely to have used ‘other drugs’ compared with blacks. Whites used significantly more alcohol, tobacco, cannabis and other drugs compared with blacks.
Estimated associations with educational attainment differed across drug types. Based upon estimates from the bivariate analyses, persons with post-matric education were more likely to have used cannabis (OR 2.8). Other drug use (e.g. cocaine) was more prevalent in the Grade 7 – 11 group (OR 3.3) and in the post-matric education group (OR 3.1), compared with the group with primary school education only. These crude associations did not persist in multivariate models.
On bivariate analysis, those who were employed were more likely to have tried all classes of drugs compared with the unemployed (Table III). This was only significant for alcohol and tobacco use. After adjustment the employed were still more likely to have tried alcohol and be smokers, but there was no association between employment status and cannabis, ‘other drugs’, or extra-medical drug use.
On bivariate analysis only, respondents with low income used significantly more alcohol compared with those with no income. No association was found between marital status and drug use.
Strong associations were found on bivariate analysis (Table III) between urban residence and alcohol, tobacco, cannabis and other drug use, but not extra-medical drug use. Those living in urban areas were more than twice as likely to have used cannabis (OR 2.2) and other (OR 2.5) drugs. On multivariate analysis, cannabis, ‘other drugs’ and extra-medical drugs were used more in urban areas, but only cannabis use reached statistical significance.
On bivariate analysis, possessing more assets was associated with a higher prevalence of substance use. On multivariate analysis, respondents with an average number of assets showed statistically higher use of alcohol compared with those with no income.
Initiation of drug use across birth cohorts
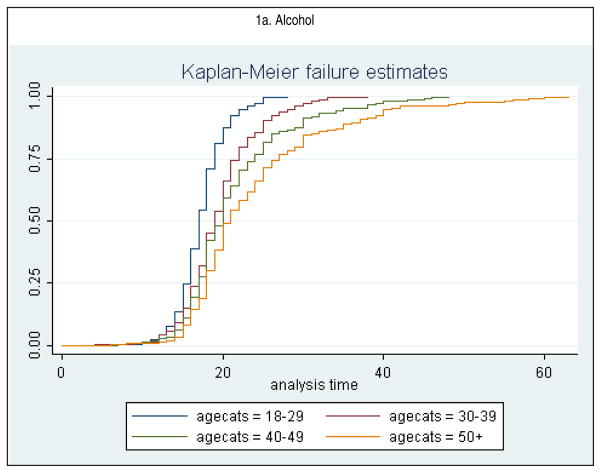
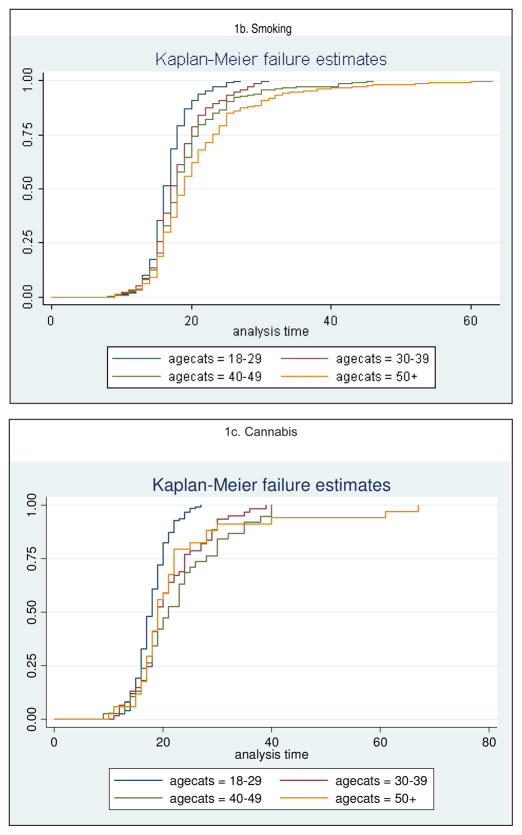
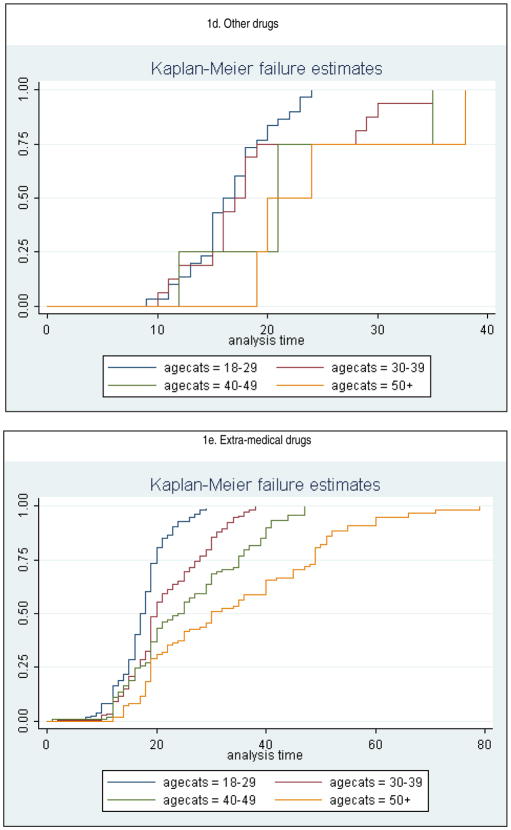
Fig. 1, a – e, presents the cumulative occurrence of drug use by age, and according to birth cohort. Of those in the youngest cohort (18 – 29 years) who had used alcohol, 89.4% had used it by the time of turning 20; in contrast, only 53.6% of the oldest cohort (≥50) who used alcohol had done so by age 20. Both tobacco smoking and cannabis use show similar trends, where at age 20 more than 80% of the youngest cohort (18 – 29 years) had used these two drugs compared with just over 50% of the oldest cohort (≥50).
Fig. 1.
Estimated age-specific cumulative occurrence of drug use by birth cohort.
More pronounced cohort-associated variations were found when cumulative proportions of those who had used other drugs (stimulants, cocaine, etc.) by the age of 17 years were examined. In both the two younger cohorts, of those who used this group of drugs, more than 60% had already used them by age 17, whereas no one had used them by age 17 in the oldest cohort (≥50 years) and only 25% had used them by age 17 in the second-oldest cohort (40 – 49 years). In the youngest cohort (18 – 29 years), 66% of those who used extra-medical drugs had used them by age 18, compared with only 20% in the oldest cohort.
Discussion
These findings are in keeping with countrywide estimates of alcohol, tobacco and cannabis use. Alcohol remains the substance most often used by South Africans (38.7%), which is consistently lower than prior data from less representative reports and surveys.1,2 The prevalence of tobacco use (30.0%) is consistent with data on lifetime tobacco use in South Africa (27% in 2007 and 37.6% for South African high-school students in 2002).8 The rate of cannabis use (8.3%) is also in keeping with prior data on annual prevalence from the World Drug Report (8.4%).9 At 2% the use of other drugs, including methamphetamine, might be an underestimation of drug use trends in South Africa. During 2005, after this survey was conducted, methamphetamine was documented as the primary drug of abuse in the Western Cape, replacing alcohol and overtaking cannabis.2
Limitations of this study deserve mention. First, a cross-sectional survey does not include drug-related deaths, i.e. persons who have died secondary to substance use were not included.5 However, it is improbable that drug-related mortality could explain these differences. For cannabis, there is no proven increased mortality risk and in this study there were large differences in the cumulative occurrence of use by age 15 years between adjacent cohorts (see, for example, the ‘other drugs’ estimates for the two oldest birth cohorts). Even if those who began use early had substantially increased mortality rates, this increased mortality would be unlikely to account for cumulative incidence proportions of cannabis use by age 20 years (around 15% lower in the oldest cohort compared with the youngest cohort). In addition, tobacco-associated mortality should have been especially high; however, this was the drug with the smallest cohort-associated variations.
Second, the report of first use of drugs might be ‘right censored’:10 because younger birth cohorts have not yet reached an older age, their reported drug use necessarily occurs at a younger age. However, such a bias is not relevant for estimates of the cumulative incidence proportion for ages through which all cohorts have passed, since comparisons are made across cohorts for a given age in the lifespan (e.g. age 15 years).
A third possible bias is that older respondents may have struggled to remember events long ago.5 However, this cannot account for all the differences in age of onset observed here, since the cumulative incidence of alcohol use was lower for the two more recent cohorts (1965 – 1974 and 1975 – 1986) than it was for the next older one (1955 – 1964). It is therefore unlikely that response or other biases completely account for the trends observed here. Similar birth cohort trends in the age of initiation of illegal drug use have been observed in surveys in the USA11 and Australia,12 some of which used data collected across time rather than relying solely on retrospective reports. The trends are also consistent with data concerning illegal drug markets in South Africa. There is good evidence that drug availability and drug use in the general population co-vary. For example, since the first democratic elections in South Africa in 1994 there has been an increase in the trafficking and use of heroin, cocaine, and amphetamine-type stimulants in the country. The trends found by the SACENDU project are largely replicated in this study.
A fourth limitation might be that drug availability simply changes patterns of use in a given population. Since there is no simple relationship between drug availability and drug use in a population, drug availability cannot be the sole cause for changes in the cumulative incidence of drug use.5 There have been many changes in South Africa in the past 14 years. The country has gone through major political, economic and cultural changes. There has been an influx of foreign people, trade and culture into and through South Africa with transitions in several provinces from a predominantly rural-cultural society into an urban westernised society, all of which could play a role in the trends described here. Finally, these data do not capture the dramatic increase in the use of methamphetamine and other drugs. Since 2004, methamphetamine has become the primary drug of abuse in the Western Cape.2 The use of heroin has steadily increased and so has the use of methcathinone (CAT). It is therefore vital to replicate the present survey.
Despite these limitations, the following findings are notable. Males as well as whites and coloureds had a considerably higher prevalence of substance use compared with females and blacks and Indians. Compared with blacks, coloureds were 8.4 times more likely to have used ‘other drugs’, 3.9 times as likely to have used alcohol, and 5.3 times more likely to have used tobacco. Whites were consistently the second-highest users, with the exception of cannabis, for which they were the highest users. Indians were least likely to have used any type of substance. These and other socio-demographic correlates – substance use being more common in males13 and in urban populations14 – are consistent with previous reports.
The use of all drug types has increased in younger populations, with younger cohorts starting to use ‘harder’ drugs at a younger age. Whereas early cohorts had a particularly higher prevalence of alcohol use, more recent cohorts demonstrated a particularly high prevalence of cannabis use. More recent cohorts were much more likely to start drug use, particularly extra-medical and other drug use, in childhood and in early to mid-adolescence. Of those who had used any substance, the age of onset was earlier for younger cohorts, and this was more evident for ‘other drugs’ than for alcohol and tobacco.
Conclusion
Substance use has multiple adverse consequences for individuals and for society in general. Prior work has demonstrated associations between substance use and health, crime and sexual behaviour. Substance abuse and its many interactions with the aforementioned and with mental illness must be taken into account in the allocation of resources and in the planning of health services.
Acknowledgments
The South African Stress and Health study was carried out in conjunction with the World Health Organization World Mental Health (WMH) Survey Initiative. We thank the WMH staff for assistance with instrumentation, fieldwork, and data analysis. These activities were supported by the US National Institute of Mental Health (R01MH070884), the John D and Catherine T MacArthur Foundation, the Pfizer Foundation, the US Public Health Service (R13-MH066849, R01-MH069864 and R01 DA016558), the Fogarty International Center (FIRCA R01-TW006481), the Pan American Health Organization, Eli Lilly and Company, Ortho-McNeil Pharmaceutical, Inc., GlaxoSmithKline, and Bristol-Myers Squibb. The South African Stress and Health study was funded by grant R01-MH059575 from the National Institute of Mental Health and the National Institute of Drug Abuse with supplemental funding from the South African Department of Health and the University of Michigan. Dan Stein and Soraya Seedat are also supported by the Medical Research Council of South Africa. A complete list of WMH publications can be found at http://www.hcp.med.harvard.edu/wmh/
Ms K Cloete, science writer, Department of Psychiatry, Stellenbosch University, is thanked for her contribution to the preparation and formatting of this manuscript.
Contributor Information
Margaretha S van Heerden, Department of Psychiatry, Stellenbosch University, Tygerberg, W Cape.
Anna T Grimsrud, School of Public Health and Family Medicine, University of Cape Town.
Soraya Seedat, MRC Stress and Anxiety Disorders Unit, Department of Psychiatry, Stellenbosch University, Tygerberg, W Cape.
Landon Myer, School of Public Health and Family Medicine, University of Cape Town.
David R Williams, Department of Society, Human Development and Health, Harvard School of Public Health, and Department of African and African American Studies, Harvard University, Cambridge, Mass., USA.
Dan J Stein, Department of Psychiatry and Mental Health, University of Cape Town.
References
- 1.Parry CDH. Prepared for the WHO/UNDCP regional consultation – Global initiative on primary prevention of substance abuse among young people, Harare. Zimbabwe: Feb 24–26, 1998. [accessed 3 March 2009]. Substance use in South Africa: Country report focusing on young persons. www.sahealthinfo.org/admodule/countryreport.pdf. [Google Scholar]
- 2.South African Community Epidemiology Network on Drug Use (SACENDU) Report Back Meetings, Medical Research Council, Alcohol and Drug Abuse Research Unit, October/November 2006. Tygerberg, W Cape: Medical Research Council; 2006. [Google Scholar]
- 3.Williams DR, Herman A, Kessler RA, et al. The South Africa Stress and Health Study: Rationale and design. Metab Brain Dis. 2004;19(1–2):135–147. doi: 10.1023/b:mebr.0000027424.86587.74. [DOI] [PubMed] [Google Scholar]
- 4.Anthony JC, Warner L, Kessler R. Comparative epidemiology of dependence on tobacco, alcohol, controlled substances, and inhalants: Basic findings from the National Comorbidity Survey. Exp Clin Psychopharmacol. 2004;2:244–268. [Google Scholar]
- 5.Degenhardt L, Chu WT, Sampson N, et al. Epidemiological patterns of extra medical drug use in the United States: Evidence from the national Comorbidity Survey Replication, 2001 – 2003. Drug Alcohol Depend. 2007;90:210–223. doi: 10.1016/j.drugalcdep.2007.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Myer L, Stein DJ, Grimsrud A, et al. Social determinants of psychological distress in a nationally-representative sample of South African adults. Soc Sci Med. 2008;66:1828–1840. doi: 10.1016/j.socscimed.2008.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Van Walbeek C. Political change in South Africa: New tobacco control and public health policies. In: de Beer J, Waverley Brigden I, editors. Tobacco Control Policy: Strategies, Successes and Setbacks. Washington, DC: World Bank and Research for International Tobacco Control; 2002. pp. 121–153. [Google Scholar]
- 8.Reddy P, Swart D. Prepared for World No Tobacco Day. Medical Research Council; KwaZulu-Natal, South Africa: May, 2003. [accessed 3 March 2009]. Preliminary report on Global Youth tobacco survey 2002. www.who.int/entity/tobacco/surveillance/South%20Africa%20GYTS%20Report%202002.pdf. [Google Scholar]
- 9.United Nations. Office on Drugs and Crime. [accessed 3 March 2009];2004 World Drug Report. 2:394. www.unodc.org/pdf/WDR_2004/volume_2.pdf.
- 10.Wu LT, Korper S, Marsden ME, Lewis C, Bray RM. Use of Incidence and Prevalence in the Substance Use Literature: A Review. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2003. [Google Scholar]
- 11.Jonhson RA, Gerstein D. Initiation of use of alcohol, cigarettes, marijuana, cocaine and other substances in US birth cohorts since 1919. Am J Public Health. 1998;88:27–33. doi: 10.2105/ajph.88.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Degenhardt L, Lynskey M, Hall W. Cohort trends in the age of initiation of drug use in Australia. Aust N Z J Public Health. 2000;24:421–426. doi: 10.1111/j.1467-842x.2000.tb01605.x. [DOI] [PubMed] [Google Scholar]
- 13.Parry CDH. Alcohol, drug abuse and public health. In: Foster D, Freeman M, Pillay Y, editors. Mental Health Policy for South Africa. Cape Town: Medical Association of South Africa; 1997. pp. 290–315. [Google Scholar]
- 14.Rocha-Silva L. Alcohol and Other Drug Use by Residents of Major Districts in the Self-governing States in South Africa. Pretoria: Human Sciences Research Council; 1991. [Google Scholar]