Abstract
Background
There are few reports from South Africa on how common mental disorders may be associated with HIV-related perceptions and behaviours.
Methods
Between 2002 and 2004, 4 351 South African adults were interviewed. Psychiatric diagnoses of depression, anxiety and substance abuse disorders were based on the Diagnostic and Statistical Manual, 4th edition (DSM-IV). HIV-related fears, perceived risk and behaviour change were measured using multi-item scales. We analysed forms of behaviour change that were appropriate for risk reduction (such as changes in sexual behaviour) separately from behaviour changes that were inappropriate to prevent HIV (such as care over things touched or avoiding certain social situations).
Results
The presence of any DSM-IV-defined disorder during the previous 12 months was associated with previous HIV testing, increased HIV-related fears, and high levels of perceived risk of HIV. There were no associations between depression, anxiety and substance abuse disorders and appropriate forms of behaviour change for HIV risk reduction. However, individuals with an anxiety or a depressive disorder were more likely to report inappropriate forms of behaviour change. For example, individuals with any depressive and/or anxiety disorders were 1.57 and 1.47 times more likely, respectively, to report avoiding certain social situations to prevent HIV/AIDS compared with those who did not have such disorders (p<0.01 for both associations).
Discussion
The lack of appropriate forms of behaviour change to prevent HIV transmission, despite increased levels of HIV-related fear and perceived risk, underscores the need for HIV risk reduction interventions for individuals living with common mental disorders in South Africa.
The interactions between HIV/AIDS and mental health have received little attention in South Africa and other low- and middle-income countries,1,2 despite the heavy impact of HIV and mental disorders on the public health. It is estimated that more than 15% of South African adults are infected with HIV,3 and 16%, 10% and 13% of South African adults have had an anxiety, mood or substance-related disorder in their lifetime.4 Better understanding of the inter-relationships between common mental disorders and HIV/AIDS-related behaviours and risk perception is essential to improving population health.
A high prevalence of mental disorders among HIV-infected individuals has been shown in South Africa,5–7 other parts of sub-Saharan Africa8–9 and Europe and North America.10–11 This association is widely thought to be attributable to the stress associated with being diagnosed as having a highly stigmatised chronic condition, although the direct effect of HIV on the central nervous system plays an important role in mental disorders later in the course of disease. There is also increasing evidence that risk behaviours related to HIV acquisition are associated with common mental disorders. For example, a cross-sectional study from a township near Cape Town found that individuals with evidence of depression, post-traumatic stress disorder (PTSD) and/or alcohol abuse were more likely to report both transactional and forced sex.12 However, the causal relationships between these factors remain unclear: mental disorders may increase HIV risk (e.g. by impairing risk perception and impulse control), or this association may be confounded by a common cause (e.g. lower socio-economic status leading to increased vulnerability to both mental disorders and HIV risk behaviours).
Despite this evidence, there are few insights from population-based samples in South Africa and sub-Saharan Africa into how common mental disorders may be associated with HIV-related perceptions and behaviours. We investigated these issues in an analysis of the South African Stress and Health (SASH) study, a nationally representative survey of South African adults conducted between 2002 and 2004.
Methods
The SASH survey methods have been described.13 Briefly, a probability sample of adults was selected using three-stage design. Enumeration areas (EAs, the units of census administration) were stratified according to province, urban or rural location and majority population group (black, coloured, white or Indian), and 960 units were selected with probability proportional to EA size. Within an EA a random sample of five households was selected; one adult (age 18 years or older) was then randomly selected from each household. Home visits took place between 2002 and 2004. The overall response rate was 86%, and the final sample size was 4 351 individuals. Interviews lasting between 3 and 4 hours were conducted by fieldworkers with specialised training in psychiatric interviewing in one of seven local languages. The survey protocol was approved by the Human Subjects Committees of the University of Michigan and Harvard Medical School, and by a single project assurance of compliance from the Medical University of South Africa that was approved by the National Institute of Mental Health (USA).
The World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) Version 3.014 was used to measure mental disorders prevalent in the preceding 12 months, based on the Diagnostic and Statistical Manual, 4th edition (DSM-IV). The CIDI has demonstrated excellent test characteristics, including validity compared with clinical assessment.15,16 For the SASH survey, the English CIDI was translated into six other major languages used in South Africa (Zulu, Xhosa, Southern Sotho, Northern Sotho, Tswana and Afrikaans), with repeated back-translations following WHO recommendations; discrepancies were resolved by an expert panel. This analysis includes only 12-month anxiety (agoraphobia, generalised anxiety disorder, social phobia, panic disorder and post-traumatic stress disorder (PTSD)), depressive (major and minor depression) and substance-related (alcohol dependence or abuse and drug dependence or abuse) disorders. The overall prevalence and demographic correlates of each of these 12-month DSM-IV disorders has been reported.17
HIV-related fears were measured using a 5-item scale which asked: ‘Because of HIV/AIDS, how much are you afraid of the following: (i) safety of blood and body fluids; (ii) giving blood; (iii) receiving blood; (iv) having an injection; and (v) having an operation?’ Each item could be responded to on a 4-point scale from ‘Not at all’ to ‘A lot’. This scale showed excellent internal reliability (Cronbach’s alpha, 0.82). Perceived risk of HIV/AIDS was measured using a single item phrased as ‘Would you say your chances of getting HIV/AIDS are very high, high, medium, low, or none?’; the highest score was assigned to ‘very high’ chances. To investigate behavioural changes in response to HIV/AIDS, participants were asked if they had personally done any of the following to prevent themselves becoming infected with HIV/AIDS: (i) seeking more stability in choice of partners; (ii) taking precautions in sexual intercourse; (iii) taking more care over things touched; (iv) avoiding certain social situations and places; and (v) avoiding some types of people. For this analysis, items (i) and (ii) were regarded as appropriate risk-reduction practices, and items (iii), (iv) and (v) as inappropriate. This scale showed good internal consistency reliability (Cronbach’s alpha, 0.72), but we analysed items individually to assess potential differences between appropriate and inappropriate behaviours.
Participant demographic characteristics (age, gender, race, urban/rural location) were collected using standard questionnaire items. Racial groupings (black, coloured, Asian and white) are used as a marker of historical social and economic opportunity, and many health outcomes in South Africa (including HIV/AIDS) are patterned according to these racial categories as a legacy of apartheid. Estimated household income, years of participant education, participant employment and household asset ownership were included as measures of socio-economic status.
Data were analysed using Stata Version 9.2 (Stata Corporation, College Station, USA). Analyses included person-level weights that accounted for survey design features, including sample selection, non-response and post-stratification. The HIV-related fears variable was recoded and analysed as a continuous scale with higher scores indicating greater fear. In analysis of the perceived HIV risk scale, 607 participants responded ‘Don’t know’; these observations were excluded from the analysis of this variable. Pearson’s chi-square tests were used to examine crude associations between participant demographic characteristics, 12-month mental disorders, and HIV-related fears, perceived risks and preventive actions. We developed separate multiple logistic regression models to adjust for covariation in participant demographic and socio-economic characteristics in examining the association between different mental disorders and HIV testing, HIV-related fears, perceived risk and preventive behaviours. The coefficients from these models are reported as odds ratios with 95% confidence intervals.
Results
Overall, the mean age of participants was 36.8 years (standard deviation 14.6 years); 55% were female; 77% were black, and 61% lived in an urban area (Table I). Approximately one-fifth of participants reported that they had been tested for HIV infection previously. A DSM-IV-defined mental disorder had been present during the previous year in 16.5% of the sample, anxiety disorders being the most common (8.1%), followed by depressive and substance-related disorders (4.9% and 5.8%, respectively).
Table I.
Participant demographic characteristics, 12-month DSM-IV disorders and HIV-related fears, actions and perceived risks
| Participant demographics | Characteristics (N=4 287) |
|---|---|
| Age (yrs) (mean) | 36.8 |
| Gender (%) | |
| Male | 45.0 |
| Female | 55.0 |
| Location (%) | |
| Rural | 39.2 |
| Urban | 60.8 |
| Race (%) | |
| Black | 77.0 |
| Coloured | 10.9 |
| White | 8.7 |
| Asian | 3.4 |
| Education (%) | |
| None | 6.9 |
| Grade 1 – 7 | 19.4 |
| Grade 8 – 11 | 35.3 |
| Completed high school | 23.3 |
| Post-high school education | 15.1 |
| Tested for HIV in the past (%) | 20.9 |
| HIV-related fears (%) | |
| Fear of blood and body fluids: high | 56.1 |
| Fear of giving blood: high | 36.4 |
| Fear of receiving blood: high | 60.6 |
| Fear of having an injection: high | 38.3 |
| Fear of having an operation: high | 49.4 |
| Mean score on HIV fear scale | 3.55 |
| Perceived HIV risk (%) | |
| None | 42.8 |
| Low | 33.9 |
| Medium | 13.8 |
| High | 4.9 |
| Very high | 4.6 |
| Mean score for perceived risk of HIV | 1.9 |
| HIV-related actions (%) | |
| Seek more stable partnerships | 80.0 |
| Precautions in sexual intercourse | 80.0 |
| Care over things touched | 62.1 |
| Avoid certain social situations/places | 50.7 |
| Avoid certain people | 45.6 |
| Mean number of actions taken to prevent HIV | 3.0 |
| 12-month DSM-IV disorders (%) | |
| Any disorder | 16.5 |
| Any depressive disorder | 4.9 |
| Any anxiety disorder | 8.1 |
| Generalised anxiety disorder | 1.4 |
| Post-traumatic stress disorder | 0.6 |
| Agoraphobia | 4.8 |
| Panic disorder | 0.8 |
| Social phobia | 1.9 |
| Any substance-related disorder | 5.8 |
| Any alcohol abuse/dependence | 4.7 |
| Any drug abuse/dependence | 1.5 |
High levels of fear in response to individual items on the HIV-related fears scale were reported by 40 – 60%; the highest levels of fear were associated with blood and body fluids. Almost 10% perceived that they were at high or very high risk of becoming infected with HIV. Levels of self-reported behaviour change to reduce HIV infection risk were high for appropriate forms of behaviour change (seeking stable partnerships and taking precautions during intercourse), but significantly lower for inappropriate behaviours: 62% reported that they took care over things touched, 51% said that they avoided certain social situations or places, and 46% said that they avoided certain people to prevent becoming infected with HIV.
HIV testing, HIV-related fears and perceived risk were strongly patterned according to participant demographic characteristics (Table II). Previous HIV testing and perceived risk of HIV were greatest among young people, and increased with increasing education. Younger and better educated participants were also more likely to report appropriate forms of behaviour change to prevent HIV infection. However, inappropriate behaviours to prevent HIV infection, particularly avoidance of certain social settings and people, had few demographic correlates.
Table II.
Crude associations between participant demographic characteristics and HIV-related fears, actions and perceived risk (all cells are row percentages unless otherwise specified)
| Previous HIV testing | HIV-related fears scale (mean) | Perceived risk of HIV scale (mean) | HIV-related actions
|
|||||
|---|---|---|---|---|---|---|---|---|
| Seek more stable partnerships | Precautions in sexual intercourse | Care over things touched | Avoid certain social situations/places | Avoid certain people | ||||
| Total population | 20.9 | 3.5 | 1.9 | 80.0 | 80.0 | 62.1 | 50.7 | 45.6 |
| Age (yrs) | ||||||||
| 18 – 29 | 21.3 (p<0.001) | 3.7 (p<0.001) | 2.1 (p<0.001) | 83.7 (p<0.001) | 86.3 (p<0.001) | 62.2 (p=0.788) | 52.9 (p=0.208) | 47.9 (p=0.138) |
| 30 – 39 | 26.6 | 3.5 | 2.1 | 80.9 | 81.5 | 61.1 | 49.9 | 45.5 |
| ≥40 | 17.2 | 3.4 | 1.7 | 75.4 | 72.1 | 62.6 | 48.9 | 43.2 |
| Gender | ||||||||
| Male | 21.0 (p=0.865) | 3.5 (p=0.017) | 2.0 (p=0.312) | 81.2 (p=0.199) | 82.1 (p=0.003) | 59.2 (p=0.007) | 49.1 (p=0.155) | 44.9 (p=0.554) |
| Female | 20.8 | 3.6 | 1.9 | 79.0 | 78.1 | 64.5 | 52.1 | 46.1 |
| Location | ||||||||
| Rural | 13.3 (p<0.001) | 3.6 (p=0.039) | 2.0 (p=0.397) | 80.2 (p=0.789) | 80.5 (p=0.665) | 66.1 (p=0.017) | 51.5 (p=0.616) | 46.5 (p=0.586) |
| Urban | 25.8 | 3.5 | 1.9 | 79.8 | 79.6 | 59.5 | 50.2 | 45.0 |
| Race | ||||||||
| Black | 16.9 (p<0.001) | 3.6 (p<0.001) | 2.0 (p<0.001) | 80.4 (p=0.163) | 82.1 (p<0.001) | 64.5 (p<0.001) | 51.6 (p=0.487) | 46.9 (p=0.187) |
| Coloured | 36.4 | 3.3 | 1.6 | 84.0 | 79.1 | 59.9 | 49.1 | 41.8 |
| White | 34.2 | 3.1 | 1.6 | 72.8 | 64.0 | 46.1 | 45.9 | 39.3 |
| Asian | 28.8 | 3.4 | 1.7 | 75.7 | 74.7 | 56.1 | 49.3 | 45.3 |
| Education | ||||||||
| None | 7.2 (p<0.001) | 3.6 (p=0.007) | 1.7 (p=0.003) | 69.8 (p<0.001) | 67.1 (p<0.001) | 66.2 (p=0.021) | 51.8 (p=0.596) | 44.1 (p=0.744) |
| Grade 1 – 7 | 11.6 | 3.6 | 1.8 | 74.7 | 73.5 | 66.5 | 49.8 | 45.2 |
| Grade 8 – 11 | 18.6 | 3.6 | 2.0 | 81.7 | 80.5 | 63.0 | 50.9 | 45.4 |
| Completed high school | 26.0 | 3.5 | 2.0 | 84.3 | 87.8 | 60.3 | 52.8 | 47.8 |
| Post-high school education | 37.5 | 3.3 | 2.0 | 81.1 | 80.5 | 56.8 | 47.6 | 43.9 |
Table III shows the association between DSM-IV disorders, HIV testing, and HIV-related fears, perceived risk and behaviour change. On average, individuals with any DSM-IV disorder in the previous 12 months reported higher levels of fear related to HIV/AIDS. However, this appears to be driven largely by increased fears regarding blood and body fluids, and the associations only reached statistical significance when comparing any disorder, and any anxiety disorder specifically. Perceived risk of HIV infection was similar in individuals with depressive disorders and those with no disorder, but significantly higher in those with anxiety or substance-related disorders. Individuals with DSM-IV-defined anxiety or depressive disorders were more likely than individuals with no disorder to report behavioural changes to protect against HIV/AIDS. However, these differences were primarily in inappropriate protective behaviours, most notably avoiding certain social situations and places, and/or avoiding certain people; no significant differences were observed in the proportion of participants reporting seeking stable partnerships or taking precautions during sexual intercourse. When restricted to individuals who had not tested for HIV previously, the strength of these associations increased slightly but there was no evidence of statistical interaction (data not shown).
Table III.
Crude associations between 12-month DSM-IV-defined mental disorders and previous HIV testing, HIV-related fears, actions and perceived risk (all cells are column percentages unless otherwise specified)
| No disorder | Any disorder | p-value | Any depressive disorder | p-value | Any anxiety disorder | p-value | Any substance disorder | p-value | |
|---|---|---|---|---|---|---|---|---|---|
| Previously tested for HIV | 20.1 | 24.8 | 0.030 | 26.6 | 0.107 | 25.0 | 0.057 | 25.6 | 0.115 |
| HIV-related fears | |||||||||
| Fear of blood and body fluids: high | 52.5 | 62.5 | <0.001 | 64.4 | 0.007 | 64.3 | <0.001 | 60.9 | 0.042 |
| Fear of giving blood: high | 35.8 | 39.3 | 0.144 | 42.3 | 0.053 | 41.9 | 0.151 | 34.9 | 0.806 |
| Fear of receiving blood: high | 60.3 | 62.1 | 0.469 | 64.7 | 0.254 | 67.1 | 0.079 | 53.9 | 0.075 |
| Fear of having an injection: high | 38.1 | 39.7 | 0.517 | 37.1 | 0.821 | 43.0 | 0.161 | 32.8 | 0.129 |
| Fear of having an operation: high | 48.9 | 52.1 | 0.270 | 54.8 | 0.261 | 54.5 | 0.146 | 48.4 | 0.915 |
| Mean score on HIV fear scale | 3.5 | 3.7 | 0.023 | 3.7 | 0.122 | 3.7 | 0.047 | 3.6 | 0.270 |
| Perceived HIV risk high or very high | 7.6 | 12.0 | 0.025 | 7.2 | 0.889 | 14.7 | 0.001 | 14.1 | 0.024 |
| Mean score for perceived risk of HIV | 1.9 | 2.1 | 0.002 | 2.0 | 0.264 | 2.1 | 0.004 | 2.3 | 0.004 |
| HIV-related actions | |||||||||
| Seek more stable partnerships | 79.4 | 82.6 | 0.164 | 82.9 | 0.433 | 82.8 | 0.281 | 80.1 | 0.866 |
| Precautions in sexual intercourse | 79.8 | 80.9 | 0.636 | 80.2 | 0.920 | 81.8 | 0.459 | 80.8 | 0.745 |
| Care over things touched | 61.6 | 64.7 | 0.203 | 66.2 | 0.216 | 68.1 | 0.053 | 57.8 | 0.385 |
| Avoid certain social situations/places | 49.5 | 56.5 | 0.004 | 60.8 | <0.001 | 59.6 | 0.003 | 46.6 | 0.490 |
| Avoid certain people | 44.2 | 52.2 | 0.003 | 59.8 | <0.001 | 51.4 | 0.050 | 45.5 | 0.151 |
| Mean number of actions taken | 3.0 | 3.2 | 0.001 | 3.4 | <0.001 | 3.3 | 0.005 | 3.0 | 0.630 |
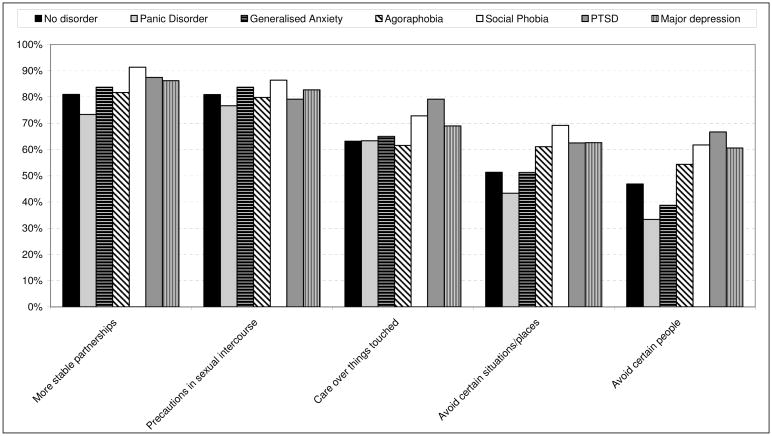
When comparing different types of reported behaviour change among individuals with specific DSM-IV-defined anxiety and depressive disorders during the previous 12 months (Fig. 1), individuals with panic disorder and generalised anxiety disorder showed similar levels of behaviour change (both appropriate and inappropriate). Individuals with agoraphobia, social phobia, PTSD and major depression reported similar levels of appropriate behaviour change to those with no disorder, but generally higher levels of inappropriate behaviour change. For example, compared with individuals with no disorder during the previous 12 months, individuals with major depressive disorder were 1.5 times as likely to report avoiding certain social situations or places, and 1.8 times as likely to report avoiding certain people, in order to prevent HIV infection (p=0.001 and 0.005, respectively).
Fig. 1.
Percentage of participants reporting different actions to prevent themselves from becoming infected with HIV, according to specific anxiety disorders and major depression.
In multivariate models adjusting for participant demographic characteristics and socio-economic status (Table IV), a previous HIV test was more common among individuals with any depressive, anxiety or substance-related disorder. The perceived risk of HIV infection was significantly greater among individuals with an anxiety disorder and those with a substance-related disorder, compared with no disorder. There was no difference in appropriate forms of reported behaviour change between individuals with and without mental disorder, but avoidance of both certain social situations and certain people was increased among individuals with a depressive or anxiety disorder.
Table IV.
Adjusted odds ratios (OR) and 95% confidence intervals (CI) for the associations between 12-month DSM-IV disorders and HIV testing, HIV-related fears, actions and perceived risk*
| Any disorder
|
Any depressive disorder
|
Any anxiety disorder
|
Any substance disorder
|
|||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Previous HIV testing | 1.41 | 1.06 – 1.87 | 1.54 | 0.94 – 2.52 | 1.46 | 1.05 – 2.02 | 1.41 | 0.91 – 2.17 |
| HIV-related fears scale (continuous) | 1.10 | 1.00 – 1.20 | 1.11 | 0.95 – 1.29 | 1.12 | 0.97 – 1.29 | 1.08 | 0.96 – 1.22 |
| Perceived HIV risk high or very high | 1.66 | 1.02 – 2.70 | 1.02 | 0.49 – 2.14 | 2.11 | 1.31 – 3.42 | 1.97 | 1.04 – 3.75 |
| HIV-related actions | ||||||||
| Seek more stable partnerships | 1.17 | 0.85 – 1.60 | 1.27 | 0.71 – 2.29 | 1.18 | 0.74 – 1.86 | 0.91 | 0.54 – 1.51 |
| Precautions in sexual intercourse | 1.04 | 0.75 – 1.45 | 1.09 | 0.61 – 1.92 | 1.14 | 0.77 – 1.71 | 0.91 | 0.57 – 1.43 |
| Care over things touched | 1.09 | 0.91 – 1.32 | 1.13 | 0.83 – 1.56 | 1.23 | 0.93 – 1.63 | 0.92 | 0.65 – 1.30 |
| Avoid certain social situations/places | 1.31 | 1.08 – 1.59 | 1.57 | 1.19 – 2.06 | 1.47 | 1.14 – 1.90 | 0.94 | 0.67 – 1.32 |
| Avoid certain people | 1.34 | 1.09 – 1.64 | 1.92 | 1.45 – 2.54 | 1.29 | 0.96 – 1.74 | 1.03 | 0.72 – 1.48 |
All logistic regression models are adjusted for participant age, gender, race, education, employment status, family income and personal asset ownership. Individuals without any 12-month DSM disorder are the reference group for all comparisons.
Discussion
This analysis presents important data on the association of DSM-IV-defined common mental disorders with HIV-related fears, perceptions of risk and behaviour change. Individuals with common mental disorders are more likely to have had an HIV test previously, and to have increased HIV-related fears, than individuals without disorders. There is also evidence of an association between inappropriate HIV-related actions and mental disorders, as individuals with depressive or anxiety disorders were more likely to report avoiding social situations or places, and individuals with depressive disorders were more likely to report avoiding certain people, in an attempt to prevent HIV infection.
These results should be interpreted in light of a number of limitations. These are cross-sectional data, and the temporal order of these associations is therefore unclear, e.g. it is difficult to decipher whether mental disorders motivate HIV-related fears and testing, or whether HIV-related fears or testing contribute to the causation of different mental disorders. Still, the persistence of the associations after adjustment for participant demographic characteristics and socio-economic status, coupled with the importance of widespread HIV testing as an integral strategy for targeting HIV-related interventions, highlights the need for prospective studies to investigate these issues. Second, the analysis focused on DSM-IV-defined mental disorders, and did not address aspects of psychological distress that do not meet DSM-IV criteria. It is possible that subclinical mental disorders, as well as forms of alcohol and substance use that do not meet formal criteria for dependence or abuse, may have different relationships to HIV-related perceptions and behaviours. In addition, we did not have an objective measure of HIV infection status, and the measures of HIV-related behaviours used here are not exhaustive; further research is required to investigate how specific aspects of behaviour change such as condom use or partner selection may be influenced by mental health.
One striking aspect of these findings is that despite an association between increased perceived risk of HIV and different mental disorders, there was no association between depressive disorders, anxiety disorders or substance-related disorders and appropriate forms of behaviour change to reduce HIV risk. This seemingly contradictory finding is in keeping with evidence that fear-based HIV risk reduction counselling may increase perceived risk but paradoxically lead to lower levels of behaviour change.18 The absence of risk reduction behaviour change among individuals with alcohol- or drug-related disorders is of particular concern. There is ample evidence that substance use among infected individuals or those who are susceptible is associated with increased risk of HIV transmission.19–21 There is growing emphasis on different approaches to risk reduction interventions in these groups, either by targeting substance users as a high-risk population or by focusing interventions on locations where alcohol is dispensed. More intensive interventions in this area are warranted.
In contrast to the above, there were persistent associations between depressive and anxiety disorders and inappropriate forms of HIV-related behaviour change, in keeping with evidence of increased health-related anxieties among individuals with common mental disorders.22 While HIV-related hypochondriasis is well documented at an individual patient level, usually in the context of obsessive-compulsive disorders, these are the first data to demonstrate this phenomenon related to HIV/AIDS in a population-based sample from sub-Saharan Africa. In this case, it is plausible to view inappropriate forms of behaviour change as a manifestation of anxiety and/or depressive disorders, but further research is required to understand other possible influences of the HIV epidemic on the behaviours of individuals with mental illness.
These results point to a substantial missed opportunity to promote HIV risk reduction among individuals with anxiety and depression. While there is increased perception of HIV-related risk, and increased fear of becoming infected with the virus, among individuals with common mental disorders, this is accompanied by only inappropriate forms of behaviour change. In this context, individuals with anxiety and depressive disorders may represent a population in which appropriate HIV risk reduction interventions may have a substantial positive impact. While promoting sexual risk reduction among individuals with mental illness has unique challenges,23 there are examples of successful interventions from North America,24,25 and locally adapted interventions to reduce HIV risk behaviours among individuals with mental disorders in South Africa are clearly needed.
Given the significant roles that both HIV/AIDS and common mental disorders play in shaping population health, there is a need for better understanding of both the role of mental illness in the acquisition and course of HIV infection, and how HIV/AIDS influences the mental health of those who are either at risk or already infected. In particular, with increasing emphasis on the provision of care and treatment services to individuals living with HIV infection, these services provide important opportunity to identify and treat common mental illnesses.26 Strengthening the links between HIV/AIDS and mental health services should contribute to substantial gains in the prevention and more optimal management of both conditions.
Acknowledgments
The South African Stress and Health study was carried out in conjunction with the World Health Organization World Mental Health (WMH) Survey Initiative. We thank the WMH staff for assistance with instrumentation, fieldwork, and data analysis. These activities were supported by the US National Institute of Mental Health (R01MH070884), the John D and Catherine T MacArthur Foundation, the Pfizer Foundation, the US Public Health Service (R13-MH066849, R01-MH069864 and R01 DA016558), the Fogarty International Center (FIRCA R01-TW006481), the Pan American Health Organization, Eli Lilly and Company, Ortho-McNeil Pharmaceutical, Inc., GlaxoSmithKline and Bristol-Myers Squibb. The South African Stress and Health study was funded by grant R01-MH059575 from the National Institute of Mental Health and the National Institute of Drug Abuse with supplemental funding from the South African Department of Health and the University of Michigan. Dan Stein and Soraya Seedat are also supported by the Medical Research Council of South Africa. A complete list of WMH publications can be found at http://www.hcp.med.harvard.edu/wmh/
Contributor Information
Landon Myer, School of Public Health and Family Medicine, University of Cape Town.
Dan J Stein, Department of Psychiatry and Mental Health, University of Cape Town.
Anna T Grimsrud, School of Public Health and Family Medicine, University of Cape Town.
Allen Herman, National School of Public Health, University of Limpopo (Medunsa Campus), Pretoria.
Soraya Seedat, MRC Stress and Anxiety Disorders Unit, Department of Psychiatry, Stellenbosch University, Tygerberg, W Cape.
Hashim Moomal, African Public Health Initiatives, Johannesburg.
David R Williams, Department of Society, Human Development and Health, Harvard School of Public Health, and Department of African and African American Studies, Harvard University, Cambridge, Mass., USA.
References
- 1.Prince M, Patel V, Saxena S, et al. No health without mental health. Lancet. 2007;370:859–877. doi: 10.1016/S0140-6736(07)61238-0. [DOI] [PubMed] [Google Scholar]
- 2.Collins PY, Holman AR, Freeman MC, Patel V. What is the relevance of mental health to HIV/AIDS care and treatment programs in developing countries? A systematic review. AIDS. 2006;20(12):1571–1582. doi: 10.1097/01.aids.0000238402.70379.d4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dorrington R, Johnson L, Bradshaw D, Daniel T. The Demographic Impact of HIV/AIDS in South Africa. National and Provincial Indicators for 2006. Cape Town: Centre for Actuarial Research, South African Medical Research Council and Actuarial Society of Southern Africa; 2006. [Google Scholar]
- 4.Stein DJ, Seedat S, Herman A, et al. Lifetime prevalence of psychiatric disorders in South Africa. Br J Psychiatry. 2008;192(2):112–117. doi: 10.1192/bjp.bp.106.029280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Freeman M, Nkomo N, Kafaar Z, Kelly K. Factors associated with prevalence of mental disorder in people living with HIV/AIDS in South Africa. AIDS Care. 2007;19(10):1201–1209. doi: 10.1080/09540120701426482. [DOI] [PubMed] [Google Scholar]
- 6.Olley BO, Zeier MD, Seedat S, Stein DJ. Post-traumatic stress disorder among recently diagnosed patients with HIV/AIDS in South Africa. AIDS Care. 2005;17(5):550–557. doi: 10.1080/09540120412331319741. [DOI] [PubMed] [Google Scholar]
- 7.Myer L, Smit J, Roux LL, Parker S, Stein DJ, Seedat S. Common mental disorders among HIV-infected individuals in South Africa: prevalence, predictors, and validation of brief psychiatric rating scales. AIDS Patient Care STDs. 2008;22(2):147–158. doi: 10.1089/apc.2007.0102. [DOI] [PubMed] [Google Scholar]
- 8.Sebit MB, Tombe M, Siziya S, Balus S, Nkmomo SD, Maramba P. Prevalence of HIV/AIDS and psychiatric disorders and their related risk factors among adults in Epworth, Zimbabwe. East Afr Med J. 2003;80:503–512. doi: 10.4314/eamj.v80i10.8752. [DOI] [PubMed] [Google Scholar]
- 9.Kaaya SF, Fawzi MC, Mbwambo JK, Lee B, Msamanga GI, Fawzi W. Validity of the Hopkins Symptom Checklist-25 amongst HIV-positive pregnant women in Tanzania. Acta Psychiatr Scand. 2002;106:9–19. doi: 10.1034/j.1600-0447.2002.01205.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ciesla JA, Roberts JE. Meta-analysis of the relationship between HIV infection and risk for depressive disorders. Am J Psychiatry. 2001;158:725–730. doi: 10.1176/appi.ajp.158.5.725. [DOI] [PubMed] [Google Scholar]
- 11.Leserman J, Pence BW, Whetten K, et al. Relation of lifetime trauma and depressive symptoms to mortality in HIV. Am J Psychiatry. 2007;164(11):1707–1713. doi: 10.1176/appi.ajp.2007.06111775. [DOI] [PubMed] [Google Scholar]
- 12.Smit J, Myer L, Middelkoop K, et al. Mental health and sexual risk behaviours in a South African township: a community-based cross-sectional study. Public Health. 2006;120(6):534–542. doi: 10.1016/j.puhe.2006.01.009. [DOI] [PubMed] [Google Scholar]
- 13.Williams DR, Herman A, Kessler RC, et al. The South Africa Stress and Health Study: rationale and design. Metab Brain Dis. 2004;19(1–2):135–147. doi: 10.1023/b:mebr.0000027424.86587.74. [DOI] [PubMed] [Google Scholar]
- 14.Kessler RC, Ustün TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) Int J Methods Psychiatr Res. 2004;13(2):93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Andrew G, Peters L. The psychometric properties of the Composite International Diagnostic Interview. Soc Psychiatry Psychiatr Epidemiol. 1998;33:80–88. doi: 10.1007/s001270050026. [DOI] [PubMed] [Google Scholar]
- 16.Haro JM, Arbabzadeh-Bouchez S, Brugha TS, et al. Concordance of the Composite International Diagnostic Interview Version 3.0 (CIDI 3.0) with standardized clinical assessments in the WHO World Mental Health Surveys. Int J Methods Psychiatr Res. 2006;15:167–180. doi: 10.1002/mpr.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Williams DR, Herman A, Stein DJ, et al. Twelve-month mental disorders in South Africa: prevalence, service use and demographic correlates in the population-based South African Stress and Health Study. Psychol Med. 2008;38(2):211–220. doi: 10.1017/S0033291707001420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Earl A, Albarracín D. Nature, decay, and spiraling of the effects of fear-inducing arguments and HIV counseling and testing: a meta-analysis of the short- and long-term outcomes of HIV-prevention interventions. Health Psychol. 2007;26(4):496–506. doi: 10.1037/0278-6133.26.4.496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kalichman SC, Simbayi LC, Vermaak R, Jooste S, Cain D. HIV/AIDS risks among men and women who drink at informal alcohol serving establishments (shebeens) in Cape Town, South Africa. Prev Sci. doi: 10.1007/s11121-008-0085-x. (in press) [DOI] [PubMed] [Google Scholar]
- 20.Myer L, Mathews C, Little F. Condom use and sexual behaviors among individuals procuring free male condoms in South Africa: a prospective study. Sex Transm Dis. 2002;29(4):239–241. doi: 10.1097/00007435-200204000-00009. [DOI] [PubMed] [Google Scholar]
- 21.Zablotska IB, Gray RH, Serwadda D, et al. Alcohol use before sex and HIV acquisition: a longitudinal study in Rakai, Uganda. AIDS. 2006;20(8):1191–1196. doi: 10.1097/01.aids.0000226960.25589.72. [DOI] [PubMed] [Google Scholar]
- 22.Deale A. Psychopathology and treatment of severe health anxiety. Psychiatry. 2007;6(6):240–246. [Google Scholar]
- 23.Berkman A, Cerwonka E, Sohler N, Susser E. A randomized trial of a brief HIV risk reduction intervention for men with severe mental illness. Psychiatr Serv. 2006;57(3):407–409. doi: 10.1176/appi.ps.57.3.407. [DOI] [PubMed] [Google Scholar]
- 24.Susser E, Valencia E, Sohler N, Gheith A, Conover S, Torres J. Interventions for homeless men and women with mental illness: reducing sexual risk behaviours for HIV. Int J STD AIDS. 1996;7(Suppl 2):66–70. doi: 10.1258/0956462961917672. [DOI] [PubMed] [Google Scholar]
- 25.Collins PY, Geller PA, Miller S, Toro P, Susser ES. Ourselves, our bodies, our realities: an HIV prevention intervention for women with severe mental illness. J Urban Health. 2001;78(1):162–175. doi: 10.1093/jurban/78.1.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Freeman M, Patel V, Collins PY, Bertolote J. Integrating mental health in global initiatives for HIV/AIDS. Br J Psychiatry. 2005;187:1–3. doi: 10.1192/bjp.187.1.1. [DOI] [PubMed] [Google Scholar]