Abstract
C–X–C motif chemokine 10 (CXCL10) also known as interferon γ-induced protein 10 kDa (IP-10) or small-inducible cytokine B10 is a cytokine belonging to the CXC chemokine family. CXCL10 binds CXCR3 receptor to induce chemotaxis, apoptosis, cell growth and angiostasis. Alterations in CXCL10 expression levels have been associated with inflammatory diseases including infectious diseases, immune dysfunction and tumor development. CXCL10 is also recognized as a biomarker that predicts severity of various diseases. A review of the emerging role of CXCL10 in pathogenesis of infectious diseases revealed diverse roles of CXCL10 in disease initiation and progression. The potential utilization of CXCL10 as a therapeutic target for infectious diseases is discussed.
Keywords: Chemokine, CXCL10, CXCR3, Infectious diseases
1. Introduction
Inflammation is associated with secretion of CXCL10 from leukocytes, neutrophils, eosinophils [1], monocytes, epithelia, endothelial and stromal cells, and keratinocytes in response to IFN-γ [2], [3]. CXCL10 specifically activates CXCR3 receptor, a seven trans-membrane-spanning G protein-coupled receptor (GPCR) [4], which is predominantly expressed on activated T, B lymphocyte [5], natural killer (NK), dendritic and macrophage cells. CXCL10 induces chemotaxis, apoptosis, cell growth inhibition and angiostasis. Abnormal levels of CXCL10 have been observed in body fluids of individuals infected with viruses [1], [6], [7], bacteria [8], [9], fungi [10] and parasites [11], [12], [13] indicating an important role in pathogenesis of these diseases.
2. The CXCL10 gene structure, function, and signaling pathways
2.1. CXCL10 gene structure
Human CXCL10 gene, was initially isolated in 1985 by Luster [14] while treating a lymphoma cell line (U937) with recombinant IFN-γ. CXCL10 cDNA has an open reading frame of 1173-bp containing 4 exons and encoding a protein of 98-amino acids with a molecular mass of 10 kDa. The primary translational product of the CXCL10 gene is a 12 kDa protein containing two internal disulfide cross bridges [2]. The predicted signal peptidase cleavage generates a 10 kDa secreted polypeptide with four conserved cysteine residues in the N-terminal [2]. CXCL10 gene localizes on chromosome 4 at band q21, a locus associated with an acute monocytic/B-lymphocyte lineage leukemia exhibiting translocation of t(4;11)(q21;q23). CXCL10 protein shows significant homology in sequence with a family of proteins having chemotactic (platelet factor 4, β-thromboglobulin) and mitogenic (connective tissue-activating peptide HI) activities, which are associated with inflammation and cell proliferation [2], [15]. Human CXCL10 has 63% homology in cDNA sequence with mouse CXCL10.
2.2. CXCL10 functions
CXCL10 exerts its biological effects by binding to CXCR3, a seven trans-membrane-spanning G protein-coupled receptor in a paracrine or autocrine fashion [3]. CXCL10 induction depends predominantly on the carboxyl-terminal region of CXCR3, which is essential for CXCR3 internalization, chemotaxis and calcium mobilization induced by the CXCL10 ligand [16], [17]. CXCL10 is a pleiotropic molecule capable of exerting potent biological functions, including promoting the chemotactic activity of CXCR3+ cells, inducing apoptosis, regulating cell growth and proliferation as well as angiogenesis in infectious and inflammatory diseases and cancer.
2.2.1. Regulation of CXCR3+ cell chemotaxis
All three CXCR3 receptor ligands (CXCL9, CXCL10, and CXCL11) have been shown to induce chemotaxis in different cell types of the immune system [18]. CXCL10 performs “homing” functions to chemoattract CXCR3-positive cells, including macrophages (microglia cell in CNS), dendritic cells, NK cells and activated T lymphocytes (CD4+ Th cells, CD8+ Tc cells) toward inflamed, infected and/or neoplastic areas. CD4+ Th cells are subdivided into two different types, known as type 1 Th (Th1) and type 2 Th (Th2). Th1 cells produce cytokines, such as IL-2, IFN-γ, and lymphotoxin-α, which cause the activation of macrophages and the process of opsonization and cytotoxicity [19]. In contrast, Th2 cells are considered to play a regulatory rather than protective role, since cytokines produced by these cells (i.e., IL-4 and IL-13) inhibit the production of Th1 cytokines and activation of macrophages [19]. The fact that Th1 cells produce IFN-γ, which induces the production by different cell types of CXCL10, enables CXCL10 in turn to attract and recruit Th1 cells, suggesting the existence of a positive feedback loop between IFN-γ producing Th1 cells and resident cells producing CXCL10 [20]. The powerful chemotactic action of CXCL10 on activated lymphocytes allows it to modulate both innate and adaptive immunity, inducing tissue damage and modulating tumor formation [18], [21], [22].
2.2.2. CXCL10 mediated induction of apoptosis
CXCL10 induces apoptosis under varied conditions. Neuronal apoptosis is mediated by over expression of CXCL10 in simian human immunodeficiency virus encephalitis via activation of caspase-3 [23]. Further exploration revealed the utilization of the intrinsic pathway activation in CXCL10-mediated apoptosis. For example, Sui et al. show that incubation of fetal neurons in vitro with CXCL10 increased Ca2+ uptake by the mitochondria, which released cytochrome C and activated the initiator caspase-9. Caspase-9 sequentially activated the effector caspase-3, ultimately causing apoptosis in HIV-associated dementia [24]. Klein's group used a murine model of West Nile virus (WNV) encephalitis to determine how pretreatment with TNF-α prevented neuronal apoptosis during in vitro WNV infection [25]. They found WNV-infected neurons that expressed TNF-α, interact with its receptor TNFR1 to down-regulate CXCR3 expression, and reduced CXCL10 mediated calcium transients and prevent Caspase-3 activation [26]. Some studies revealed that CXCL10 significantly increased the apoptotic rate of cancer cells in HPV-related cervical carcinoma [27], [28]. CXCL10 not only induces apoptosis in infectious diseases, it might also be involved in apoptosis during development of the nervous system and myeloma [29], [30], [31]. However, the precise mechanism is not yet understood although neuronal CXCL10 mediated recruitment and homing glial cells during embryogenesis in an in vitro model of cultured cortical neurons [29], [30]. CXCR3 has two isoforms (see Section 2.2.3), which show paradoxical effects on cell growth after interaction with its corresponding CXCL10 ligand. Alexander et al. in 2006 demonstrated that the ratio of CXCR3B to CXCR3A mRNA in different cell lines determined the selectivity of CXCLl0 for cellular proliferation or apoptosis. CXCL10 selectively induced apoptosis in HUVECs without changing the status of apoptosis in fibroblasts or human melanoma-A375 cells, since HUVECs have a predominance of CXCR3B, the inhibitory receptor [32].
2.2.3. CXCL10 regulation of cell growth and proliferation
CXCL10 has dual effects on cell growth [33]. The proliferative or anti-proliferative action of CXCL10 appears to be cell-type dependent, in other words, it may depend on the subtype of its receptor CXCR3. Three CXCR3 splice variants have been reported: CXCR3-A, CXCR3-B, and CXCR3-alt, which are differentially expressed by different cell types, resulting in divergent effects on proliferation when bound to its ligand CXCL10 [33]. CXCL10 co-localizes with a cell proliferation marker, cytokeratin 17 (K17) in tumor cells [3]. Its cell proliferating actions are cell cycle dependent. The main isoform, CXCR3-A, found in most cell types, codes for a protein of 368 amino acids [33] and couples with Gαi to activate ERK1/2, p38/MAPK, JNK and PI3-kinase/Akt signaling pathways, subsequently inducing intracellular calcium influx, DNA synthesis, and cell proliferation or chemotaxis [17], [33], [34], [35]. These types of cells include human normal bronchial epithelial cells [33], astrocytes, glioma cells [35], microglia cells [36], as well as breast cancer cells [3], [37]. Unfortunately studies on the interactions of CXCL10 and CXCR3-A in infectious disease are underdeveloped. Only one report documents that CXCR3(−/−) mice survived longer than wild type controls when infected with prion [38]. CXCR3-alt, which always co-expresses with CXCR3-A at a very low level [3], [33] has not been found associated with cell growth. The anti-proliferative function of CXCL10 is regulated by CXCR3-B. However, the mechanisms mediating CXCR3-B effects in the context of infectious diseases are unclear, most observations are from the field of cancer research. CXCR3-B codes for a larger protein of 416 amino acids, couples with Gαs to activate adenyl cyclase and causes inhibition of endothelial cell proliferation and migration [31], [33], [39]. Interestingly, this receptor subtype does not induce chemotaxis [31], [34]. These cell types have been found in uterine endometrial cancer [37], [40], glioblastoma [21], CCL-51 mammary tumor [41], [42] and colorectal cancer [43]. CXCR3+ T cell migration into inflamed and/or neoplastic areas attracted by CXCL10 along with CXCL9 and CXCL11 also contributes to anti-tumor progression and anti-metastasis mechanisms [21]. The variant CXCR3-B, a common receptor for all four angiostatic chemokines (CXCL4, CXCL9, CXCL10 and CXCL11), has enabled a better understanding of the role of CXC chemokines in the regulation of inflammation, angiostasis, and inhibition of endothelial cell proliferation [44].
2.2.4. CXCL10 and regulation of angiostasis
The CXC chemokines have dual effects on angiogenesis, depending on the presence or absence of the Glu–Leu–Arg (ELR) motif. ELR-negative CXCL10 is an angiostatic chemokine, which inhibits angiogenesis. Studies in Indian and Ghanaian patients with malaria revealed a hither to unknown angiostatic effects of elevated levels of CXCL10 in severe malaria patients coupled with reduced levels of vascular endothelial growth factor (VEGF) and platelet derived growth factor (PDGF) [11], [12]. Remarkably, angiogenic chemokine CXCL10 has been applied in gene therapy to treat high-risk HPV-related cervical carcinoma in mice models and shown to inhibit the growth of cervical carcinoma through combined actions, including reducing the formation of microvessels, down-regulation of the expression of proliferating cell nuclear antigen (PCNA) and human papillomavirus (HPV) oncoproteins E6 and E7, as well as increasing apoptotic rate of cancer cells [27]. As an ELR-negative CXC chemokine, CXCL10 exerts important effects in anti-tumor effects which cannot be omitted when we review angiostatic functions of CXCL10 [45], [46], [47]. In xenograft models of lymphoma, squamous cell carcinoma (SCCA) and adenocarcinoma of lung, the production of CXCL10 was inversely correlated with tumor growth. This resulted in marked reduction in tumor-associated angiogenesis. CXCL10 induced angiostatic action in a T-, NK-cells or macrophage independent manner [46], [47]. CXCL10 was reported to antagonize the action of fibroblast growth factor (bFGF), thus suppressing angiogenesis induced by bFGF in advanced uterine endometrial cancers [40]. In estrogen receptor positive (ER+) mammary tumor, CXCL10 inhibits vascular endothelial growth factor (VEGF) levels to reduce tumor burden [41].
2.3. Potential CXCL10 signaling pathways
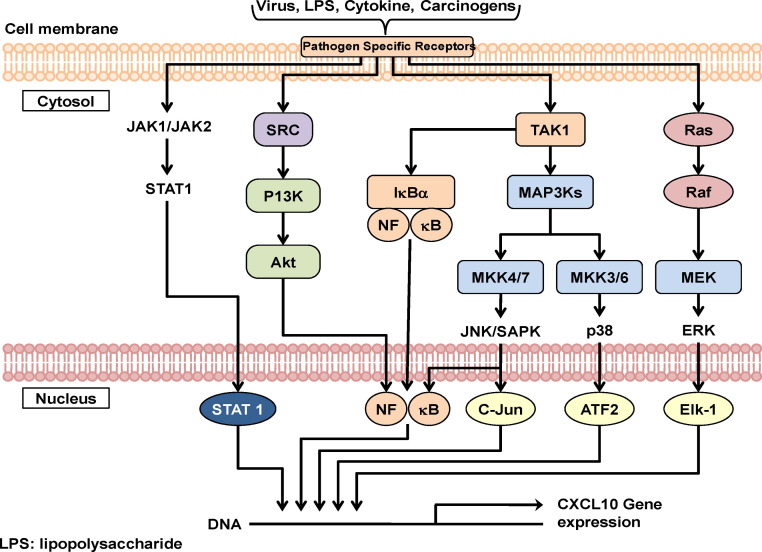
Recent studies have shown the importance of CXCL10 signaling and relevant downstream pathways in the regulation of different biological responses such as chemotaxis, cell motility and growth [36], [37], [48]. Interaction of CXCL10 with its receptor CXCR3, results in increased chemotactic activity through several signaling pathways. p38/MAPK and PI3K signaling play important roles in the CXCL10/CXCR3 chemokine receptor-induced chemotaxis in human airway epithelial cells [36], [37], [48]; in human type II pneumocytes, CXCL10/CXCR3 interaction induces chemotaxis via mitogen-activated protein kinase (MAPK) and PI 3-kinase pathways (PI3K) [34]; CXCL10 induces chemotactic responses in eosinophils possibly through the cAMP-dependent protein kinase A (PKA) signaling pathways [49]. Cell motility and proliferation are controlled through the activation of Ras/ERK, Src, and phosphatidylinositol 3-Kinase/Akt [50]. A proposed model of CXCL10 signaling in the regulation of biological responses in human airway epithelial cells and vascular pericytes is shown in Fig. 1 .
Fig. 1.
A model of CXCL10 signaling in human airway epithelial cells and vascular pericytes. ERK and p38 MAPK and PI3K/Akt [36], [37], [48] are all activated by interaction of CXCL10 with its receptor CXCR3. P38, PI3K/Akt and cAMP-dependent protein kinase A (PKA) [49] signaling pathways appear to regulate chemotaxis in human eosinophils, pneumocyte and epithelial cells. Activation of Ras/ERK, Src and PI3K/Akt [36], [50] controls cell migration and proliferation in human vascular pericytes.
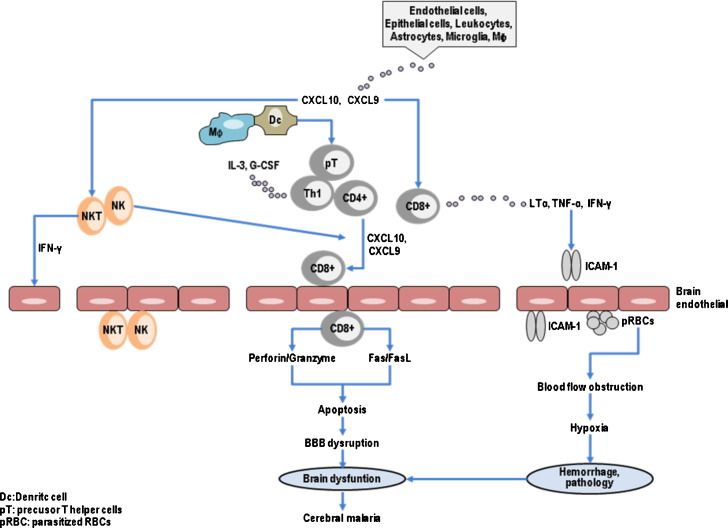
Since CXCL10 levels are linked with severe illness, understanding the mechanism of CXCL10 production and regulation could assist in the generation of therapeutic interventions in human diseases. We also reviewed how CXCL10 is produced and regulated under different conditions of infection. Chemokine CXCL10 is released from astrocytes by the combined actions of viral factors HIV-1 Tat and pro-inflammatory cytokines IFN-γ and TNF-α. During this process CXCL10 up regulation at both mRNA and protein levels is mediated through the activation of the p38, JNK, and Akt signaling pathways and their downstream transcription factors, NF-κB and STAT1 [51]. Mycobacterium bovis Bacillus Calmette-Guérin (BCG) regulates expression of CXCL10 in epithelial cells by induced activation of PI3K/Akt and NF-κB signaling pathways [52]. In murine macrophage-like cells, activation of JAK1, JAK2/STAT1 but not p38 pathways up regulate the expression of CXCL10 which is a strong inflammatory factor [53]. Thus it seems that inhibition of CXCL10 expression in target cells by targeting the JAK/STAT1 signaling pathway could exert anti-inflammatory effects through attenuation of chemokine CXCL10 production. Rabies virus (RV) stimulates CXCL10 expression in macrophages through activation of extracellular signal-regulated kinases 1 and 2 (ERK1/2) [54], whereas in microglia in CNS this was achieved by the activation of p38 and NF-κB pathways [55]. Regarding cancer studies, over expression of CXCL10 in human cancer is mediated through the Raf, PI3K, p38/MAPK, JNK/MAPK and NF-κB signaling cascades which promote cell proliferation and contribute to the development of tumors [36], [37]. A proposed schematic model of the signaling pathways involved in the increased induction of CXCL10 in human macrophages, microglia, epithelial and cancer cells in response to various stimuli are shown in Fig. 2 .
Fig. 2.
Schematic model of the signaling pathways involved in the induction of CXCL10 in human macrophages, microglia, epithelial and cancer cells in response to various stimulus. The major signaling pathways activated include p38, JNK, ERK, Akt and NFκB [51], [52], [53], [54], [55]. The activation of corresponding downstream nuclear signaling of above molecules, along with the activation of STAT1, results in the transcription of CXCL10 [51], [53]. P38 and ERK are able to converge on NFκB [52] (not shown for clarity).
3. CXCL10 in infectious disease
The role of CXCL10 has been discovered in various infectious diseases. The multifunctional features of CXCL10 make it a promising target for the treatment of infectious diseases. However, the mechanism of CXCL10 in the pathogenesis of infectious disease remains unclear. At present the studies in this field have been left far behind other fields such as tumor biology studies. Here we review the alteration of CXCL10 levels in infectious diseases with the aim to raise the awareness of its importance.
3.1. Altered expression of CXCL10 and viral infection
CXCL10 has been implicated in rhinovirus [56], respiratory syncytial virus (RSV) [1], [6], [7], Coxsackie virus, hepatitis virus B and C [57], Ebola [58], dengue (DENV) [59], [60] and equine infectious anemia virus (EIAV) [61] infections. CXCL10 either protects or promotes infection, depending on host immune status and genetic background [62]. CXCL10 is protective in coronavirus (CoV)-induced severe acute respiratory syndrome (SARS) [63], [64] and EBV-immortalized cells [65]. In contrast, CXCL10 facilitates herpes simplex virus type 2 (HSV-2) [66] and HIV infection by stimulating virus replication in macrophages and lymphocytes [67]. Over expression of CXCL10 may precede or follow onset of certain diseases [68], [69], [70]. For example, the increased expression of CXCL10 occurs prior to the development of clinical symptoms, as observed during HIV infection, in brain tissue of neonatal mice infected with virulent (Fr98) polytropic murine retroviruses [69]; whereas in SARS patients, elevation of CXCL10 levels occurred for at least two weeks after disease onset [68], [70]. Persistently high levels of CXCL10 have been reported to be associated with immunological treatment failure following highly active anti-retroviral therapy (HAART) in HIV-infected patients [71]. The CXCL10 levels were positively correlated with the extent of organ damage and pathogen burden [72]. In both HCV-monoinfected and HCV/HIV-co-infected patients, elevated CXCL10 levels were positively correlated with liver damage (as indicated by high liver fibrosis scores and liver enzyme levels) [72], [73]. Co-infections with HIV virus and other pathogens up regulated CXCL10 beyond that observed in mono-infected patients. For instance, CXCL10 was significantly more elevated in HCV/HIV co-infected patients than mono-infected ones [72], as well as elevated in AIDS/cryptosporidiosis co-infection [74] than AIDS alone. In a case-control study in Chinese HBV carriers, the polymorphism G-201A in the promoter of the CXCL10 gene predicted susceptibility to chronic HBV infection [62]. Decreased plasma CXCL10 levels have been achieved by corticosteroid hormone in SARS [68], [70]. Anti-retroviral therapy or other interference of CXCL10 and CXCR3 interactions also reduces plasma CXCL10 levels in HIV infection [67]. Anti-retrovirus treatment reduced plasma CXCL10 indicating an important role of CXCL10 in pathogenesis of the diseases.
3.2. CXCL10 and bacterial infection
CXCL10 have been shown to play a role in Helicobacter pylori [75], Mycoplasma [75], [76] and marginal periodontitis [77] infections by recruitment of inflammatory T cells into the mucosa [75] and inflamed gingival tissues [77]. Elevation of CXCL10 levels appears to be an early host response to scrub typhus infection [78] and is associated with severity of Legionnaire's disease and tuberculosis (TB) [79]. Antimicrobial treatment significantly decreased the level of CXCL10 in a murine model of Mycoplasma pneumonia [76]. In tuberculosis (TB), a significantly high level of CXCL10, like adenosine deaminase (ADA), is indicative of acute disease and may be used as a suitable surrogate or additional marker for immunodiagnosis [80], [81], [82], [83]. Furthermore the enhanced CXCL10 transactivation is achieved by a specific SNP genotype (−135G>A) of the CXCL10 gene promoter, upstream of the NF-κB binding site [84] indicating that CXCL10 gene polymorphism may be associated with observed disparities in CXCL10 levels in subset of individuals during diseases. During Chlamydia infections the signaling events induced by IFN via CXCL10 ligand is associated with a MyD88-dependent pathway in mouse ex vivo infected macrophages and fibroblast cells [85]. In other instances, impaired CXCL10 production leads to susceptibility to infection. For instance, impaired CXCL10 production led to susceptibility to Leginella pneumophila infection [79], the levels of CXCL10 were markedly increased in plasma and infected kidney tissues in leptospirosis [86].
3.3. CXCL10 and mycotic infection
Fewer studies on role of CXCL10 in fungal infections have been reported. Fungal infections abrogate CXCL10 expression in human cells [10]. Impaired CXCL10 production contributes to the pathogenesis of cutaneous candidiasis caused by Candida albicans [10] whereas in the case of murine Pneumocystis carinii and Cryptococcus neoformans infections in the brains of immunized mice, CXCL10 seems to be protective [87], [88].
3.4. CXCL10 and protozoan infection
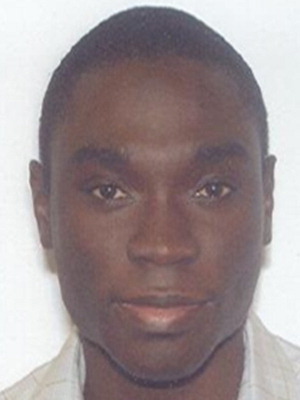
In AIDS-associated cryptosporidiosis patients, increased mucosal CXCL10 levels are consistent with the histopathology in jejunal biopsies, which correlate with parasite burden [74]. Interestingly, CXCL10 helps to eliminate cryptosporidiosis in the presence of immune effector cells, to favor immunopathogenesis in the absence of effector cells in AIDS patients [74]. CXCL10 has been shown to be a novel biomarker for severity of Human African trypanosomiasis (HAT) caused by infection with sub-species of Trypanosoma brucei (T. brucei) [89], Plasmodium falciparum (P. falciparum) and Plasmodium vivax malaria [11], [12], [13], Toxoplasma gondii [90] and Leishmania major [91]. It appears that most of the parasitic diseases of the CNS involve significant alterations of CXCL10 expression in peripheral blood of infected host. In 2003, CXCL10 was first reported to be a host-protective factor in murine experimental malaria (ECM) [92]. CXCL10 expression was expressed early in either cerebral malaria-susceptible or -resistant strains of mice to Plasmodium berghei ANKA infection [93], [94]. More recently, a pioneering study conducted both in India and Ghana, identified CXCL10 as a serum and CSF biomarker associated with increased risk of fatal P. falciparum-mediated cerebral malaria (CM) in humans [11], [12], [13]. Subsequent confirmatory studies in murine ECM revealed that the CXCL10/CXCR3 axis plays a crucial role in CD8+T cell recruitment into the brain and activation of CD8+ T cells to develop murine CM [95]. The study also revealed that CXCR3−/− mice were resistant to CM as a result of a reduction in the number of CD8+ T cells [96]. Adoptive transfer of CD8+ cells abrogated protection of CM in CXCR3−/− mice while CXCL10−/− mice were partially resistant to P. berghei-mediated CM. Notably, only CD8+ cells which were located in microvessels expressed perforin and induced granule exocytosis and cytolysis [96], [97], and activated cytotoxicity by a Fas dependent pathway [96]. Proposed cellular pathway of CXCL10-mediated severe malaria was shown in Fig. 3 . CXCL10 is elevated in association with chills, rigors, anemia [98] and pre-chloroquine/primaquine chemotherapy and disappears after chemotherapy against malaria. Interestingly, HIV infection increases susceptibility to malaria when CXCL10 levels are elevated [99] while filariasis produces resistance to malaria by down-regulating CXCL10 [100]. Recent studies suggest that altered levels of CXCL4 and CXCL10 play a prominent role in pathogenesis of fatal CM associated death and may be used as functional or surrogate biomarkers for predicting CM severity [101]. This remarkable link between increased CXCL10 and severity of parasitic diseases suggest further studies be conducted on the mechanisms involved.
Fig. 3.
Proposed cellular pathway of CXCL10-mediated severe malaria. Endothelial cell, astrocytes and microglia are a prominent source of CXCL10 and CXCL9. (1) Through T cells sequestration [95], [96], [97], [129]. CXCL10 could attract activated T cells and mediate Th1-type response, characterized by the sequestration of monocytes and T cells (mainly CD8+) in cerebral microvessels. Granule exocytosis and Fas/Fas ligand activation pathways are two distinct mechanisms involved in the death of brain endothelial cells by CD8+ lymphocytes. (2) Through NK cell sequestration [130], [131], NK cells mediate direct cytotoxic activity or reconstitution of capacity of T cells to migrate in response to CXCL10 to the CNS. (3) Through upregulation of ICAM-1 on brain microvascular endothelial cells [132], LTα and IFN-γ are required for P. berghei ANKA(PbA)-induced endothelial ICAM-1 up regulation, increased in cytoadherence of sequestration of parasitized RBC (pRBC) to the endothelium of cerebral vessels, resulting in hypoxia, hemorrhage and pathology representing another potential mechanism of CM pathogenesis.
4. Therapeutic applications of CXCL10
The CXCL10–CXCR3 axis represents a potential pharmacologic target for various human diseases such as infectious diseases and cancer, however, current studies on therapeutic uses of CXCL10 therapy have been few. For example, application of anti-CXCL10 antibody decreased the clinical and histological manifestation of experimental autoimmune encephalomyelitis (EAE) [102]. Singh et al. [103] have also demonstrated that targeted blocking of CXCL10 or CXCR3 receptor with antibodies attenuated inflammatory colitis in mice. The crucial point in relation to CXCL10/CXCR3 and colitis pathogenesis is that Th1 cells are differentiated from precursor T cells instead of regulatory T cells (Tr1). Th1 cells expressing CXCL10/CXCR3, recruit polymorphonuclear cells (PMN), NK and NKT cells to specific locations with the aid of antigen-presenting cells to initiate colitis. Regarding malaria Nie et al. [104] found that CXCL10 neutralization either with specific antibodies or genetic deletion (CXCL10−/− mice) protected against cerebral malaria infection and inflammation. Passive transfer of anti-CXCL10 antibodies reduced the recruitment of inflammatory leukocytes across the blood brain barrier. While genetic deletion of CXCL10 not only alleviated intravascular inflammation but also reduced pRBC sequestration in the brain [104]. The increased resistance to parasite infection observed in the absence of CXCL10-mediated trafficking was associated with retention of parasite-specific T cells in the spleen. Very interestingly, various studies recently indicate that statins (Atovastatin) used for lowering blood cholesterol have anti-inflammatory function and may contribute to modulation the immune system [105]. Grip and Janciauskiene [106] in 2009 described a new in vivo function of atovastatin, which reduces plasma levels of CXCL10 in patients with Crohn's Disease (CD), thus provides support for the use of statins in therapy for patients with CD or any other CXCL10-mediated diseases. In contrast, high levels of CXCL10 mediated protection against Leishmania amazonensis infection in mice, delayed lesion development and reduced parasite burden via interferon-γ and IL-12 secretion [107]. The application of CXCL10 has been extended to some other areas. An example is an in vitro study involving kidney allograft rejection, a novel drug BXL-01-0029 was reported to decrease the expression of CXCL10 in human renal tubular cells and thus reduce kidney allograft rejection [108]. More promising is that Lee [109] have generated and patented the antibody against CXCL10 and found that CXCL10 up regulated the expression of receptor activator of NF-κB ligand (RANKL) which plays an important role in the formation of osteoclasts. Blocking CXCL10 using this antibody resulted in the inhibition of RANKL expression, thus, this antibody could be utilized as a novel therapy for preventing and treating human bone diseases. All the above studies indicate that CXCL10 could be targeted therapeutically for treatment of a plethora of infectious diseases that must be pursued. Detailed translational studies on CXCL10 are summarized in Table 1 .
Table 1.
Potential therapeutic implications of CXCL10.
| Type of compound | Type of studies (experimental models) | Biological effects reported | Reference | |
|---|---|---|---|---|
| Anti-CXCL10 mAb | C57BL/6 mice infected with Toxoplasma gondii | In vivo | Inhibits massive influx of T cells into tissues and impairs antigen specific T cell effector functions | [110] |
| C57BL/6 mice infected P. berghei ANKA | In vivo | Reduces the recruitment of inflammatory leukocytes across the blood brain barrier | [104] | |
| Experimental autoimmune encephalomyelitis (EAE) in SJL mice | In vivo | Specifically decreases accumulation of encephalitogenic PLP139–151 Ag-specific CD4+T cells | [102] | |
| Murine inflammatory bowel disease | In vivo | Attenuates Th1 mediated inflammatory colitis | [103] | |
| Murine AIDS (MAIDS) colitis | In vivo | Blocks cellular trafficking and protects intestinal epithelial cells, attenuate chronic experimental colitis | [111] | |
| Transgenic mice infected with lymphocytic choriomeningitis virus (LCMV)-type 1 diabetes model | In vivo | Impedes expansion of peripheral Ag-specific T cells and hinders their migration into the pancreas | [112] | |
| C57 BL/6 Wild type, RAG-null, CXCR−/− mice | In vivo | Reduces Th1-cell mediated lung injury and inflammation | [113] | |
| Animal models of inflammation | In vivo | Antagonizes CXCL10 mediated chemotaxis in vitro and in vivo, causes a therapeutic benefit in multiple mouse models of inflammatory disease | ||
| HUVEC | In vitro | Restores vessel formation | [114] | |
| C57BL/6 mice with spinal cord injury (SCI) | In vivo | Reduces T-lymphocyte invasion and inflammation, reduces apoptosis, neuronal loss and whole tissue loss, promotes angiogenesis and revascularization, enhances tissue sparing, increases axon sprouting, reduces secondary degeneration after SCI | [115], [116], [117], [118] | |
| CXCL10 antagonist (truncated CXCL10 at the N-terminal) | Autoimmune sialadenitis in MRL/lpr mice | In vivo | Fails to induce chemotaxis and calcium influx by CXCR3-expressing cells, reduces infiltration of CXCR3+ T cells | [119] |
| DNA plasmid encoding recombinant immunotoxin DT390-CXCL10 | EAE in C57BL/6 mice | In vivo | Eliminates CXCR3+ autoimmune T cells, attenuate EAE | [120] |
| DNA plasmid encoding CXCL10 | Non-obese diabetic (NOD) mice with diabetes | In vivo | Produces anti-CXCL10 antibody by CXCL10 DNA vaccination, increases regulatory T cells expressing CXCR3 in local pancreatic regions, reverses diabetes, increases residual beta-cell mass, promotes beta-cell proliferation | [121], [122] |
| Pseudorabies virus (PrV) infected C57 BL/6 mice | In vivo | Induces immune responses of the Th1-type, causes a rebalance of the immunity, protects against a virulent virus infection | [123] | |
| Dentritic cell-based vaccine, cancer immunology | In vivo | Increases anti-tumor vaccine potency | [124] | |
| C57BL/6 and BALB/c mice with lung cancer and hepatocarcinoma | In vivo | Inhibits the proliferation of endothelial cells, induces the apoptosis of tumor cells, and recruits lymphocytes to tumor | [125] | |
| CXCL10 | Organogenesis and wound repair models using human dermal micro vascular endothelial cells (HMEC-1), adult dermal microvascular (dHMEC), human Lung microvascular (hLMEC) and human umbilical vein endothelial cells (HUVEC), as well as C57BL/6 wild type and CXCR3−/− mice | In vitro In vivo | Blocks VEGF induced endothelial cell migration and tube formation, through a PKA mediated inhibition of m-calpain, limits new vessel growth; triggers μ-calpain, which cleaves the tail of the β3 integrin, leading to endothelial cell dissociation and cell death; activates caspase 3, induces vessel regression | [126], [127] |
| Chimeric ITIP (substituting N-terminal and N-loop of CXCL10 with CXCL11) | BALB/c (H-2d) and C57BL/6 (H-2d) colon, mammary, lung carcinoma | In vivo | A synergistic antitumor effect by CXCL11 moiety induces CXCR3+ cells chemotaxis and CXCL10 moiety mediates anti-angiogenesis | [128] |
5. Conclusion
Although CXCL10 was originally identified as a proinflammatory chemokine mediating leukocyte trafficking, it has been found to activate T lymphocytes (Th1) [5], NK cells, macrophages, dendritic and B cells. All of these cells home in on target/threat areas via CXCL10 to modulate innate and adaptive immune responses and regulate cell growth and angiostasis. Alterations in CXCL10 mRNA and protein expression have been associated with pathogenesis of various infectious diseases, chronic inflammatory and autoimmune diseases as well as cancer. The molecular characteristics of CXCL10 make it a potential candidate for therapies against the pathological consequences of these diseases. Further research is needed to understand the downstream and upstream signaling pathways regulating CXCL10 and other CXCR3 receptor ligands, with the aim of developing a class of novel interventions against infectious diseases mediated by this chemokine.
Conflict of interest
None.
Acknowledgements
This work was supported by the National Institutes of Health grant numbers NIH-FIC (1T90-HG004151-01) for postdoctoral training in Genomics and Hemoglobinopathies, NIH/FIC/NINDS R21 and NIH-RCMI (RR033062). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The support of the Center for Disease Diagnosis and Research (CDDR) in Ghana is acknowledged.
Biographies

Mingli Liu obtained her medical degree from Peking University School of Medicine with a specialization in Hematology. She obtained her Ph.D. degree from Chinese Academy of Medical Sciences. She is currently working on the pathogenesis of severe malaria and sickle cell disease which results from a natural selection process in response to the high prevalence of malaria.
Shanchun Guo received his PhD in molecular pathology from Beijing Medical University, postdoctoral training in biochemistry from Tokyo Metropolitan Institute of Gerontology and Molecular Genetics from Fox Chase Cancer Center, Philadelphia. He is currently working as faculty member at Morehouse School of Medicine.

Dr. Jacqueline M. Hibbert's research program is focused on the nutritional and metabolic pathogenesis of sickle cell disease (SCD) with respect to impact, prevention and treatment of nutritional problems. In particular, her lab performs clinical and animal studies to determine how body composition, protein/energy metabolism and immune response are altered by SCD, and studies to test targeted dietary interventions to correct harmful adaptations to SCD.

Dr. Vidhan Jain is working as senior research fellow at Regional medical Research Centre for Tribals, ICMR, Jabalpur, India. He obtained his Ph.D in “Immunopathogenesis of Cerebral Malaria” from Rani Durgavati University Jabalpur, India. His main focus area of research is to explore the link between immunomodulatory cytokines, chemokines, growth factors and severity of cerebral malaria.

Dr. Neeru Singh is the Director of Regional Medical Research Centre for Tribals (RMRCT). She is also the Officer in Charge of the National Institute of Malaria Research (NIMR) Field Station also based in RMRCT, Jabalpur. She is a recipient of WHO/ UNDP fellowship (1990). She is a short term consultant to WHO for malaria diagnostics and Malaria in pregnancy. She is a member of technical working group (TWG) at NIH for Iron and Malaria.
Nana O. Wilson is a Ph.D. student at Morehouse School of Medicine, studying biomedical science. He received a Bachelor of Science degree in biological sciences from Kwame Nkrumah University of Science and Technology, Kumasi, Ghana (2004), and a Master of Public Health degree in international health from Morehouse School of Medicine (2010).

Dr. Jonathan K. Stiles is a Professor of Microbiology in the Department of Microbiology, Biochemistry & Immunology. He has over the last eight years led a multidisciplinary team of scientists in USA, India and Ghana to conduct malaria research with funds from the NIH/Fogarty International Center (FIC). Currently, he serve as Director for the Training in Genomics and Hemoglobinopathies program at Morehouse School of Medicine which provides training in Genomics and sickle cell disease (SCD) research to researchers from the USA and the developing world.
Contributor Information
Mingli Liu, Email: mliu@msm.edu.
Shanchun Guo, Email: sguo@msm.edu.
Jacqueline M. Hibbert, Email: Jhibbert@msm.edu.
Vidhan Jain, Email: vidhanjain78@yahoo.com.
Neeru Singh, Email: neeru.singh@gmail.com.
Nana O. Wilson, Email: nwilson@msm.edu.
Jonathan K. Stiles, Email: jstiles@msm.edu.
References
- 1.Dyer K.D., Percopo C.M., Fischer E.R., Gabryszewski S.J., Rosenberg H.F. Pneumoviruses infect eosinophils and elicit MyD88-dependent release of chemoattractant cytokines and interleukin-6. Blood. 2009;114:2649–2656. doi: 10.1182/blood-2009-01-199497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Luster A.D., Ravetch J.V. Biochemical characterization of a gamma interferon-inducible cytokine (IP-10) J Exp Med. 1987;166:1084–1097. doi: 10.1084/jem.166.4.1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lo B.K., Yu M., Zloty D., Cowan B., Shapiro J., McElwee K.J. CXCR3/ligands are significantly involved in the tumorigenesis of basal cell carcinomas. Am J Pathol. 2010:12. doi: 10.2353/ajpath.2010.081059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Loetscher M., Gerber B., Loetscher P., Jones S.A., Piali L., Clark-Lewis I. Chemokine receptor specific for IP10 and mig: structure, function, and expression in activated T-lymphocytes. J Exp Med. 1996;184:963–969. doi: 10.1084/jem.184.3.963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sallusto F., Lenig D., Mackay C.R., Lanzavecchia A. Flexible programs of chemokine receptor expression on human polarized T helper 1 and 2 lymphocytes. J Exp Med. 1998;187:875–883. doi: 10.1084/jem.187.6.875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haeberle H.A., Kuziel W.A., Dieterich H.J., Casola A., Gatalica Z., Garofalo R.P. Inducible expression of inflammatory chemokines in respiratory syncytial virus-infected mice: role of MIP-1alpha in lung pathology. J Virol. 2001;75:878–890. doi: 10.1128/JVI.75.2.878-890.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tripp R.A., Jones L., Anderson L.J. Respiratory syncytial virus G and/or SH glycoproteins modify CC and CXC chemokine mRNA expression in the BALB/c mouse. J Virol. 2000;74:6227–6229. doi: 10.1128/jvi.74.13.6227-6229.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Azzurri A., Sow O.Y., Amedei A., Bah B., Diallo S., Peri G. IFN-gamma-inducible protein 10 and pentraxin 3 plasma levels are tools for monitoring inflammation and disease activity in Mycobacterium tuberculosis infection. Microbes Infect. 2005;7:1–8. doi: 10.1016/j.micinf.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 9.Lienhardt C., Azzurri A., Amedei A., Fielding K., Sillah J., Sow O.Y. Active tuberculosis in Africa is associated with reduced Th1 and increased Th2 activity in vivo. Eur J Immunol. 2002;32:1605–1613. doi: 10.1002/1521-4141(200206)32:6<1605::AID-IMMU1605>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 10.Shiraki Y., Ishibashi Y., Hiruma M., Nishikawa A., Ikeda S. Candida albicans abrogates the expression of interferon-gamma-inducible protein-10 in human keratinocytes. FEMS Immunol Med Microbiol. 2008;54:122–128. doi: 10.1111/j.1574-695X.2008.00457.x. [DOI] [PubMed] [Google Scholar]
- 11.Armah H.B., Wilson N.O., Sarfo B.Y., Powell M.D., Bond V.C., Anderson W. Cerebrospinal fluid and serum biomarkers of cerebral malaria mortality in Ghanaian children. Malar J. 2007;6:147. doi: 10.1186/1475-2875-6-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jain V., Armah H.B., Tongren J.E., Ned R.M., Wilson N.O., Crawford S. Plasma IP-10, apoptotic and angiogenic factors associated with fatal cerebral malaria in India. Malar J. 2008;7:83. doi: 10.1186/1475-2875-7-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wilson N.O., Huang M.B., Anderson W., Bond V., Powell M., Thompson W.E. Soluble factors from Plasmodium falciparum-infected erythrocytes induce apoptosis in human brain vascular endothelial and neuroglia cells. Mol Biochem Parasitol. 2008;162:172–176. doi: 10.1016/j.molbiopara.2008.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Luster A.D., Unkeless J.C., Ravetch J.V. Gamma-interferon transcriptionally regulates an early-response gene containing homology to platelet proteins. Nature. 1985;315:672–676. doi: 10.1038/315672a0. [DOI] [PubMed] [Google Scholar]
- 15.Luster A.D., Jhanwar S.C., Chaganti R.S., Kersey J.H., Ravetch J.V. Interferon-inducible gene maps to a chromosomal band associated with a (4;11) translocation in acute leukemia cells. Proc Natl Acad Sci U S A. 1987;84:2868–2871. doi: 10.1073/pnas.84.9.2868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Colvin R.A., Campanella G.S., Sun J., Luster A.D. Intracellular domains of CXCR3 that mediate CXCL9 CXCL10, and CXCL11 function. J Biol Chem. 2004;279:30219–30227. doi: 10.1074/jbc.M403595200. [DOI] [PubMed] [Google Scholar]
- 17.Loetscher M., Loetscher P., Brass N., Meese E., Moser B. Lymphocyte-specific chemokine receptor CXCR3: regulation, chemokine binding and gene localization. Eur J Immunol. 1998;28:3696–3705. doi: 10.1002/(SICI)1521-4141(199811)28:11<3696::AID-IMMU3696>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 18.Neville L.F., Mathiak G., Bagasra O. The immunobiology of interferon-gamma inducible protein 10 kDa (IP-10): a novel, pleiotropic member of the C–X–C chemokine superfamily. Cytokine Growth Factor Rev. 1997;8:207–219. doi: 10.1016/s1359-6101(97)00015-4. [DOI] [PubMed] [Google Scholar]
- 19.Romagnani S. The Th1/Th2 paradigm. Immunol Today. 1997;18:263–266. doi: 10.1016/s0167-5699(97)80019-9. [DOI] [PubMed] [Google Scholar]
- 20.Campbell J.D., Gangur V., Simons F.E., HayGlass K.T. Allergic humans are hyporesponsive to a CXCR3 ligand-mediated Th1 immunity-promoting loop. FASEB J. 2004;18:329–331. doi: 10.1096/fj.02-0908fje. [DOI] [PubMed] [Google Scholar]
- 21.Enderlin M., Kleinmann E.V., Struyf S., Buracchi C., Vecchi A., Kinscherf R. TNF-alpha and the IFN-gamma-inducible protein 10 (IP-10/CXCL-10) delivered by parvoviral vectors act in synergy to induce antitumor effects in mouse glioblastoma. Cancer Gene Ther. 2009;16:149–160. doi: 10.1038/cgt.2008.62. [DOI] [PubMed] [Google Scholar]
- 22.Liu L., Callahan M.K., Huang D., Ransohoff R.M. Chemokine receptor CXCR3: an unexpected enigma. Curr Top Dev Biol. 2005;68:149–181. doi: 10.1016/S0070-2153(05)68006-4. [DOI] [PubMed] [Google Scholar]
- 23.Sui Y., Potula R., Dhillon N., Pinson D., Li S., Nath A. Neuronal apoptosis is mediated by CXCL10 overexpression in simian human immunodeficiency virus encephalitis. Am J Pathol. 2004;164:1557–1566. doi: 10.1016/S0002-9440(10)63714-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sui Y., Stehno-Bittel L., Li S., Loganathan R., Dhillon N.K., Pinson D. CXCL10-induced cell death in neurons: role of calcium dysregulation. Eur J Neurosci. 2006;23:957–964. doi: 10.1111/j.1460-9568.2006.04631.x. [DOI] [PubMed] [Google Scholar]
- 25.Klein R.S., Izikson L., Means T., Gibson H.D., Lin E., Sobel R.A. IFN-inducible protein 10/CXC chemokine ligand 10-independent induction of experimental autoimmune encephalomyelitis. J Immunol. 2004;172:550–559. doi: 10.4049/jimmunol.172.1.550. [DOI] [PubMed] [Google Scholar]
- 26.Zhang B., Patel J., Croyle M., Diamond M.S., Klein R.S. TNF-alpha-dependent regulation of CXCR3 expression modulates neuronal survival during West Nile virus encephalitis. J Neuroimmunol. 2010;224:28–38. doi: 10.1016/j.jneuroim.2010.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yang L.L., Ping C., Luo S., Li J., Liu K., Hu H.Z. CXCL10 gene therapy efficiently inhibited the growth of cervical carcinoma based on the antiangiogenic and antiviral activity. Biotechnol Appl Biochem. 2009;3:3. doi: 10.1042/BA20090012. [DOI] [PubMed] [Google Scholar]
- 28.Li H., Yi T., Zhao S., Chen P., Cheng C., Wei Y. The anti-condyloma acuminatum effects of interferon-inducible protein 10 in vitro. Int J Dermatol. 2009;48:136–141. doi: 10.1111/j.1365-4632.2009.03776.x. [DOI] [PubMed] [Google Scholar]
- 29.Rice D., Barone S., Jr. Critical periods of vulnerability for the developing nervous system: evidence from humans and animal models. Environ Health Perspect. 2000;108(Suppl 3):511–533. doi: 10.1289/ehp.00108s3511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vinet J., de Jong E.K., Boddeke H.W., Stanulovic V., Brouwer N., Granic I. Expression of CXCL10 in cultured cortical neurons. J Neurochem. 2009;112:703–714. doi: 10.1111/j.1471-4159.2009.06495.x. [DOI] [PubMed] [Google Scholar]
- 31.Giuliani N., Bonomini S., Romagnani P., Lazzaretti M., Morandi F., Colla S. CXCR3 and its binding chemokines in myeloma cells: expression of isoforms and potential relationships with myeloma cell proliferation and survival. Haematologica. 2006;91:1489–1497. [PubMed] [Google Scholar]
- 32.Feldman E.D., Weinreich D.M., Carroll N.M., Burness M.L., Feldman A.L., Turner E. Interferon gamma-inducible protein 10 selectively inhibits proliferation and induces apoptosis in endothelial cells. Ann Surg Oncol. 2006;13:125–133. doi: 10.1245/ASO.2006.03.038. [DOI] [PubMed] [Google Scholar]
- 33.Aksoy M.O., Yang Y., Ji R., Reddy P.J., Shahabuddin S., Litvin J. CXCR3 surface expression in human airway epithelial cells: cell cycle dependence and effect on cell proliferation. Am J Physiol Lung Cell Mol Physiol. 2006;290:L909–918. doi: 10.1152/ajplung.00430.2005. [DOI] [PubMed] [Google Scholar]
- 34.Ji R., Lee C.M., Gonzales L.W., Yang Y., Aksoy M.O., Wang P. Human type II pneumocyte chemotactic responses to CXCR3 activation are mediated by splice variant A. Am J Physiol Lung Cell Mol Physiol. 2008;294:L1187–1196. doi: 10.1152/ajplung.00388.2007. [DOI] [PubMed] [Google Scholar]
- 35.Maru S.V., Holloway K.A., Flynn G., Lancashire C.L., Loughlin A.J., Male D.K. Chemokine production and chemokine receptor expression by human glioma cells: role of CXCL10 in tumour cell proliferation. J Neuroimmunol. 2008;199:35–45. doi: 10.1016/j.jneuroim.2008.04.029. [DOI] [PubMed] [Google Scholar]
- 36.Shen Q., Zhang R., Bhat N.R. MAP kinase regulation of IP10/CXCL10 chemokine gene expression in microglial cells. Brain Res. 2006;1086:9–16. doi: 10.1016/j.brainres.2006.02.116. [DOI] [PubMed] [Google Scholar]
- 37.Datta D., Flaxenburg J.A., Laxmanan S., Geehan C., Grimm M., Waaga-Gasser A.M. Ras-induced modulation of CXCL10 and its receptor splice variant CXCR3-B in MDA-MB-435 and MCF-7 cells: relevance for the development of human breast cancer. Cancer Res. 2006;66:9509–9518. doi: 10.1158/0008-5472.CAN-05-4345. [DOI] [PubMed] [Google Scholar]
- 38.Riemer C., Schultz J., Burwinkel M., Schwarz A., Mok S.W., Gultner S. Accelerated prion replication in, but prolonged survival times of, prion-infected CXCR3−/− mice. J Virol. 2008;82:12464–12471. doi: 10.1128/JVI.01371-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kim S., Bakre M., Yin H., Varner J.A. Inhibition of endothelial cell survival and angiogenesis by protein kinase A. J Clin Invest. 2002;110:933–941. doi: 10.1172/JCI14268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sato E., Fujimoto J., Tamaya T. Expression of interferon-gamma-inducible protein 10 related to angiogenesis in uterine endometrial cancers. Oncology. 2007;73:246–251. doi: 10.1159/000127422. [DOI] [PubMed] [Google Scholar]
- 41.Aronica S.M., Raiber L., Hanzly M., Kisela C. Antitumor/antiestrogenic effect of the chemokine interferon inducible protein 10 (IP-10) involves suppression of VEGF expression in mammary tissue. J Interferon Cytokine Res. 2009;29:83–92. doi: 10.1089/jir.2008.0034. [DOI] [PubMed] [Google Scholar]
- 42.Aronica S.M., Fanti P., Kaminskaya K., Gibbs K., Raiber L., Nazareth M. Estrogen disrupts chemokine-mediated chemokine release from mammary cells: implications for the interplay between estrogen and IP-10 in the regulation of mammary tumor formation. Breast Cancer Res Treat. 2004;84:235–245. doi: 10.1023/B:BREA.0000019961.59306.f6. [DOI] [PubMed] [Google Scholar]
- 43.Jiang Z., Xu Y., Cai S. CXCL10 expression and prognostic significance in stage II and III colorectal cancer. Mol Biol Rep. 2009;10:10. doi: 10.1007/s11033-009-9873-z. [DOI] [PubMed] [Google Scholar]
- 44.Romagnani P., Lasagni L., Annunziato F., Serio M., Romagnani S. CXC chemokines: the regulatory link between inflammation and angiogenesis. Trends Immunol. 2004;25:201–209. doi: 10.1016/j.it.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 45.Angiolillo A.L., Sgadari C., Taub D.D., Liao F., Farber J.M., Maheshwari S. Human interferon-inducible protein 10 is a potent inhibitor of angiogenesis in vivo. J Exp Med. 1995;182:155–162. doi: 10.1084/jem.182.1.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Persano L., Crescenzi M., Indraccolo S. Anti-angiogenic gene therapy of cancer: current status and future prospects. Mol Aspects Med. 2007;28:87–114. doi: 10.1016/j.mam.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 47.Belperio J.A., Keane M.P., Arenberg D.A., Addison C.L., Ehlert J.E., Burdick M.D. CXC chemokines in angiogenesis. J Leukoc Biol. 2000;68:1–8. [PubMed] [Google Scholar]
- 48.Shahabuddin S., Ji R., Wang P., Brailoiu E., Dun N., Yang Y. CXCR3 chemokine receptor-induced chemotaxis in human airway epithelial cells: role of p38 MAPK and PI3K signaling pathways. Am J Physiol Cell Physiol. 2006;291:C34–C39. doi: 10.1152/ajpcell.00441.2005. [DOI] [PubMed] [Google Scholar]
- 49.Jinquan T., Jing C., Jacobi H.H., Reimert C.M., Millner A., Quan S. CXCR3 expression and activation of eosinophils: role of IFN-gamma-inducible protein-10 and monokine induced by IFN-gamma. J Immunol. 2000;165:1548–1556. doi: 10.4049/jimmunol.165.3.1548. [DOI] [PubMed] [Google Scholar]
- 50.Bonacchi A., Romagnani P., Romanelli R.G., Efsen E., Annunziato F., Lasagni L. Signal transduction by the chemokine receptor CXCR3: activation of Ras/ERK Src, and phosphatidylinositol 3-kinase/Akt controls cell migration and proliferation in human vascular pericytes. J Biol Chem. 2001;276:9945–9954. doi: 10.1074/jbc.M010303200. [DOI] [PubMed] [Google Scholar]
- 51.Williams R., Yao H., Dhillon N.K., Buch S.J. HIV-1 Tat co-operates with IFN-gamma and TNF-alpha to increase CXCL10 in human astrocytes. PLoS One. 2009;4:e5709. doi: 10.1371/journal.pone.0005709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mendez-Samperio P., Perez A., Rivera L. Mycobacterium bovis Bacillus Calmette-Guerin (BCG)-induced activation of PI3K/Akt and NF-κB signaling pathways regulates expression of CXCL10 in epithelial cells. Cell Immunol. 2009;256:12–18. doi: 10.1016/j.cellimm.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 53.Han C., Fu J., Liu Z., Huang H., Luo L., Yin Z. Dipyrithione inhibits IFN-gamma-induced JAK/STAT1 signaling pathway activation and IP-10/CXCL10 expression in RAW264.7 cells. Inflamm Res. 2010;7 doi: 10.1007/s00011-010-0192-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nakamichi K., Inoue S., Takasaki T., Morimoto K., Kurane I. Rabies virus stimulates nitric oxide production and CXC chemokine ligand 10 expression in macrophages through activation of extracellular signal-regulated kinases 1 and 2. J Virol. 2004;78:9376–9388. doi: 10.1128/JVI.78.17.9376-9388.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nakamichi K., Saiki M., Sawada M., Takayama-Ito M., Yamamuro Y., Morimoto K. Rabies virus-induced activation of mitogen-activated protein kinase and NF-kappaB signaling pathways regulates expression of CXC and CC chemokine ligands in microglia. J Virol. 2005;79:11801–11812. doi: 10.1128/JVI.79.18.11801-11812.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Schneider D., Ganesan S., Comstock A.T., Meldrum C.A., Mahidhara R., Goldsmith A.M. Increased cytokine response of rhinovirus-infected airway epithelial cells in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2010;15 doi: 10.1164/rccm.200911-1673OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mihm S., Schweyer S., Ramadori G. Expression of the chemokine IP-10 correlates with the accumulation of hepatic IFN-gamma and IL-18 mRNA in chronic hepatitis C but not in hepatitis B. J Med Virol. 2003;70:562–570. doi: 10.1002/jmv.10431. [DOI] [PubMed] [Google Scholar]
- 58.Mahanty S., Gupta M., Paragas J., Bray M., Ahmed R., Rollin P.E. Protection from lethal infection is determined by innate immune responses in a mouse model of Ebola virus infection. Virology. 2003;312:415–424. doi: 10.1016/s0042-6822(03)00233-2. [DOI] [PubMed] [Google Scholar]
- 59.Nightingale Z.D., Patkar C., Rothman A.L. Viral replication and paracrine effects result in distinct, functional responses of dendritic cells following infection with dengue 2 virus. J Leukoc Biol. 2008;84:1028–1038. doi: 10.1189/jlb.0208105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Warke R.V., Becerra A., Zawadzka A., Schmidt D.J., Martin K.J., Giaya K. Efficient dengue virus (DENV) infection of human muscle satellite cells upregulates type I interferon response genes and differentially modulates MHC I expression on bystander and DENV-infected cells. J Gen Virol. 2008;89:1605–1615. doi: 10.1099/vir.0.2008/000968-0. [DOI] [PubMed] [Google Scholar]
- 61.Covaleda L., Fuller F.J., Payne S.L. EIAV S2 enhances pro-inflammatory cytokine and chemokine response in infected macrophages. Virology. 2009;397:217–223. doi: 10.1016/j.virol.2009.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Deng G., Zhou G., Zhang R., Zhai Y., Zhao W., Yan Z. Regulatory polymorphisms in the promoter of CXCL10 gene and disease progression in male hepatitis B virus carriers. Gastroenterology. 2008;134:716–726. doi: 10.1053/j.gastro.2007.12.044. [DOI] [PubMed] [Google Scholar]
- 63.Chen J., Subbarao K. The immunobiology of SARS*. Annu Rev Immunol. 2007;25:443–472. doi: 10.1146/annurev.immunol.25.022106.141706. [DOI] [PubMed] [Google Scholar]
- 64.Hsieh Y.H., Chen C.W., Schmitz S.F., King C.C., Chen W.J., Wu Y.C. Candidate genes associated with susceptibility for SARS-coronavirus. Bull Math Biol. 2009;72:122–132. doi: 10.1007/s11538-009-9440-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sgadari C., Angiolillo A.L., Cherney B.W., Pike S.E., Farber J.M., Koniaris L.G. Interferon-inducible protein-10 identified as a mediator of tumor necrosis in vivo. Proc Natl Acad Sci U S A. 1996;93:13791–13796. doi: 10.1073/pnas.93.24.13791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sin J., Kim J.J., Pachuk C., Satishchandran C., Weiner D.B. DNA vaccines encoding interleukin-8 and RANTES enhance antigen-specific Th1-type CD4(+) T-cell-mediated protective immunity against herpes simplex virus type 2 in vivo. J Virol. 2000;74:11173–11180. doi: 10.1128/jvi.74.23.11173-11180.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lane B.R., King S.R., Bock P.J., Strieter R.M., Coffey M.J., Markovitz D.M. The C–X–C chemokine IP-10 stimulates HIV-1 replication. Virology. 2003;307:122–134. doi: 10.1016/s0042-6822(02)00045-4. [DOI] [PubMed] [Google Scholar]
- 68.Lam C.W., Chan M.H., Wong C.K. Severe acute respiratory syndrome: clinical and laboratory manifestations. Clin Biochem Rev. 2004;25:121–132. [PMC free article] [PubMed] [Google Scholar]
- 69.Peterson K.E., Robertson S.J., Portis J.L., Chesebro B. Differences in cytokine and chemokine responses during neurological disease induced by polytropic murine retroviruses Map to separate regions of the viral envelope gene. J Virol. 2001;75:2848–2856. doi: 10.1128/JVI.75.6.2848-2856.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wong C.K., Lam C.W., Wu A.K., Ip W.K., Lee N.L., Chan I.H. Plasma inflammatory cytokines and chemokines in severe acute respiratory syndrome. Clin Exp Immunol. 2004;136:95–103. doi: 10.1111/j.1365-2249.2004.02415.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Stylianou E., Aukrust P., Bendtzen K., Muller F., Froland S.S. Interferons and interferon (IFN)-inducible protein 10 during highly active anti-retroviral therapy (HAART)-possible immunosuppressive role of IFN-alpha in HIV infection. Clin Exp Immunol. 2000;119:479–485. doi: 10.1046/j.1365-2249.2000.01144.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Roe B., Coughlan S., Hassan J., Grogan A., Farrell G., Norris S. Elevated serum levels of interferon-gamma-inducible protein-10 in patients coinfected with hepatitis C virus and HIV. J Infect Dis. 2007;196:1053–1057. doi: 10.1086/520935. [DOI] [PubMed] [Google Scholar]
- 73.Lagging M., Romero A.I., Westin J., Norkrans G., Dhillon A.P., Pawlotsky J.M. IP-10 predicts viral response and therapeutic outcome in difficult-to-treat patients with HCV genotype 1 infection. Hepatology. 2006;44:1617–1625. doi: 10.1002/hep.21407. [DOI] [PubMed] [Google Scholar]
- 74.Wang H.C., Dann S.M., Okhuysen P.C., Lewis D.E., Chappell C.L., Adler D.G. High levels of CXCL10 are produced by intestinal epithelial cells in AIDS patients with active cryptosporidiosis but not after reconstitution of immunity. Infect Immun. 2007;75:481–487. doi: 10.1128/IAI.01237-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Eck M., Schmausser B., Scheller K., Toksoy A., Kraus M., Menzel T. CXC chemokines Gro(alpha)/IL-8 and IP-10/MIG in Helicobacter pylori gastritis. Clin Exp Immunol. 2000;122:192–199. doi: 10.1046/j.1365-2249.2000.01374.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Salvatore C.M., Techasaensiri C., Tagliabue C., Katz K., Leos N., Gomez A.M. Tigecycline therapy significantly reduces the concentrations of inflammatory pulmonary cytokines and chemokines in a murine model of Mycoplasma pneumoniae pneumonia. Antimicrob Agents Chemother. 2009;53:1546–1551. doi: 10.1128/AAC.00979-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kabashima H., Yoneda M., Nagata K., Hirofuji T., Maeda K. The presence of chemokine (MCP-1, MIP-1alpha, MIP-1beta, IP-10, RANTES)-positive cells and chemokine receptor (CCR5 CXCR3)-positive cells in inflamed human gingival tissues. Cytokine. 2002;20:70–77. doi: 10.1006/cyto.2002.1985. [DOI] [PubMed] [Google Scholar]
- 78.de Fost M., Chierakul W., Pimda K., Dondorp A.M., White N.J., Van der Poll T. Activation of cytotoxic lymphocytes in patients with scrub typhus. Am J Trop Med Hyg. 2005;72:465–467. [PubMed] [Google Scholar]
- 79.Lettinga K.D., Weijer S., Speelman P., Prins J.M., Van Der Poll T., Verbon A. Reduced interferon-gamma release in patients recovered from Legionnaires’ disease. Thorax. 2003;58:63–67. doi: 10.1136/thorax.58.1.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Dheda K., Van-Zyl Smit R.N., Sechi L.A., Badri M., Meldau R., Symons G. Clinical diagnostic utility of IP-10 and LAM antigen levels for the diagnosis of tuberculous pleural effusions in a high burden setting. PLoS One. 2009;4:e4689. doi: 10.1371/journal.pone.0004689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ruhwald M., Bjerregaard-Andersen M., Rabna P., Eugen-Olsen J., Ravn P. IP-10, MCP-1, MCP-2 MCP-3, and IL-1RA hold promise as biomarkers for infection with M. tuberculosis in a whole blood based T-cell assay. BMC Res Notes. 2009;2:19. doi: 10.1186/1756-0500-2-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ruhwald M., Bjerregaard-Andersen M., Rabna P., Kofoed K., Eugen-Olsen J., Ravn P. CXCL10/IP-10 release is induced by incubation of whole blood from tuberculosis patients with ESAT-6 CFP10 and TB7.7. Microbes Infect. 2007;9:806–812. doi: 10.1016/j.micinf.2007.02.021. [DOI] [PubMed] [Google Scholar]
- 83.Lighter J., Rigaud M., Huie M., Peng C.H., Pollack H., Chemokine IP-10: an adjunct marker for latent tuberculosis infection in children. Int J Tuberc Lung Dis. 2009;13:731–736. [PubMed] [Google Scholar]
- 84.Tang N.L., Fan H.P., Chang K.C., Ching J.K., Kong K.P., Yew W.W. Genetic association between a chemokine gene CXCL-10 (IP-10, interferon gamma inducible protein 10) and susceptibility to tuberculosis. Clin Chim Acta. 2009;406:98–102. doi: 10.1016/j.cca.2009.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Nagarajan U.M., Ojcius D.M., Stahl L., Rank R.G., Darville T. Chlamydia trachomatis induces expression of IFN-gamma-inducible protein 10 and IFN-beta independent of TLR2 and TLR4, but largely dependent on MyD88. J Immunol. 2005;175:450–460. doi: 10.4049/jimmunol.175.1.450. [DOI] [PubMed] [Google Scholar]
- 86.Lowanitchapat A., Payungporn S., Sereemaspun A., Ekpo P., Phulsuksombati D., Poovorawan Y. Expression of TNF-alpha, TGF-beta IP-10 and IL-10 mRNA in kidneys of hamsters infected with pathogenic Leptospira. Comp Immunol Microbiol Infect Dis. 2009;25:25. doi: 10.1016/j.cimid.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 87.Uicker W.C., Doyle H.A., McCracken J.P., Langlois M., Buchanan K.L. Cytokine and chemokine expression in the central nervous system associated with protective cell-mediated immunity against Cryptococcus neoformans. Med Mycol. 2005;43:27–38. doi: 10.1080/13693780410001731510. [DOI] [PubMed] [Google Scholar]
- 88.Rudner X.L., Happel K.I., Young E.A., Shellito J.E. Interleukin-23 (IL-23)–IL-17 cytokine axis in murine Pneumocystis carinii infection. Infect Immun. 2007;75:3055–3061. doi: 10.1128/IAI.01329-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Amin D.N., Ngoyi D.M., Nhkwachi G.M., Palomba M., Rottenberg M., Buscher P. Identification of stage biomarkers for human African trypanosomiasis. Am J Trop Med Hyg. 2010;82:983–990. doi: 10.4269/ajtmh.2010.09-0770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Norose K., Kikumura A., Luster A.D., Hunter C.A., Harris T.H. CXCL10 is required to maintain T cell populations and control parasite replication during chronic ocular toxoplasmosis. Invest Ophthalmol Vis Sci. 2010 doi: 10.1167/iovs.10-5819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Vasquez R.E., Xin L., Soong L. Effects of CXCL10 on dendritic cell and CD4+ T-cell functions during Leishmania amazonensis infection. Infect Immun. 2008;76:161–169. doi: 10.1128/IAI.00825-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Hunt N.H., Grau G.E. Cytokines: accelerators and brakes in the pathogenesis of cerebral malaria. Trends Immunol. 2003;24:491–499. doi: 10.1016/s1471-4906(03)00229-1. [DOI] [PubMed] [Google Scholar]
- 93.Hanum P.S., Hayano M., Kojima S. Cytokine and chemokine responses in a cerebral malaria-susceptible or -resistant strain of mice to Plasmodium berghei ANKA infection: early chemokine expression in the brain. Int Immunol. 2003;15:633–640. doi: 10.1093/intimm/dxg065. [DOI] [PubMed] [Google Scholar]
- 94.Chen L., Sendo F. Cytokine and chemokine mRNA expression in neutrophils from CBA/NSlc mice infected with Plasmodium berghei ANKA that induces experimental cerebral malaria. Parasitol Int. 2001;50:139–143. doi: 10.1016/s1383-5769(01)00063-0. [DOI] [PubMed] [Google Scholar]
- 95.Campanella G.S., Tager A.M., El Khoury J.K., Thomas S.Y., Abrazinski T.A., Manice L.A. Chemokine receptor CXCR3 and its ligands CXCL9 and CXCL10 are required for the development of murine cerebral malaria. Proc Natl Acad Sci U S A. 2008;105:4814–4819. doi: 10.1073/pnas.0801544105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Miu J., Mitchell A.J., Muller M., Carter S.L., Manders P.M., McQuillan J.A. Chemokine gene expression during fatal murine cerebral malaria and protection due to CXCR3 deficiency. J Immunol. 2008;180:1217–1230. doi: 10.4049/jimmunol.180.2.1217. [DOI] [PubMed] [Google Scholar]
- 97.Nitcheu J., Bonduelle O., Combadiere C., Tefit M., Seilhean D., Mazier D. Perforin-dependent brain-infiltrating cytotoxic CD8+ T lymphocytes mediate experimental cerebral malaria pathogenesis. J Immunol. 2003;170:2221–2228. doi: 10.4049/jimmunol.170.4.2221. [DOI] [PubMed] [Google Scholar]
- 98.Jain V., Singh P.P., Silawat N., Patel R., Saxena A., Bharti P.K. A preliminary study on pro- and anti-inflammatory cytokine profiles in Plasmodium vivax malaria patients from central zone of India. Acta Trop. 2009;113:263–268. doi: 10.1016/j.actatropica.2009.11.009. [DOI] [PubMed] [Google Scholar]
- 99.Chaisavaneeyakorn S., Moore J.M., Otieno J., Chaiyaroj S.C., Perkins D.J., Shi Y.P. Immunity to placental malaria III. Impairment of interleukin (IL)-12, not IL-18, and interferon-inducible protein-10 responses in the placental intervillous blood of human immunodeficiency virus/malaria-coinfected women. J Infect Dis. 2002;185:127–131. doi: 10.1086/338013. [DOI] [PubMed] [Google Scholar]
- 100.Metenou S., Dembele B., Konate S., Dolo H., Coulibaly S.Y., Coulibaly Y.I. Patent filarial infection modulates malaria-specific type 1 cytokine responses in an IL-10-dependent manner in a filaria/malaria-coinfected population. J Immunol. 2009;183:916–924. doi: 10.4049/jimmunol.0900257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Wilson N.O., Jain V., Roberts C.E., Lucchi N., Joel P.K., Singh M.P. CXCL4 and CXCL10 predict risk of fatal cerebral malaria. Dis Markers. 2011;30:39–49. doi: 10.3233/DMA-2011-0763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Fife B.T., Kennedy K.J., Paniagua M.C., Lukacs N.W., Kunkel S.L., Luster A.D. CXCL10 (IFN-gamma-inducible protein-10) control of encephalitogenic CD4+ T cell accumulation in the central nervous system during experimental autoimmune encephalomyelitis. J Immunol. 2001;166:7617–7624. doi: 10.4049/jimmunol.166.12.7617. [DOI] [PubMed] [Google Scholar]
- 103.Singh U.P., Venkataraman C., Singh R., Lillard J.W., Jr CXCR3 axis: role in inflammatory bowel disease and its therapeutic implication. Endocr Metab Immune Disord Drug Targets. 2007;7:111–123. doi: 10.2174/187153007780832109. [DOI] [PubMed] [Google Scholar]
- 104.Nie C.Q., Bernard N.J., Norman M.U., Amante F.H., Lundie R.J., Crabb B.S. IP-10-mediated T cell homing promotes cerebral inflammation over splenic immunity to malaria infection. PLoS Pathog. 2009;5:e1000369. doi: 10.1371/journal.ppat.1000369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Jain M.K., Ridker P.M. Anti-inflammatory effects of statins: clinical evidence and basic mechanisms. Nat Rev Drug Discov. 2005;4:977–987. doi: 10.1038/nrd1901. [DOI] [PubMed] [Google Scholar]
- 106.Grip O., Janciauskiene S. Atorvastatin reduces plasma levels of chemokine (CXCL10) in patients with Crohn's disease. PLoS One. 2009;4:e5263. doi: 10.1371/journal.pone.0005263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Vasquez R.E., Soong L. CXCL10/gamma interferon-inducible protein 10-mediated protection against Leishmania amazonensis infection in mice. Infect Immun. 2006;74:6769–6777. doi: 10.1128/IAI.01073-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Sagrinati C., Sottili M., Mazzinghi B., Borgogni E., Adorini L., Serio M. Comparison between VDR analogs and current immunosuppressive drugs in relation to CXCL10 secretion by human renal tubular cells. Transpl Int. 2010;23:914–923. doi: 10.1111/j.1432-2277.2010.01078.x. [DOI] [PubMed] [Google Scholar]
- 109.Lee E. Patent application number: 20100021463 http://wwwfaqsorg/patents/app/20100021463#ixzz0wjHObVXs.
- 110.Khan I.A., MacLean J.A., Lee F.S., Casciotti L., DeHaan E., Schwartzman J.D. IP-10 is critical for effector T cell trafficking and host survival in Toxoplasma gondii infection. Immunity. 2000;12:483–494. doi: 10.1016/s1074-7613(00)80200-9. [DOI] [PubMed] [Google Scholar]
- 111.Suzuki K., Kawauchi Y., Palaniyandi S.S., Veeraveedu P.T., Fujii M., Yamagiwa S. Blockade of interferon-gamma-inducible protein-10 attenuates chronic experimental colitis by blocking cellular trafficking and protecting intestinal epithelial cells. Pathol Int. 2007;57:413–420. doi: 10.1111/j.1440-1827.2007.02117.x. [DOI] [PubMed] [Google Scholar]
- 112.Christen U., McGavern D.B., Luster A.D., von Herrath M.G., Oldstone M.B. Among CXCR3 chemokines, IFN-gamma-inducible protein of 10 kDa (CXC chemokine ligand (CXCL) 10) but not monokine induced by IFN-gamma (CXCL9) imprints a pattern for the subsequent development of autoimmune disease. J Immunol. 2003;171:6838–6845. doi: 10.4049/jimmunol.171.12.6838. [DOI] [PubMed] [Google Scholar]
- 113.Manicone A.M., Burkhart K.M., Lu B., Clark J.G. CXCR3 ligands contribute to Th1-induced inflammation but not to homing of Th1 cells into the lung. Exp Lung Res. 2008;34:391–407. doi: 10.1080/01902140802221987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Taylor K.L., Oates R.K., Grane R., Leaman D.W., Borden E.C., Lindner D.J. IFN-alpha1,8 inhibits tumor-induced angiogenesis in murine angiosarcomas. J Interferon Cytokine Res. 2006;26:353–361. doi: 10.1089/jir.2006.26.353. [DOI] [PubMed] [Google Scholar]
- 115.Glaser J., Gonzalez R., Perreau V.M., Cotman C.W., Keirstead H.S. Neutralization of the chemokine CXCL10 enhances tissue sparing and angiogenesis following spinal cord injury. J Neurosci Res. 2004;77:701–708. doi: 10.1002/jnr.20204. [DOI] [PubMed] [Google Scholar]
- 116.Glaser J., Gonzalez R., Sadr E., Keirstead H.S. Neutralization of the chemokine CXCL10 reduces apoptosis and increases axon sprouting after spinal cord injury. J Neurosci Res. 2006;84:724–734. doi: 10.1002/jnr.20982. [DOI] [PubMed] [Google Scholar]
- 117.Gonzalez R., Glaser J., Liu M.T., Lane T.E., Keirstead H.S. Reducing inflammation decreases secondary degeneration and functional deficit after spinal cord injury. Exp Neurol. 2003;184:456–463. doi: 10.1016/s0014-4886(03)00257-7. [DOI] [PubMed] [Google Scholar]
- 118.Gonzalez R., Hickey M.J., Espinosa J.M., Nistor G., Lane T.E., Keirstead H.S. Therapeutic neutralization of CXCL10 decreases secondary degeneration and functional deficit after spinal cord injury in mice. Regen Med. 2007;2:771–783. doi: 10.2217/17460751.2.5.771. [DOI] [PubMed] [Google Scholar]
- 119.Hasegawa H., Inoue A., Kohno M., Muraoka M., Miyazaki T., Terada M. Antagonist of interferon-inducible protein 10/CXCL10 ameliorates the progression of autoimmune sialadenitis in MRL/lpr mice. Arthritis Rheum. 2006;54:1174–1183. doi: 10.1002/art.21745. [DOI] [PubMed] [Google Scholar]
- 120.Chen W., Li H., Jia Y., Lv M., Li M., Feng P. In vivo administration of plasmid DNA encoding recombinant immunotoxin DT390-IP-10 attenuates experimental autoimmune encephalomyelitis. J Autoimmun. 2007;28:30–40. doi: 10.1016/j.jaut.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 121.Morimoto J., Yoneyama H., Shimada A., Shigihara T., Yamada S., Oikawa Y. CXC chemokine ligand 10 neutralization suppresses the occurrence of diabetes in nonobese diabetic mice through enhanced beta cell proliferation without affecting insulitis. J Immunol. 2004;173:7017–7024. doi: 10.4049/jimmunol.173.11.7017. [DOI] [PubMed] [Google Scholar]
- 122.Oikawa Y., Shimada A., Yamada Y., Okubo Y., Katsuki T., Shigihara T. CXC chemokine ligand 10 DNA vaccination plus complete Freund's adjuvant reverses hyperglycemia in non-obese diabetic mice. Rev Diabet Stud. 2010;7:209–224. doi: 10.1900/RDS.2010.7.209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Yoon H.A., Eo S.K. Differential polarization of immune responses by genetic cotransfer of chemokines changes the protective immunity of DNA vaccine against pseudorabies virus. Immunology. 2007;120:182–191. doi: 10.1111/j.1365-2567.2006.02490.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Kang T.H., Bae H.C., Kim S.H., Seo S.H., Son S.W., Choi E.Y. Modification of dendritic cells with interferon-gamma-inducible protein-10 gene to enhance vaccine potency. J Gene Med. 2009;11:889–898. doi: 10.1002/jgm.1371. [DOI] [PubMed] [Google Scholar]
- 125.Mei K., Wang L., Tian L., Yu J., Zhang Z., Wei Y. Antitumor efficacy of combination of interferon-gamma-inducible protein 10 gene with gemcitabine, a study in murine model. J Exp Clin Cancer Res. 2008;27:63. doi: 10.1186/1756-9966-27-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Bodnar R.J., Yates C.C., Rodgers M.E., Du X., Wells A. IP-10 induces dissociation of newly formed blood vessels. J Cell Sci. 2009;122:2064–2077. doi: 10.1242/jcs.048793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Bodnar R.J., Yates C.C., Wells A. IP-10 blocks vascular endothelial growth factor-induced endothelial cell motility and tube formation via inhibition of calpain. Circ Res. 2006;98:617–625. doi: 10.1161/01.RES.0000209968.66606.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Wang P., Yang X., Xu W., Li K., Chu Y., Xiong S. Integrating individual functional moieties of CXCL10 and CXCL11 into a novel chimeric chemokine leads to synergistic antitumor effects: a strategy for chemokine-based multi-target-directed cancer therapy. Cancer Immunol Immunother. 2010;59:1715–1726. doi: 10.1007/s00262-010-0901-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Belnoue E., Kayibanda M., Vigario A.M., Deschemin J.C., van Rooijen N., Viguier M. On the pathogenic role of brain-sequestered alphabeta CD8+ T cells in experimental cerebral malaria. J Immunol. 2002;169:6369–6375. doi: 10.4049/jimmunol.169.11.6369. [DOI] [PubMed] [Google Scholar]
- 130.Hansen D.S., Bernard N.J., Nie C.Q., Schofield L. NK cells stimulate recruitment of CXCR3+ T cells to the brain during Plasmodium berghei-mediated cerebral malaria. J Immunol. 2007;178:5779–5788. doi: 10.4049/jimmunol.178.9.5779. [DOI] [PubMed] [Google Scholar]
- 131.Hansen D.S., Siomos M.A., Buckingham L., Scalzo A.A., Schofield L. Regulation of murine cerebral malaria pathogenesis by CD1d-restricted NKT cells and the natural killer complex. Immunity. 2003;18:391–402. doi: 10.1016/s1074-7613(03)00052-9. [DOI] [PubMed] [Google Scholar]
- 132.Bauer P.R., Van Der Heyde H.C., Sun G., Specian R.D., Granger D.N. Regulation of endothelial cell adhesion molecule expression in an experimental model of cerebral malaria. Microcirculation. 2002;9:463–470. doi: 10.1038/sj.mn.7800159. [DOI] [PubMed] [Google Scholar]