SUMMARY
A case is presented of a young female with parotid recurrent pleomorphic adenoma and skin infiltration treated with subtotal parotidectomy combined with a bilateral superficial muscular aponeurotic system rhytidectomy.
KEY WORDS: Pleomorphic adenoma, Parotidectomy, Rhytidectomy, Tumour recurrence, Skin infiltration
RIASSUNTO
Gli autori descrivono il caso di una giovane donna affetta da adenoma pleomorfo parotideo ricorrente ed infiltrazione cutanea trattato mediante parotidectomia subtotale in associazione a ritidectomia bilaterale.
Introduction
The parotid gland is the most common site of salivary glands tumours; 50-74% of all parotid lesions are benign pleomorphic adenomas. The recurrence rate of pleomorphic adenoma has been dramatically reduced from 20- 45% to less than 4% over the last few decades 1.
Nevertheless, the management of recurrent pleomorphic adenomas of the parotid gland is a major challenge for the clinician 2. With surgical treatment there is a considerable risk of facial nerve injury and a high recurrence rate. Moreover, on account of the high incidence in healthy young people, the aesthetic issues are not negligible. Surgeons can use a rhytidectomy incision, for a parotidectomy, to avoid a visible scar 3 and use a superficial musculo-aponeurotic system (SMAS) flap 4 5 or fat 6 grafts to fill any hollow or recess in the retro-mandibular region 7. Nodular dissemination with skin infiltration requires parotidectomy and excision of a huge skin paddle over the tumour. Direct closure of a unilateral excision can leave an asymmetric "pulled appearance" to one side of the face. In order to preserve facial contour and symmetry, we suggest to balance the skin paddle sacrifice of the tumour affected side with a contralateral SMAS rhytidectomy 8.
Case report
A 32-year-old female (Fig. 1A) with a 10-year history of multiple residual pleomorphic adenomas underwent superficial parotidectomy three times, which resulted in a facial nerve deficiency (Fig. 1B). She was referred to our Department following recurrence involving a right parotid mass with cutaneous infiltration that had grown over the last two years.
Fig. 1.

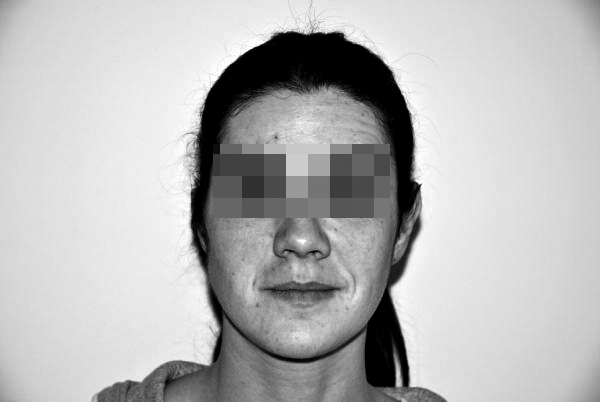
Frontal static view (A) of a 32-year-old female with recurrence of a pleomorphic adenomas. Frontal dynamic view (B) showing a facial nerve deficiency, outcome of three superficial parotidectomies.
After performing magnetic resonance imaging (MRI) (Fig. 2) and considering the patient's age, it was decided to perform a subtotal parotidectomy with facial nerve preservation and skin resection (Fig. 3A-B).
Fig. 2.
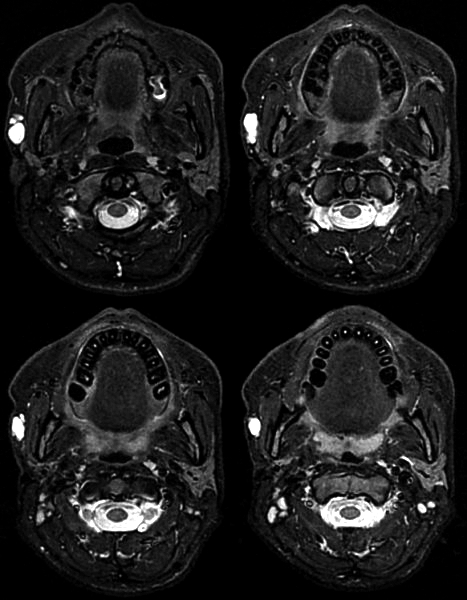
Pre-operative magnetic resonance imaging showing a right parotid mass with cutaneous infiltration.
Fig. 3.




Intra-operative views: (A) skin paddle design; (B) facial nerve identification and preservation; (C, D) extent of surgical resection.
An intra-operative frozen section confirmed the clinical diagnosis and excluded malignant transformation. The residual parotid gland was raised together with the skin and SMAS over the neoplasm (Fig. 3C-D). Subcutaneous and sub-SMAS flaps were prepared on the affected side in order to close the skin defect, with SMAS plication to fill the parotid defect. Then, to balance the facial symmetry, a SMAS and skin rhytidectomy were performed on the non-affected left side. The patient recovered very well, without any additional facial nerve dysfunction. The final pathology report confirmed that the mass was a benign pleomorphic adenoma. One month post-operatively, a satisfactory aesthetic result was achieved with perfect symmetry of the face and facial rejuvenation (Fig. 4A-B-C. One year post-operatively, there is no evidence of either disease recurrence or Frey's syndrome.
Fig. 4.



Frontal (A) and profile, right (B) and left (C), views one month post-operatively, showing symmetry of the face and facial rejuvenation without any additional facial nerve dysfunction.
Discussion
Recurrent pleomorphic adenoma presents an increased risk of malignant transformation and facial nerve damage. Skin infiltration is another of the main problems of residual adenomas, often requiring sacrifice of the skin and SMAS over the tumour with poor aesthetic results. The aims of surgical treatment of recurrent pleomorphic adenomas are wide excision of the lesions (total or subtotal parotidectomy with facial nerve preservation, whenever possible, and skin excisions, when necessary), prevention of gustatory sweating, and restoration of the facial symmetry. Surgical options should be tailored to the individual patient.
Defects of the parotid region, that include the gland and 4-5 cm of skin, can be reconstructed using non-vascularized dermal fat grafts, local skin or muscle flaps, regional myocutaneous flaps, and revascularized free tissue transfer 10 11. Each reconstructive method has inherent strengths and weaknesses, and all these options may fail to provide an excellent colour match and result in donor site morbidity. Direct closure can leave an asymmetric "pulled appearance".
In our case, we performed an aggressive unilateral face lift to obtain initial closure of the resected site and performed the same procedure on the contralateral side to obtain facial symmetry and the best aesthetic results. With SMAS plicature, this procedure allowed us to avoid Frey's Syndrome 12 13 and obtain excellent aesthetic results in terms of colour match and symmetry.
In multiple residual pleomorphic adenoma with skin infiltration, a contralateral face lift is a good choice for obtaining facial balance.
References
- 1.Redaelli de Zinis LO, Piccioni M, Antonelli AR, et al. Management and prognostic factors of recurrent pleomorphic adenoma of the parotid gland: personal experience and review of the literature. Eur Arch Otorhinolaryngol. 2008;265:447–452. doi: 10.1007/s00405-007-0502-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Valentini V, Fabiani F, Perugini M, et al. Surgical techniques in the treatment of pleomorphic adenoma of the parotid gland: our experience and review of literature. J Craniofac Surg. 2001;12:565–568. doi: 10.1097/00001665-200111000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Lohuis PJ, Tan ML, Brekel MW, et al. Superficial parotidectomy via facelift incision. Ann Otol Rhinol Laryngol. 2009;118:276–280. doi: 10.1177/000348940911800407. [DOI] [PubMed] [Google Scholar]
- 4.Marchal F, Sacoun A, Pieyre JM. Advantage of lifting in parotidectomy. Schweiz Med Wochenschr. 2000;125:116S–121S. [PubMed] [Google Scholar]
- 5.Foustanos A, Zavrides H. Face-lift approach combined with a superficial musculoaponeurotic system advancement flap in parotidectomy. Br J Oral Maxillofac Surg. 2007;45:652–655. doi: 10.1016/j.bjoms.2007.05.008. [DOI] [PubMed] [Google Scholar]
- 6.Curry JM, Fisher KW, Heffelfinger RN, et al. Superficial musculoaponeurotic system elevation and fat graft reconstruction after superficial parotidectomy. Laryngoscope. 2008;118:210–215. doi: 10.1097/MLG.0b013e3181581f94. [DOI] [PubMed] [Google Scholar]
- 7.Nouraei SA, Al-Yaghchi C, Ahmed J, et al. An anatomical comparison of Blair and facelift incisions for parotid surgery. Clin Otolaryngol. 2006;31:531–534. doi: 10.1111/j.1365-2273.2006.01334.x. [DOI] [PubMed] [Google Scholar]
- 8.Boynton JF, Cohen BE, Barrera A. Rhytidectomy and parotidectomy combined in the same patient. Aesthethic Plast Surg. 2006;30:125–131. doi: 10.1007/s00266-005-0153-6. [DOI] [PubMed] [Google Scholar]
- 9.Glas AS, Vermey A, Hollema H, et al. Surgical treatment of recurrent pleomorphic adenoma of the parotid gland: a clinical analiysis of 52 patients. Head Neck. 2001;23:311–316. doi: 10.1002/hed.1036. [DOI] [PubMed] [Google Scholar]
- 10.Teknos TN, Nussenbaum B, Bradford CR, et al. Reconstruction of complex parotidectomy defects using the lateral arm free tissue transfer. Otolaryngol Head Neck Surg. 2003;129:183–191. doi: 10.1016/S0194-5998(03)00718-6. [DOI] [PubMed] [Google Scholar]
- 11.Asal K, Köybaşioğlu A, Inal E, et al. Sternocleidomastoid muscle flap reconstruction during parotidectomy to prevent Frey's syndrome and facial contour deformity. Ear Nose Throat J. 2005;84:173–176. [PubMed] [Google Scholar]
- 12.Cesteleyn L, Helman J, King S, et al. Temporoparietal fascia flaps and superficial musculoaponeurotic system plication in parotid surgery reduces Frey's syndrome. J Oral Maxillofac Surg. 2002;60:1284–1297. doi: 10.1053/joms.2002.35725. [DOI] [PubMed] [Google Scholar]
- 13.Angspatt A, Yangyuen T, Jindarak S, et al. The role of SMAS flap in preventing Frey's syndrome following standard superficial parotidectomy. J Med Assoc Thai. 2004;87:624–627. [PubMed] [Google Scholar]


