Abstract
Introduction
Improper inhaler technique is a common problem affecting asthma control and healthcare costs. Telephonic asthma management can increase access to care while reducing costs and hospitalizations. However, no reliable method has been established for telephonically evaluating and correcting inhaler technique.
Objective
The purpose of this study was to pilot test a method for assessing and correcting patient inhaler technique via telephone.
Methods
Participants (n=30) were adults with asthma using metered-dose inhalers (MDIs) and diskus inhalers. A pharmacist was located in one room and communicated via telephone with a participant in another room. The pharmacist telephonically assessed and taught inhaler technique. Participants were video-recorded, and videos were later examined by a second pharmacist to visually evaluate inhaler technique. Participants were assigned pre- and posteducation inhaler technique scores for the telephonic and video assessments. Scores were based on summated scales for MDI (0–9) and diskus (0–11) inhalers. Paired samples t-tests were used to compare telephone and video assessments.
Results
Findings indicated a significant difference between the telephone and video assessments of MDI technique (p<0.05); however, no difference was found for the diskus inhaler. Comparing pre- and posteducation inhaler technique for MDI and diskus, mean scores significantly improved from 5.7 to 7.8 (p<0.05) and from 8.5 to 10.4 (p<0.05), respectively.
Conclusions
The telephonic method was able to improve and detect some deficiencies in patients' inhaler technique. However, modifications and further investigation will more clearly determine the role and value of such a telephonic intervention.
Key words: asthma, asthma management, telephonic monitoring, inhaler, metered-dose inhalers, MDI, diskus, dry powder inhalers, patient education as topic, telemedicine
Introduction
Estimations from 2008 indicate that over 38 million Americans have been diagnosed with asthma in their lifetime. The estimated annual economic cost associated with asthma care in the United States is $20.7 billion, with prescription medications being the largest direct medical expenditure, accounting for $5.9 billion.1 However, incorrect inhaler technique occurs in up to 90% of patients using either a metered-dose inhaler (MDI) or a dry powder inhaler (DPI).2,3 This is of major concern, since improper inhaler technique adversely affects asthma control and contributes to greater healthcare costs.4–6 Consequently, current asthma guidelines emphasize the importance of regularly assessing inhaler technique.7
Methods used to assess and teach inhaler technique include physical demonstration done either in-person, in a group, or through video instruction.8–11 Both in-person and video instruction improve proper technique more than providing written instruction alone.8–9 Patients physically demonstrating inhaler use and providers repeatedly teaching inhaler technique are associated with higher rates of correct inhaler use.2,12 In addition, repeated instruction of proper technique increases adherence to inhalation therapies.13
Access to in-person inhaler technique monitoring and optimization is inadequate for some asthma patients, especially for those with limited access to healthcare.14 Live remote video as a means to assess and teach inhaler technique among rural asthma patients was evaluated in a randomized controlled trial.15 Inhaler technique demonstration using live video by a remote pharmacist was compared to written instructions alone. The live video intervention group had the greatest improvement in baseline inhaler technique at postintervention and after a 2- to 4-week follow-up. However, the widespread use of live video to assess and correct inhaler technique may be problematic due to connectivity and a lack of equipment in patients' homes.
Telephonic asthma management increases access to care,16,17 is well accepted by patients,17–19 and is associated with both lower cost16,20 and reduced hospital readmission rates.18,21 However, to the best of our knowledge no reliable method has been established to evaluate and correct inhaler technique over the telephone. The objective of this study was to conduct a pilot test of a method for assessing and correcting patient inhaler technique via telephone. The researchers examined the differences between (1) the initial assessments of inhaler technique as determined by telephone and video, and (2) the pre-education (initial) and posteducation assessments of inhaler technique.
Methods
This prospective pilot study was conducted in the Usability Lab at Marshfield Clinic's Biomedical Informatics Research Center (BIRC), in Marshfield, Wisconsin. Marshfield Clinic is a large, integrated healthcare delivery system serving rural central, western, and northern Wisconsin. Before beginning enrollment, the study was approved by the Marshfield Clinic's Institutional Review Board.
Participants
Patients who received care from Marshfield Clinic, had a diagnosis of asthma, were 18 years of age or older, were English-speaking, and were currently using both an albuterol MDI and a fluticasone/salmeterol (Advair®) diskus inhaler were eligible for inclusion. Patients were included who were using both a rescue and controller inhaler, because combination therapy is commonly used in asthma treatment.7 Albuterol MDIs were chosen because of widespread use as a rescue medication22 and cross-application to MDI controller medications. Additionally, the fluticasone/salmeterol diskus was assessed because of common use among the DPI controller medications.22 Inhaler use was determined through electronic prescribing software data and verbal confirmation during recruitment.
After eligible patients were identified for recruitment, a telephone call was made to solicit participation, explain study details, confirm inclusion criteria, and schedule an appointment. Participants were informed the study would take approximately 1 h and they would be compensated $25 for time and travel.
Procedure
Telephone assessment of inhaler technique
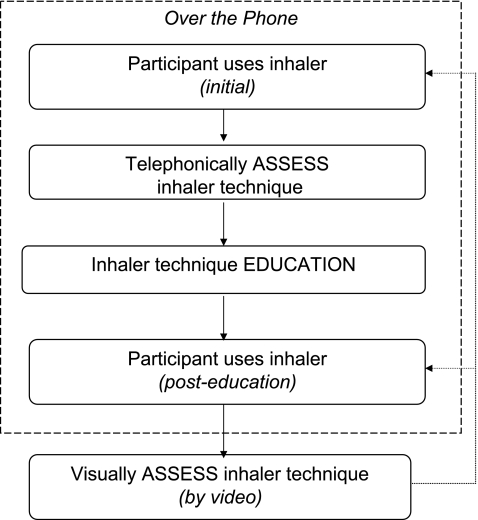
Upon arrival, lab staff obtained informed consent from participants and demographic information was collected. Participants agreed to be video-recorded during the entire encounter. After the pharmacist (P.N.) and participant were placed in separate rooms connected by telephone, the pharmacist called the participant and asked the participant to use one of two placebo inhalers (MDI or diskus) as he/she normally would to determine initial inhaler technique (Fig. 1). After the participant used the inhaler, the pharmacist asked for a step-by-step explanation of how it was used. If the pharmacist was unsure about the performance of any step, specific probing questions were used to clarify (Table 1). Then, from the information verbally provided by the participant, the pharmacist documented the inhaler technique on a checklist, indicating which steps were correctly or incorrectly performed. Checklists were based upon steps for proper inhaler use (Table 1), as determined by Food and Drug Administration–approved product package inserts and guidelines from the American College of Chest Physicians.7,23–28 Additionally, inhaler technique steps that patients commonly perform incorrectly (i.e., rate of inhalation and timing of actuation) were identified beforehand.29
Fig. 1.
Diagram of study procedures (repeated for both inhalers).
Table 1.
Inhaler Technique Steps and Questions
| INHALER | STEP | DESCRIPTION | PRIMARY PROBING QUESTIONSa |
|---|---|---|---|
| MDI | 1 | Remove cap | What did you do with the cap on the mouthpiece? |
| 2 | Hold inhaler upright | How were you holding the inhaler? | |
| 3 | Shake inhaler | What did you do with the inhaler right before using it? | |
| 4 | Exhale | What did you do with your breath right before using the inhaler? | |
| 5 | Put mouthpiece in mouth | Where did you put the mouthpiece? | |
| Were your lips closed around the mouthpiece? | |||
| 6 | Inhale through mouth | When you used the inhaler, did you breathe in through your nose or your mouth? | |
| 7 | Inhale slow and deepb | When you breathed in from the inhaler, how many seconds did you breathe in for? | |
| When did you stop breathing in? | |||
| 8 | Actuate after start inhalingb | In relation to breathing in, when did you make the mist come out? | |
| 9 | Hold breath | What did you do after you were done breathing in from the inhaler? | |
| How many seconds did you hold your breath for? | |||
| Diskus | 1 | Open inhaler | Did you slide the inhaler open so you could see the mouthpiece? |
| 2 | Push lever | What did you do with the lever before you used the inhaler? | |
| 3 | Inhaler level and flat (after dose activated) | What did you do with the inhaler after you pushed the lever? | |
| Right when you pushed the lever, was the inhaler level and flat or up and down or tilted? | |||
| 4 | Exhale (away from mouthpiece) | What did you do with your breath right before using the inhaler? | |
| Where was the inhaler mouthpiece when you breathed out the first time? | |||
| 5 | Put mouthpiece in mouth | Where did you put the mouthpiece? | |
| Were your lips closed around the mouthpiece? | |||
| 6 | Inhaler level and flat (when inhaling) | When you breathed in from the inhaler, how did you hold the inhaler? | |
| 7 | Inhale through mouth | When you used the inhaler, did you breathe in through your nose or your mouth? | |
| 8 | Inhale fast and deepb | When you breathed in from the inhaler, how many seconds did you breathe in for? | |
| How fast did you breathe in? | |||
| When did you stop breathing in? | |||
| 9 | Hold breath | What did you do after you were done breathing in from the inhaler? | |
| How many seconds did you hold your breath for? | |||
| 10 | Exhale (away from mouthpiece) | When you breathed out, after you were done using the inhaler, where was the mouthpiece? | |
| 11 | Close inhaler | What did you do with the inhaler once you were done using it? |
Secondary questions were also used when needed (available upon request).
Common problem steps.29
MDI, metered-dose inhaler.
Telephonic educational session
After this initial assessment, the pharmacist educated the participant over the telephone about how to properly use the inhaler. The educational session was developed following recommendations on effectively teaching inhaler technique skills.6,30 The pharmacist targeted steps performed incorrectly (identified from the initial assessment) as well as common problem steps. The pharmacist also audibly demonstrated, and the participant audibly practiced the proper speed of inhalation without the inhaler during the education session. Participants were encouraged to use a clock in the room to time both the pharmacist and themselves while practicing the proper inhalation speed. All participants were encouraged to practice the common problem steps until comfortable with them.
Continuing with the educational session, the pharmacist verbalized all the steps for proper inhaler use. The participant was asked to verbally repeat all the steps, after which the pharmacist corrected any misunderstandings and used probing questions to reinforce any steps the participant failed to mention. The participant subsequently practiced all the steps, after which the pharmacist assessed whether both the common problem steps and the steps done incorrectly on the initial assessment were now performed correctly. Finally, the participant was asked to physically use the inhaler one last time (posteducation inhaler technique).
This pattern of assessment and education was repeated with the second inhaler for all participants. The first inhaler used for each participant was alternated between MDI and diskus. All telephonic interactions between participants and the pharmacist occurred using a speakerphone. Neither the pharmacist nor the participant saw each other during the telephonic interaction. To ensure that participants had been taught proper inhaler technique before leaving, the pharmacist entered the participant's room and evaluated and corrected (if applicable) participant inhaler technique in person.
Video assessment and scoring of inhaler technique
A second pharmacist (Griesbach) visually evaluated each participant's inhaler technique by reviewing the video recordings. For the video assessments, checklists were used to score all participants' initial inhaler technique and posteducation inhaler technique for both the MDI and diskus. In scoring participants' inhaler technique, one point was given for each step completed correctly, with each step equally weighted. Scores could range from 0 to 9 for the MDI and 0 to 11 for the diskus inhaler. This algorithm also was used to score the telephone-based assessments of participants' initial inhaler technique.
Analysis
Descriptive statistics were calculated to describe participants' initial and posteducation inhaler technique for both devices. Paired samples t-tests were used to examine the differences between the overall mean scores determined by assessment method (telephone versus video assessment of initial inhaler technique) and by time period (video assessments of initial versus posteducation inhaler technique). In addition, total percent agreements and phi coefficients were calculated to examine the consistency (reliability) between the telephone and visual assessment of initial inhaler technique (by step).
Results
Thirty patients participated in this study. To obtain 30 participants, 104 patients were called, with 43 agreeing to participate and 61 declining. Of the 43 who agreed to enroll, 13 cancelled or failed to attend the scheduled appointment time. Ninety-three percent of participants were Caucasian, 60% were women, and 62% were over 50 years of age (Table 2). All telephonic lab interventions were completed within a 2 week period of time.
Table 2.
Participant Demographics (n=30)
| VARIABLE | N (%) |
|---|---|
| Agea | |
| 18–30 | 1 (3) |
| 31–40 | 3 (10) |
| 41–50 | 7 (24) |
| 51+ | 18 (62) |
| Gender | |
| Male | 12 (40) |
| Female | 18 (60) |
| Race | |
| Asian | 1 (3) |
| Black or African American | 1 (3) |
| White or Caucasian | 28 (93) |
| Highest education | |
| Completed grade school | 1 (3) |
| HS diploma/GED | 5 (17) |
| Some college | 11 (37) |
| College degree | 9 (30) |
| Graduate/professional degree | 4 (13) |
| How long been using diskus | |
| <1 year | 1 (3) |
| 1–3 years | 10 (33) |
| >3 years | 19 (63) |
| How long been using MDIa | |
| <1 year | 0 (0) |
| 1–3 years | 4 (14) |
| >3 years | 25 (86) |
n=29 (one was not answered).
HS, high school; GED, general equivalency degree.
The mean initial MDI inhaler technique scores for the telephone and video methods of assessment were 7.2 (standard deviation [SD]=1.1) and 5.7 (SD=1.6), respectively. Results from a paired samples t-test showed a significant difference between these two assessments of inhaler technique (t=4.90; p<0.05). The mean initial diskus inhaler technique scores for the telephonic and video methods were 8.8 (SD=1.4) and 8.5 (SD=1.7), respectively; the difference between the scores was not statistically significant.
The mean MDI technique scores (determined by video) at pre- and posteducation significantly improved from 5.7 (SD=1.6) to 7.8 (SD=1.1) (t=6.7; p<0.05). Overall, a greater percentage of participants displayed the correct technique for each MDI step during the posteducation assessment as compared to the initial assessment (Table 3). More than 80% of participants displayed the correct technique for seven of the nine steps at posteducation. The greatest improvements in MDI technique were in exhaling prior to inhalation (from 40% to 97%) and actuating inhaler after starting to inhale (from 17% to 67%). In addition, the majority of participants' MDI scores improved (90%) in comparison to those who remained the same (7%) or worsened (3%).
Table 3.
Comparison of Initial and Posteducation Scores (by Step)
| |
|
VIDEO |
|
|---|---|---|---|
| INHALER | STEP | INITIALa | POSTa |
| MDI | 1. Remove cap | 97% | 100% |
| 2. Sit upright | 83% | 87% | |
| 3. Hold inhaler upright | 93% | 97% | |
| 4. Shake inhaler | 70% | 90% | |
| 5. Exhale | 40% | 97% | |
| 6. Put mouthpiece in mouth | 87% | 100% | |
| 7. Inhale through mouth | 100% | 100% | |
| 8. Inhale slow and deep | 17% | 50% | |
| 9. Actuate after start inhaling | 17% | 67% | |
| 10. Hold breath | 50% | 83% | |
| Diskus | 1. Open inhaler | 100% | 100% |
| 2. Sit upright | 77% | 97% | |
| 3. Push lever | 97% | 93% | |
| 4. Keep inhaler level and flat | 27% | 83% | |
| 5. Exhale (away from mouthpiece) | 37% | 93% | |
| 6. Put mouthpiece in mouth | 100% | 100% | |
| 7. Inhaler level and flat (when inhaling) | 63% | 93% | |
| 8. Inhale through mouth | 100% | 100% | |
| 9. Inhale fast and deep | 93% | 97% | |
| 10. Hold breath | 57% | 83% | |
| 11. Exhale (away from mouthpiece) | 93% | 100% | |
| 12. Close inhaler | 80% | 97% | |
Reflects percentage of participants with correct inhaler technique.
The mean diskus inhaler technique scores (determined by video) also significantly improved from 8.5 (SD=1.7) to 10.4 (SD=1.1) (t=7.14; p<0.05). At least 80% of participants performed each diskus inhaler step correctly at posteducation (Table 3). The greatest improvements in diskus technique were in exhaling before inhalation (from 37% to 93%) and holding the inhaler level and flat when activating the dose (from 27% to 83%). The majority of participants' diskus inhaler scores improved (90%) in comparison to those who worsened (7%) or remained the same (3%).
Comparing individual steps of the phone and video initial assessments of MDI technique, the overall percent agreement ranged from 47% to 97% and phi coefficients ranged from 0.12 to 0.85 (Table 4). The telephone assessment rated more steps as being performed correctly than the video assessment. In a similar comparison of the two initial assessments of diskus technique, the overall percent agreement ranged from 30% to 100% and phi coefficients ranged from 0.07 to 0.60. Overall, the telephonic assessment rated more steps as being performed correctly than the video assessment; although, one step broke this trend considerably (breathing in fast and deep).
Table 4.
Comparison of Phone and Video Inhaler Technique Scores (by Step)
| INHALER | STEP | VIDEOa | PHONEa | % | PHI |
|---|---|---|---|---|---|
| MDI | 1. Remove cap | 97% | 100% | 97 | b |
| 2. Hold inhaler upright | 93% | 100% | 93 | b | |
| 3. Shake inhaler | 70% | 77% | 93 | 0.84 | |
| 4. Exhale | 40% | 87% | 47 | 0.12 | |
| 5. Put mouthpiece in mouth | 87% | 90% | 97 | 0.85 | |
| 6. Inhale through mouth | 100% | 97% | 97 | b | |
| 7. Inhale slow and deep | 17% | 37% | 53 | 0.15 | |
| 8. Actuate after start inhaling | 17% | 40% | 63 | 0.18 | |
| 9. Hold breath | 50% | 93% | 57 | 0.27 | |
| Diskus | 1. Open inhaler | 100% | 100% | 100 | b |
| 2. Push lever | 97% | 87% | 83 | 0.07 | |
| 3. Keep inhaler level and flat | 27% | 67% | 60 | 0.45 | |
| 4. Exhale (away from mouthpiece) | 37% | 67% | 57 | 0.24 | |
| 5. Put mouthpiece in mouth | 100% | 100% | 100 | b | |
| 6. Inhaler level and flat (when inhaling) | 63% | 90% | 67 | 0.21 | |
| 7. Inhale through mouth | 100% | 100% | 100 | b | |
| 8. Inhale fast and deep | 93% | 30% | 30 | 0.12 | |
| 9. Hold breath | 57% | 70% | 80 | 0.60 | |
| 10. Exhale (away from mouthpiece) | 93% | 90% | 83 | 0.09 | |
| 11. Close inhaler | 80% | 80% | 87 | 0.58 |
Reflects percentage of participants with correct inhaler technique.
Unable to be determined due to lack of variation.
%, percent agreement.
Discussion
The objective of the study was to pilot test a method of assessing and teaching inhaler technique over the phone. Study findings suggest that there may be a role for telephonically teaching and assessing patient inhaler technique.
To determine whether telephonic teaching improved inhaler technique, visual assessments of inhaler technique were compared before and after the educational session. The teaching method significantly improved participants' inhaler technique for both inhalers. Overall, scores improved by 23% and 17% for the MDI and diskus, respectively. Studies examining various methods of instruction have reported similar improvements of 14% to 44%.10,11,15 In addition, participants showed improvements on three MDI steps that have been previously noted as being most important (i.e., exhale, inhale slow and deep, and hold breath).31
In an effort to examine the feasibility of assessing inhaler technique telephonically, assessments made aurally over the telephone were compared to those done visually by video. The overall ratings of initial inhaler technique, using both methods, were similar for the diskus inhalers. However, the telephone method tended to rate MDI technique as being better than did the video method. In addition, findings indicated a reasonable level of agreement between the two methods for several inhaler technique steps but low agreement for others. One plausible explanation for the discrepancies may be the telephonic communication process—participants may have been unable to explain how they used the inhaler or the pharmacist may have misinterpreted participants' responses. A second explanation may be the problem of obtaining high inter-rater reliability between healthcare professionals' ratings of inhaler technique. Gray et al.32 reported difficulties in achieving high interrater reliability among healthcare professionals assessing MDI technique, even though a 2-h training session was used. Thus, the variability in the assessment of inhaler technique found in this study may have been increased due to using two raters (pharmacists) in addition to using two assessment methods (telephone and visual).
An effective telephonic method of teaching and assessing inhaler technique may be useful in caring for patients with asthma. With clinicians using this method for repeated teaching, rates of proper inhaler use and adherence to prescribed regimens may increase, which consequently could improve asthma control and reduce asthma-related healthcare costs. In addition, it would provide a means for increasing access to healthcare, especially for asthma patients in rural settings. Lastly, such a telephonic method also may provide great benefit when integrated into telephonic disease state management for patients with asthma.
To the best of our knowledge, this is the first study to evaluate a telephonic method of assessing and teaching inhaler technique. Preliminary findings suggest value in this approach; however, additional study is warranted. Future research should validate this study's findings in larger, more diverse populations and settings. Studies also may assess patients' retention of improved inhaler technique and evaluate important outcomes such as asthma control and patient satisfaction. In addition, comparing this telephonic approach to other methods of instruction (e.g., face-to-face, written, and Web-based tools) would be important before integrating it into widespread practice.
This study has limitations that should be considered. First, this study consists of a small sample with limited diversity. Study participants were mostly older, fairly well-educated Caucasians; the effectiveness of this intervention may differ across a broader population. Next, this pilot study was conducted in a controlled environment. A home or clinic setting may present barriers, such as background noise, that may affect a clinician's ability to assess and provide education regarding inhaler technique. In addition, participants may have adjusted their normal inhaler technique because they knew they were being studied (i.e., Hawthorne effect). Finally, this pilot study focused on limited outcomes (i.e., inhaler technique scores) and not long-term outcomes. Because of the pilot nature of this study, we sought to explore the feasibility of this telephonic intervention. An examination of outcomes such as costs or hospitalizations would provide information about the broader clinical impact of this telephonic method.
Conclusions
With incorrect inhaler technique being common, adversely affecting asthma control, and increasing healthcare costs, asthma patients could benefit from a wide-reaching method for ensuring proper inhaler technique. This pilot study provides evidence to support the plausibility of detecting deficiencies in and improving patients' inhaler technique via the telephone. However, modifications and further investigation will more clearly determine the role and value of such a telephonic intervention.
Acknowledgments
The authors are grateful to Andrea Mahnke, BIRC usability analyst, for the wonderful technical support in utilizing the Marshfield Clinic Research Foundation's BIRC lab. We also thank Nina M. Antoniotti, RN, MBA, PhD; Elizabeth D. Cox, MD, PhD; and Megan A. Moreno, MD, MSEd, MPH, for their review of the article. We further thank Marie Fleisner of the Marshfield Clinic Research Foundation's Office of Scientific Publication for editorial assistance in the preparation of this article. Funding for this study was provided by Marshfield Clinic's Division of Education Resident Research Program and supported by grant 1UL1RR025011 from the Clinical and Translational Science Award program of the National Center for Research Resources, National Institutes of Health.
Disclosure Statement
No competing financial interests exist.
References
- 1.American Lung Association. Trends in asthma morbidity and mortality. 2010. www.lungusa.org/finding-cures/our-research/trend-reports/asthma-trend-report.pdf. [Nov 20;2010 ]. www.lungusa.org/finding-cures/our-research/trend-reports/asthma-trend-report.pdf
- 2.Basheti IA. Armour CL. Bosnic-Anticevich SZ. Reddel HK. Evaluation of a novel educational strategy, including inhaler-based reminder labels, to improve asthma inhaler technique. Patient Educ Couns. 2008;72:26–33. doi: 10.1016/j.pec.2008.01.014. [DOI] [PubMed] [Google Scholar]
- 3.Souza ML. Meneghini AC. Ferraz E. Vianna EO. Borges MC. Knowledge of and technique for using inhalation devices among asthma patients and COPD patients. J Bras Pneumol. 2009;35:824–831. doi: 10.1590/s1806-37132009000900002. [DOI] [PubMed] [Google Scholar]
- 4.Giraud V. Roche N. Misuse of corticosteroid metered-dose inhaler is associated with decreased asthma stability. Eur Respir J. 2002;19:246–251. doi: 10.1183/09031936.02.00218402. [DOI] [PubMed] [Google Scholar]
- 5.Molimard M. Le Gros V. Impact of patient-related factors on asthma control. J Asthma. 2008;45:109–113. doi: 10.1080/02770900701815727. [DOI] [PubMed] [Google Scholar]
- 6.Fink JB. Rubin BK. Problems with inhaler use: A call for improved clinician and patient education. Respir Care. 2005;50:1360–1374. discussion 1374–1375. [PubMed] [Google Scholar]
- 7.National Heart, Lung, and Blood Institute. National Asthma Education and Prevention Program. Expert panel report 3: Guidelines for the diagnosis and management of asthma. Full report 2007. www.nhlbi.nih.gov/guidelines/asthma/asthgdln.pdf. [Nov 20;2010 ]. www.nhlbi.nih.gov/guidelines/asthma/asthgdln.pdf
- 8.McElnay JC. Scott MG. Armstrong AP. Stanford CF. Audiovisual demonstration for patient counselling in the use of pressurised aerosol bronchodilator inhalers. J Clin Pharm Ther. 1989;14:135–144. doi: 10.1111/j.1365-2710.1989.tb00232.x. [DOI] [PubMed] [Google Scholar]
- 9.Self TH. Brooks JB. Lieberman P. Ryan MR. The value of demonstration and role of the pharmacist in teaching the correct use of pressurized bronchodilators. Can Med Assoc J. 1983;128:129–131. [PMC free article] [PubMed] [Google Scholar]
- 10.van der Palen J. Klein JJ. Kerkhoff AH. van Herwaarden CL. Seydel ER. Evaluation of the long-term effectiveness of three instruction modes for inhaling medicines. Patient Educ Couns. 1997;32:S87–S95. doi: 10.1016/s0738-3991(97)00100-6. [DOI] [PubMed] [Google Scholar]
- 11.Bosnic-Anticevich SZ. Sinha H. So S. Reddel HK. Metered-dose inhaler technique: The effect of two educational interventions delivered in community pharmacy over time. J Asthma. 2010;47:251–256. doi: 10.3109/02770900903580843. [DOI] [PubMed] [Google Scholar]
- 12.Kamps AW. Brand PL. Roorda RJ. Determinants of correct inhalation technique in children attending a hospital-based asthma clinic. Acta Paediatr. 2002;91:159–163. doi: 10.1080/080352502317285144. [DOI] [PubMed] [Google Scholar]
- 13.Takemura M. Kobayashi M. Kimura K. Mitsui K. Masui H. Koyama M. Itotani R. Ishitoko M. Suzuki S. Aihara K. Matsumoto M. Oguma T. Ueda T. Kagioka H. Fukui M. Repeated instruction on inhalation technique improves adherence to the therapeutic regimen in asthma. J Asthma. 2010;47:202–208. doi: 10.3109/02770900903581692. [DOI] [PubMed] [Google Scholar]
- 14.Valet RS. Perry TT. Hartert TV. Rural health disparities in asthma care and outcomes. J Allergy Clin Immunol. 2009;123:1220–1225. doi: 10.1016/j.jaci.2008.12.1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bynum A. Hopkins D. Thomas A. Copeland N. Irwin C. The effect of telepharmacy counseling on metered-dose inhaler technique among adolescents with asthma in rural Arkansas. Telemed J E Health. 2001;7:207–217. doi: 10.1089/153056201316970902. [DOI] [PubMed] [Google Scholar]
- 16.Pinnock H. Adlem L. Gaskin S. Harris J. Snellgrove C. Sheikh A. Accessibility, clinical effectiveness, and practice costs of providing a telephone option for routine asthma reviews: Phase IV controlled implementation study. Br J Gen Pract. 2007;57:714–722. [PMC free article] [PubMed] [Google Scholar]
- 17.Pinnock H. Bawden R. Proctor S. Wolfe S. Scullion J. Price D. Sheikh A. Accessibility, acceptability, and effectiveness in primary care of routine telephone review of asthma: Pragmatic, randomised controlled trial. BMJ. 2003;326:477–479. doi: 10.1136/bmj.326.7387.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Donald KJ. McBurney H. Teichtahl H. Irving L. A pilot study of telephone based asthma management. Aust Fam Physician. 2008;37:170–173. [PubMed] [Google Scholar]
- 19.Pinnock H. Madden V. Snellgrove C. Sheikh A. Telephone or surgery asthma reviews? Preferences of participants in a primary care randomised controlled trial. Prim Care Respir J. 2005;14:42–46. doi: 10.1016/j.pcrj.2004.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pinnock H. McKenzie L. Price D. Sheikh A. Cost-effectiveness of telephone or surgery asthma reviews: Economic analysis of a randomised controlled trial. Br J Gen Pract. 2005;55:119–124. [PMC free article] [PubMed] [Google Scholar]
- 21.Coughey K. Klein G. West C. Diamond JJ. Santana A. McCarville E. Rosenthal MP. The child asthma link line: A coalition-initiated, telephone-based, care coordination intervention for childhood asthma. J Asthma. 2010;47:303–309. doi: 10.3109/02770900903580835. [DOI] [PubMed] [Google Scholar]
- 22.Bartholow M. Top 200 prescription drugs of 2009. Pharmacy Times® 2009. www.pharmacytimes.com/issue/pharmacy/2010/May2010/RxFocusTopDrugs-0510. [Jun 24;2010 ]. www.pharmacytimes.com/issue/pharmacy/2010/May2010/RxFocusTopDrugs-0510
- 23.Using Your MDI—Closed Mouth Technique. Patient Education Guide. American College of Chest Physicians 2006. www.accpstorage.org/newOrganization/patients/inhaledDevices/patientEducation6.pdf. [Sep 14;2009 ]. www.accpstorage.org/newOrganization/patients/inhaledDevices/patientEducation6.pdf
- 24.Using Your Diskus. Patient Education Guide. American College of Chest Physicians 2006. www.accpstorage.org/newOrganization/patients/inhaledDevices/patientEducation1.pdf. [Sep 14;2009 ]. www.accpstorage.org/newOrganization/patients/inhaledDevices/patientEducation1.pdf
- 25.Advair® [package insert] Research Triangle Park, NC: GlaxoSmithKline; 2009. [Google Scholar]
- 26.ProAir® [package insert] Horsham, PA: Teva Specialty Pharmaceuticals LLC; 2008. [Google Scholar]
- 27.Proventil® [package insert] Kenilworth, NJ: Schering Corporation; 2007. [Google Scholar]
- 28.Ventolin® [package insert] Research Triangle Park, NC: GlaxoSmithKline; 2009. [Google Scholar]
- 29.Melani AS. Zanchetta D. Barbato N. Sestini P. Cinti C. Canessa PA. Aiolfi S. Neri M. Associazione Italiana Pneumologi Ospedalieri Educational Group. Inhalation technique and variables associated with misuse of conventional metered-dose inhalers and newer dry powder inhalers in experienced adults. Ann Allergy Asthma Immunol. 2004;93:439–446. doi: 10.1016/s1081-1206(10)61410-x. [DOI] [PubMed] [Google Scholar]
- 30.National Heart, Lung, and Blood Institute. National Asthma Education and Prevention. Practical Guide for the Diagnosis and Management of Asthma. 1997. www.niehs.nih.gov/health/docs/asthma-plan.pdf. [Nov 20;2010 ]. www.niehs.nih.gov/health/docs/asthma-plan.pdf
- 31.National Heart, Lung, and Blood Institute. The role of the pharmacist in improving asthma care. NIH Publication No. 95–3280. National Heart, Lung, and Blood Institute; Bethesda, MD: 1995. [Google Scholar]
- 32.Gray SL. Nance AC. Williams DM. Pulliam CC. Assessment of interrater and intrarater reliability in the evaluation of metered dose inhaler technique. Chest. 1994;105:710–714. doi: 10.1378/chest.105.3.710. [DOI] [PubMed] [Google Scholar]