Abstract
Purpose
To investigate abandonment rate of prescribed low vision devices for near tasks and factors associated with abandonment in a U.S. outpatient population.
Methods
A telephone survey was administered to 88 patients with low vision from four clinical sites approximately one year after examination and prescription of devices. Patients were surveyed on timing and frequency of use and reasons for abandonment of devices. The main outcome measure (abandonment) was defined as patient report of no use of prescribed device in the previous three months. Multivariate logistic regression was used to investigate significant vision and demographic factors related to abandonment.
Results
Of 119 prescribed devices, 19% (95% CI, 12–26) had not been used within the previous three months. Mean (±SD) better eye visual acuity at examination was 0.61±0.29 logMAR and mean age was 77±17 years. Mean time between device prescription and survey was 11±3 months. Device abandonment was not associated with age (p = 0.863), time since prescription (p = 0.125), visual acuity (p = 0.804), or category of magnification device (spectacle, handheld, stand, or video) (p = 0.412). There was a significant association between documented non-central visual field loss and abandonment of magnification device (p=0.046). Repeat administration of the survey resulted in the same abandonment classification in 15 of 15 patients (100%).
Conclusions
Abandonment rate was similar for this outpatient population to those previously reported in the U.S. veteran inpatient population and in other countries. Patients with visual field loss may be more likely to abandon prescribed devices.
Keywords: low vision rehabilitation
The number of blind and visually impaired patients in the United States is expected to increase dramatically over the next 20 years due largely to age-related eye disease.1 One study predicted a doubling of the number of new cases of low vision and blindness by the year 2025.2 Magnification devices are among the most common forms of intervention in a low vision rehabilitation program.3–5 They are typically prescribed to allow people with vision impairments to read small print more easily and are most commonly simple handheld devices or plus lens spectacles. They can also be video camera based. Given the frequency with which these devices are prescribed and their importance to patients with low vision, it is surprising how little is known about how much they are actually used after the initial examination, the rate at which they are abandoned, and the factors responsible for abandonment.
Various studies have investigated usage rates of devices in particular populations. Results from one of the first of these were published by Fonda in 1956.6 In a sample of 240 patients with low vision who were prescribed lenses 72% were judged to be “successful” after an interview two months after prescription. The criteria for success included frequency of use and the tasks lenses were used for, but specific usage rates were not reported.
Watson et al. conducted a study of aid usage in veterans who had been prescribed aids through the U.S. Department of Veterans Affairs.7–8 This study consisted of two hundred subjects who were surveyed regarding their device usage between 12 and twenty-four months after prescription. The investigators found that 85.4% of the prescribed devices were being used regularly. In this case, use was defined as a patient statement that the device was at least “somewhat helpful”. Having someone in the home to aid the patient was significantly related to use of the device. The authors found no significant relationship between age, visual acuity, or disease process and the usage of prescribed aids.
Watson et al. found that video-based magnification devices were the type of aid reported to be most helpful by the veterans surveyed.8 They also reported that the most common reason given for discontinuation of device usage was that another aid was used for reading in place of the discontinued aid. Other commonly-reported reasons for abandonment of prescribed devices were that the device did not provide enough magnification and that the ergonomics of the device were poor. A previous study of CCTV usage in the U.S. Veteran’s Affairs population found that 87% of patients prescribed CCTVs still used them regularly after at least two years.9 Usage was determined by questioning during a home visit and confirmation that the patient could demonstrate proficiency with the device.
Harper et al. studied device usage rates in 56 patients with macular degeneration in the United Kingdom 10 and found that 87% of subjects reported regularly using their devices and 65% reported using them at least once per day. Several factors were found to be significantly related to the rating of a low vision aid as “important”. These included the number of tasks that the device was used for and the frequency and ease of usage.
Leat et al. examined low vision aid usage in Wales 11 (n = 57) and found that 81% of patients reported regular use of prescribed aids. Usage was defined as at least once per day. They found a relationship between perceived benefit of the device and frequency of use that bordered on statistical significance.
Elliott et al.12 surveyed 34 patients in England with visual acuity ranging from 20/200 to counting fingers who had undergone a hospital-based low vision program. In contrast to the relatively high usage rates found in the studies previously discussed, Elliott et al. found that only 20% of respondents reported using their low vision aids frequently and one third never used the aids at all.12
There is still a lack of knowledge regarding abandonment rates and the factors related to abandonment of prescribed devices in the U.S. outpatient population, especially since much of the work done in the U.S. has been with inpatient programs in the veteran population. The importance of studying the outpatient population is highlighted by Owsley et al.’s recent finding that the vast majority of vision rehabilitation services provided in the U.S. are provided on an outpatient basis.13
We have conducted a preliminary study of low vision device abandonment in an outpatient-based, non-veteran U.S. population. Feasibility of delivering the survey by telephone and repeatability of the instrument were assessed. Rates of device abandonment were determined and the relationship between visual and non-visual factors and abandonment was evaluated.
METHODS
Survey Instrument
A telephone survey instrument (see Appendix–available at [LWW insert link]) was developed to measure usage rates of low vision devices for near tasks prescribed in U.S. outpatient clinics.
The instrument assesses timing and frequency of device use, nature of the near task for which the device is used, payment type (self pay versus family, agency, or other), and reasons for abandonment. It was designed to be administered by telephone.
Participants
In a multi-center pilot study, the survey was administered to 88 patients who had been prescribed a total of 119 magnification devices for near tasks at four separate clinical sites. A chart review was performed in order to identify adult patients who had been prescribed a magnification low vision device approximately one year prior to the time of the review. We attempted to contact all patients who had been prescribed any device used for near tasks. This included handheld or stand magnifiers, video magnifiers, microscopics, loupes, or near additions in spectacles of at least +4.00 diopters.
Informed consent was obtained from all participants over the telephone before administration of the survey and after an explanation of the nature of the study and the procedures was given. Any patient with a hearing or cognitive impairment that was, in the interviewer’s judgment, severe enough to prevent adequate understanding of the investigator’s phone call was excluded from the study. Study procedures were approved by institutional review boards at all clinical sites. This research was conducted in compliance with the Declaration of Helsinki.
Clinical Sites
All four clinical sites were associated with colleges or universities. Three of the four sites were colleges of optometry (The Ohio State University, The New England College of Optometry, and Nova Southeastern University), and the fourth was a university ophthalmology clinic (Vanderbilt University). Low vision devices were prescribed by an optometrist after a low vision examination at all sites with an in-office demonstration of use of the device and a trial of the device by the patient. No effort was made to control for individual variations in the nature of the examination that may have occurred between sites.
At three of the four sites, the patient may have been referred for additional care by an occupational therapist or certified low vision therapist if deemed appropriate by the prescribing optometrist. This additional visit may have included specific training in the use of the prescribed device, or it may have consisted of other training and discussion of strategies for coping with vision impairment. There was not, however, a standardized protocol for training in the use of prescribed devices that was followed at the sites.
Abandonment
Device abandonment was defined as no use in the past three months. Patients were asked to specify the last time they used the device in question. If a patient reported no use of a device in the past three months, he or she was asked to specify the reason for abandonment of that device. All patients were asked to specify the tasks for which they frequently used prescribed devices. In addition, patients were surveyed about the timing and frequency of device use and payment type (whether the patient paid for the device or it was paid for by another entity). In addition to structured categorical responses, the survey also contained open-ended questions to capture the patient’s initial response regarding the above items.
All survey questions were asked separately for each device if more than one device had been prescribed at the low vision examination. Care was taken by interviewers to ensure that the patient was clear about which specific device was being discussed. Physical characteristics of the particular device, including size, shape, color, and markings were discussed in order to confirm that both interviewer and patient were discussing the same device. If the interviewer was unable to confirm that the patient was aware of which device he or she was being questioned about, a survey was not completed for that device.
Repeatability
The survey was administered a second time one to three weeks later to a subset of patients (n = 15) who had been successfully surveyed to assess repeatability. This subset included patients from all four sites. The patients who participated in the repeatability study were selected based on their willingness to participate in a second survey. The second survey was administered in an identical manner as the first, using the same script. Abandonment of the device (whether the patient reported any use in the past three months) was the primary outcome measure used to assess repeatability. Responses to survey items regarding frequency of use were also analyzed for consistency.
Statistical Analysis
T tests and Fisher’s exact tests were performed to determine whether there were differences in characteristics of patients who had abandoned a prescribed device and those who had not. A logistic regression analysis was used to determine whether vision and demographic variables were significantly associated with the primary outcome measure–abandonment of a prescribed low vision device. Vision and demographic characteristics were all entered in to a model simultaneously in order to determine whether any relationships were significant after controlling for the other factors. Goodness of fit of the logistic regression model was assessed using the Hosmer-Lemeshow goodness of fit test. Statistical analyses were performed using SPSS version 17.0 (SPSS Inc., Chicago, IL).
RESULTS
Mean (±SD) visual acuity of study participants at examination was 0.61±0.29 logMAR (Snellen equivalent = 20/82, range 20/30 to 20/400). Mean age was 77±17 years. Mean time between device prescription and telephone survey was 11±3 months.
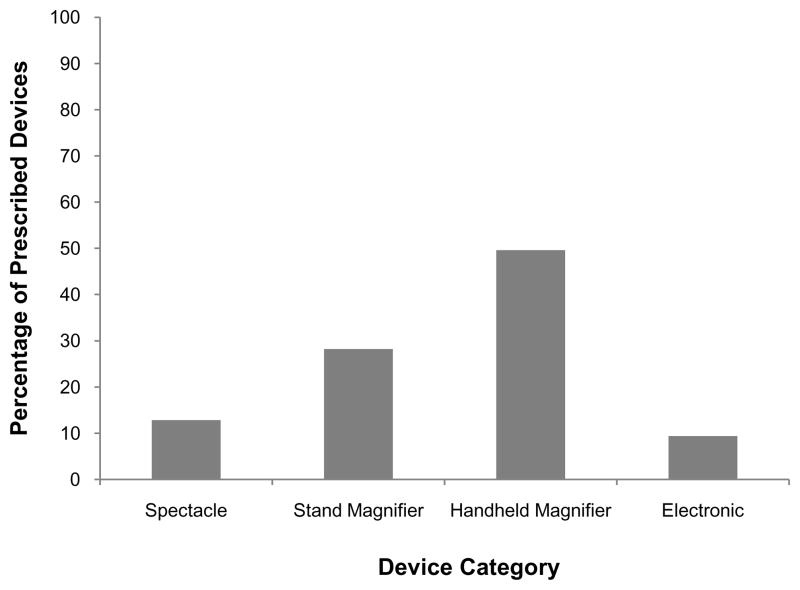
A total of 119 devices were documented as prescribed at the visit of interest. The distribution of prescribed devices is shown in Figure 1. The most frequently prescribed device type was handheld magnifier (49% of all devices prescribed). Stand magnifiers were the next most commonly-prescribed device type (29%).
Figure 1.
Percent of prescribed low vision devices by type.
Of a total of 88 patients, 19 had abandoned at least one prescribed device. Of all prescribed devices, 19% (95% CI, 12–26) had reportedly not been used within the previous three months. 71% of all devices were reported to have been used within the previous week.
Of the 22 devices reported to have been abandoned, the reason for abandonment was recorded for 18 of them. Six patients (33%) reported having stopped using the device because it was ineffective for the task, five (28%) because they used a different device for the task, and three (17%) because their vision had worsened. Other reported reasons for abandonment included being pressured into getting the device by family members but never really wanting it, a defective lens which appeared to have a spot in the center of it which interfered with use, lack of a reading desk to use the device with, and general inability to use device.
Vision and demographic characteristics of participant patients, grouped by whether or not they had abandoned a device, are presented in Table 1. Patients who abandoned any prescribed device (even if they had not abandoned other devices prescribed at the examination) were included in the “abandoned” group. None of the demographic characteristics was significantly different between those who had abandoned a device and those who had not.
Table 1.
Characteristics of patients who abandoned at least one prescribed device and those who did not abandon any devices. P values for t-tests or Fisher’s exact tests are of differences in characteristics between groups are listed.
| Abandoned at least one device (n=19) | Did not abandon a device (n=69) | P value | |
|---|---|---|---|
| BCVA (logMAR) | 0.60 (0.29) | 0.63 (0.30) | 0.734 |
|
| |||
| Months Since Prescription | 11.7 (3.9) | 11.0 (3.2) | 0.393 |
|
| |||
| Age | 79 (13) | 79 (17) | 0.545 |
|
| |||
| Gender | |||
| male | 8 | 24 | 0.597 |
| female | 11 | 45 | |
|
| |||
| Ocular Disease | |||
| AMD | 11 | 40 | 0.537 |
| DM retinopathy | 1 | 5 | |
| glaucoma | 4 | 8 | |
| macular dystrophy | 1 | 2 | |
| albinism | 0 | 1 | |
| retinitis pigmentosa | 1 | 1 | |
| other | 1 | 11 | |
Table 2 shows the results of the logistic regression in which better eye visual acuity, ocular disease classification, visual field restriction, age, sex, payment type (self or other entity), exam site, and whether the patient received any additional occupational therapy were all included in the model. When all of these variables were included together, the only one which showed a significant association with abandonment of a prescribed device was documentation of non-central visual field loss (p=0.049). For the purpose of this study, non-central visual field loss was considered any loss outside the central 20 degrees. Because this was a retrospective study, visual field loss was not uniformly quantified and may have been measured by Goldmann perimetry, automated testing or confrontation. Patients who had a documented loss of non-central visual field were significantly more likely to have abandoned at least one device. The odds ratio for abandonment given documented visual field loss was 4.97. The Hosmer-Lemeshow test showed no gross lack of fit of the model to the data (p = 0.76).
Table 2.
Results of the logistic regression analysis in which all listed variables were placed in the model together. Only non-central visual field loss was significantly related to abandonment of a prescribed device.
| Variable | β | SE | Wald Statistic | df | P value |
|---|---|---|---|---|---|
| Age | 0.023 | 0.027 | 0.71 | 1 | 0.401 |
| Sex | 0.009 | 0.649 | 0.00 | 1 | 0.989 |
| Best VA | 0.935 | 1.117 | 0.70 | 1 | 0.403 |
| Training | -- | 0.707 | 0.18 | 1 | 0.669 |
| Non-central Visual Field Loss | 1.603 | 0.815 | 3.87 | 1 | 0.049* |
| Ocular Diagnosis | -- | -- | 1.19 | 6 | 0.977 |
| Payment Method | 0.971 | 0.916 | 1.12 | 1 | 0.289 |
| Study Center | -- | -- | 1.76 | 3 | 0.624 |
p < 0.05
The telephone survey was administered a second time to a subgroup of patients (n=15) in order to assess its repeatability. Repeat administration resulted in the same abandonment classification in 15 of the 15 patients (100%). There were some differences in responses to the question regarding frequency of device use. The same frequency of use category was used in 12 of 15 (80%) cases. For all 3 cases which were classified differently in the second interview, the category used in the second interview was within one category of that used in the first (for example “daily” in the first interview and “several times per week” in the second).
While the rate of response among patients contacted by telephone and asked to complete the survey was very high, the number of patients who were actually reached by phone relative to the number who we attempted to contact was considerably lower. We estimate that approximately 50% of those patients who were called were actually reached. Two patients who were successfully contacted by phone refused to participate.
DISCUSSION
We found an overall abandonment rate of 19% in this study of low vision devices prescribed at outpatient clinical sites. This is similar to the rates previously found in other clinical settings and in other countries, including the U.S. VA hospital low vision rehabilitation program and university-based clinics in the U.K. and Canada. This study is the first of which we are aware investigating the abandonment of prescribed low vision devices in a non-veteran U.S. outpatient population. A recent large survey of U.S. low vision providers found that the vast majority were outpatient-based.13
There are important differences in the rehabilitation programs common in U.S. outpatient clinical settings and those in the Veterans Affairs program. One difference is the gender makeup of the populations, with the VA population being largely male. For instance, in the study of device use in the VA population by Watson et al., 97% of the patients surveyed were male.8 In the present study, 64% of the participants were female. However, we found no significant relationship between gender and device abandonment. Another important difference is that the amount and frequency of training in device use that patients received in VA programs is also considerably greater than is typically received in outpatient settings (an average of 32 hours per patient in the VA7 vs. only 10% of practitioners providing more than 3 hours per patient in outpatient settings14). In this study some patients (36%) did receive training, however no standard training protocol was used and thorough documentation of the nature of the training performed was not available. Prospective studies of device abandonment which include standardization of training variables (type, amount etc.) should be undertaken in order to more fully characterize the role training plays in determining usage of low vision devices. It should also be noted that poorer vision among patients in the VA population should be considered when comparing the respective abandonment rates. For instance, Watson et al.8 reported that 37% of their sample was 20/80 or better, 41% was 20/80-20/200, and 23% was 20/200-20/800. In the present study, 48% of patients were better than 20/80, 44% were between 20/80 and 20/100, and 8% were worse than 20/200.
Of the factors that could lead to abandonment we investigated, the only factor that was significantly related to abandonment of a device was the notation in the patient’s medical record of a non-central visual field defect. Those who had a noted non-central visual field defect were more likely to have abandoned a prescribed device. Loss of visual field has been shown to be related to decreased vision-related and health-related quality of life in many studies. For instance, Ringsdorf et al. found that severity of visual field defects were related to reduced visual functioning, including near vision subscale scores.15 Health-related quality of life has been shown to be negatively affected by visual field loss.16–21 It may be that some of these impacts of visual field loss on other aspects of the patient’s life might make abandonment of a low vision device more likely.
Because this was a retrospective study, we were unable to study the effects of several potentially important factors on device abandonment. For instance, cognitive status and living arrangements were not uniformly documented and could not be analyzed but may very well play an important role in whether a prescribed device is used frequently. Similarly, vision data such as contrast sensitivity and carefully plotted visual fields were not available for many of the patients studied.
There are other limitations to this study. In many cases, the telephone survey regarding device usage was administered by the prescribing practitioner. This may have resulted in an overestimation of usage rates, as some patients may have been inclined to answer in a way that they thought would please the prescriber. Also, the patients who were contacted were not randomly selected. Although an attempt was made to contact all patients identified during the chart review who had been prescribed a low vision device which met the criteria determined before beginning the study, it is possible that the selection of patients who were contacted resulted in some bias.
Supplementary Material
Acknowledgments
This work was supported by grants from the National Eye Institute (5T32EY013359-10) and the National Center for Research Resources (1 UL1 RR024975), an American Optometric Foundation Ezell fellowship, an unrestricted grant from Research to Prevent Blindness to Vanderbilt Ophthalmology, and the American Optometric Association/American Academy of Optometry Summer Research Institute. The authors would like to thank Joan Stelmack, Robert Massof, and Mark Bullimore for comments on the manuscript and study design. Portions of this work were presented at the meetings of the Association for Research in Vision and Ophthalmology (Ft. Lauderdale, FL May 2010) and the American Academy of Optometry (Orlando, 2009).
APPENDIX
The Appendix is available at [LWW insert link].
References
- 1.Congdon N, O'Colmain B, Klaver CC, Klein R, Munoz B, Friedman DS, Kempen J, Taylor HR, Mitchell P. Causes and prevalence of visual impairment among adults in the United States. Arch Ophthalmol. 2004;122:477–85. doi: 10.1001/archopht.122.4.477. [DOI] [PubMed] [Google Scholar]
- 2.Massof RW. A model of the prevalence and incidence of low vision and blindness among adults in the U. S Optom Vis Sci. 2002;79:31–8. doi: 10.1097/00006324-200201000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Trauzettel-Klosinski S. Rehabilitation for visual disorders. J Neuroophthalmol. 2010;30:73–84. doi: 10.1097/WNO.0b013e3181ce7e8f. [DOI] [PubMed] [Google Scholar]
- 4.Hooper P, Jutai JW, Strong G, Russell-Minda E. Age-related macular degeneration and low-vision rehabilitation: a systematic review. Can J Ophthalmol. 2008;43:180–7. doi: 10.3129/i08-001. [DOI] [PubMed] [Google Scholar]
- 5.Robillard N, Overbury O. Quebec model for low vision rehabilitation. Can J Ophthalmol. 2006;41:362–6. doi: 10.1139/I06-022. [DOI] [PubMed] [Google Scholar]
- 6.Fonda G. Report of five hundred patients examined for low vision. AMA Arch Ophthalmol. 1956;56:171–5. doi: 10.1001/archopht.1956.00930040179002. [DOI] [PubMed] [Google Scholar]
- 7.Watson GR, De l'Aune W, Stelmack J, Maino J, Long S. National survey of the impact of low vision device use among veterans. Optom Vis Sci. 1997;74:249–59. doi: 10.1097/00006324-199705000-00019. [DOI] [PubMed] [Google Scholar]
- 8.Watson GR, De l'Aune W, Long S, Maino J, Stelmack J. Veterans' use of low vision devices for reading. Optom Vis Sci. 1997;74:260–5. doi: 10.1097/00006324-199705000-00020. [DOI] [PubMed] [Google Scholar]
- 9.Goodrich GL, Mehr EB, Darling NC. Parameters in the use of CCTV's and optical aids. Am J Optom Physiol Opt. 1980;57:881–92. doi: 10.1097/00006324-198012000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Harper R, Doorduyn K, Reeves B, Slater L. Evaluating the outcomes of low vision rehabilitation. Ophthalmic Physiol Opt. 1999;19:3–11. doi: 10.1046/j.1475-1313.1999.00411.x. [DOI] [PubMed] [Google Scholar]
- 11.Leat SJ, Fryer A, Rumney NJ. Outcome of low vision aid provision: the effectiveness of a low vision clinic. Optom Vis Sci. 1994;71:199–206. doi: 10.1097/00006324-199403000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Elliott AJ. Poor vision and the elderly—a domiciliary study. Eye (Lond) 1989;3(Pt. 3):365–9. doi: 10.1038/eye.1989.53. [DOI] [PubMed] [Google Scholar]
- 13.Owsley C, McGwin G, Jr, Lee PP, Wasserman N, Searcey K. Characteristics of low-vision rehabilitation services in the United States. Arch Ophthalmol. 2009;127:681–9. doi: 10.1001/archophthalmol.2009.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kammer R, Sell C, Jamara RJ, Kollbaum E. Survey of optometric low vision rehabilitation training methods for the moderately visually impaired. Optometry. 2009;80:185–92. doi: 10.1016/j.optm.2008.10.015. [DOI] [PubMed] [Google Scholar]
- 15.Ringsdorf L, McGwin G, Jr, Owsley C. Visual field defects and vision-specific health-related quality of life in African Americans and whites with glaucoma. J Glaucoma. 2006;15:414–8. doi: 10.1097/01.ijg.0000212252.72207.c2. [DOI] [PubMed] [Google Scholar]
- 16.Gutierrez P, Wilson MR, Johnson C, Gordon M, Cioffi GA, Ritch R, Sherwood M, Meng K, Mangione CM. Influence of glaucomatous visual field loss on health-related quality of life. Arch Ophthalmol. 1997;115:777–84. doi: 10.1001/archopht.1997.01100150779014. [DOI] [PubMed] [Google Scholar]
- 17.Papageorgiou E, Hardiess G, Schaeffel F, Wiethoelter H, Karnath HO, Mallot H, Schoenfisch B, Schiefer U. Assessment of vision-related quality of life in patients with homonymous visual field defects. Graefes Arch Clin Exp Ophthalmol. 2007;245:1749–58. doi: 10.1007/s00417-007-0644-z. [DOI] [PubMed] [Google Scholar]
- 18.McKean-Cowdin R, Varma R, Wu J, Hays RD, Azen SP. Severity of visual field loss and health-related quality of life. Am J Ophthalmol. 2007;143:1013–23. doi: 10.1016/j.ajo.2007.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sherwood MB, Garcia-Siekavizza A, Meltzer MI, Hebert A, Burns AF, McGorray S. Glaucoma's impact on quality of life and its relation to clinical indicators. A pilot study. Ophthalmology. 1998;105:561–6. doi: 10.1016/S0161-6420(98)93043-3. [DOI] [PubMed] [Google Scholar]
- 20.Wandell PE, Lundstrom M, Brorsson B, Aberg H. Quality of life among patients with glaucoma in Sweden. Acta Ophthalmol Scand. 1997;75:584–8. doi: 10.1111/j.1600-0420.1997.tb00154.x. [DOI] [PubMed] [Google Scholar]
- 21.Stelmack J. Quality of life of low-vision patients and outcomes of low-vision rehabilitation. Optom Vis Sci. 2001;78:335–42. doi: 10.1097/00006324-200105000-00017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.