Abstract
Bisphenol A-glycidyl methacrylate (BisGMA) is monomer of dental filling composites, which can be released from these materials and cause adverse biologic effects in human cells. In the present work, we investigated genotoxic effect of BisGMA on human lymphocytes and human acute lymphoblastic leukemia cell line (CCRF-CEM) cells. Our results indicate that BisGMA is genotoxic for human lymphocytes. The compound induced DNA damage evaluated by the alkaline, neutral, and pH 12.1 version of the comet assay. This damage included oxidative modifications of the DNA bases, as checked by DNA repair enzymes EndoIII and Fpg, alkali-labile sites and DNA double-strand breaks. BisGMA induced DNA-strand breaks in the isolated plasmid. Lymphocytes incubated with BisGMA at 1 mM were able to remove about 50% of DNA damage during 120-min repair incubation. The monomer at 1 mM evoked a delay of the cell cycle in the S phase in CCRF-CEM cells. The experiment with spin trap—DMPO demonstrated that BisGMA induced reactive oxygen species, which were able to damage DNA. BisGMA is able to induce a broad spectrum of DNA damage including severe DNA double-strand breaks, which can be responsible for a delay of the cell cycle in the S phase.
Keywords: BisGMA, DNA damage, DNA repair, Reactive oxygen species, Cell cycle
Introduction
Dental filling composites are mixtures of materials that generally consist of an organic resin matrix, reinforcing inorganic filler and an agent that connects the filler and the resin matrix. The polymerizable matrix contains one or more base monomers such as bisphenol A-glycidyl methacrylate (BisGMA) and/or urethane dimethacrylate (UDMA), diluent co-monomers (2-hydroxyethylene methacrylate, HEMA; triethylene glycol dimethacrylate, TEGDMA) and various additives, like photoinitiators (e.g., camphoroquinone), co-initiators (e.g., dimethyl-aminobenzoic-acid-ester), inhibitor of polymerization (BHT) and photostabilizers (e.g., benzophenone).
Numerous studies indicate that various components may be released from composite restorations into the oral environment and may cause adverse local and systemic effects, like irritation to skin or eyes and gastrointestinal complaints (Mathias et al. 1979; Lonnroth and Shahnavaz 1997). In vitro studies revealed cytotoxic and genotoxic (Engelmann et al. 2004; Kleinsasser et al. 2004, 2006; Lee et al. 2006; Reichl et al. 2008; Poplawski et al. 2009, 2010; Pawlowska et al. 2010), mutagenic (Schweikl and Schmalz 1997; Arossi et al. 2010), estrogenic (Wada et al. 2004) and teratogenic (Schwengberg et al. 2005) effects of composite components. Dental composites may reach a millimolar concentration in the pulp, which can be high enough to be considered as potentially harmful for pulp cells and other cells in the human organism (Bouillaguet 2004). For example, HEMA leaching from dentin adhesives may reach concentrations as high as 1.5–8 mM (Bouillaguet et al. 1996). Similarly, the TEGDMA concentrations reaching the pulp could be around 4 mM (Noda et al. 2002). The diffusion of monomers through the dentin is facilitated by the microchannels present in its structure. After diffusion through the dentin, the monomers may migrate further into the bloodstream.
Previously, it was observed that BisGMA (Fig. 1) showed relevant enhancement of DNA migration of lymphocytes in the comet assay starting at 10−4 M with a maximum at 2.5 × 10−2 M (Kleinsasser et al. 2004). It demonstrated the highest DNA migration in comparison with HEMA, TEGDMA, and UDMA. It was also shown that BisGMA at the EC50 concentration of 0.09 mM evoked the highest rate of DNA double-strand breaks formation in human gingival fibroblasts (HGF) (Urcan et al. 2010). In the present study, we investigated the genotoxic effect of BisGMA in human lymphocytes in detail. We employed the comet assay at three different pHs: >13 version revealing DNA single- and double-strand breaks as well as alkali labile sites, the pH 12.1 version eliminating the expression of alkali labile sites and the pH 9 version revealing only DNA double-strand breaks. In order to assess whether oxidative DNA damage may contribute to BisGMA-induced lesions, we employed two enzymes: endonuclease III (EndoIII) and formamidopyrimidine-DNA glycosylase (Fpg). EndoIII converts oxidized pyrimidines into strand breaks, which can be detected by the comet assay (Collins et al. 1993). Fpg is a glycosylase initiating base excision repair in E. coli. It recognizes and removes 7,8-dihydro-8-oxoguanine (8-oxoguanine), the imidazole ring-opened purines 2,6-diamino-4-hydroxy-5-formamidopyrimidine (Fapy-Gua) and 4,6-diamino-5-formamido-pyrimidine (Fapy-Ade) as well as small amounts of 7,8-dihydro-8-oxoadenine (8-oxoadenine) (Krokan et al. 1997). The removing of specific modified bases from DNA by this enzyme leads to apurinic or apyrimidinic sites, which are subsequently cleaved by its AP-lyase activity giving a gap in the DNA strand, which can be detected by the comet assay (Evans et al. 1995). The kinetics of DNA damage repair was also measured. In order to evaluate the involvement of free radicals in the genotoxicity of BisGMA, we pre-treated the cells with nitrone spin trap—DMPO. Moreover, we checked the ability of BisGMA to DNA damage directly by using the plasmid relaxation assay. We used the cancer cells line—human acute lymphoblastic leukemia cell line (CCRF-CEM) to analysis of BisGMA-induced changes in the cell cycle.
Fig. 1.
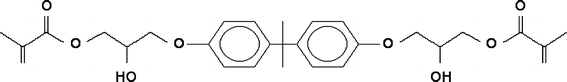
Structure of BisGMA
Materials and methods
Chemicals
Bisphenol A-glycidyl methacrylate (BisGMA) (CAS number 1565-94-2), 5,5-dimethyl-1-pyrroline N-oxide (DMPO), low-melting-point (LMP) and normal-melting-point (NMP) agarose, phosphate-buffered saline (PBS), DAPI (4′,6-diamidino-2-phenylindole), fetal bovine serum (FBS), penicillin, streptomycin and hydrogen peroxide were purchased from Sigma–Aldrich Co. (St. Louis, MO, USA). Plasmid DNA purification kit was provided by EURx (Gdansk, Poland). Cell viability and cell cycle kits were purchased in BD Bioscience (San Jose, CA, USA). All other chemicals were of the highest commercial grade available.
Cells
Lymphocytes were isolated from peripheral blood obtained from three, young (23–35 years), non-smoking men by centrifugation in a density gradient of Gradisol L (15 min, 280×g, 4°C).
Human acute lymphoblastic leukemia cell line (CCRF-CEM) cells were grown in RPMI 1640 medium supplemented with 10% FBS, 2 mM l-glutamine, 100 IU/ml penicillin, and 100 μg/ml streptomycin in the presence of a 5% CO2 atmosphere at 37°C.
E. coli cells, strain DH5α cells with pUC19 plasmid, were grown in a LB broth at 37°C overnight.
Cell treatment
BisGMA was taken from stock ethanolic solution (1 M) and added to the suspension of the cells in RPMI 1640 medium to give final concentrations of 0.015, 0.03, 0.06, 0.125, 0.25, 0.5, and 1 mM. Lymphocytes were incubated with BisGMA for 1 h at 37°C. The final concentration of ethanol in each sample was equal, i.e. 0.9%. The control cells received the medium and ethanol at 0.9%. Each experiment included a positive control, which was hydrogen peroxide at 20 μM applied for 10 min at 4°C. In spin trapping experiments, the incubation with BisGMA was preceded by addition of DMPO to a final concentration of 100 μM.
In the case of lymphocytes, each experiment was performed on the cells obtained from blood of three different donors.
Cell viability
The BD Cell Viability Kit was used to determine the cell viability. The kit contains thiazole orange (TO) solution to stain all cells and propidium iodide (PI) to stain dead cells. Aliquots of 2 μl of TO and 1 μl of PI were added to 1 ml of cell suspension containing 5 × 105 cells, producing the final staining concentrations of 84 nM and 4.3 μM, respectively. The mixture was gently shaken and incubated for 5 min in room temperature to allow both dyes to enter the cells. The samples were acquired on a LSRII (Becton–Dickinson, San Jose, USA) flow cytometer equipped with 488 nm laser excitation and BD FACSDiva software v. 4.1.2. 5 × 105 cells were analyzed in each experiment repeated in triplicate.
Comet assay
The comet assay was performed under alkaline conditions essentially according to the procedure of Singh et al. (1988) with modifications (Collins et al. 1993; Evans et al. 1995) as described previously (Blasiak and Kowalik 2000). A freshly prepared suspension of the cells (1–3 × 105 cells/ml) in 0.75% LMP agarose dissolved in PBS was spread onto microscope slides precoated with 0.5% NMP agarose. The cells were then lysed for 1 h at 4°C in a buffer consisting of 2.5 M NaCl, 100 mM EDTA, 1% Triton X-100, 10 mM Tris, pH 10. After the lysis, the slides were placed in an electrophoresis unit, DNA was allowed to unwind for 20 min in the solution consisting of 300 mM NaOH and 1 mM EDTA, pH > 13. Electrophoresis was conducted in the electrophoretic solution containing 30 mM NaOH and 1 mM EDTA, pH > 13 at ambient temperature of 4°C (the temperature of the running buffer did not exceed 12°C) for 20 min at an electric field strength of 0.73 V/cm (28 mA). The slides were then washed in water, drained, and stained with 2 μg/ml DAPI and covered with cover slips. To prevent additional DNA damage, all the steps described above were conducted under dimmed light or in the dark.
The assay at pH 12.1 was performed essentially according to the same procedure as the alkaline version except the pH value. In the neutral version, electrophoresis was run in a buffer consisting of 100 mM Tris and 300 mM sodium acetate at pH adjusted to 9.0 by glacial acetic acid (Singh and Stephens 1997). Electrophoresis was conducted for 60 min, after a 20-min equilibrium period, at 12 V (100 mA) at 4°C.
The comets were observed at 200× magnification in an Eclipse fluorescence microscope (Nikon, Tokyo, Japan) attached to COHU 4910 video camera (Cohu, San Diego, CA, USA) equipped with a UV-1 filter block (an excitation filter of 359 nm and a barrier filter of 461 nm) and connected to a personal computer-based image analysis system Lucia-Comet v. 4.51 (Laboratory Imaging, Praha, Czech Republic). Fifty images were randomly selected from each sample.
The mean value of tail DNA (%) in a particular sample was taken as an index of DNA damage in this sample and was used to display the results of all experiments.
DNA repair
To examine DNA repair by the comet assay, lymphocytes after treatment with BisGMA were washed and resuspended in a fresh, RPMI 1640 medium preheated to 37°C. Aliquots of the cell suspension were taken immediately (“time zero”) and at 30, 60, and 120 min later. Placing the samples in an ice bath stopped DNA repair.
Oxidative DNA damage
The slides after cell lysis were washed three times (5 min, 4°C) in an enzyme buffer containing 40 mM HEPES–KOH, 0.1 M KCl, 0.5 mM EDTA, and 0.2 mg/ml bovine serum albumin, pH 8.0. The slides were then drained. Aliquots of 30 μl of EndoIII or Fpg at 1 μg/ml in the buffer were applied to the agarose on slides and incubation for 30 min at 37°C was performed (Collins et al. 1993; Evans et al. 1995). The slides were processed as describe above.
Cell cycle
The CycleTEST PLUS DNA Reagent Kit was used to determine the DNA index (DI) and cell cycle phase distributions. The method involved dissolving of the cell membrane lipids, eliminating the cell cytoskeleton with trypsin, digesting the cellular RNA and stabilizing the chromatin with spermine. Propidium iodine was bound to isolated nuclei, which were then run on the LSRII flow cytometer, emitting fluorescence in the range of 580–650 nm and equipped with a 585/42 filter to analyze the light emitting between 564 and 606 nm by the stained cells. The DI was obtained by dividing the mean of the relative content of the exposed G0/G1 population by the mean of the control G0/G1 population.
In the cell cycle experiment, we used highly proliferating cells, human acute lymphoblastic leukemia cell line (CCRF-CEM) cells. Suspension of cells was washed three times in buffer solution, adjusted to the concentration of 106/ml and then stained according to the manufacturer instruction. Results were analyzed by CellFIT software.
Plasmid relaxation assay
pUC19 plasmid were isolated from DH5α E. coli cells with Genemtrix Plasmid Miniprep DNA Purification Kit (EURx, Gdansk, Poland) according to the manufacturer’s instruction. The plasmid was exposed to 200 μM H2O2 and 20 μM FeCl3 (Fenton reaction). We performed this reaction as a positive control to check the migration of the pUC19 plasmid multimeric forms (supercoiled (SC), open circular (OC) and linear (L)). Hydroxyl radical, which was generated in Fenton reaction, induced strand breaks in DNA and caused the relaxation of supercoiled plasmid. Structural differences between supercoiled, open circular, and linear forms of the plasmid accounted for their different electrophoretic mobility. Plasmid samples at 250 ng/μl were subjected to 1% agarose gel electrophoresis carried out in TAE (Tris–Acetate-EDTA) buffer. The gel was stained with ethidium bromide (0.5 μg/ml), and the plasmid DNA was visualized under ultraviolet light (302 nm) and scanned by a CCD camera, and densitometry analysis was performed with the GeneTools by Syngene (Cambridge, UK) software.
Data analysis
The values of the comet assay in this study were expressed as mean ± SEM from three experiments, i.e., data from three experiments were pooled and the statistical parameters were calculated. The data obtained from cell viability, cell cycle, and DNA damage in the plasmid as mean ± SD. The differences between samples were evaluated by applying the Student’s t test.
Results
Cell viability
BisGMA evoked the significant decrease (P < 0.05) in the viability of lymphocytes only at maximal applied concentration equal to 1 mM (Fig. 2).
Fig. 2.
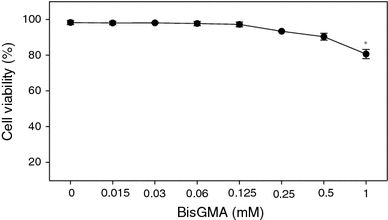
Cell viability of human peripheral blood lymphocytes in the presence of BisGMA measured by flow cytometry with thiazole orange and propidium iodide. The figure shows mean results from three independent experiments. Error bars denote standard deviation; *P < 0.05 when compared with the control (0.9% ethanol)
DNA damage
The distributions of lymphocytes exposed to BisGMA according to their DNA damage (DNA in comet tail) measured in the alkaline version of the comet assay are displayed in Fig. 3. In the control, we observed the large fraction of comets, which had DNA damage between 0 and 5% and the small fraction of comets, which had DNA damage between 5 and 10%. After incubation of the cells with increasing concentrations of BisGMA, we observed the increase of the comet fractions number with DNA damage. At maximal concentration of BisGMA, 1 mM, we noticed the most abundant fraction of the comets (40%), which had DNA damage between 20 and 25%. In lymphocytes exposed to hydrogen peroxide (positive control), the most abundant fraction (40%) had DNA damage between 10 and 15%.
Fig. 3.
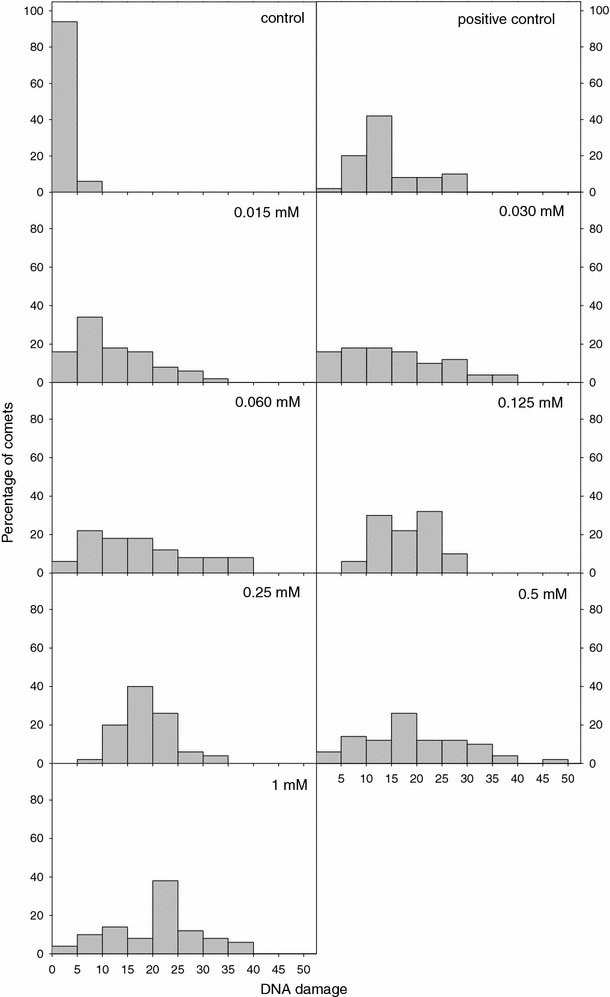
Histograms of the distribution of DNA damage in the comet alkaline version of lymphocytes incubated for 1 h at 37°C with BisGMA at various concentrations when compared with the control (0.9% ethanol). The results for positive control (20 μM H2O2 at 4°C for 10 min) are also presented. The number of cells scored in each treatment was 50. The figure shows mean results from three independent experiments
Figure 4 displays DNA damage of lymphocytes exposed to BisGMA and analyzed by the comet assay in three versions of pHs: >13, pH 9, and pH 12.1. We observed significant differences between DNA damage at pH > 13 and pH 12.1 versions (P < 0.001), which indicates that alkali-labile sites in DNA contributed to observed increase in DNA damage in the presence of BisGMA. We also observed significant increase at pH 9, which indicates that DNA double-strand breaks also contributed to observed increase DNA damage after incubation with BisGMA. This experiment indicates that BisGMA can induce alkali-labile sites and double-strand breaks in DNA of human lymphocytes.
Fig. 4.
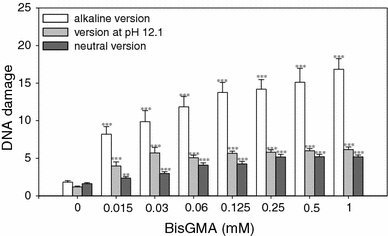
DNA damage, measured as the comet tail DNA of lymphocytes incubated for 1 h at 37°C with BisGMA and analyzed by the comet assay in the alkaline (white), neutral (gray) or pH 12.1 (black) version. The results for positive control were: at pH > 13 16.19 ± 2.08; at pH 12.1 7.59 ± 1.10, and at pH 9 6.05 ± 0.53. The number of cells scored in each treatment was 50. The figure shows mean results from three independent experiments. Error bars denote SEM. The concentration axis is not linear and distances between points are chosen arbitrarily; **P < 0.01; ***P < 0.001 when compared with the control (0.9% ethanol)
Induction of oxidized bases
Figure 5 shows DNA damage of lymphocytes exposed for 1 h at 37°C to BisGMA with post-treatment with EndoIII and Fpg. DNA originated from lymphocytes incubated at 0.015, 0.125, and 1 mM BisGMA and treated with EndoIII and Fpg showed significant increase in DNA damage compared with DNA without treatment with BisGMA. This indicates that oxidative modifications of the DNA bases play a role in the genotoxic action of BisGMA.
Fig. 5.

DNA damage, measured as the comet tail DNA of lymphocytes incubated for 1 h at 37°C with BisGMA and treated with EndoIII (white) or Fpg (gray) at 1 μg/ml. The value of comet tail DNA in the presence of either enzyme for all BisGMA concentrations was reduced by the value obtained in comet assay without any enzyme and the value for enzymatic buffer only. The number of cells scored in each treatment was 50. The figure shows mean results from three independent experiments. Error bars denote SEM. The concentration axis is not linear and distances between points are chosen arbitrarily; ***P < 0.001
DNA repair
Figure 6 shows DNA damage of lymphocytes exposed to BisGMA at 0.015 and 1 mM immediately after exposure and 30, 60, and 120 min thereafter. Lymphocytes were not able to repair all BisGMA-induced DNA damage. After incubation with BisGMA at 0.015 mM, the cells were able to repair about 65% DNA damage. After incubation with BisGMA at maximal concentration, 1 mM, the cells were able to restore about 53% of DNA damage.
Fig. 6.
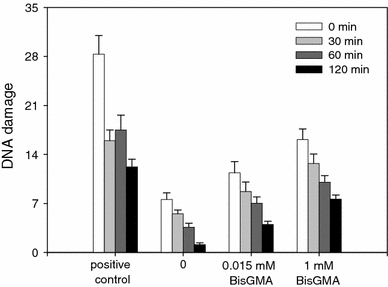
Time course of the repair of DNA damage, measured as the comet tail DNA, in lymphocytes treated for 1 h at 37°C with BisGMA at 0.015 and 1 mM. The number of cells scored for each treatment was 50. The figure shows mean results from three independent experiments. Error bars denote SEM. The statistical significance is not indicated for the sake of clarity
The cells exposed to 20 μM H2O2 for 10 min at 4°C (positive control) were able to repair about 57% DNA damage within the repair incubation time of 120 min (Fig. 6).
Effect of spin traps on DNA damage
To check whether free radicals could contribute to observed DNA damage, we pre-incubated lymphocytes with spin trap DMPO. To check the ability of DMPO to scavenge reactive oxygen species (ROS) in our experimental conditions, incubation of lymphocytes with H2O2 at concentration of 20 μM for 10 min at 4°C in the presence or in the absence of DMPO was performed. A significant decrease (P < 0.001) in DNA damage was observed after incubation of the cells with H2O2 (positive control) and DMPO in comparison with cells not treated with the trap (18.02 ± 1.31 vs. 1.44 ± 0.23). We observed a significant decrease (P < 0.001) in DNA damage induced by BisGMA in human lymphocytes in the presence of DMPO. This indicates that BisGMA induces ROS, which cause DNA damage (Fig. 7).
Fig. 7.
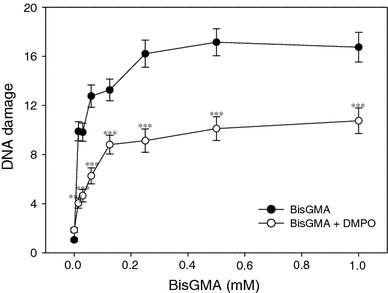
DNA damage, measured as the comet tail DNA of lymphocytes incubated for 1 h at 37°C with BisGMA in the presence of DMPO at 100 μM. The number of analyzed cells in each treatment was 50. The figure shows mean results from three independent experiments. Error bars denote SEM; ***P < 0.001
Cell cycle
In order to determine whether BisGMA has an influence on the progression of the cell cycle, human acute lymphoblastic leukemia cell line (CCRF-CEM) cells were exposed to BisGMA at increasing concentrations. BisGMA evoked an increase in the S cell population accompanied by a decrease in G2/M cell population (Fig. 8).
Fig. 8.
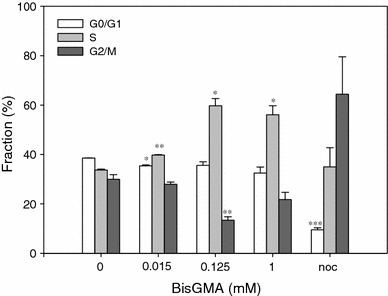
Cell cycle analysis in CCRF-CEM cells exposed to BisGMA for 1 h at 37°C. Percentage of cells in G0/G1 (white bars), S (light gray bars) and G2/M (dark gray bars) stage of cell cycle after treatment with BisGMA was presented. Nocodazole (noc) was used as a positive control. Data are expressed as means of three independent experiments, error bars denote SD; *P < 0.05; **P < 0.01; ***P < 0.001
DNA damage in vitro
BisGMA introduced DNA breaks to isolated DNA at the highest used concentration, as assessed by the plasmid relaxation assay (Fig. 9). The plasmid used in our experiment was sensitive to DNA-breaking agents as checked by Fenton reaction.
Fig. 9.
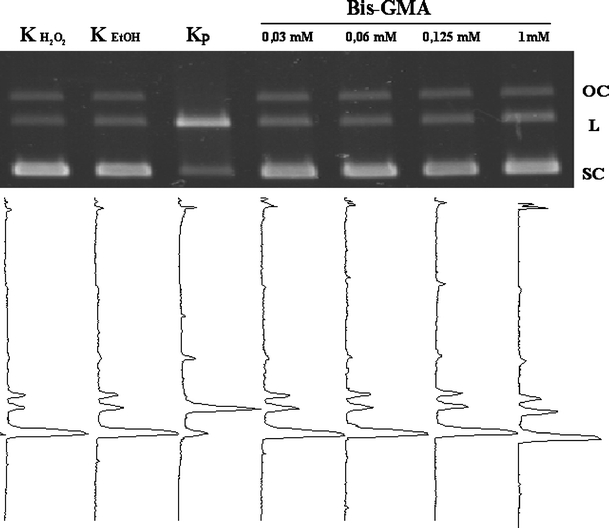
DNA damage induced by BisGMA in the isolated pUC19 plasmid. The picture shows three forms of the plasmid: linear (L), open circular (OC) and super coiled (SC) exposed to BisGMA for 1 h at 37°C at indicated concentrations or Fenton reaction (positive control). The samples were separated on a 1% agarose gel, stained with ethidium bromide, and visualized in UV light
Discussion
Bisphenol A-glycidyl methacrylate (BisGMA) is used as to build the three-dimensional structure of the dental resin composites. The resin composites have been proposed as an alternative to amalgam, ceramic, and gold restorations due to esthetic and toxicologic considerations. However, numerous studies indicated that various components of the resin composites, like BisGMA, UDMA, and TEGDMA, may be released from composite into the oral environment and induced a variety of adverse biologic effects (Geurtsen 1998; Bouillaguet 2004). The release of monomers remains at a high level for a long time (7–28 days) after polymerization. A higher amount of BisGMA was eluted compared to TEGDMA. The 40 s that are usually used for the polymerization of resin composites seems insufficient in order to prevent a high release of monomers (Polydorou et al. 2007).
We showed that BisGMA is genotoxic for human lymphocytes. The compound induced mainly DNA alkali-labile sites and DNA double-strand breaks (Fig. 4). In our study, BisGMA was able to cause DNA-strand breaks in the isolated DNA plasmid (Fig. 9). This suggests that BisGMA can directly interact with DNA.
Reichl et al. (2008) showed that the addition of hydrogen peroxide (0.06 or 0.1 mM) resulted in a toxicity potentiation of TEGDMA and UDMA, but not of HEMA and BisGMA, on human gingival fibroblasts (HGF) and human pulp fibroblasts (HPF). Under physiologic conditions, the antioxidative enzymes catalase and glutathione peroxidase are able to maintain the concentration of hydrogen peroxide in cells on level of about 10−7 M. Otherwise damage of the antioxidative systems and/or increased oxidative stress can lead to dramatic endogenous increase of hydrogen peroxide in the cells and thereby can lead to cell damage (Reichl et al. 2008). It was shown that BisGMA at concentrations >0.1 mM caused an extreme depletion of the intracellular GSH pool as well as apoptosis in HGF (Engelmann et al. 2004). Moreover, it was found that BisGMA significantly influences the activity of cytochrome P450 (Cannon et al. 2000). An elevated activity of this mitochondrial enzyme complex may by associated with an increase of the intracellular concentration of ROS, which subsequently deplete the cells’ pool of detoxifying glutathione (Engelmann et al. 2004; Sapone et al. 2003). We showed that lymphocytes exposed to BisGMA in the presence of spin trap, DMPO, had smaller DNA damage than the cells exposed without DMPO (Fig. 7). This finding indicates that BisGMA induces ROS, which damage DNA. We also speculate that oxidative modifications of DNA recognized by EndoIII and Fpg, which we noticed after incubation with BisGMA (Fig. 5), could be a result of ROS action.
Probably, the disruption of stable redox balance between ROS and antioxidant protective systems can be responsible for cell-cycle arrest induced by BisGMA (Fig. 8). BisGMA evoked an increase in the S cell population accompanied by a decrease in G2/M cell population. DNA damage can block the progression of cell cycle giving more time for DNA repair. Schweikl et al. (2005) investigated the effect of TEGDMA on the cell cycle and showed that this compound caused cell cycle delays through p53-dependent and independent pathways in various mammalian cell lines, including pulp fibroblasts. N-acetylcysteine protected mammalian cells from the cell cycle delay induced by TEGDMA and HEMA (Schweikl et al. 2007). Previously, it was shown that BisGMA evaluated to produce DNA damage but without cell-cycle effects, suggesting that DNA repair mechanisms were effective (Kostoryz et al. 2004). In our studies, the cells were able to restore about 53% of DNA damage after incubation with maximal, 1 mM concentration of BisGMA (Fig. 6). This suggests that DNA damage may be persistent at about 50% and potentially dangerous for the cells.
Conclusion
BisGMA is able to induce a broad spectrum of DNA damage including severe DNA double-strand breaks in human lymphocytes. The monomer can also directly interact with DNA and introduce DNA-strand breaks. BisGMA-induced DNA damage can be responsible for a delay of the cell cycle in the S phase.
Acknowledgments
This work was supported by the grant NN 403 188 134 of Ministry of Science and Higher Education. The authors thank Malgorzata Stanczyk for the gift of CCRF-CEM cell line and Dominika Ksiazek for her technical assistance.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- Arossi GA, Lehmann M, Dihl RR, Reguly ML, de Andrade HH. Induced DNA damage by dental resin monomers in somatic cells. Basis Clin Pharmacol Toxicol. 2010;106:124–129. doi: 10.1111/j.1742-7843.2009.00479.x. [DOI] [PubMed] [Google Scholar]
- Blasiak J, Kowalik J. A comparison of the in vitro genotoxicity of tri- and hexavalent chromium. Mutat Res. 2000;469:135–145. doi: 10.1016/s1383-5718(00)00065-6. [DOI] [PubMed] [Google Scholar]
- Bouillaguet S. Biological risks of resin-based materials to the dentin–pulp complex. Crit Rev Oral Biol Med. 2004;15:47–60. doi: 10.1177/154411130401500105. [DOI] [PubMed] [Google Scholar]
- Bouillaguet S, Wataha JC, Hanks CT, Ciucchi B, Holtz J. In vitro cytotoxicity and dentin permeability of HEMA. J Endod. 1996;22:244–248. doi: 10.1016/S0099-2399(06)80141-X. [DOI] [PubMed] [Google Scholar]
- Cannon MJ, Kostoryz E, Russo KA, Smith RE, Yourtee DM. Bisphenol A and its biomaterial monomer derivatives alteration of in vitro cytochrome P450 metabolism in rat, minipiug and human. Biomacromolecules. 2000;1:656–664. doi: 10.1021/bm005564+. [DOI] [PubMed] [Google Scholar]
- Collins AR, Duthie SJ, Dobson VL. Direct enzymatic detection of endogenous base damage in human lymphocyte DNA. Carcinogenesis. 1993;14:1733–1735. doi: 10.1093/carcin/14.9.1733. [DOI] [PubMed] [Google Scholar]
- Engelmann J, Janke V, Volk J, Leyhausen G, Von Neuhoff N, Schlegelberger B, Geurtsen W. Effects of BisGMA on glutathione metabolism and apoptosis in human gingival fibroblasts in vitro. Biomaterials. 2004;25:4573–4580. doi: 10.1016/j.biomaterials.2003.11.048. [DOI] [PubMed] [Google Scholar]
- Evans MD, Podmore ID, Daly GJ, Perrett D, Lunec J, Herbert KE. Detection of purine lesions in cellular DNA using single cell gel electrophoresis with Fpg protein. Biochem Soc Trans. 1995;23:434S. doi: 10.1042/bst023434s. [DOI] [PubMed] [Google Scholar]
- Geurtsen W. Substances released from dental composites and glass ionomer cement. Eur J Oral Sci. 1998;106:687–695. doi: 10.1046/j.0909-8836.1998.eos10602ii04.x. [DOI] [PubMed] [Google Scholar]
- Kleinsasser NH, Wallner BC, Harreus UA, Kleinjung T, Folwaczny M, Hickel R, Kehe K, Reichl F-X. Genotoxicity and cytotoxicity of dental materials in human lymphocytes as assessed by the single cell microgel electrophoresis (comet) assay. J Dent. 2004;32:229–234. doi: 10.1016/j.jdent.2003.11.002. [DOI] [PubMed] [Google Scholar]
- Kleinsasser NH, Schmid K, Sassen AW, Harreus UA, Staudenmaier R, Folwaczny M, Glas J, Reichl F-X. Cytotoxic and genotoxic effects of resin monomers in human salivary gland tissue and lymphocytes as assessed by the single cell microgel electrophoresis (Comet) assay. Biomaterials. 2006;27:1762–1770. doi: 10.1016/j.biomaterials.2005.09.023. [DOI] [PubMed] [Google Scholar]
- Kostoryz EL, Wetmore LA, Brockmann WG, Yourtee DM, Eick JD. Genotoxicity assessment of oxirane-based dental monomers in mammalian cells. J Biomed Mater Res. 2004;68A:660–667. doi: 10.1002/jbm.a.20077. [DOI] [PubMed] [Google Scholar]
- Krokan HE, Standal R, Slupphaug G. DNA glycosylases in the base excision repair. Biochem J. 1997;325:1–16. doi: 10.1042/bj3250001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee DH, Lim B-S, Lee Y-K, Ahn S-J, Yang H-C. Involvement of oxidative stress in mutagenicity and apoptosis caused by dental resin monomers in cell cultures. Dent Mater. 2006;22:1086–1092. doi: 10.1016/j.dental.2005.09.002. [DOI] [PubMed] [Google Scholar]
- Lonnroth EC, Shahnavaz H. Use of polymer materials in dental clinics, case study. Swed Dent J. 1997;21:149–159. [PubMed] [Google Scholar]
- Mathias CGT, Caldwell TM, Maibach HI. Contact-dermatitis and gastro-intestinal symptoms from hydroxyethylmethacrylate. Br J Dermatol. 1979;100:447–449. doi: 10.1111/j.1365-2133.1979.tb01648.x. [DOI] [PubMed] [Google Scholar]
- Noda M, Wataha JC, Kaga M, Lockwood PE, Volkmann KR, Sano H. Components of dentinal adhesives modulate heat shock protein 72 expression in heat-stressed THP-1 human monocytes at sublethal concentrations. J Dent Res. 2002;81:265–269. doi: 10.1177/154405910208100408. [DOI] [PubMed] [Google Scholar]
- Pawlowska E, Poplawski T, Ksiazek D, Szczepanska J, Blasiak J. Genotoxicity and cytotoxicity of 2-hydroxyethyl methacrylate. Mutat Res. 2010;696:122–129. doi: 10.1016/j.mrgentox.2009.12.019. [DOI] [PubMed] [Google Scholar]
- Polydorou O, Trittler R, Hellwig E, Kummerer K. Elution of monomers from two conventional dental composite materials. Dent Mater. 2007;23:1535–1541. doi: 10.1016/j.dental.2006.12.011. [DOI] [PubMed] [Google Scholar]
- Poplawski T, Pawlowska E, Wisniewska-Jarosinska M, Ksiazek D, Wozniak K, Szczepanska J, Blasiak J. Cytotoxicity and genotoxicity of glycidyl methacrylate. Chem Biol Interact. 2009;180:69–78. doi: 10.1016/j.cbi.2009.02.001. [DOI] [PubMed] [Google Scholar]
- Poplawski T, Loba K, Pawlowska E, Szczepanska J, Blasiak J. Genotoxicity of urethane dimethacrylate, a tooth restoration component. Toxicol In Vitro. 2010;24:854–862. doi: 10.1016/j.tiv.2009.12.004. [DOI] [PubMed] [Google Scholar]
- Reichl F-X, Seiss M, Marquardt W, Kleinsasser N, Schweikl H, Kehe K, Hickel R. Toxicity potentiation by H2O2 with components of dental restorative materials on human oral cells. Arch Toxicol. 2008;82:21–28. doi: 10.1007/s00204-007-0226-1. [DOI] [PubMed] [Google Scholar]
- Sapone A, Affato A, Canistro D, Broccoli M, Trespidi S, Pozzetti L, Biagi CL, Cantelli-Forti G, Paolini M. Induction and suppression of cytochrome P450 isoenzymes and generation of oxygen radicals by procymidone in liver, kidney and lung of CD1 mice. Mutat Res. 2003;527:67–80. doi: 10.1016/S0027-5107(03)00055-1. [DOI] [PubMed] [Google Scholar]
- Schweikl H, Schmalz G. Glutaraldehyde-containing dentin bonding agents are mutagens in mammalian cells in vitro. J Biomed Mater Res. 1997;36:284–288. doi: 10.1002/(SICI)1097-4636(19970905)36:3<284::AID-JBM2>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- Schweikl H, Altmannberger I, Hanser N, Hiller KA, Bolay C, Brockhoff G, Spagnuolo G, Galler K, Schmalz G. The effect of triethylene glycol dimethacrylate on the cell cycle of mammalian cells. Biomaterials. 2005;26:4111–4118. doi: 10.1016/j.biomaterials.2004.10.026. [DOI] [PubMed] [Google Scholar]
- Schweikl H, Hartmann A, Hiller KA, Spagnuolo G, Bolay C, Brockhoff G, Schmalz G. Inhibition of TEGDMA and HEMA-induced genotoxicity and cell cycle arrest by N-acetylcysteine. Dent Mater. 2007;23:688–695. doi: 10.1016/j.dental.2006.06.021. [DOI] [PubMed] [Google Scholar]
- Schwengberg S, Bohlen H, Kleinsasser N, Kehe K, Seiss M, Walther UI, Hickel R, Reichl FX. In vitro embryotoxicity assessment with dental restorative materials. J Dent. 2005;33:49–55. doi: 10.1016/j.jdent.2004.08.001. [DOI] [PubMed] [Google Scholar]
- Singh NP, Stephens RE. Microgel electrophoresis: sensitivity, mechanisms and DNA electrostretching. Mutat Res. 1997;383:167–175. doi: 10.1016/s0921-8777(96)00056-0. [DOI] [PubMed] [Google Scholar]
- Singh NP, McCoy T, Tice RR, Schneider EL. A simple technique for quantitation of low levels of DNA damage in individual cells. Exp Cell Res. 1988;175:184–192. doi: 10.1016/0014-4827(88)90265-0. [DOI] [PubMed] [Google Scholar]
- Urcan E, Scherthan H, Styllou M, Haertel U, Hickel R, Reichl F-X. Induction of DNA double-strand breaks in primary gingival fibroblasts by exposure to dental resin composites. Biomaterials. 2010;31:2010–2014. doi: 10.1016/j.biomaterials.2009.11.065. [DOI] [PubMed] [Google Scholar]
- Wada H, Tarumi H, Imazato S, Narimatsu M, Ebisu S. In vitro estrogenicity of resin composites. J Dent Res. 2004;83:222–226. doi: 10.1177/154405910408300307. [DOI] [PubMed] [Google Scholar]


