Abstract
Purpose
When performing a laparoscopic assisted gastrectomy, a function-preserving gastrectomy is performed depending on the location of the primary gastric cancer. This study examined the incidence of lymph node metastasis by the lymph node station number by tumor location to determine the optimal extent of the lymph node dissection.
Materials and Methods
The subjects consisted of 1,510 patients diagnosed with gastric cancer who underwent a gastrectomy between 1996 and 2005. The patients were divided into three groups: upper, middle and lower third, depending on the location of the primary tumor. The lymph node metastasis patterns were analyzed in the total and early gastric cancer patients.
Results
In all patients, lymph node station numbers 1, 2, 3, 7, 10 and 11 metastases were dominant in the cancer originating in the upper third, whereas station numbers 4, 5, 6 and 8 were dominant in the lower third. In early gastric cancer patients, the station number of lymph nodes with a metastasis did not show a significant difference in stage pT1a disease. On the other hand, a metastasis in lymph node station number 6 was dominant in stage pT1b disease that originated in the lower third of the stomach.
Conclusions
When performing a laparoscopic-assisted gastrectomy for early gastric cancer, a limited lymphadenectomy is considered adequate during a function-preserving gastrectomy in mucosal (T1a) cancer. On the other hand, for submucosal (T1b) cancer, a number 6 node dissection should be performed when performing a pylorus preserving gastrectomy.
Keywords: Stomach neoplasms, Tumor location, Lymphatic metastasis
Introduction
Endoscopic resection has been performed widely in recent times to enable rapid recovery after early gastric cancer treatment. However, with the rate of lymph node metastasis reportedly close to 20% in cancer invading into the submucosal layer, endoscopic resection has its limitations.(1,2) Accordingly, for early gastric cancer invading beyond the middle of the submucosal layer (SM2) - itself a contraindication to endoscopic resection - open gastrectomy is required.(3,4)
When performing gastrectomy for early gastric cancer, where radical resection is viable, laparoscopic assisted gastrectomy which enables rapid recovery with less pain compared to open abdominal surgery is on the rise.(5) However, lymphadenectomy cannot be performed readily in a wide area with laparoscopic assisted gastrectomy compared to open gastrectomy due to limited surgical visibility and restricted surgical instrument mobility. Consequently, inadequate lymphadenectomy may result that negatively impacts on patient prognosis. On the other hand, if unnecessarily extensive lymphadenectomy is performed in a wide area, the incidence of post-surgical complications and morbidity increases.(6)
Recently, during laparoscopic assisted gastrectomy for early gastric cancer, function-preserving gastrectomy, such as proximal gastrectomy and pylorus-preserving gastrectomy, is performed in selected cases depending on the tumor location. In such cases, partial lymphadenectomy can be performed instead of extensive lymphadenectomy.(7,8)
However, the presence or absence of lymph node metastasis is very important for the prognosis of gastric cancer.(9) As such, the extent of lymphadenectomy should be determined considering the patient prognosis and post-surgical complications.
To date, laparoscopic assisted gastrectomy is limited to early gastric cancer. However, if the flow of lymph node metastasis depending on the gastric cancer location can be elucidated, guidelines on extending laparoscopic assisted gastrectomy to advanced gastric cancer may be suggested.
The aims of this study were to examine the incidence of metastasis in lymph node stations by primary gastric cancer location to determine the optimal extent of lymphadenectomy and function-preserving surgery in early gastric cancer patients.
Materials and Methods
Among 1,701 patients diagnosed with gastric cancer who underwent gastrectomy at our institution from 1996 to 2005, 22 patients developed invasion throughout the entire stomach were not classified and therefore excluded from this study. A total of 1,679 patients were included and classified into 3 groups, based on the location of the primary lesion: in the upper third (the upper third group), the middle third (the middle third group) and the lower third (the lower third group). The upper third designated cancer developed in the gastric cardia and fundus, the middle third designated cancer in the gastric body and the lower third designated cancer in the antrum and pylorus.
The upper third group was comprised of 188 patients, the middle third group was comprised of 605 patients, and the lower third group was comprised of 886 patients. Excluding 109 patients with tumor invasion into adjacent organs (T4) and 60 patients with unclassified extent of tumor invasion of the 3 aforementioned groups, 169 patients with cancer originated in the upper third, 561 patients in the middle third and 790 patients in the lower third were analyzed.
The clinico-pathological characteristics and patterns of lymph node metastasis were analyzed by the depth of tumor invasion. The tumor stage was classified according to the UICC, sixth edition.(10) Metastasis of the first and second tier lymph nodes was evaluated according to standards established by the Japanese Gastric Cancer Association (JGCA) to determine the extent of lymphadenectomy. To help decide surgical intervention by minimally invasive surgery, the depth of tumor invasion was subdivided into the mucosal and submucosal layers.
Regarding the pattern of lymph node metastasis of first tier lymph nodes based on the classification criteria of the JGCA for gastric cancer located in the upper third, the lymph node station numbers are defined as 1, 2, 3, 4sa and 4sb. In the middle third, the lymph node station numbers are defined as 1, 3, 4sb, 4d, 5 and 6 while that in the lower third are defined as 3, 4d, 5 and 6. As for second tier lymph nodes, the upper third lymph node station numbers are defined as 4d, 7, 8a, 9, 10 and 11, that of the middle third are defined as 7, 8a, 9, 11p and 12a, and that of the lower third are defined as 1, 7, 8a, 9, 11p, 12a and 14v.(11)
In this study, the total number of lymph node metastasis identified in 1,510 patients was 1,419. The number of lymph nodes metastasis higher than 12 were found in 29 patients, which corresponded to third tier lymph nodes or distant metastasis regardless of gastric cancer location and were thus excluded. As such, only 1,390 confirmed metastases in lymph node stations number 1 through to 11 were included in this study.
The station number of each lymph node was determined immediately after resection based on the location of blood vessels neighboring the stomach, the anatomical location in accordance with the standards established by the JGCA. Metastases in the classified lymph nodes and resected specimens were determined microscopically by specialist pathologists.
For statistical analysis, SPSS ver. 13.0 (SPSS Inc., Chicago, IL, USA) was used. For comparative analysis of the clinicopathological factors and the incidence of lymph node metastasis depending on the position of the tumor, Chi-square test and Student`s t-test was applied. A P-value under 0.05 (P<0.05) was defined as statistically significant.
Results
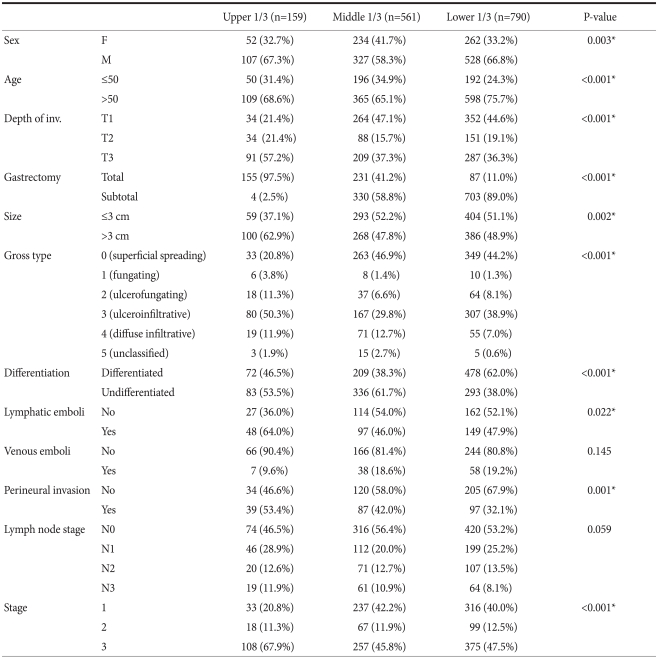
In total, 650 patients had pT1 disease with tumor invasion into the mucosal and submucosal layers, 273 patients had pT2 disease with invasion into the muscle and subserosal layers and 587 patients had pT3 disease with the invasion into the serosa. When tumors were classified based on location and characteristics, cancer developed in the middle third was relatively more prevalent than in the upper and lower third in females (P=0.003). As for age, cancer in the lower third was more common than in the upper and middle third in patients older than 50 years (P<0.001). For disease in the upper third, pT3 was relatively more prevalent compared to the middle and lower third (P<0.001). Regarding surgical methods, total gastrectomy was more commonly performed for disease in the upper third than in the middle and lower third (P<0.001). Tumors of diameter exceeding 3 cm were more abundant in the upper third than in the middle and lower third (P=0.002). Undifferentiated tumors were prevalent in the upper and middle third, while differentiated tumors were abundant in the lower third (P<0.001). Lymphatic and perineural invasion was more prevalent in the upper third of the stomach in comparison with the middle and lower third. Concerning the TNM stage, disease in the upper third was more advanced compared to the middle and lower third (P<0.001) (Table 1).
Table 1.
Patient's characteristics according to the tumor location
*P<0.05: statistically significant.
When the incidence of lymph node metastasis was compared by the depth of tumor invasion, metastasis in pT1 turned out to be 64/650 (9.8%), pT2 turned out to be 114/273 (41.8%) and pT3 turned out to be 341/587 (58.1%). However, no difference was detected according to tumor location.
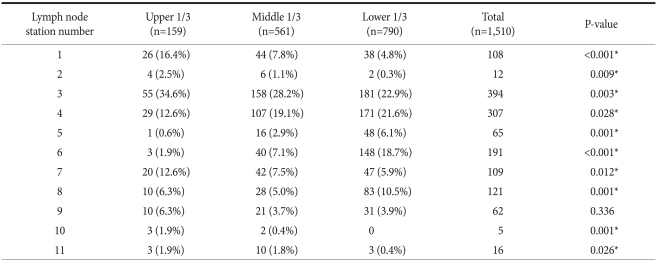
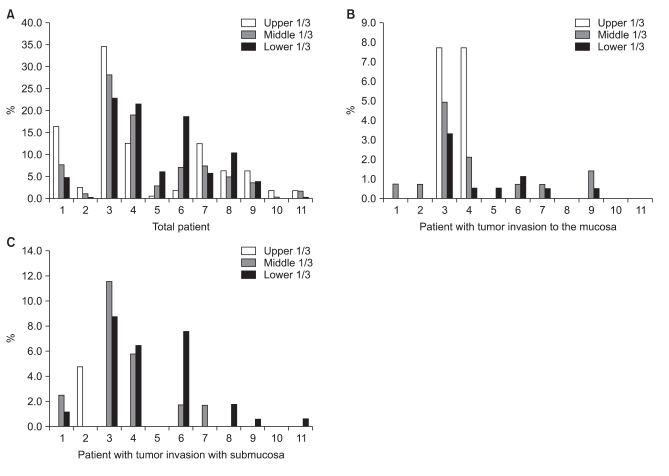
When the lymph node stations with metastasis based on tumor location were compared, metastasis in station numbers 1, 2, 3, 7, 10 and 11 was most commonly caused by disease in the upper third, while metastasis in station numbers 4, 5, 6 and 8 was significantly abundant in the lower third. Number 9 lymph node, however, did not show significant difference. Examining cases of lymph node metastasis beyond the second tier, number 7, 10 and 11 lymph node metastasis was dominant in the upper third. Number 8 was dominant in the lower third and as such, lymph node metastasis in the second tier of lymph nodes was abundant in the upper and lower third compared to the middle third (Table 2, Fig. 1A).
Table 2.
Number of patients with metastatic lymph nodes according to tumor location
*P<0.05: statistically significant.
Fig. 1.
Percentages of metastatic lymph nodes according to the tumor location. (A) Total patient. (B) T1a (mucosa). (C) T1b (Submucosa).
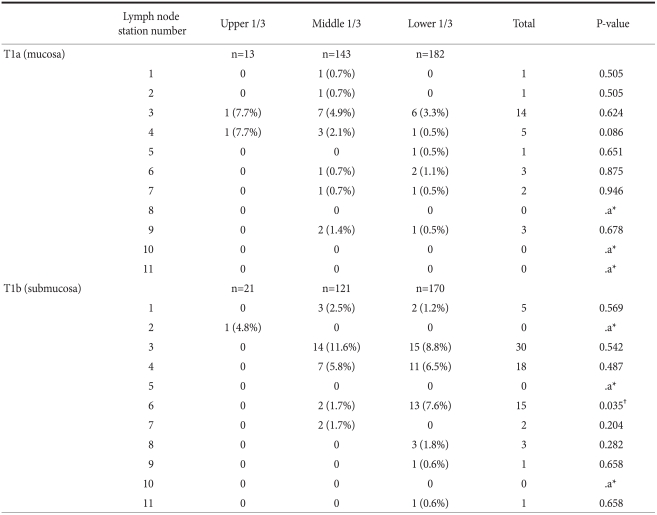
When dividing early gastric cancer into the mucosal (pT1a) and submucosal layer (pT1b) and comparing metastasis with each lymph node by tumor location, the number of lymph nodes with metastasis did not show significant difference in pT1a. In pT1b, metastasis was significantly abundant in the number 6 lymph node in disease originated in the lower third. In pT1a, none metastasized beyond the second tier in the upper third. As for metastasis beyond the second tier lymph nodes in the middle third, number 2 lymph node was found positive in 1 patient (0.7%), number 7 in 1 patient (0.7%) and number 9 in 2 patients (1.4%). Regarding metastasis beyond the second tier lymph nodes in the lower third, number 7 lymph node was positive in 1 patient (0.5%) and number 9 in 1 patient (0.5%). However, there was no statistical significance. In pT1b in the upper third of the stomach, none metastasized beyond second tier lymph nodes. Regarding metastasis beyond the second tier in disease originated in the middle third of the stomach, number 7 lymph node was positive in 2 patients (1.7%). In the lower third, number 1 lymph node was positive in 2 patients (1.2%), number 8 in 3 patients (1.8%), number 9 in 1 patient (0.6%), and number 11 in 1 patient (0.6%), which was not statistically significant (Table 3, Fig. 1B, C).
Table 3.
Number of patients with metastatic lymph nodes according to the tumor location in early gastric cancer
*Not enough data for calculation; †P<0.05: statistically significant.
Discussion
In this study, patients were divided into three groups, the upper third, the middle third and the lower third, depending on the location of the tumor, and their characteristics were compared. Differences were found in age, gender, tumor size, macroscopic morphology, differentiation grade, lymph node infiltration, invasion to the perineural area and tumor node metastasis (TNM) stage. The extent of tumor invasion was relatively severe and lymph node metastasis was more common secondary to disease in the upper third of the stomach, compared to the middle and lower third. Tumor development was once predominantly found in the lower third in contrast to recent observation that more diseases develop in the middle third, particularly in the angle of the lesser curvature, and the incidence of gastric cancer in the upper third is on the rise.(12) According to recent reports, disease is relatively more common in the middle and lower third, and tends to be associated with early lymph node metastasis. Particularly, there is a tendency of lymph node metastasis to the vicinity of the splenic artery and hilum. As such, it has been proposed that total gastrectomy, extended lymphadenectomy and splenectomy are required to manage disease originated in the middle and lower third.(13) Nevertheless, due to recent advancement in surgical technique, extended lymphadenectomy, including lymph node station numbers 10 and 11 in the splenic hilum without splenectomy, is being performed widely. At our institution, gastrectomy for cancer in the upper third is performed by such methods.(14)
Recently, with the development of minimally invasive surgical techniques such as laparoscopic gastrectomy, much effort has been made to avoid total gastrectomy and proximal gastrectomy is being commonly performed.(15) As such, it is important to determine the range of lymphadenectomy associated with gastrectomy. Due to advancement of laparoscopic techniques, it has become possible to perform lymphadenectomy while observing the lymph node anatomical structure comprehensively. As a consequence, resection of station number 5 and 6 lymph nodes in the vicinity of the pylorus area is now possible without resecting the right gastroepiploic vessels below the pylorus and the right gastric vessels above the pylorus. However, if such vessels are injured during surgery, ligation must be performed to ensure patient safety. Therefore, for gastric cancer in the upper third, the range of lymphadenectomy may be reduced if the extent of lymph node metastasis in the area is not severe. In this study, when gastric cancer developed in the upper third, lymph node metastasis would be classified according to the depth of tumor invasion. Lymph node metastasis was not detected in early gastric cancer invading into the mucosal layer. Accordingly, modified lymphadectomy without resecting lymph nodes in the vicinity of the pylorus area is considered adequate, when proximal gastrectomy is performed on early gastric cancer.
When patient groups were classified based on tumor invasion depth, the deeper the invasion, the higher the incidence of lymph node metastasis. In Korea, Japan and other countries where gastric cancer incidence is high, lymphadenectomy higher than D2 is already being adopted.(16) Nonetheless, in terms of lymphadenectomy for early gastric cancer with low risk of lymph node metastasis, D1+α (resection of number 7 lymph node) or D1+β (resection of lymph nodes 7, 8 and 9) is sufficient in some cases. However, lymphadenectomy higher than D2 is considered necessary in other cases. This remains an area of controversy.(17)
Recently, sentinel lymph node biopsy has been performed in selected cases of early gastric cancers to avoid extensive lymphadenectomy. However, sentinel lymphadenectomy is not being practiced widely due to questionable accuracy and the presence of skip metastases.(18)
Extended lymphadenectomy higher than D2 was considered necessary for early gastric cancer in the past.(19) Nonetheless, due to the advent of minimally invasive surgical techniques, efforts have been made to reduce the extent of lymph node resection. In this study, invasion of early gastric cancer was subdivided into the mucosa and the submucosal layers, and metastasis of number 2 lymph nodes was not detected in disease originated in the upper third. On the other hand, metastasis was identified in number 7 and 9 lymph nodes in disease originated from the middle third while metastasis in lymph nodes number 1, 7, 8, 9 and 11 was identified in disease originated in the lower third. At any rate, the number was meager and statistical significance was not detected. On the contrary, in disease invaded into the submucosal layer, statistical differences were seen in 13 cases of metastasis in lymph nodes below the pylorus (number 6) in cancer originated in the lower third of the stomach. In summary, when performing laparoscopic gastrectomy in early gastric cancer, modified D1+β lymphadenectomy (resection of number 7, 8 and 9 lymph nodes) is considered a better option than conventional D2 extension lymphadenectomy. In particular, for diseases shown to have invaded into the mucosal layer at the clinical stage, it may be sufficient to perform such modified lymphadenectomy.
Recently, for early gastric cancer located more than 3 cm from the pylorus for the middle third, attempts have been made to perform pylorus preserving gastrectomy as a form of function-preserving gastrectomy. According to recent studies reported by Ikeguchi et al. in Japan, the post-surgical quality-of-life was better when pylorus-preserving gastrectomy was performed compared to conventional distal resection.(20,21) However, when performing such pylorus-preserving gastrectomy, resection of number 5 and 6 lymph nodes in the vicinity of the pylorus remains technically challenging. Hence, for gastric cancer originated in the middle third, the presence or absence of metastasis in number 5 and 6 lymph nodes was examined based on the depth of tumor invasion in this study.(22) Among all early gastric cancer cases, there was 1 case of metastasis in number 6 lymph node due to cancer originated in the middle third restricted to the mucosal layer, and there were 2 cases of metastasis in the number 6 lymph node from disease invading into the submucosal layer. Thus, it may be necessary to perform pylorus-preserving gastrectomy and number 6 node dissection for disease originated in the middle third with submucosal invasion (pT1b).
The limitations of this study included relatively low incidence of gastric cancer in the upper third of the stomach, compared to that in the middle and the lower third as well as relatively small patient cohort.
Based on the results, guidelines for modified reduced lymphadenectomy that potentially replaces conventional extended lymphadenectomy in a wide area can be considered to be adopted when function-preserving gastrectomy is performed for the treatment of early gastric cancer in the future, to be supported by the conduct of a large-scale study.
Footnotes
Supported by a Korea University Grant.
References
- 1.Kwee RM, Kwee TC. Predicting lymph node status in early gastric cancer. Gastric Cancer. 2008;11:134–148. doi: 10.1007/s10120-008-0476-5. [DOI] [PubMed] [Google Scholar]
- 2.Novotny AR, Schuhmacher C. Predicting lymph node metastases in early gastric cancer: radical resection or organ-sparing therapy? Gastric Cancer. 2008;11:131–133. doi: 10.1007/s10120-008-0479-2. [DOI] [PubMed] [Google Scholar]
- 3.Nieminen A, Kokkola A, Ylä-Liedenpohja J, Louhimo J, Mustonen H, Puolakkainen P. Early gastric cancer: clinical characteristics and results of surgery. Dig Surg. 2009;26:378–383. doi: 10.1159/000226765. [DOI] [PubMed] [Google Scholar]
- 4.Goto O, Fujishiro M, Kodashima S, Ono S, Omata M. Outcomes of endoscopic submucosal dissection for early gastric cancer with special reference to validation for curability criteria. Endoscopy. 2009;41:118–122. doi: 10.1055/s-0028-1119452. [DOI] [PubMed] [Google Scholar]
- 5.Strong VE, Devaud N, Allen PJ, Gonen M, Brennan MF, Coit D. Laparoscopic versus open subtotal gastrectomy for adenocarcinoma: a case-control study. Ann Surg Oncol. 2009;16:1507–1513. doi: 10.1245/s10434-009-0386-8. [DOI] [PubMed] [Google Scholar]
- 6.Kunisaki C, Makino H, Takagawa R, Oshima T, Nagano Y, Ono HA, et al. Efficacy of laparoscopy-assisted distal gastrectomy for gastric cancer in the elderly. Surg Endosc. 2009;23:377–383. doi: 10.1007/s00464-008-9949-1. [DOI] [PubMed] [Google Scholar]
- 7.Aihara R, Mochiki E, Ohno T, Yanai M, Toyomasu Y, Ogata K, et al. Laparoscopy-assisted proximal gastrectomy with gastric tube reconstruction for early gastric cancer. Surg Endosc. 2010;24:2343–2348. doi: 10.1007/s00464-010-0947-8. [DOI] [PubMed] [Google Scholar]
- 8.Hiki N, Shimoyama S, Yamaguchi H, Kubota K, Kaminishi M. Laparoscopy-assisted pylorus-preserving gastrectomy with quality controlled lymph node dissection in gastric cancer operation. J Am Coll Surg. 2006;203:162–169. doi: 10.1016/j.jamcollsurg.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 9.Huang B, Zheng X, Wang Z, Wang M, Dong Y, Zhao B, et al. Prognostic significance of the number of metastatic lymph nodes: is UICC/TNM node classification perfectly suitable for early gastric cancer? Ann Surg Oncol. 2009;16:61–67. doi: 10.1245/s10434-008-0193-7. [DOI] [PubMed] [Google Scholar]
- 10.Greene FL. TNM staging for malignancies of the digestive tract: 2003 changes and beyond. Semin Surg Oncol. 2003;21:23–29. doi: 10.1002/ssu.10018. [DOI] [PubMed] [Google Scholar]
- 11.Japanese Gastric Cancer Association. Japanese Classification of Gastric Carcinoma - 2nd English Edition - Gastric Cancer. 1998;1:10–24. doi: 10.1007/s101209800016. [DOI] [PubMed] [Google Scholar]
- 12.An JY, Youn HG, Choi MG, Noh JH, Sohn TS, Kim S. The difficult choice between total and proximal gastrectomy in proximal early gastric cancer. Am J Surg. 2008;196:587–591. doi: 10.1016/j.amjsurg.2007.09.040. [DOI] [PubMed] [Google Scholar]
- 13.Yang K, Chen XZ, Hu JK, Zhang B, Chen ZX, Chen JP. Effectiveness and safety of splenectomy for gastric carcinoma: a meta-analysis. World J Gastroenterol. 2009;15:5352–5359. doi: 10.3748/wjg.15.5352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Oh SJ, Hyung WJ, Li C, Song J, Kang W, Rha SY, et al. Yonsei Gastric Cancer Clinic. The effect of spleen-preserving lymphadenectomy on surgical outcomes of locally advanced proximal gastric cancer. J Surg Oncol. 2009;99:275–280. doi: 10.1002/jso.21229. [DOI] [PubMed] [Google Scholar]
- 15.Cheong O, Kim BS, Yook JH, Oh ST, Park YK, Ryu SY. Modified radical lymphadenectomy without splenectomy in patients with proximal gastric cancer: comparison with standard D2 lymphadenectomy for distal gastric cancer. J Surg Oncol. 2008;98:500–504. doi: 10.1002/jso.21137. [DOI] [PubMed] [Google Scholar]
- 16.Deng J, Liang H, Sun D, Wang D, Pan Y. Suitability of 7th UICC N stage for predicting the overall survival of gastric cancer patients after curative resection in China. Ann Surg Oncol. 2010;17:1259–1266. doi: 10.1245/s10434-010-0939-x. [DOI] [PubMed] [Google Scholar]
- 17.Morita H, Ishikawa Y, Akishima-Fukasawa Y, Ito K, Akasaka Y, Nishimura C, et al. Histopathological predictor for regional lymph node metastasis in gastric cancer. Virchows Arch. 2009;454:143–151. doi: 10.1007/s00428-008-0717-3. [DOI] [PubMed] [Google Scholar]
- 18.Ichikura T, Sugasawa H, Sakamoto N, Yaguchi Y, Tsujimoto H, Ono S. Limited gastrectomy with dissection of sentinel node stations for early gastric cancer with negative sentinel node biopsy. Ann Surg. 2009;249:942–947. doi: 10.1097/SLA.0b013e3181a77e7e. [DOI] [PubMed] [Google Scholar]
- 19.Pugliese R, Maggioni D, Sansonna F, Ferrari GC, Forgione A, Costanzi A, et al. Outcomes and survival after laparoscopic gastrectomy for adenocarcinoma. Analysis on 65 patients operated on by conventional or robot-assisted minimal access procedures. Eur J Surg Oncol. 2009;35:281–288. doi: 10.1016/j.ejso.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 20.Ikeguchi M, Hatada T, Yamamoto M, Miyake T, Matsunaga T, Fukuda K, et al. Evaluation of a pylorus-preserving gastrectomy for patients preoperatively diagnosed with early gastric cancer located in the middle third of the stomach. Surg Today. 2010;40:228–233. doi: 10.1007/s00595-009-4043-4. [DOI] [PubMed] [Google Scholar]
- 21.Shibata C, Shiiba KI, Funayama Y, Ishii S, Fukushima K, Mizoi T, et al. Outcomes after pylorus-preserving gastrectomy for early gastric cancer: a prospective multicenter trial. World J Surg. 2004;28:857–861. doi: 10.1007/s00268-004-7369-5. [DOI] [PubMed] [Google Scholar]
- 22.Kong SH, Kim JW, Lee HJ, Kim WH, Lee KU, Yang HK. The safety of the dissection of lymph node stations 5 and 6 in pylorus-preserving gastrectomy. Ann Surg Oncol. 2009;16:3252–3258. doi: 10.1245/s10434-009-0646-7. [DOI] [PubMed] [Google Scholar]