Abstract
Purpose
Despite the compelling scientific and clinical data supporting the use of early oral nutrition after major gastrointestinal surgery, traditional bowel rest and intravenous nutrition for several postoperative days is still being used widely after gastric cancer surgery.
Materials and Methods
A phase II study was carried out to evaluate the feasibility and safety of postoperative early oral intake (water intake on postoperative days (POD) 1-2, and soft diet on POD 3) after a gastrectomy. The primary outcome was morbidity within 30 postoperative days, which was targeted at <25% based on pilot study data.
Results
The study subjects were 90 males and 42 females with a mean age 61.5 years. One hundred and four (79%) and 28 (21%) patients underwent a distal and total gastrectomy, respectively. The postoperative morbidity rate was within the targeted range (15.2%, 95% CI, 10.0~22.3%), and there was no hospital mortality. Of the 132 patients, 117 (89%) successfully completed a postoperative early oral intake regimen without deviation; deviation in 10 (8%) due to gastrointestinal symptoms and in five (4%) due to the management of postoperative complications. The mean times to water intake and a soft diet were 1.0±0.2 and 3.2±0.7 days, respectively, and the mean hospital stay was 10.0±6.1 days.
Conclusions
Postoperative early oral intake after a gastrectomy is feasible and safe, and can be adopted as a standard perioperative care after a gastrectomy. Nevertheless, further clinical trials will be needed to evaluate the benefits of early oral nutrition after upper gastrointestinal surgery.
Keywords: Postoperative care, Gastrectomy, Stomach neoplasms
Introduction
postoperative management of patients undergoing gastrointestinal (GI) surgery traditionally involves bowel rest and the avoidance of oral intake of fluid or meals until the resolution of postoperative ileus. However, compelling scientific and clinical data support the use of early enteral nutrition rather than intravenous nutrition and bowel rest after major abdominal surgery.(1) Recent randomized trials and a meta-analysis have shown the customary withholding of oral intake (nil-by-mouth) over the first postoperative days is unnecessary and that patients should be allowed food without delay after colorectal surgery.(2,3) The benefits of early oral nutrition as part of multimodal rehabilitation also have been well documented after major gynecologic,(4) urologic,(5) and vascular surgery.(6) However, many surgeons still adhere to 'nil-by-mouth' during the early postoperative period after upper GI surgery and prefer enteral tube feeding distal to a new anastomosis for enteral nutritional support.
The major factors used to justify the traditional practice of oral intake restriction after upper GI surgeries are a fear of anastomosis dehiscence and postoperative ileus. However, this rationale of restricted oral nutrition is not evidence-based. A systemic review of early oral nutrition after upper GI surgery showed that no high quality trial has been conducted to address the topic of early oral nutrition after upper GI surgery.(7) On the contrary, some experimental and clinical studies have demonstrated that early enteral nutrition may increase wound healing and anastomotic strength in intestines and somatic tissues.(2,8)
The lack of comprehensive evidence regarding best clinical practice for perioperative care after gastrectomy has led to a lack of uniformity of several postoperative routines between countries and institutions. According to a survey on postoperative practice after gastrectomy in five Northern European countries, the majority of centers still adopt conservative nasogastric tube and 'nil-by-mouth' regimens for several days after gastrectomy.(9) In Japan, the so-called 'conventional fixed diet regimen' which includes the restriction of oral intake for the first 3~4 postoperative days is prevalent among institutions.(10) Furthermore, despite the current practice of postoperative early oral nutrition after colorectal and gynecologic surgery, relatively few studies have evaluated the feasibility and safety of early oral intake after gastric surgery. Accordingly, in this study, we evaluated the feasibility and safety of perioperative care adopting postoperative early oral intake in patients that had undergone elective gastrectomy for gastric carcinoma.
Materials and Methods
1. Study design and sample size
This study was designed as a phase 2 trial aimed at evaluating the feasibility of early oral intake after gastrectomy. Inclusion criteria were; histologically proven gastric adenocarcinoma, elective gastrectomy (distal or total) either via an open or laparoscopic approach, an age of <80 years, adequate organ function, no history of preoperative chemotherapy or radiotherapy, and the provision of written informed consent. Exclusion criteria were; an operation under emergency conditions (e.g., a gastric outlet obstruction perforation or bleeding), a severe underlying medical illness, impaired renal, hepatic, cardiovascular, or endocrine function, and severe malnutrition [body mass index (BMI) <15 kg/m2].
The primary endpoint was postoperative morbidity within 30 postoperative days. Previous clinical trials have reported morbidity rates after gastrectomy for gastric cancer ranging from 10% to 30%.(11-13) Our preliminary data of postoperative morbidity for patients that met the same inclusion and exclusion criteria showed an overall morbidity rate of 20% (95% CI, 16~26%). Assuming an upper limit of acceptable morbidity for patients managed with early oral intake postoperative care regimen of <25%, a sample size of 130 was found to be required for a single-stage phase 2 design, 80% power, and a significance level of 0.05.
2. Surgical procedure and the perioperative care protocol
Distal or total gastrectomy was performed according to tumor location, so as to secure a surgical margin of >5 cm in advanced gastric cancer and of >2 cm in early gastric cancer. D2 lymphadenectomy as described by the guidelines issued by the Japanese Gastric Cancer Association was used as a standard procedure in advanced gastric cancer, and limited lymphadenectomy (D1 plus beta) was used in early gastric cancer.(14) Laparoscopic surgery was indicated for clinically diagnosed T1N0-1 gastric cancer. After distal gastrectomy, gastroduodenostomy (Billroth I) or gastrojejunostomy (Billroth II or Roux-en Y method) was performed for reconstruction according to surgeon's discretion, and Roux-en Y esophagojejunostomy was performed after total gastrectomy. All reconstruction procedures were performed using a circular or linear stapler. An abdominal drain was used in selected cases, again according to surgeon's discretion.
All patients were managed postoperatively using a standardized clinical pathway. No preoperative bowel preparation was performed (patients were only fasted overnight before surgery) and a nasogastric tube was not used perioperatively. Postoperative pain was managed by intravenous patient-controlled analgesia (PCA) during the first three postoperative days. A second-generation cephalosporin was used for prophylaxis before skin incision until 24 hours postop. Patients started ingesting water on postoperative day 1 [postoperative days (POD) 1], and if patient did not develop any specific complaints, such as, nausea, vomiting, or abdominal discomfort, a soft diet was given (six times a day) to patients from POD 3 until hospital discharge. Intravenous fluid was given during the first three postoperative days in the form of a fluid restriction regimen (1,400~1,500 ml/day, standard=60 kg, 1,000 kcal). No routine pro-motility or anti-emesis agent was used. Gradual compression stockings or an intermittent pneumatic compression device was used for venous thrombosis prophylaxis in all patients. Patients were encouraged to ambulate actively from POD 1. Hospital discharge was targeted on POD 8, and objective discharge criteria were used to make decisions regarding discharge, namely; no sign of a postoperative complication, an ability to ambulate without assistance, tolerable pain on oral analgesia, able to take more than 70% of a given meal, and a willingness to go home.
3. Outcome measures
The primary outcome was postoperative morbidity, and the secondary outcomes were hospital course criteria, such as, compliance with early oral intake, nausea and vomiting, time to soft diet, onset of flatus, postoperative mortality, and hospital stay. The following postoperative complications were predefined and prospectively measured; abdominal bleeding, luminal bleeding, abdominal infection, pancreatic fistula, pancreatitis, anastomosis leakage, anastomosis stricture, ileus, duodenal stump leakage, and wound infection. Other complications were recorded as appropriate. Hospital mortality was defined as postoperative death for any cause within 30 postoperative days, or death within the hospitalization period. Late complications, such as, dumping, diarrhea, anemia, and quality of life issues were not included in this study.
4. Statistical analyses
Statistical analyses were performed using the chi-square test or the independent t-test as appropriate. SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA) was used throughout, and statistical significance was accepted for P-value of less than 0.05.
Results
1. Clinicopathological characteristics
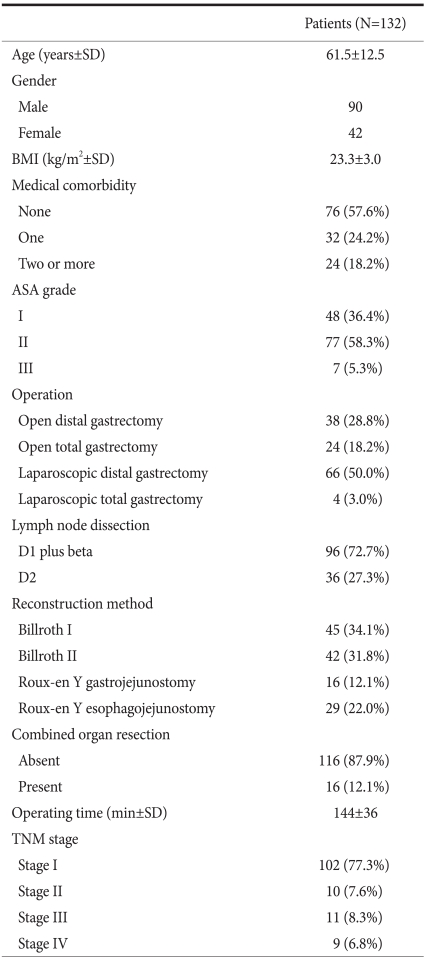
Between July 2009 and April 2010, 132 eligible patients with a diagnosis of gastric adenocarcinoma and who underwent elective gastrectomy were enrolled in this study. Table 1 details patient demographic and clinicopathological features. There were 90 males and 42 females of mean age 61.5 years. Fifty-six (42%) had one or more preoperative medical illnesses, and 125 (95%) were assessed as having American Society of Anesthesiologists (ASA) grade I or II. Distal gastrectomy was performed in 104 (79%), and total gastrectomy in 28 (21%) patients (70 (53%) laparoscopic surgeries were performed). Thirty-six (27%) patients underwent D2 lymph node dissection, and 16 (12%) patients underwent combined organ resection during operation. Final TNM stages were; stage I in 102 (77%), stage II in 10 (8%), stage III in 11 (8%), and stage IV in 9 (7%) patients, according to 6th edition of the AJCC TNM classification.
Table 1.
Clinicopathological features
SD = standard deviation; BMI = body mass index; ASA = American Society of Anesthesiologists.
2. Surgical outcomes
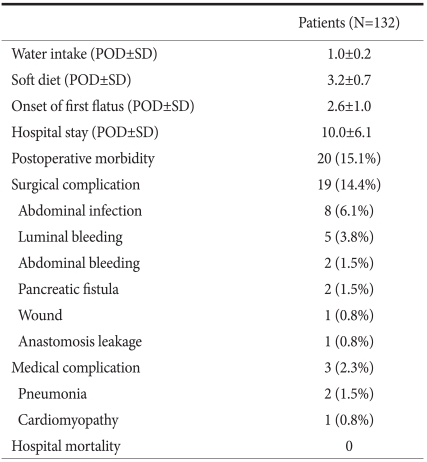
The mean times to water intake and a soft diet were 1.0±0.2 and 3.2±0.7 days, respectively, and mean time to onset of first flatus was 2.6±1.0 days. Of the 132 patients, 100 (81.3%) patients were discharged from hospital on POD 8 after fulfilling the discharge criteria, and the mean hospital stay of all patients was 10.0±6.1 days (Table 2).
Table 2.
Surgical outcomes
POD = postoperative days; SD = standard deviation.
During the postoperative period, 20 patients developed 19 surgical and 3 medical complications. The overall postoperative morbidity rate was 15.2% (95% CI, 10.0~22.3%). Regarding surgical complications, abdominal infection (n=8) was the most common, followed by luminal bleeding (n=5). Of the 19 patients with a surgical complication, one patient required reoperation due to an anastomosis leakage, and two patients with a pancreatic fistula were managed by radiologic intervention. The remaining 16 patients responded to conservative treatment. No in-hospital mortality occurred.
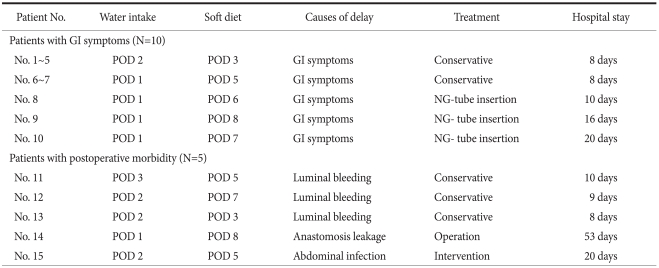
3. Adherence to postoperative early oral intake
117 (89%) of the 132 patients successfully started water intake on POD 1 and a soft diet on POD 3. Fifteen (11%) patients failed to adhere to the postoperative early oral intake schedule. Of these 15 patients, 5 stopped oral intake due to the management of postoperative complication (3 luminal bleedings, 1 abdominal infection, and 1 anastomosis leakage), and in 10 patients, an oral diet schedule was delayed due to gastrointestinal symptoms, such as, nausea, vomiting, and abdominal discomfort. Of the 10 patients with gastrointestinal symptoms, 7 resumed an oral diet on conservative treatment and were discharged from hospital on POD 8, but the other 3 required nasogastric tube insertion and hospital discharge was delayed (Table 3).
Table 3.
Hospital courses of the 15 patients who failed to adhere to the postoperative early oral intake schedule
POD = postoperative days; GI = gastrointestinal; NG = nasogastric.
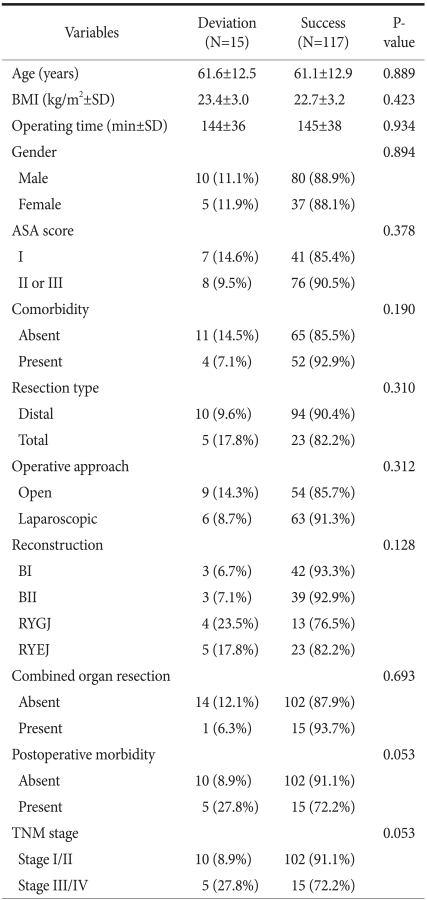
4. Factors that may predict early oral intake failure after gastrectomy
A total of 15 (11.4%, 95% CI 7.0~17.9%) patients deviated from the postoperative early oral intake schedule with respect to water intake or soft diet commencement. To identify variables predictive of early postoperative oral intake failure, we compared successes and failures with respect to age, gender, BMI, comorbidity, ASA score, operation type, reconstruction method, combined organ resection, operating time, TNM stage, and postoperative morbidity. However, no factor was found to be significantly associated with deviation from the early oral intake regimen, but postoperative morbidity (P=0.053) and TNM stage (P=0.053) showed a tendency to be associated with a deviation (Table 4).
Table 4.
Analysis of factors associated with deviation from the postoperative early oral intake schedule
RYGJ = Roux-en Y gastrojejunostomy; RYEJ = Roux-en Y esophagojejunostomy.
Discussion
Current practice regarding postoperative early oral nutrition has been well established for several abdominal surgical procedures.(15) Several randomized controlled trials and meta-analysis have shown that early oral food intake is both feasible and safe after gastrointestinal surgery, and suggested that it may reduce infection-related complications and length of hospital stay as compared with the traditional 'nil-by-mouth' approach.(2) Theoretically, the earlier use of the enteral route for nutritional support has several advantages over bowel rest and intravenous nutrition, as it may activate normal digestive reflexes, which have an important impact on gut recovery, which is central to overall recovery after gastrointestinal surgery.(16) Furthermore, hospital stays can be reduced by shortening the fasting period after surgery. Not only does this provide more physiologic and efficient nutrition, but it also minimizes patient discomfort and anxiety caused by an enforced fast after surgery. Better protein kinetics and preservation of the immune system as compared with intravenous nutrition may also contribute to enhanced wound healing and resistance to infection.(17,18) Therefore, enteral nutrition should be initiated as soon as possible after major abdominal surgery, unless it is contraindicated, and oral intake is preferable to enteral tube feeding as a route of enteral nutrition support.(19)
Despite advances in surgical techniques and perioperative care, limited compelling scientific data regarding best clinical practice has led to a lack of national or international consensus on standard perioperative care after gastric cancer surgery. As for postoperative nutritional support, for example, traditional bowel rest and intravenous nutrition for several postoperative days is still being widely used after gastric surgery.(9) Furthermore, although anastomosis safety and postoperative ileus are the main concerns which have lead to the careful introduction of dietary schedule after gastrectomy, no high quality trials have provided evidence to support this rationale.(7) To the best of our knowledge, this study is the first phase 2 clinical trial to evaluate the feasibility and safety of early oral intake after gastrectomy. In this study, the primary outcome, postoperative morbidity rate, was within the targeted range (15.2%, 95% CI, 10.0~22.3%), and most patients (89%) were able to tolerate the early oral dietary schedule uneventfully. Therefore, our results indicate that early oral intake is feasible and safe after gastrectomy, as has been shown after other types of gastrointestinal surgery, and suggest that it could be adopted as a standard for perioperative care after gastric cancer surgery.
The practice of enteral tube feeding after esophagectomy or gastrectomy has been extensively documented in the literature.(20,21) However, studies on the safety and feasibility of early oral intake after gastric surgery are limited. Suehiro et al.(22) first reported accelerated rehabilitation with postoperative early oral intake in patients undergoing gastrectomy. In their study, surgical outcomes after gastrectomy of an early oral intake group (liquid diet within 48 hrs) and a traditional group ('nil-by-mouth' until resolution of postoperative ileus) were retrospectively reviewed, and it was found that postoperative recovery was better in the early oral intake group, as indicated by earlier onset of flatus, and shorter fasting period and hospital stays. In a subsequent non-randomized comparative study conducted by Hirao et al.(10) a so called 'patient-controlled dietary schedule' (water intake on POD 1, liquid diet on POD 2, and solid diet on demand) was compared with a conventional diet regimen (postoperative nil-by-mouth) in patients that had undergone distal gastrectomy. Like Suehiro et al.(22), they found that early oral intake after gastrectomy was feasible and that it caused no increase in postoperative morbidity. A large multicenter randomized trial conducted by Lassen and colleagues compared a routine of allowing normal food at will from POD 1 with a nil-by-mouth/enteral tube feeding routine for 5 days after upper gastrointestinal surgery. They concluded that the early institution of an oral diet probably enhances postoperative recovery, as indicated by time to first flatus and shorter hospital stay, and that it has no adverse effect on major morbidities.(23) However, only 36% of the patients enrolled underwent gastric surgery, and thus, further clinical trials are needed for each type of surgery to determine best postoperative practice. Recently, Hur et al.(24) reported the results of a small pilot study on early oral intake after gastrectomy, which showed better postoperative recovery and no increased risk of gastrointestinal complications.
The early resumption of oral nutrition could probably be enhanced by adopting multimodal approaches to improve gastrointestinal recovery and reduce postoperative surgical stress. Postoperative nausea and vomiting and transient ileus are predominantly neural and inflammatory responses to abdominal surgery, and may markedly delay the early resumption of oral nutrition. However, during past decades, substantial advances have been made in our understanding of surgical stress response and postoperative recovery.(15) For example, as demonstrated by our standardized perioperative care procedure, preoperative bowel preparation, routine use of an abdominal drain, and nasogastric tube insertion are no longer considered indispensible for patients undergoing elective gastrectomy.(25) Intravenous fluid infusion restriction may also enhance bowel recovery and reduce postoperative complications,(26) and the use of epidural analgesia, short acting intraoperative opioids, and effective antiemetic agents may promote the success of early oral nutrition after surgery.(27) Recently, these multimodal strategies, also known as 'fast-track surgery', have been extensively investigated in the contexts of colonic, gynecologic, and upper abdominal laparoscopic procedures.(15) However, reports regarding gastric surgery are scarce, and study is required to evaluate the benefits of these multimodal strategies in gastric cancer patients.
The extent of resection or type of operative approach might influence on the feasibility of early oral intake after gastric surgery. However, in this study, no significant variables including patient and operation-related factors were found to predict a failure of postoperative early oral intake regimen. Theoretically, total gastrectomy is presumed to be less tolerable to early oral intake than distal gastrectomy due to no gastric reservoir after surgery. Laparoscopic surgery is also believed to contribute to enhancing postoperative bowel recovery as compared with open surgery.(28) Despites not reaching statistical significance, 17.8% of patients with total gastrectomy failed to adhere to early oral dietary schedule, compared to 9.6% in patients with distal gastrectomy. Laparoscopic surgery also showed lower failure rate than open surgery (8.7% vs. 14.3% in open surgery). Considering relatively small size of this study, we think these factors should be further evaluated in large clinical trials for establishing proper indication of early oral intake perioperative care after gastric cancer surgery.
In the colcusion, this study shows that a perioperative care program incorporating the early institution of oral intake is feasible and safe after gastrectomy. Furthermore, early oral intake was not found to increase postoperative morbidity, and was tolerated by most patients without any adverse event. Accordingly, we suggest that early oral feeding could be adopted as a standardized perioperative care procedure after gastrectomy. Finally, further clinical trials are warranted to evaluate the benefits of early oral feeding on postoperative recovery, reducing postoperative complications, and on immunologic and nutritional functions.
References
- 1.Dervenis C, Avgerinos C, Lytras D, Delis S. Benefits and limitations of enteral nutrition in the early postoperative period. Langenbecks Arch Surg. 2003;387:441–449. doi: 10.1007/s00423-003-0350-1. [DOI] [PubMed] [Google Scholar]
- 2.Lewis SJ, Egger M, Sylvester PA, Thomas S. Early enteral feeding versus "nil by mouth" after gastrointestinal surgery: systematic review and meta-analysis of controlled trials. BMJ. 2001;323:773–776. doi: 10.1136/bmj.323.7316.773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Soop M, Carlson GL, Hopkinson J, Clarke S, Thorell A, Nygren J, et al. Randomized clinical trial of the effects of immediate enteral nutrition on metabolic responses to major colorectal surgery in an enhanced recovery protocol. Br J Surg. 2004;91:1138–1145. doi: 10.1002/bjs.4642. [DOI] [PubMed] [Google Scholar]
- 4.Steed HL, Capstick V, Flood C, Schepansky A, Schulz J, Mayes DC. A randomized controlled trial of early versus "traditional" postoperative oral intake after major abdominal gynecologic surgery. Am J Obstet Gynecol. 2002;186:861–865. doi: 10.1067/mob.2002.123057. [DOI] [PubMed] [Google Scholar]
- 5.Brodner G, Van Aken H, Hertle L, Fobker M, Von Eckardstein A, Goeters C, et al. Multimodal perioperative management--combining thoracic epidural analgesia, forced mobilization, and oral nutrition--reduces hormonal and metabolic stress and improves convalescence after major urologic surgery. Anesth Analg. 2001;92:1594–1600. doi: 10.1097/00000539-200106000-00049. [DOI] [PubMed] [Google Scholar]
- 6.Mukherjee D. "Fast-track" abdominal aortic aneurysm repair. Vasc Endovascular Surg. 2003;37:329–334. doi: 10.1177/153857440303700504. [DOI] [PubMed] [Google Scholar]
- 7.Lassen K, Revhaug A. Early oral nutrition after major upper gastrointestinal surgery: why not? Curr Opin Clin Nutr Metab Care. 2006;9:613–617. doi: 10.1097/01.mco.0000241673.17300.87. [DOI] [PubMed] [Google Scholar]
- 8.Moss G. Maintenance of gastrointestinal function after bowel surgery and immediate enteral full nutrition. II. Clinical experience, with objective demonstration of intestinal absorption and motility. JPEN J Parenter Enteral Nutr. 1981;5:215–220. doi: 10.1177/0148607181005003215. [DOI] [PubMed] [Google Scholar]
- 9.Lassen K, Dejong CH, Ljungqvist O, Fearon K, Andersen J, Hannemann P, et al. Nutritional support and oral intake after gastric resection in five northern European countries. Dig Surg. 2005;22:346–352. doi: 10.1159/000089770. [DOI] [PubMed] [Google Scholar]
- 10.Hirao M, Tsujinaka T, Takeno A, Fujitani K, Kurata M. Patient-controlled dietary schedule improves clinical outcome after gastrectomy for gastric cancer. World J Surg. 2005;29:853–857. doi: 10.1007/s00268-005-7760-x. [DOI] [PubMed] [Google Scholar]
- 11.Degiuli M, Sasako M, Calgaro M, Garino M, Rebecchi F, Mineccia M, et al. Morbidity and mortality after D1 and D2 gastrectomy for cancer: interim analysis of the Italian Gastric Cancer Study Group (IGCSG) randomised surgical trial. Eur J Surg Oncol. 2004;30:303–308. doi: 10.1016/j.ejso.2003.11.020. [DOI] [PubMed] [Google Scholar]
- 12.Sasako M, Sano T, Yamamoto S, Kurokawa Y, Nashimoto A, Kurita A, et al. D2 lymphadenectomy alone or with para-aortic nodal dissection for gastric cancer. N Engl J Med. 2008;359:453–462. doi: 10.1056/NEJMoa0707035. [DOI] [PubMed] [Google Scholar]
- 13.Wu CW, Hsieh MC, Lo SS, Wang LS, Hsu WH, Lui WY, et al. Morbidity and mortality after radical gastrectomy for patients with carcinoma of the stomach. J Am Coll Surg. 1995;181:26–32. [PubMed] [Google Scholar]
- 14.Japanese Gastric Cancer Association. Japanese Classification of Gastric Carcinoma - 2nd English Edition - Gastric Cancer. 1998;1:10–24. doi: 10.1007/s101209800016. [DOI] [PubMed] [Google Scholar]
- 15.Kehlet H, Wilmore DW. Evidence-based surgical care and the evolution of fast-track surgery. Ann Surg. 2008;248:189–198. doi: 10.1097/SLA.0b013e31817f2c1a. [DOI] [PubMed] [Google Scholar]
- 16.Braga M, Gianotti L, Gentilini O, Parisi V, Salis C, Di Carlo V. Early postoperative enteral nutrition improves gut oxygenation and reduces costs compared with total parenteral nutrition. Crit Care Med. 2001;29:242–248. doi: 10.1097/00003246-200102000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Hochwald SN, Harrison LE, Heslin MJ, Burt ME, Brennan MF. Early postoperative enteral feeding improves whole body protein kinetics in upper gastrointestinal cancer patients. Am J Surg. 1997;174:325–330. doi: 10.1016/s0002-9610(97)00095-0. [DOI] [PubMed] [Google Scholar]
- 18.Schroeder D, Gillanders L, Mahr K, Hill GL. Effects of immediate postoperative enteral nutrition on body composition, muscle function, and wound healing. JPEN J Parenter Enteral Nutr. 1991;15:376–383. doi: 10.1177/0148607191015004376. [DOI] [PubMed] [Google Scholar]
- 19.Brandstrup B, Tønnesen H, Beier-Holgersen R, Hjortsø E, Ørding H, Lindorff-Larsen K, et al. Effects of intravenous fluid restriction on postoperative complications: comparison of two perioperative fluid regimens: a randomized assessor-blinded multicenter trial. Ann Surg. 2003;238:641–648. doi: 10.1097/01.sla.0000094387.50865.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baigrie RJ, Devitt PG, Watkin DS. Enteral versus parenteral nutrition after oesophagogastric surgery: a prospective randomized comparison. Aust N Z J Surg. 1996;66:668–670. doi: 10.1111/j.1445-2197.1996.tb00714.x. [DOI] [PubMed] [Google Scholar]
- 21.Heslin MJ, Latkany L, Leung D, Brooks AD, Hochwald SN, Pisters PW, et al. A prospective, randomized trial of early enteral feeding after resection of upper gastrointestinal malignancy. Ann Surg. 1997;226:567–577. doi: 10.1097/00000658-199710000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Suehiro T, Matsumata T, Shikada Y, Sugimachi K. Accelerated rehabilitation with early postoperative oral feeding following gastrectomy. Hepatogastroenterology. 2004;51:1852–1855. [PubMed] [Google Scholar]
- 23.Lassen K, Kjaeve J, Fetveit T, Tranø G, Sigurdsson HK, Horn A, et al. Allowing normal food at will after major upper gastrointestinal surgery does not increase morbidity: a randomized multicenter trial. Ann Surg. 2008;247:721–729. doi: 10.1097/SLA.0b013e31815cca68. [DOI] [PubMed] [Google Scholar]
- 24.Hur H, Si Y, Kang WK, Kim W, Jeon HM. Effects of early oral feeding on surgical outcomes and recovery after curative surgery for gastric cancer: pilot study results. World J Surg. 2009;33:1454–1458. doi: 10.1007/s00268-009-0009-3. [DOI] [PubMed] [Google Scholar]
- 25.Yoo CH, Son BH, Han WK, Pae WK. Nasogastric decompression is not necessary in operations for gastric cancer: prospective randomised trial. Eur J Surg. 2002;168:379–383. doi: 10.1080/110241502320789041. [DOI] [PubMed] [Google Scholar]
- 26.Lobo DN, Bostock KA, Neal KR, Perkins AC, Rowlands BJ, Allison SP. Effect of salt and water balance on recovery of gastrointestinal function after elective colonic resection: a randomised controlled trial. Lancet. 2002;359:1812–1818. doi: 10.1016/S0140-6736(02)08711-1. [DOI] [PubMed] [Google Scholar]
- 27.Bisgaard T, Kehlet H. Early oral feeding after elective abdominal surgery--what are the issues? Nutrition. 2002;18:944–948. doi: 10.1016/s0899-9007(02)00990-5. [DOI] [PubMed] [Google Scholar]
- 28.Bardram L, Funch-Jensen P, Jensen P, Crawford ME, Kehlet H. Recovery after laparoscopic colonic surgery with epidural analgesia, and early oral nutrition and mobilisation. Lancet. 1995;345:763–764. doi: 10.1016/s0140-6736(95)90643-6. [DOI] [PubMed] [Google Scholar]