Abstract
A laparoscopic wedge resection for a submucosal tumor, which is close to the gastroesophageal junction, is technically challenging. This can be a dilemma to both patients and surgeons when the tumor margin involves the gastroesophageal junction because a wedge resection in this situation might result in a deformity of the gastroesophageal junction or an injury to the lower esophageal sphincter, which ultimately results in lifelong gastroesophageal reflux disease. The patient was a 42 year-old male, whose preoperative endoscopic ultrasonographic finding did not rule out a gastrointestinal stromal tumor. He underwent a laparoscopic gastric wedge resection and prophylactic anterior partial fundoplication (Dor) and was discharged from hospital on the fifth postoperative day without any complications. There were no symptoms of reflux 5 months after surgery. A laparoscopic wedge resection and prophylactic anti-reflux surgery might be a good surgical option for a submucosal tumor at the gastroesophageal junction.
Keywords: Submucosal tumor, Esophagogastric junction, Laparoscopic wedge resection, Antireflux surgery
Introduction
Most of the gastric submucosal tumor (SMT), which originates between muscularis mucosa and proper muscle layer, are benign but some of it have the potential of malignant tumor and may require surgical resection when the size of the tumor exceeds more than 2 cm because of the risks of malignancy or when there are higher risks of obstruction or bleeding.(1-3) Gastric wedge resection with proper margin is the basic principle of treatment even in the case of malignant SMT because lymph node metastasis is rare.(4) Recently, a laparoscopic approach is well accepted as a safe and useful approach in this situation by several reports.(5) However, it may be very difficult to get an enough surgical margin when the tumor is very closely located to the gastroesophageal junction (GEJ) and moreover, wedge resection of the tumor may result in stenosis of GEJ or injury to the lower esophageal sphincter (LES) with subsequent lifelong gastroesophageal reflux disease (GERD) when the margin of the tumor involves the GEJ.(1) It is not easy for the surgeon to make a decision of performing proximal or total gastrectomy for the SMT of GEJ because preoperative differential diagnosis between benign and malignant SMT is very difficult and even in the case of confirmed malignancy before the operation by endoscopic ultrasonography (EUS)-guided fine needle aspiration biopsy (FNAB), it is still difficult to make a decision of performing total gastrectomy.(1,2)
Herein the authors present a case of SMT of GEJ which was successfully treated by laparoscopic wedge resection with prophylactic antireflux surgery.
Case Report
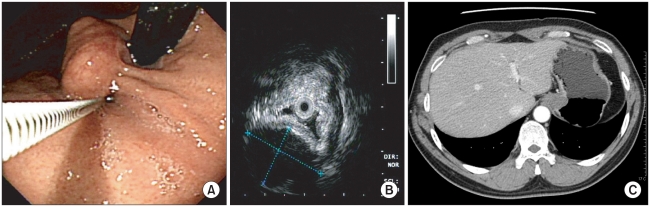
A 42 year-old male patient was admitted to Incheon St. Mary's Hospital, The Catholic University of Korea to undergo surgery under diagnosis of SMT of GEJ by screening endoscopy. There was no symptom related to the tumor and there was no abnormality in physical examination and laboratory tests. The endoscopic finding revealed a 2.5 cm-sized SMT which involved the GEJ (Fig. 1A), and this tumor was originated from the proper muscle layer by the finding of EUS (Fig. 1B). The EUS-guided FNAB failed to get enough specimen for diagnosis, and a homogeneously enhanced SMT around the GEJ was observed by abdominal computed tomography (CT) scan (Fig. 1C). The patient underwent laparoscopic gastric wedge resection.
Fig. 1.
The findings of preoperative study of the patient with a submucosal tumor of gastoresophageal junction. (A) Endoscopic finding showed 2.5 cm sized submucosal tumor involving the Z-line. (B) Endoscopic ultrasonographic finding showed hypoechoic submucosal mass originating from muscle layer. (C) Computed tomographic finding showed homogeneous mass at gastric cardia.
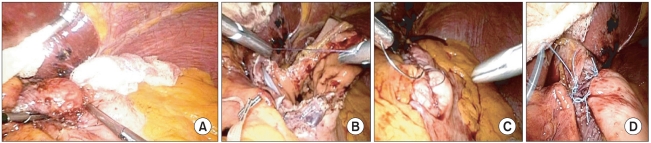
Under general anesthesia, the patient was put in reverse Trendelenburg position with his legs apart. The operator was positioned on the right side, and the first assistant was positioned on the left side of the patient. The camera operator was poisoned between the legs of the patient. A 10 mm trocar was inserted through the umbilicus for the camera, and a 5 mm trocar was inserted just below the xiphoid process for liver retractor. One 5 mm trocar on right upper abdomen and one 12 mm trocar on left upper abdomen were used as working channels for the operator. Another 5 mm trocar on left upper abdomen was used for the first assistant. The lesser curvature of the cardia was dissected first as close as possible not to damage right and left vagus nerves and the lesser omentum including both vagus nerves was taped with an umbilical tape. After the tumor mass, which was located at antero-greater curvature side of cardia, was identified (Fig. 2A), a small gastrotomy incision was made on the anterior gastric wall near the tumor by ultrasonic shears and wedge resection proceeded along with the tumor border. After the resection, about 2/3 of the circumference of the esophagus was detatched from the stomach with a large gastrotomy incision on the upper stomach (Fig. 2B). The esophagus was reimplanted by intracorporeal 2-layered interrupted sutures with #3-0 vicryl. After reimplantation of the esophagus, a 4 cm length gastrotomy incision was remained along the lesser curvature side of cardia. This gastrotomy incision was repaired by intracorporeal 2-layered continuous sutures with #3-0 vicryl (Fig. 2C). Two to three short gastric arteries were divided in order to mobilize the fundus and the mobilized fundus was sutured to anterior abdominal esophageal wall. Dor, anterior partial fundoplication was performed (Fig. 2D). Crural repair was not performed because the size of esophageal hiatus of this patient was normal.
Fig. 2.
Intraoperative view. (A) After careful division of lesser omentum from gastric cardia, 2.5 cm sized mass was identified at anterior and greater curvature side of cardia. (B) After wedge resection, about 2/3 of the circumference of the esophagus was detatched from the stomach with a large gastrotomy incision on the upper stomach. (C) New gastroesophageal junction was formed by intracorporeal 2-layerd interrupted and continuous sutures. (D) An anterior partial wrap was applied to the anterior wall of the abdominal esophagus.
An upper gastrointestinal series was taken at the first postoperative day. There was no leakage nor stenosis in rebuilt, partially wrapped new GEJ (Fig. 3). Nasogastric tube was removed and oral feeding proceeded just after upper gastrointestinal series was taken. The final pathologic report revealed leiomyoma of GEJ. The result of immunochemical stain was that C-kit tyrosine kinase was not expressed and actin, desmin was expressed. The patient was discharged at fifth postoperative day without any complication. There had been no symptom of reflux or dysphasia on 5 months of postoperative follow up.
Fig. 3.
Findings of upper gastrointestinal series on the 1st postoperative day. A small indentation which was formed by anterior partial wrap was shown at gastroesophageal junction.
Discussion
Several methods of laparoscopic wedge resection techniques for gastric SMT have been reported according to location and size of the tumor.(6) There are laparoscopic exogastric resection, laparoscopic transgastric tumor-everting resection, intragastric tumor wedge resection and laparoscopic esophagogastrectomy.(2) Among them, exogastric resection technique is one of the most popularized techniques that are good for extraluminlly growing tumors which are located at anterior wall and lesser curvature side of gastric antrum and greater curvature side of gastric body. It can easily be performed by linear stapling method.(7) Transgastric resection technique is good for the tumor which is located at posterior wall of stomach.(8)
However, if the tumor is located at less than 1~2 cm from the GEJ or involves the GEJ, it is very difficult to perform stapled resection without injuring angle of His and LES.(9) Shim et al.(9) reported submucosal dissection technique for the SMT which was close to the GEJ by using laparoscopic and endoscopic hybrid technique. However, the surgical margin would not be enough when the final pathology revealed malignancy, like gastrointestinal stromal tumor (GIST), and second look operation with additive resection may be needed.(1) Uyama et al.(10) reported laparoscopic proximal gastrectomy for the SMT's located at cardia, Dulucq et al. reported laparoscopic transhiatal esophagogastrectomy in the similar situation.(11) If the final pathologic result of these reports were benign, these surgical approaches would have been too invasive. Moreover, GERD after surgery has been reported in these two studies.(4,10-12)
Resection of the gastroesophageal junction, and thus the lower esophagea sphincter, result in a reluxogenic state, and 60~80% of such patients experience symptoms of GERD.(13) Tsiouris et al reported that the patients with concomitant fundoplication after resection of the gastroesophageal junction have much lower incidence of development of Barrett`s esophagus compared with the patients without fundoplication.(14)
In our case, oncologically complete resection of the tumor with proper surgical margin was obtained unlike the case of Shim et al. There was no need to perform second look operation or additive resection, though the final pathologic result was GIST. After successful wedge resection, we reimplanted the esophagus into upper stomach with 2-layerd interrupted sutures in order to prevent stricture of the new GEJ. We tried to prevent reflux, possibly being able to result from destruction of LES, by reinforcing the new GEJ with anterior partial fundoplication. Moreover, this partial wrap was very useful in protecting the anastomosis because it successfully covered the esophagogastrostomy suture line. The patient recovered well without any complication and remained free from any symptoms of reflux or dysphagia during 5 months after surgery.
Although there should be much longer period of follow up and the result of comparative study with other surgical techniques to support our suggestion, laparoscopic wedge resection with prophylactic antireflux surgery can be a good function-preserving surgical option for a SMT of GEJ.
References
- 1.Singaporewalla RM, Baladas GH, Lee TD. Laparoendoscopic removal of a benign gastric stromal tumor at the cardia. JSLS. 2006;10:117–121. [PMC free article] [PubMed] [Google Scholar]
- 2.Ke CW, Cai JL, Chen DL, Zheng CZ. Extraluminal laparoscopic wedge resection of gastric submucosal tumors: a retrospective review of 84 cases. Surg Endosc. 2010;24:1962–1968. doi: 10.1007/s00464-010-0888-2. [DOI] [PubMed] [Google Scholar]
- 3.Basso N, Rosato P, De Leo A, Picconi T, Trentino P, Fantini A, et al. Laparoscopic treatment of gastric stromal tumors. Surg Endosc. 2000;14:524–526. doi: 10.1007/s004640000021. [DOI] [PubMed] [Google Scholar]
- 4.Hwang SH, Park do J, Kim YH, Lee KH, Lee HS, Kim HH, et al. Laparoscopic surgery for submucosal tumors located at the esophagogastric junction and the prepylorus. Surg Endosc. 2009;23:1980–1987. doi: 10.1007/s00464-008-9955-3. [DOI] [PubMed] [Google Scholar]
- 5.Karakousis GC, Singer S, Zheng J, Gonen M, Coit D, Dematteo RP, et al. Laparoscopic versus open gastric resections for primary gastrointestinal stromal tumors (GISTs): a size-matched comparison. Ann Surg Oncol. 2011;18:1599–1605. doi: 10.1245/s10434-010-1517-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tagaya N, Mikami H, Kogure H, Kubota K, Hosoya Y, Nagai H. Laparoscopic intragastric stapled resection of gastric submucosal tumors located near the esophagogastric junction. Surg Endosc. 2002;16:177–179. doi: 10.1007/s004640080158. [DOI] [PubMed] [Google Scholar]
- 7.Tagaya N, Mikami H, Igarashi A, Ishikawa K, Kogure H, Ohyama O. Laparoscopic local resection for benign nonepithelial gastric tumors. J Laparoendosc Adv Surg Tech A. 1997;7:53–58. doi: 10.1089/lap.1997.7.53. [DOI] [PubMed] [Google Scholar]
- 8.Dempsey DT, Kelberman IA, Dabezies MA. Laparoscopic resection of gastric leiomyosarcoma. J Laparoendosc Adv Surg Tech A. 1997;7:357–362. doi: 10.1089/lap.1997.7.357. [DOI] [PubMed] [Google Scholar]
- 9.Shim JH, Lee HH, Yoo HM, Jeon HM, Park CH, Kim JG, et al. Intragastric approach for submucosal tumors located near the Z-line: A hybrid laparoscopic and endoscopic technique. J Surg Oncol. 2011 Apr 04; doi: 10.1002/jso.21934. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 10.Uyama I, Ogiwara H, Takahara T, Kikuchi K, Iida S. Laparoscopic and minilaparotomy proximal gastrectomy and esophagogastrostomy: technique and case report. Surg Laparosc Endosc. 1995;5:487–491. [PubMed] [Google Scholar]
- 11.Dulucq JL, Wintringer P, Mahajna A. Totally laparoscopic trans-hiatal gastroesophagectomy for benign diseases of the esophago-gastric junction. World J Gastroenterol. 2007;13:285–288. doi: 10.3748/wjg.v13.i2.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ke ZW, Zheng CZ, Hu MG, Chen DL. Laparoscopic resection of submucosal tumor on posterior wall of gastric fundus. World J Gastroenterol. 2004;10:2850–2853. doi: 10.3748/wjg.v10.i19.2850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dresner SM, Griffin SM, Wayman J, Bennett MK, Hayes N, Raimes SA. Human model of duodenogastro-oesophageal reflux in the development of Barrett's metaplasia. Br J Surg. 2003;90:1120–1128. doi: 10.1002/bjs.4169. [DOI] [PubMed] [Google Scholar]
- 14.Tsiouris A, Hammoud Z, Velanovich V. Barrett's esophagus after resection of the gastroesophageal junction: effects of concomitant fundoplication. World J Surg. 2011 May 19; doi: 10.1007/s00268-011-1142-3. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]