Abstract
Quantitative proteomic methodologies allow profiling of hundreds to thousands of proteins in a high throughput fashion. This approach is increasingly applied to cancer biomarker discovery to identify proteins that are differentially regulated in cancers. Fractionation of protein samples based on enrichment of cellular subproteomes prior to mass spectrometric analysis can provide increased coverage of certain classes of molecules. We used a membrane protein enrichment strategy coupled with 18O labeling based quantitative proteomics to identify proteins that are highly expressed in cholangiocarcinomas. In addition to identifying several proteins previously known to be overexpressed in cholangiocarcinoma, we discovered a number of molecules that were previously not associated with cholangiocarcinoma. Using immunoblotting and immunohistochemical labeling of tissue microarrays, we validated Golgi membrane protein 1, Annexin IV and Epidermal growth factor receptor pathway substrate (Eps8) as candidate biomarkers for cholangiocarcinomas. Golgi membrane protein 1 was observed to be overexpressed in 89% of cholangiocarcinoma cases analyzed by staining tissue microarrays. In light of recent reports showing that Golgi membrane protein 1 is detectable in serum; further investigation into validation of this protein has the potential to provide a biomarker for early detection of cholangiocarcinomas.
Keywords: Liquid chromatography tandem mass spectrometry (LC-MS/MS), 18O stable isotope labeling, Quantitative proteomics, Gall bladder, Tissue microarrays, Immunohistochemistry
Introduction
Cholangiocarcinoma accounts for 3% of all gastrointestinal cancers in the world and represents the second most common hepatic tumor1, 2. In United States, about 7,500 people are diagnosed of cholangiocarcinoma every year and approximately 4,500 of them die3. At present, radiation or conventional chemotherapy does not significantly improve the survival rate, and early detection at a stage where the cancer is resectable offers the best hope for cure 4. However, laboratory tests for detection of biliary tract cancers are usually only modestly sensitive and specific, and distinguishing between benign and malignant causes of biliary tract obstruction based on biopsies is very difficult and often does not provide an accurate answer. Currently, CA19-9 is the best available fluid-based marker for detection of cholangiocarcinomas, which has a sensitivity of 50–60% and a specificity of 80% 5, 6. The use of CA19-9 in early-stage detection of cholangiocarcinomas is even more limited and better markers are needed to offer patients a better chance of survival.
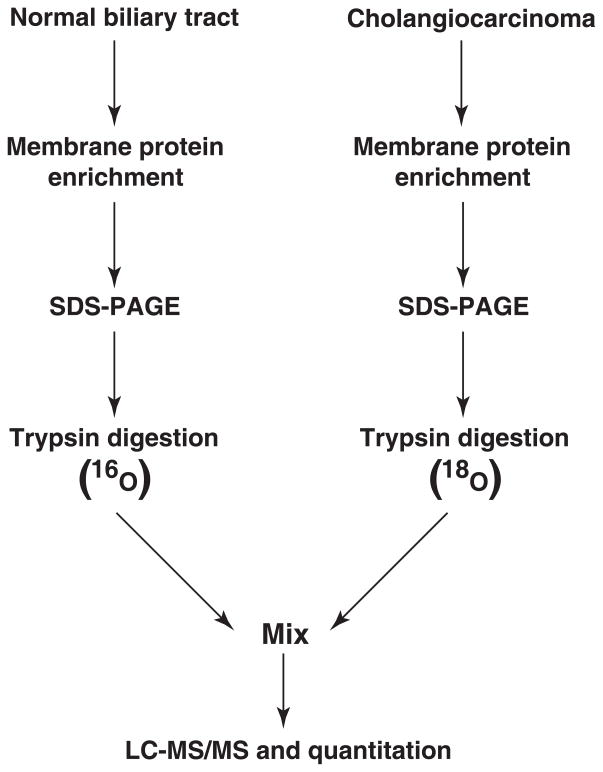
Though differential expression studies using cDNA and oligonucleotide microarrays have been undertaken, quantitative proteomic strategies for profiling cholangiocarcinomas have not been reported. Given that membrane or secreted protein biomolecules would serve as excellent biomarkers, we used preferential enrichment of membrane bound proteins followed by quantitative mass spectrometry to identify potential biomarkers for cholangiocarcinomas. Heavy water containing 18O was used to label the peptides derived from cholangiocarcinoma samples while the peptides from normal biliary tract membrane sample were labeled with 16O containing water. To identify commonly occurring but upregulated membrane proteins in cholangiocarcinoma, two independent cholangiocarcinoma membrane preparations were compared with a common normal. This resulted in the identification of several known as well as novel potential biomarkers. The candidate biomarkers identified were further validated by immunoblotting and immunohistochemical labeling of tissue microarrays.
Materials and methods
Sample preparation
This study was considered exempt by Johns Hopkins institutional review board (IRB) as the tissue samples were anonymized and delinked from direct patient identifiers. Two first passage xenografts from human cholangiocarcinomas were used for this study. The derivation of these low passage patient derived xenografts in athymic mice has been described previously7. Approximately 150 mg of frozen normal human biliary tract tissue or 150 mg of frozen xenografts derived from two human cholangiocarcinomas (designated A and B) were briefly rinsed in PBS. The rinsed tissues were blended in high salt buffer (2M NaCl, 10mM HEPES, pH 7.5, 1mM EDTA, pH 8.0) using a polytron tissue homogenizer (Kinematica AG, Littau-Lucerne, Switzerland). The disrupted tissue was centrifuged at 250,000 g for 45 min at 4°C. The supernatant was discarded, and the pellet was re-suspended in 0.1 M Na2CO3, pH 11 using polytron and left on ice for 45 min. The suspension was centrifuged as above and the pellet re-suspended in high salt buffer. The above steps were repeated once and the resulting pellet containing the membranous material was dissolved in NuPage sample buffer (Invitrogen, Carlsbad, California).
Electrophoresis, trypsin digestion and 18O labeling
25 μg of non-neoplastic human biliary tract membrane preparation and cholangiocarcinoma membrane preparation were resolved on adjacent lanes on a 4–12% NuPAGE gel (Invitrogen, Carlsbad, California). The gel was stained with colloidal coomassie. Both lanes were divided into equal sized slices from the exact same position in the gel. All gel slices were digested with sequencing grade trypsin (Promega, Madison, WI) as described8. Digestion of proteins from the cancer sample was carried out in the presence of H218O while the digestion of proteins from the corresponding normal was carried out in the presence of H216O. After in-gel digestion, the peptides were extracted in 30% water (H218O and H216O) and 70% acetonitrile and dried to approximately 5 μl in a speedvac. The peptides were end labeled with immobilized trypsin in order to achieve complete labeling of peptides with heavy oxygen increasing the peptide mass by 4 Da. Immobilized trypsin was bought from stratagene (Catalog # 271010). In order to achieve complete labeling of heavy oxygen, 1.5 μl of pre-washed immobilized trypsin suspension in 10 μl trypsin digestion buffer (50 mM Tris-HCl (pH 8), 50 mM CaCl2) was added to the extracted peptides and subsequently dried to completion in a speedvac maintained at 30°C. Depending on whether the peptides were designated for 16O or 18O labeling, the peptides were redissolved in either 8 μl H216O or H218O and 2 μl acetonitrile and end-labeled for 4 hours at 25°C. The reaction was stopped by adding 1 μl of concentrated formic acid. The immobilized trypsin was removed by repeated centrifugation and filtering through a gel-loader tip containing a small piece of silica tubing. Finally, the labeled samples were frozen at −80°C until further processing.
Liquid chromatography tandem mass spectrometry
For each pairwise comparison, labeled and unlabeled peptides from the in-gel digestion were mixed 1:1 immediately prior to analysis. First, the mix was manually desalted using micro-columns packed with R2 POROS material. After column loading, the peptides were washed 3× in 5% formic acid and eluted using 100% methanol. After elution, the peptides were briefly dried in a speedvac and reconstituted in 5% formic acid. The samples were analyzed by automated nanoflow liquid chromatography mass spectrometry. An Agilent 1100 series system (Agilent technologies, Palo Alto, CA) was used for the chromatographic separation of the peptides. The peptide mix was loaded onto an analytical column of 10 cm in length with an inner diameter of 75 μm packed with ODS-A (TMC, Ltd., Kyoto, Japan) and washed with 95% mobile phase A (100% H2O with 0.4% acetic acid and 0.005% heptafluorobutyric acid) and 5% mobile phase B (90% acetonitrile with 10% H2O, 0.4% acetic acid and 0.005% heptafluorobutyric acid). Subsequently, the peptides were eluted over 34 min from the column using a linear gradient of 10–40% mobile phase B at a flow rate of 250 nl/min. The eluted peptides were analyzed by a Micromass Q-TOF API-US (Manchester, UK) equipped with an ion source designed at Proxeon Biosystems (Odense, Denmark). The automated data-acquisition and generation of peak list files was carried out using MassLynx (version 4.0).
Data dependent acquisition parameters:
Scan cycle:
TOF survey scan: 0.9s (from 350m/z – 1500m/z).
MS/MS scans: 0.9s (for up to three selected precursor ions) (from 50–2000 m/z).
The interscan time for our instrument is 0.1s. For each survey scan, the three most intense ions in the spectrum were picked for MS/MS analysis, unless they appeared on the dynamic exclusion list, MS/MS to MS switch criteria: intensity falling below 3 counts/sec. Precursor ions selected for a given scan cycle were excluded for the next 45s of the LC-MS/MS run. Nitrogen was used as the collision gas and the collision energy was determined by charge state recognition for +2, +3 and +4 charged precursor ions.
Database searching and analysis
The peak list files were generated in MassLynx and were searched against the RefSeq database (release 11) using Mascot (version 1.9, Matrix Science) installed on a Linux cluster. The following parameters were used for searching the data: fixed modifications: carbamidomethyl modification of cysteines, variable modifications: oxidation of methionines, phosphorylation of serines, threonines and tyrosines, deamidation of asparagines, 18O modification of both C-terminal oxygen atoms on lysine and arginine residues. Peptide mass tolerance of +/− 0.4 Da and fragment ion (MS/MS) mass tolerance of +/− 0.3 Da was used. Proteins with at least one unique peptide with a Mascot score of ≥ 30 was considered for manual validation. Manually validated peptides were further used for relative quantitation using MSQuant software (http://msquant.sourceforge.net)
Western blotting
20 μg of dissolved membrane material in NuPAGE sample buffer was resolved on 4–12%, 1.5 mm Bis-Tris gels. The proteins were transferred on to nitrocellulose membrane, blocked in 5% BSA and incubated with the protein specific antibodies. Detection was carried out using horseradish peroxidase conjugated secondary antibodies using enhanced chemiluminescence detection reagent (Amersham Biosciences).
Antibodies
Anti-EPS8 (Catalog # 610144), Anti-Annexin IV (Catalog # A29920) and Anti-Moesin (Catalog # 610402) antibodies were purchased from BD Biosciences (San Jose, CA, USA). Anti-Calmyrin (Catalog # 35-4500) antibody was purchased from Zymed Laboratories (San Francisco, CA, USA). Anti-Golgi membrane protein 1 (Catalog # IMG-5280A) antibody was purchased from Imgenex (San Diego, CA, USA). Anti-Rab5A (Catalog # 18211-100) was purchased from Abcam (Cambridge, MA, USA). Anti-CD133 (Catalog # sc30219) and Anti-UQCRC1 (Catalog # sc65238) were purchased from Santa Cruz (Santa Cruz, CA, USA).
Immunohistochemistry
All the immunohistochemistry reagents were purchased from DAKO (Dako North America, Inc, CA, USA). Wash buffer (Catalog # S3006), target retrieval buffer (Catalog # S1699), antibody diluent (Catalog # S0809), secondary detection reagents for mouse primary antibody (Envision+ system-HRP, Catalog # K4007), for rabbit primary antibody (Envision+ system-HRP, Catalog # K4011). Immunohistochemical labeling was performed on tissue microarrays constructed at Johns Hopkins University. The TMAs contain histologically documented bile duct cancers arrayed in 1.4 mm cores. They include 10 intrahepatic cholangiocarcinomas, 15 distal common bile duct adenocarcinomas and 13 gall bladder carcinomas. They have been previously described in the literature9, 10. Protein specific antibodies were used at an appropriate dilution and tissue microarrays were scored in a blinded fashion by an expert in gastrointestinal pathology (A. M) with extensive familiarity in biliary cancer morphology and immunohistochemistry.
Results and discussion
Membrane proteome enrichment and 18O labeling
Membrane bound proteins represent more than half of the current drug targets, making membrane proteins the most common target for small molecules and biopharmaceuticals11, 12. In order to identify potential biomarkers of cholangiocarcinomas, a quantitative proteomic strategy was carried out following selective enrichment of membrane proteins. We employed sodium carbonate precipitation method for isolation of membrane proteins13. We used two different cholangiocarcinoma samples derived from xenografts and compared them to one normal bile duct sample. Briefly, the membrane samples from cholangiocarcinoma and normal biliary tract were resolved alongside each other on SDS-PAGE and stained with colloidal coomassie. The adjacent bands from both normal and cancer were excised and in-gel trypsin digestion was carried out in the presence of H216O and H218O respectively (Figure 1). Trypsin cleaves after every lysine and arginine and adds one or two oxygen atoms at the C-terminus of all peptides during proteolysis. In 18O based quantitative proteomic experiments, it is important to ensure addition of two 18O atoms at the C-termini of all the peptide species. However, this technique often suffers from variable incorporation of one or two 18O atoms resulting in a mixture of isotopic peaks. Addition of one 18O atom creates a mass shift of 2 Da and results in overlapping spectra during mass spectrometry. Several approaches have been used over the years to overcome this problem. Most of this has been attributed to the activity of trypsin after mixing 16O and 18O samples, which results in oxygen back exchange. To ensure near complete incorporation of two 18O atoms at the C-termini of all tryptic peptides, end labeling of the digested peptides was carried out using immobilized trypsin. As protease catalyzed oxygen back exchange reaction 14 is a point of concern in 18O based experiments, the samples were either maintained in acidic conditions or frozen at −80°C till they were subjected to LC-MS/MS.
Figure 1. Schematic illustrating the workflow of 18O labeling and comparison of membrane proteins derived from biliary tract and cholangiocarcinoma.
Membrane proteins were enriched from normal human biliary tract and cholangiocarcinoma, resolved by SDS-PAGE and subjected to trypsin digestion. The peptides derived from normal and cholangiocarcinoma membrane preparations were differentially labeled using 16O and 18O, respectively, and analyzed by liquid chromatography tandem mass spectrometry. Relative quantitation was carried out to determine the differential expression of the identified proteins.
Mass spectrometry and relative quantitation of proteins
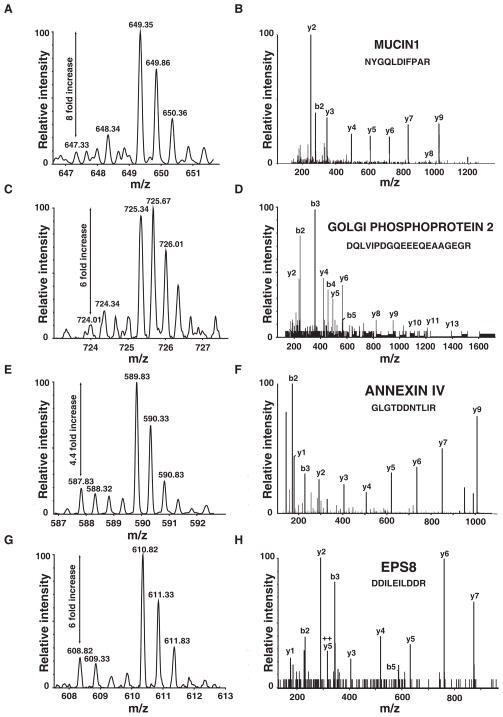
The samples from normal and cholangiocarcinoma membrane preparations were mixed and subjected to LC-MS/MS on a quadrupole time of flight mass spectrometer. The relative quantitation of proteins from both the samples was carried out based on the expected mass shift for the peptides derived from cholangiocarcinomas when compared to their normal counterparts (Figure 2). We verified the incorporation of two 18O atoms at the C-terminus of all the peptides by manually examining MS spectra of several peptides and by carrying out Mascot search with variable modifications involving both one and two 18O atoms. The majority of cases examined showed near complete incorporation of two 18O atoms with a very small percentage of peptide species with incorporation of only one 18O atom. Only peptides with incorporation of two 18O atoms were considered for relative quantitation. The quantitation was carried out using MSQuant (http://msquant.sourceforge.net/) software and all the results were validated manually. The list of proteins identified from sample A and B are provided as Supplementary table 1 and 2, respectively. A total of 52 proteins were found to be upregulated >2-fold in both cholangiocarcinoma samples (Supplementary table 3).
Figure 2. Representative mass spectra showing differential expression.
MS and representative MS/MS spectra of peptides derived from Mucin 1 (A, B), Golgi membrane protein 1 (C, D), Annexin IV (E, F) and EPS8 (G, H). The fold change (cancer/normal) is also indicated.
Identification of known biliary tract cancer markers
Among the overexpressed proteins, we found that a number of them had previously been described in the context of cholangiocarcinoma, confirming the validity of our quantitative proteomic approach (Table 1). These included several mucins and carcinoembryonic antigens among others. Mucins are a large group of glycoproteins that are predominantly expressed by the epithelial cells of the gastrointestinal and hepatobiliary organs. Mucins are frequently found to be increased in expression in a variety of cancers; for example, mucin 1 and mucin 5 are overexpressed in cholangiocarcinomas and gallbladder cancers and used for diagnostic purposes15–19. In agreement with these observations, we found both mucin 1 and mucin 5 to be highly elevated in biliary tract cancers. Among carcinoembryonic antigens, CEA and CEACAM6 were found to be overexpressed in our cholangicarcinoma samples. Table 2 shows a subset of the molecules that were identified as upregulated and have not been previously described in the context of cholangiocarcinomas.
Table 1.
A partial list of proteins previously reported as overexpressed in cholangiocarcinoma
| Protein | Fold change (Cancer/Normal) Sample A | Fold change (Cancer/Normal) Sample B | Accession number |
|---|---|---|---|
| Mucin 1 | 10.96 | 14.16 | NP_002447 |
| Mucin-5AC | 8.33 | 7.57 | XP_001130382 |
| Carcinoembryonic antigen-related cell adhesion molecule 5 | 10.66 | 8.83 | NP_004354 |
| Carcinoembryonic antigen-related cell adhesion molecule 6 | Not identified | 5.60 | NP_002474 |
| S100 calcium binding protein P | 7.05 | 12.7 | NP_005971 |
| Lipocalin 2 (oncogene 24p3) | Not identified | 8.20 | NP_005555 |
| Villin 2 | 6.59 | 5.03 | NP_003370 |
| Mucin 13 | Not identified | 2.36 | NP_149038 |
Table 2.
A partial list of proteins not previously associated with cholangiocarcinoma
| Protein | Fold change (Cancer/Normal) Sample A | Fold change (Cancer/Normal) Sample B | Accession number |
|---|---|---|---|
| Golgi membrane protein 1 | 6.59 | 2.77 | NP_057632 |
| Eps8 | Not identified | 6.21 | NP_004438 |
| Annexin IV | 4.28 | 4.4 | NP_001144 |
| CD133 (Prominin 1) | Not identified | 4.83 | NP_006008 |
| Calmyrin | Not identified | 5.37 | NP_006375 |
| Moesin | Not identified | 5.01 | NP_002435 |
| Rab5A | Not identified | 2.23 | NP_004153 |
Novel proteins identified to be differentially expressed in cholangiocarcinomas
Golgi membrane protein 1 or GP73 (GOLM1) is a Golgi transmembrane protein expressed in epithelial cells. The biological function of this protein has not yet been established, although recent reports indicate that expression of the protein is upregulated in acute and chronic liver diseases. Elevated expression of Golgi membrane protein in the liver is associated with both non-viral and viral diseases (such as hepatitis C and cirrhosis)20. Recently, GP73 was identified to be hyperfucosylated and upregulated in a glycoproteomics screen using 2D gels to identify serum markers for liver cancer21. More recently, a follow up study demonstrated that GP73 can be used as a serum marker for early detection of hepatocellular carcinoma, and that it performs better than alpha-fetoprotein, which is the serum marker currently recommended for monitoring hepatocellular carcinoma in patients with cirrhosis22, 23. We found Golgi membrane protein 1 to be upregulated 6.0 fold and 2.8 fold, respectively, in the two cholangiocarcinoma samples that we analyzed (Figure 2C, Table 2).
Annexin IV belongs to the annexin family of calcium-dependent phospholipid binding proteins. It was originally cloned as a member of the phospholipase A2 inhibitor family, which binds phospholipids and inhibits coagulation24, 25. The function of Annexin IV is poorly understood. Like the rest of the annexin family, it is believed to be involved in regulation of membrane mobility and exo- and endocytosis26. In a 2DE proteomics scan of renal cell carcinoma, annexin IV was found to be upregulated in tumor cells and immunohistochemistry showed the protein to have altered localization in the tumor cells compared to normal tissue27. Ca2+-induced annexin IV membrane aggregation strongly reduces the mobility of membrane and plasma associated proteins and it has thus been proposed that annexin 4 could play an important role in morphological specialization of tumor cells. In our experiments, we found annexin IV to be overexpressed 4.4 fold in both the cancer tissues as compared to normal (Figure 2E, Table 2). Although its role in membrane remodelling in cancer cells has not yet been established, it would be interesting to investigate how annexin IV affects migration and invasion of cholangiocarcinoma cells.
EGFR pathway substrate 8 (Eps8) was originally identified as a 97 kDa direct modulator of EGFR phosphorylation mediated signaling. It contains an N-terminal PTB (phosphotyrosine binding domain), a SH3 domain in the middle region and a C-terminal GTPase activating domain. The EPS8 complex exhibits Rac-specific GEF activity, and Rac mediated cytoskeletal remodeling induced by receptor tyrosine kinases is dependent on the presence of EPS828. EPS8 also forms a complex with IRSp53, which is an adaptor molecule involved in RhoGTPase filopodium formation and actin cytoskeleton reorganization. Precluding complex formation between IRSp53 and EPS8 severely hampers cell motility and invasiveness of a cancer cell line29. Whether EPS8 is important for metastasis in vivo has not yet been determined. Our studies revealed ~6 fold increase in EPS8 expression levels in cholangiocarcinoma tissue (Figure 2G, Table 2).
Calmyrin or CIB (Calcium and integrin binding protein) is a membrane localized 22 kDa protein that is poorly described in the literature. It is primarily defined through its interaction with platelet integrin αIIbβ3, which occurs between the putative membrane spanning region in calmyrin and the cytoplasmic tail of αIIb30. The interaction between calmyrin and integrin αIIb is required for lamellipodia formation in platelets and necessary for spreading on fibrinogen31. The spreading and migration is dependent on calmyrin mediated Rac3 and focal adhesion kinase activation, which propagates the downstream signaling events32, 33. A few integrin-independent roles for calmyrin have been reported. calmyrin is a direct activator of PAK1 activity and is required for normal PAK1 mediated cellular migration. This activation is independent of Cdc42 and Rac, which are the most widely studied PAK1 activators. CIB has also been shown to interact with presenilin-2, which is known to be mutated at high frequencies in familial Alzheimer disease cases. calmyrin itself displays abnormal distribution in the forebrain of patients with Alzheimer’s and has been suggested to be involved in the pathogenesis of the disease34. Calmyrin was identified only in one of the membrane samples analyzed by mass spectrometry (Table 2, Supplementary table 2) and showed >5 fold overexpression.
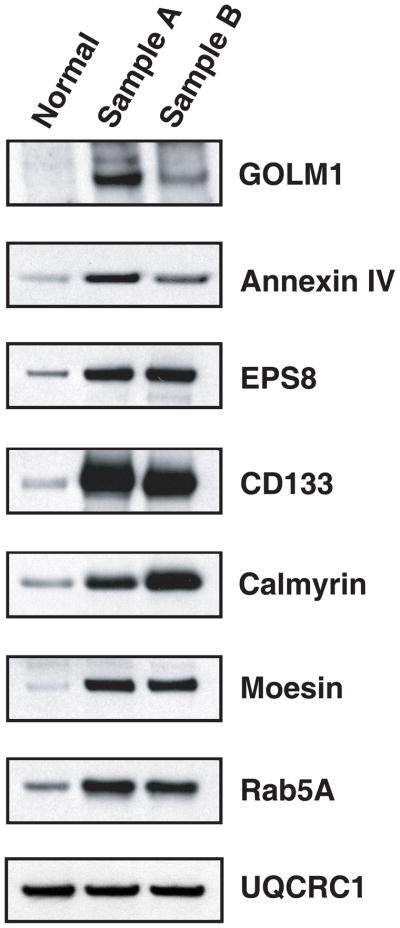
Validation of potential biomarkers
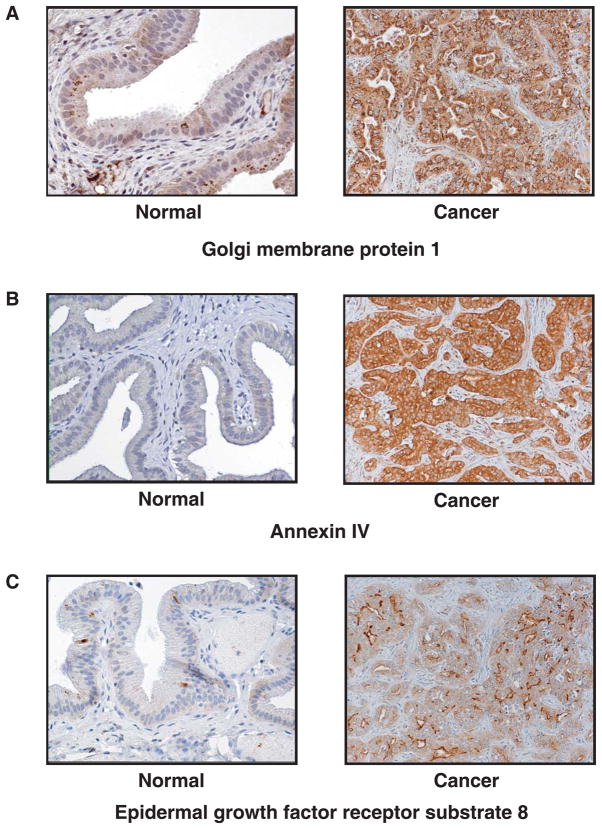
In order to confirm normalization of tissue samples, UQCRC1, a mitochondrial membrane protein part of normal cellular metabolism was validated by immunoblotting using tissue lysates used for proteomic analysis (Figure 3). The expression of UQCRC1 remained unchanged in both normal and cancer samples. This was in agreement with the ratios observed by mass spectrometry. Subsets of potential biomarkers identified through quantitative proteomics were further validated by immunoblotting and immunohistochemical labeling. One of the important criteria we considered while validating candidate biomarkers was the novelty of the finding and the availability of commercial antibodies to test on clinical samples. Immunoblotting of Golgi membrane protein 1, annexin IV, Eps8, CD133, calmyrin, moesin, and rab5A was carried out on both the membrane samples. Although some of these protein molecules had not been identified in both samples by mass spectrometry, all of them were found to be overexpressed in both cholangiocarcinoma samples analyzed by immunoblotting (Figure 3). This is because in LC-MS/MS type experiments, not every peptide is fragmented in every experiment. Further, we validated three proteins, Golgi membrane protein 1, annexin IV and Eps8 by immunohistochemical labeling using tissue microarrays. Tissue microarrays containing 36 cholangiocarcinoma tissue sections were stained using protein specific antibodies. Golgi membrane protein 1 was found to be overexpressed in 32 out of 36 (89%) cases (Figure 4A); robust expression of annexin IV was found in 16 out of 36 (44%) (Figure 4B) and Eps8 overexpression was found in 12 out of 36 (33%) cholangiocarcinoma cases (Figure 4C). As all the sections had been verified by a pathologist for the presence of cancer, the false negative rates for the candidate markers validated by immunohistochemical labeling were 11%, 56% and 67% for Golgi membrane protein 1, Annexin IV and EPS8 respectively. Golgi membrane protein 1, which showed overexpression in majority of cholangiocarcinomas that were immunohistochemically labeled, has been previously implicated in hepatocellular carcinoma and has also been shown to be secreted into blood22, 23. Golgi membrane protein 1 is an attractive candidate for further validation as a biomarker for early detection of cholangiocarcinomas, especially given that it is detectable in blood.
Figure 3. Validation of candidate biomarkers by immunoblotting.
The membrane samples from normal bile duct and cholangiocarcinoma preparation were resolved by SDS-PAGE gels and blotted onto a nitrocellulose membrane. Detection of the target proteins was carried out by horseradish peroxidase conjugated system using enhanced chemiluminescence detection reagents.
Figure 4. Immunohistochemical validation of candidate biomarkers.
Immunohistochemical labeling of cholangiocarcinoma sections was carried out using antibodies specific for Golgi membrane protein 1 (A), Annexin IV (B) and Eps8 (C). Positive staining is marked by brown color.
Conclusions
In this study, we have used pairwise comparison of two cholangiocarcinoma samples to the same normal bile duct tissue. This is mainly because in the 18O-labeling method, only two samples can be compared at a time. The two major ways that one could accomplish higher multiplexing is by pooling the samples prior to analysis or by analyzing multiple samples of the same type. In any case, using isotope labeling methods, it is difficult to multiplex a really large number of samples and one has to resort to identifying potential candidates from a small number of samples and later apply them to a larger set of samples using other platforms like tissue microarrays or ELISA. Although our study is done on limited sample numbers, we have identified several potential proteins that are differentially regulated in cholangiocarcinoma. As the study is carried out following membrane enrichment from the tumors, the identified proteins are potentially useful as biomarkers as well as possible targets for therapy. However, the validity of identified proteins as potential biomarkers should be further tested by alternative methods on panels of large number of tumors derived from different patients. Using this approach, we were able to identify several overexpressed proteins that had no previous association with cholangiocarcinoma. A subset of these candidate biomarkers, when further tested in a larger set of samples using immunohistochemical labeling of tissue microarrays, showed that the changes that we identified from two samples were observed in 33% to 89% of cases. Particularly interesting was Golgi membrane protein 1, which was overexpressed in both the cholangiocarcinoma samples we studied, and showed promising results in tissue microarrays where 89% of the tumor sections on the array showed overexpression of this protein. In the future, reagents like iTRAQ35 or ExacTag, could be used to multiplex up to eight or ten samples, respectively.
The other approach that could be adopted is to pool the samples prior to analysis. One of the major advantages of the pooling approach is that candidate biomarkers that are identified after pooling should theoretically be more reliable (fewer false positives) as they would account for tumor heterogeneity in the initial step. A disadvantage of pooling, however, is the possibility of masking real signals that are found in many but not all samples (false negatives). In any case, our results clearly demonstrate quantitative proteomics as an efficient tool to study cancer biomarkers even when one analyzes a small number of samples in the discovery phase. By carrying out quantitative membrane proteomics and validating subsets of these using immunoblotting and immunohistochemical staining, we have generated a list of candidate biomarkers for cholangiocarcinoma for more detailed investigation.
Supplementary Material
Synopsis.
18O based quantitative proteomics has been carried out to identify membrane proteins differentially expressed in cholangiocarcinomas. Subsets of potential biomarkers identified through quantitative proteomics were further validated by immunoblotting and immunohistochemical labeling of cholangiocarcinoma tissue samples. Golgi membrane protein 1(GOLM1) was found to be overexpressed in majority of cancer samples analyzed. With recent reports on detection of GOLM1 in serum, further studies to test utility of this protein as a serum marker for cholangiocarcinoma would prove valuable.
Acknowledgments
A.P. was funded by funded by the family of Margaret Lee and NCI SPORE P50 CA 62924.
References
- 1.Khan SA, Taylor-Robinson SD, Toledano MB, Beck A, Elliott P, Thomas HC. Changing international trends in mortality rates for liver, biliary and pancreatic tumours. J Hepatol. 2002;37:806–813. doi: 10.1016/s0168-8278(02)00297-0. [DOI] [PubMed] [Google Scholar]
- 2.Khan SA, Thomas HC, Davidson BR, Taylor-Robinson SD. Cholangiocarcinoma. Lancet. 2005;366:1303–1314. doi: 10.1016/S0140-6736(05)67530-7. [DOI] [PubMed] [Google Scholar]
- 3.de Groen PC, Gores GJ, LaRusso NF, Gunderson LL, Nagorney DM. Biliary tract cancers. N Engl J Med. 1999;341:1368–1378. doi: 10.1056/NEJM199910283411807. [DOI] [PubMed] [Google Scholar]
- 4.Gores GJ. Early detection and treatment of cholangiocarcinoma. Liver Transpl. 2000;6:S30–34. doi: 10.1053/jlts.2000.18688. [DOI] [PubMed] [Google Scholar]
- 5.Bjornsson E, Kilander A, Olsson R. CA 19-9 and CEA are unreliable markers for cholangiocarcinoma in patients with primary sclerosing cholangitis. Liver. 1999;19:501–508. doi: 10.1111/j.1478-3231.1999.tb00083.x. [DOI] [PubMed] [Google Scholar]
- 6.Patel AH, Harnois DM, Klee GG, LaRusso NF, Gores GJ. The utility of CA 19-9 in the diagnoses of cholangiocarcinoma in patients without primary sclerosing cholangitis. Am J Gastroenterol. 2000;95:204–207. doi: 10.1111/j.1572-0241.2000.01685.x. [DOI] [PubMed] [Google Scholar]
- 7.Rubio-Viqueira B, Jimeno A, Cusatis G, Zhang X, Iacobuzio-Donahue C, Karikari C, Shi C, Danenberg K, Danenberg PV, Kuramochi H, Tanaka K, Singh S, Salimi-Moosavi H, Bouraoud N, Amador ML, Altiok S, Kulesza P, Yeo C, Messersmith W, Eshleman J, Hruban RH, Maitra A, Hidalgo M. An in vivo platform for translational drug development in pancreatic cancer. Clin Cancer Res. 2006;12:4652–4661. doi: 10.1158/1078-0432.CCR-06-0113. [DOI] [PubMed] [Google Scholar]
- 8.Shevchenko A, Wilm M, Vorm O, Mann M. Mass spectrometric sequencing of proteins silver-stained polyacrylamide gels. Anal Chem. 1996;68:850–858. doi: 10.1021/ac950914h. [DOI] [PubMed] [Google Scholar]
- 9.Swierczynski SL, Maitra A, Abraham SC, Iacobuzio-Donahue CA, Ashfaq R, Cameron JL, Schulick RD, Yeo CJ, Rahman A, Hinkle DA, Hruban RH, Argani P. Analysis of novel tumor markers in pancreatic and biliary carcinomas using tissue microarrays. Hum Pathol. 2004;35:357–366. doi: 10.1016/j.humpath.2003.10.012. [DOI] [PubMed] [Google Scholar]
- 10.Hustinx SR, Hruban RH, Leoni LM, Iacobuzio-Donahue C, Cameron JL, Yeo CJ, Brown PN, Argani P, Ashfaq R, Fukushima N, Goggins M, Kern SE, Maitra A. Homozygous deletion of the MTAP gene in invasive adenocarcinoma of the pancreas and in periampullary cancer: a potential new target for therapy. Cancer Biol Ther. 2005;4:83–86. doi: 10.4161/cbt.4.1.1380. [DOI] [PubMed] [Google Scholar]
- 11.Russ AP, Lampel S. The druggable genome: an update. Drug Discov Today. 2005;10:1607–1610. doi: 10.1016/S1359-6446(05)03666-4. [DOI] [PubMed] [Google Scholar]
- 12.Hopkins AL, Groom CR. The druggable genome. Nat Rev Drug Discov. 2002;1:727–730. doi: 10.1038/nrd892. [DOI] [PubMed] [Google Scholar]
- 13.Fujiki Y, Hubbard AL, Fowler S, Lazarow PB. Isolation of intracellular membranes by means of sodium carbonate treatment: application to endoplasmic reticulum. J Cell Biol. 1982;93:97–102. doi: 10.1083/jcb.93.1.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sevinsky JR, Brown KJ, Cargile BJ, Bundy JL, Stephenson JL., Jr Minimizing back exchange in 18O/16O quantitative proteomics experiments by incorporation of immobilized trypsin into the initial digestion step. Anal Chem. 2007;79:2158–2162. doi: 10.1021/ac0620819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ghosh M, Kamma H, Kawamoto T, Koike N, Miwa M, Kapoor VK, Krishnani N, Agrawal S, Ohkohchi N, Todoroki T. MUC 1 core protein as a marker of gallbladder malignancy. Eur J Surg Oncol. 2005;31:891–896. doi: 10.1016/j.ejso.2005.03.008. [DOI] [PubMed] [Google Scholar]
- 16.Sasaki M, Nakanuma Y. Abnormal expression of MUC1 apomucin and mature MUC1 mucin in biliary epithelial cells in various cystic liver diseases. Hepatology. 1996;24:539–543. doi: 10.1053/jhep.1996.v24.pm0008781320. [DOI] [PubMed] [Google Scholar]
- 17.Sasaki M, Nakanuma Y. Frequent expression of MUC1 apomucin on biliary epithelial cells of damaged small bile ducts in primary biliary cirrhosis and chronic viral hepatitis: an immunohistochemical study. Hepatology. 1996;23:1313–1317. doi: 10.1053/jhep.1996.v23.pm0008675144. [DOI] [PubMed] [Google Scholar]
- 18.Takagawa M, Muguruma N, Oguri K, Imoto Y, Okamoto K, Ii K, Ito S. Prediction of prognosis in gallbladder carcinoma by mucin and p53 immunohistochemistry. Dig Dis Sci. 2005;50:1410–1413. doi: 10.1007/s10620-005-2854-8. [DOI] [PubMed] [Google Scholar]
- 19.Sasaki M, Nakanuma Y, Kim YS. Characterization of apomucin expression in intrahepatic cholangiocarcinomas and their precursor lesions: an immunohistochemical study. Hepatology. 1996;24:1074–1078. doi: 10.1002/hep.510240516. [DOI] [PubMed] [Google Scholar]
- 20.Iftikhar R, Kladney RD, Havlioglu N, Schmitt-Graff A, Gusmirovic I, Solomon H, Luxon BA, Bacon BR, Fimmel CJ. Disease- and cell-specific expression of GP73 in human liver disease. Am J Gastroenterol. 2004;99:1087–1095. doi: 10.1111/j.1572-0241.2004.30572.x. [DOI] [PubMed] [Google Scholar]
- 21.Block TM, Comunale MA, Lowman M, Steel LF, Romano PR, Fimmel C, Tennant BC, London WT, Evans AA, Blumberg BS, Dwek RA, Mattu TS, Mehta AS. Use of targeted glycoproteomics to identify serum glycoproteins that correlate with liver cancer in woodchucks and humans. Proc Natl Acad Sci U S A. 2005;102:779–784. doi: 10.1073/pnas.0408928102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schwegler EE, Cazares L, Steel LF, Adam BL, Johnson DA, Semmes OJ, Block TM, Marrero JA, Drake RR. SELDI-TOF MS profiling of serum for detection of the progression of chronic hepatitis C to hepatocellular carcinoma. Hepatology. 2005;41:634–642. doi: 10.1002/hep.20577. [DOI] [PubMed] [Google Scholar]
- 23.Marrero JA, Romano PR, Nikolaeva O, Steel L, Mehta A, Fimmel CJ, Comunale MA, D’Amelio A, Lok AS, Block TM. GP73, a resident Golgi glycoprotein, is a novel serum marker for hepatocellular carcinoma. J Hepatol. 2005;43:1007–1012. doi: 10.1016/j.jhep.2005.05.028. [DOI] [PubMed] [Google Scholar]
- 24.Grundmann U, Amann E, Abel KJ, Kupper HA. Isolation and expression of cDNA coding for a new member of the phospholipase A2 inhibitor family. Behring Inst Mitt. 1988:59–67. [PubMed] [Google Scholar]
- 25.Hauptmann R, Maurer-Fogy I, Krystek E, Bodo G, Andree H, Reutelingsperger CP. Vascular anticoagulant beta: a novel human Ca2+/phospholipid binding protein that inhibits coagulation and phospholipase A2 activity. Its molecular cloning, expression and comparison with VAC-alpha. Eur J Biochem. 1989;185:63–71. doi: 10.1111/j.1432-1033.1989.tb15082.x. [DOI] [PubMed] [Google Scholar]
- 26.Piljic A, Schultz C. Annexin A4 self-association modulates general membrane protein mobility in living cells. Mol Biol Cell. 2006;17:3318–3328. doi: 10.1091/mbc.E06-01-0041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zimmermann U, Balabanov S, Giebel J, Teller S, Junker H, Schmoll D, Protzel C, Scharf C, Kleist B, Walther R. Increased expression and altered location of annexin IV in renal clear cell carcinoma: a possible role in tumour dissemination. Cancer Lett. 2004;209:111–118. doi: 10.1016/j.canlet.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 28.Di Fiore PP, Scita G. Eps8 in the midst of GTPases. Int J Biochem Cell Biol. 2002;34:1178–1183. doi: 10.1016/s1357-2725(02)00064-x. [DOI] [PubMed] [Google Scholar]
- 29.Funato Y, Terabayashi T, Suenaga N, Seiki M, Takenawa T, Miki H. IRSp53/Eps8 complex is important for positive regulation of Rac and cancer cell motility/invasiveness. Cancer Res. 2004;64:5237–5244. doi: 10.1158/0008-5472.CAN-04-0327. [DOI] [PubMed] [Google Scholar]
- 30.Barry WT, Boudignon-Proudhon C, Shock DD, McFadden A, Weiss JM, Sondek J, Parise LV. Molecular basis of CIB binding to the integrin alpha IIb cytoplasmic domain. J Biol Chem. 2002;277:28877–28883. doi: 10.1074/jbc.M202983200. [DOI] [PubMed] [Google Scholar]
- 31.Naik UP, Naik MU. Association of CIB with GPIIb/IIIa during outside-in signaling is required for platelet spreading on fibrinogen. Blood. 2003;102:1355–1362. doi: 10.1182/blood-2003-02-0591. [DOI] [PubMed] [Google Scholar]
- 32.Naik MU, Naik UP. Calcium-and integrin-binding protein regulates focal adhesion kinase activity during platelet spreading on immobilized fibrinogen. Blood. 2003;102:3629–3636. doi: 10.1182/blood-2003-05-1703. [DOI] [PubMed] [Google Scholar]
- 33.Haataja L, Kaartinen V, Groffen J, Heisterkamp N. The small GTPase Rac3 interacts with the integrin-binding protein CIB and promotes integrin alpha(IIb)beta(3)-mediated adhesion and spreading. J Biol Chem. 2002;277:8321–8328. doi: 10.1074/jbc.M105363200. [DOI] [PubMed] [Google Scholar]
- 34.Bernstein HG, Blazejczyk M, Rudka T, Gundelfinger ED, Dobrowolny H, Bogerts B, Kreutz MR, Kuznicki J, Wojda U. The Alzheimer disease-related calcium-binding protein Calmyrin is present in human forebrain with an altered distribution in Alzheimer’s as compared to normal ageing brains. Neuropathol Appl Neurobiol. 2005;31:314–324. doi: 10.1111/j.1365-2990.2005.00646.x. [DOI] [PubMed] [Google Scholar]
- 35.DeSouza L, Diehl G, Rodrigues MJ, Guo J, Romaschin AD, Colgan TJ, Siu KW. Search for cancer markers from endometrial tissues using differentially labeled tags iTRAQ and cICAT with multidimensional liquid chromatography and tandem mass spectrometry. J Proteome Res. 2005;4:377–386. doi: 10.1021/pr049821j. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.