Abstract
Purpose
We have treated 24 patients through laparoscopic totally extraperitoneal (TEP) repair without suprapubic port by using reliability and reducing the invasiveness of two surgery. This study is aimed to assess the safety and feasibility of the TEP repair without suprapubic port compared to conventional TEP repair.
Methods
From September 2007 to 11 May 2010, we compared two groups that suffer from inguinal hernias. One is comprised of 24 patients who were treated without suprapubic port laparoscopic totally extraperitoneal repair (Group A), and the other is comprised of 100 patients who were treated with conventional laparoscopic totally extraperitoneal repair (Group B). Data regarding patient demographics (sex, age, site of hernia, and the type of hernia), operating time, postoperative hospital stay, the use of analgesics, and complications were prospectively collected.
Results
There was no significant difference noted between two groups in relation to sex, age, site, and the type of hernia. The mean operating time and postoperative hospital stay was longer for the Group B (62.9 minutes, 3.55 days) than for the Group A (59.0 minutes, 2.54 days) (P = 0.389, P < 0.001). Postoperative urinary retention, seroma, wound infection were respectively 4.2%, 8.3%, 0% in Group A, and 12.0%, 8.0%, 7% in group B. There was difference between the two groups, but not statistical significance. Group B used more analgesics than Group A (0.33 vs. 0.48), but it wasn't significant statistically (P = 0.234).
Conclusion
Although prospective randomized studies with long-term follow-up evaluation are needed to confirm our study between laparoscopic totally extraperitoneal repair without suprapubic-port and conventional laparoscopic totally extraperitoneal repair, our method have some advantages in postoperative pain, urinary retention, operating time, postoperative hospital stay, and cosmetic effect.
Keywords: Inguinal hernia, Laparoscopic surgery, Totally extraperitoneal repair
INTRODUCTION
Inguinal herniorrhaphy is one of surgeries that have been performed most frequently in the department of surgery. Since Bassini described a method in 1887, numerous surgical methods have been introduced [1]. The laparoscopic repair of a inguinal hernia was initiated from the early 1990s, and recently, totally extraperitoneal (TEP) inguinal herniorrhaphy has been applied worldwide. Several studies have reported that pain after surgery is less, the recovery period is short, and mortality rate is low [2-6]. Particularly, with the increase of interests from the aspect of esthetics and the improvement of minimal invasive surgery, after 2009, single incision laparoscopic totally extraperitoneal inguinal herniorrhaphy has been reported continuously [7-9]. However, in single incision laparoscopic totally extraperitoneal inguinal herniorrhaphy, periumbilical skin incision reaches 25 to 45 mm. However, in single incision laparoscopic totally extraperitoneal inguinal herniorrhaphy, periumbilical skin incision reaches 25 to 45 mm. Consequently, the possibility of hernia through the incision area [8,9], the crowding phenomenon and collision due to small surgical spaces [9], requirement of additional surgical instruments, and prolonged operation time, etc. have been pointed out to be problems. In conventional laparoscopic inguinal herniorrhaphy, significantly high urinary retention in comparison with open abdominal herniorrhaphy has been reported [10,11]. Therefore, we applied single incision laparoscopic inguinal herniorrhaphy but the length of periumbilical skin incision was limited to 15 mm, and by placing an additional trocar in the area below the umbilicus by 5 cm, the TEP procedure without using supurapubic trocars was attempted. We examined whether the operation time of our procedure was different from conventional procedures, and postsurgical short-term outcomes and clinical features were compared and analyzed.
METHODS
Subjects and methods
Selected from the entire 141 patients who were diagnosed as inguinal hernia, admitted to the department of surgery, and received inguinal herniorrhaphy from September 2007 to May 2010, the subjects were 24 patients who received laparoscopic TEP repair without suprapubic port (Group A) and 100 patients who received conventional laparoscopic TEP repair (Group B). Based on medical records and telephone interviews, the data on operation time, the hospitalization period after surgery, the dose of administered analgesics, postsurgical pain, and complications were collected, compared, and analyzed. Follow-up observation periods were average 19 months (range, 4 to 35 months). For the reduction of the errors on operation time and the pain level, 17 cases who received bilateral herniorrhaphy were excluded. For statistical analysis, chi-square test and t-test were applied. Cases with P value lower than 0.05 were considered to be statistically significant.
Conventional laparoscopic TEP surgical methods
General anesthesia was performed on the entire cases. In the supine position, a skin transverse incision approximately 15 mm in length including the umbilicus was made in the area immediately below the umbilicus, and the anterior rectus sheath of rectus abdominis muscle was opened. Using a balloon trocar (Spacemaker, Autosuture, Norwalk, CT, USA), the extraperitoneal space was secured. A 10 mm 30° laparoscope was inserted, and while assessing macroscopically the balloon was expanded slowly, and the balloon was broken and removed. 20 mL air was added to a trocar, CO2 gas was added until it reaches 12 mmHg, and a 10 mm 30° laparoscope was inserted. In the area immediately above the symphysis pubis, a 5 mm trocar was inserted, and in the area between the insertion site of laparoscope and the insertion site of 5 mm trocar, another 5 mm trocar was inserted. In the medial side, to the midline and the symphysis pubis, in the lateral side, to the anterior superior iliac spine, in the inferior area, from the area below the Cooper's ligaments to the psoas muscle, and in the anterior area, the rectus abdominis muscle was exposed sufficiently. The hernia sac was assessed, and after reduction, the posterior wall was strengthened by the use of commercialized polyester mesh 6 × 4 inch in size (Parietex, Sofradim, Formans, France). The mesh was fixed to the vicinity of the inferior epigastric artery using one Tacker (Autosuture), and the vicinity of the Cooper's ligament was fixed by the use of the Tissel (Baxter AG, Vienna, Austria). For direct hernia cases, the transversalis fascia was fixed to the Cooper's ligament using 1-2 Tacker (Autosuture) and the Tissel. The mesh was spread sufficiently, CO2 gas was blocked, and the gas was released slowly through the trocar placed in the suprapubic area, and the trocar was removed while assessing that the artificial mesh maintained the spread state until the gas was released completely.
The surgical procedure of laparoscopic TEP herniorrhaphy without suprapubic port
The method identical to conventional laparoscopic TEP herniorrhaphy was applied until the breaking and removal of balloon. Afterward, a wound tractor (Utractor, Yoohan Medical, Daegu, Korea) was inserted to the posterior area of the rectus abdomionin muscle. The indicis finger and the 5th finger of surgical glove were cut, two 5 mm trocars were inserted, fixed with silk to prevent the leakage of air, and fixed to the wound tractor (Fig. 1). Through the 5 mm trocar, a 5 mm 30° laparoscope (Endoeye, Olympus, Tokyo, Japan) was inserted, an additional 5 mm trocar was inserted to the area between the wound tractor and the symphysis pubis, and the reduction of the hernia sac was performed by the method identical to conventional TEP herniorrhaphy. The surgical glove was removed from the wound tractor temporarily, a polyester mesh 6 × 4 inch in size was inserted to the extraperitoneal space, and the surgical glove was fixed agin to the wound tractor. After fixing the mesh by the method identical to conventional TEP herniorrhaphy, the trocars, surgical glove and wound tractor were removed.
Fig. 1.
Image of port insertion state.
RESULTS
Clinical features
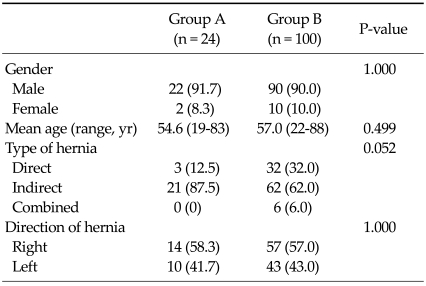
Of the entire subjects 124 patients, the male was 90.3%, the female was 9.7%, and the ratio of indirect inguinal hernia was higher (66.9%). The gender, average age, site and type of inguinal hernia of the Group A and the Group B were not significantly different (Table 1). In regard to associated diseases, the underlying disease of 24 Group A patients was that diabetes was 3 patients, hypertension was 5 patients, and prostatic hyperplasia under medication was 2 patients. Of 100 Group B patients, diabetes was 7 patients, hypertension was 23 patients, and prostatic hyperplasia was 7 patients. A significant difference between the two groups was not detected.
Table 1.
Clinical characteristics of patients
Values are presented as number (%) or mean age (range).
Operation time, hospitalization period, and postsurgical pain
The operation time of the Group A was average 59.0 ± 16.2 minutes, and it was shorter than 62.9 ± 20.6 minutes of the Group B. Nonetheless, the difference was not statistically significant (P = 0.389). The hospitalization period after surgery of the Group A was average 2.54 ± 0.65 days, and it was statistically significantly shorter than 3.55 ± 0.97 days of the Group B (P < 0.001). The pain immediately after surgery was evaluated by the number of the administration of analgesics during the hospitalization period. The number of the administration of analgesics was compared, and it was observed that the group A was average 0.33 times, and the Group B was average 0.48 times. Analgesics were used less frequently in the Group A, nonetheless, a statistically significant difference was not shown (Table 2).
Table 2.
Clinical outcomes of patients
Values are presented as mean ± SD or number (%).
Postsurgical complications
As postsurgical complications, urinary retention, postsurgical fluid retention, wound infection, and bladder perforation were assessed. Regarding urinary retention, in the Group A, it was developed in 4.2% after surgery, and in the Group B, urinary retention was detected in 12%. The difference between the two groups was 7.8%, however, it was not statistically significant (P = 0.460). In regard to body fluid retention after surgery, it was 8.3% in the Group A and 8.0% in the Group B. Wound infection of the Group A was 0% and the Group B was 7.0%. Both were not statistically significant. (P = 1.000, P = 0.344) (Table 2). Bladder perforation was detected in 1 case of the Group B during the dissection of hernia sac, and after suturing, it was healed by conservative treatments.
Chronic pain and recurrence
According to the definition of the International Association of the study of Pain, chronic pain was defined as pain persistent for longer than 3 months [12]. The level of pain was defined as the pain at the level that impairs routine life and thus the administration of analgesics is required. During the average 23 months follow-up observation period, 1 patient each of the Group A and the Group B presented with chronic pain. It was determined to be chronic pain in the Tacker fixation area, and after conservative treatments, symptoms were improved. The recurrence of inguinal hernia after surgery was not observed in both groups during the follow-up observation period.
DISCUSSION
For the treatment of inguinal hernia, numerous studies and attempts have been made for a long time, and nowadays, several surgical procedures have been performed. Inguinal herniorrhaphy was established by Bassini in 1887 [1]. Afterward, Lichtenstein and Shore performed notension herniorrhaphy using the Marlex mesh made of polypropylene and polyethylene in 1989, and afterward, the procedure has been used as the representative surgical method of herniorrhaphy [13,14]. In 1993, Ger et al. [15] performed laparoscopic inguinal herniorrhaphy on dogs, and afterward, diverse surgical methods using caps or meshes have been reported [16]. In regard to laparoscopic inguinal herniorrhaphy, transabdominal totally peritoneal herniorrhaphy that has been performed by Arregui et al. [17] for the first time in 1992 and totally extraperitoneal herniorrhaphy performed in 1993 by McKernan and Laws [18] for the first time have been performed worldwide.
The advantages of laparoscopic inguinal herniorrhaphy are that postsurgical pain is less severe, the recovery period is short, and thus the early return to routine life is possible. In addition, since it is performed within tissues that were not dissected previously, recurrent hernia could be repaired readily, bilateral hernia could be repaired by a single surgery, the ligation of the uppermost hernia sac is possible, and esthetics are good [2-6,19]. Nevertheless, it requires general anesthesia, and although the results vary depending on reports, the mortality rate, surgical cost, and the incidence of urinary retention after surgery have been reported to be higher than open abdominal inguinal herniorrhaphy [11,12,20,21].
Recently, with the increased interests on the esthetic aspect and the improvement of minimal invasive surgery, in 1998, appendectomy [22] and cholecystectomy [23] were performed by single-incision laparoscopic surgery. Afterward, single-incision laparoscopic inguinal herniorrhaphy has been performed from 2009 [7-9]. As the biggest advantage of single-incision laparoscopic inguinal herniorrhaphy, excellent esthetic effects due to single incision could be pointed out. Nonetheless, prolonged operation time [7], the possibility of hernia through the incision area that reaches 25 to 45 mm [8,9], and the difficulty of the traction and dissection of tissues because of the crowding phenomenon and collision of surgical instruments due to small surgical spaces [9] have been pointed out to be problems.
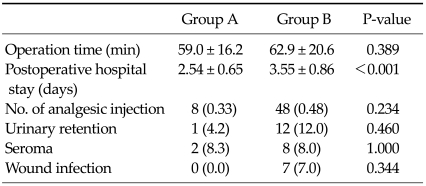
In our study, laparoscopic TEP inguinal herniorrhaphy without suprapubic port was performed. The advantages of our procedure were the advantages that have been pointed out to be the advantages of single-incision herniorrhaphy: the impediment of the mesh placement caused by suprapubic trocars could be prevented [8], the risk for hernia is small since the size of incision in the umbilical area is identical to conventional laparoscopic TEP, and it is performed after securing sufficient operation spaces without the crowding phenomenon and collision of surgical instruments similar to conventional laparoscopic TEP herniorrhaphy (Fig. 2). Thus, the actual operation time was 59.0 minutes, and it was not different from 62.9 minutes of conventional laparoscopic TEP herniorrhaphy, and it showed a trend that it was rather shortened. It was considered to be due to that the surgical procedure without using suprapubic port was performed after learning conventional surgical techniques and thus surgical skills were acquired, and since 5 mm 30° laparoscopes were used, the instruments could be used efficiently even in small spaces. In regard to the 5mm 0° laparoscopes (Olympus) used in the initial period of laparoscopic TEP herniorrhaphy without using suprapubic port, in a small surgical space, the crowding phenomenon and collision of surgical instruments were severe, and even in cases used 5 mm flexible 30° laparoscopes (Visera, Olympus), due to the collision of surgical instruments because of the limitation of flexion in a small surgery space and the limitation of surgical view, the operation time was prolonged to 70 minutes and 90 minutes, respectively. Nevertheless, after the use of 5 mm 30° laparoscopes, the site without the collision of surgical instruments was found, and operation time could be shortened. When photographs of laparoscopic view of herniorrhaphy actually performed at our hospital were compared (Fig. 2), it was determined that except the resolution of conventional TEP herniorrhaphy cases used 10 mm 30° laparoscopes was slightly different from cases used 5 mm 30° laparoscopes, it was almost similar. It thus is thought that surgeons who could perform conventional laparoscopic TEP surgery are able to perform laparoscopic TEP surgery without suprapubic port sufficiently.
Fig. 2.
Intraoperative appearance in totally extraperitoneal approach with (A) vs. without (B) suprapubic port.
Urinary retention is a common complication that could be developed immediately after herniorrhaphy, and the incidence has been reported to be 3 to 25% [24,25]. The incidence of urinary retention that is developed after laparoscopic TEP herniorrhaphy varies depending on investigators, nonetheless, it has been reported to be from 1.6 [26] to 6.3% [27]. The factors that are associated with the development are reported to be the combination of age, dissection of pelvic tissues, postsurgical pain, the use of opioid analgesics, and the bladder expansion due to excessive fluid supply [27,28]. The incidence of urinary retention after conventional laparoscopic TEP herniorrhaphy performed by us was 12.0%, and it was higher than the previous reports from 1.6 [26] to 6.3% [27]. Kulaçoğlu et al. [29] have reported that the ratio of urinary retention after laparoscopic cholecystectomy which required the installation of catheters was 0.9%, which was substantially lower than the incidence after laparoscopic TEP procedure. Therefore, we considered that the rate of urinary retention became lower when trocars were inserted to the area away from the bladder as much as possible and thus the dissection of pelvic tissues, particularly, tissues in the vicinity of the bladder was less required, which became the chance to start this study, and actually, the results that in laparoscopic TEP surgery without suprapubic port, the ratio of urinary retention was lowered to 4.2% were obtained. Although the results were not obtained from lone-term prospective random controlled experiments, it was considered that in the two surgical procedures of which other conditions were almost identical, the number of trocars was reduced, which may exert effects on the reduction of urinearyretention. In addition, among the complex factors of several factors of the development of urinary retention after laparoscopic herniorrhaphy, as significant factors, Koch et al. [28] have suggested the volume of fluid supply after surgery and the use of opioid analgesics. In other words, if postsurgical pain and the use of analgesic could be reduced, the possibility of reducing urinary retention developed after surgery is high. In our study similarly, although it was not statistically significant, the number of the administration of analgesics was shown to be small in herniorrhaphy without suprapubic port and thus postsurgical pain was reduced, and the rate of urinary retention was also low. In addition, Koch et al. [28] have reported that urinary retention is one of causes that prolong the hospitalization period. In our study, similarly, postsurgical urinary retention was not statistically significantly. Nonetheless, in the Group A that showed lower urinary retention, the hospitalization was 2.5 days, and it was shorter than 3.5 days of the Group B. Based on such results, although it was not statistically significant, it was confirmed that TEP herniorrhaphy without suprapubic port was less invasive.
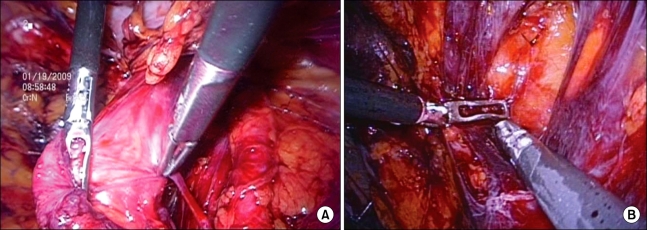
The reasons of the common application of laparoscopic herniorrhaphy are several, however, the biggest reasons are that pain is less severe due to minimal invasive surgery and esthetic effects are excellent [30]. In our study, laparoscopic extraperitoneal herniorrhaphy without suprapubic port does not require to shave pubic hairs that may cause embarrassment of patients prior to surgery, and on accounts of Korean characteristics, the advantage that allows to use public baths immediately after surgery, the satisfaction level of patients prior to and after surgery was higher (Fig. 3).
Fig. 3.
Postoperative appearance in totally extraperitoneal approach without suprapubic port.
In our study, bladder perforation was 1 case, and it occurred in the initial period of TEP surgery during the dissection procedure of hernia sac while performing surgery on a rare hernia case that a portion of bladder was included in the hernia sac. It was observed that among postsurgical complications, retention of body fluid, wound infection, etc. were identical without differences, and recurrence was not detected in the two groups during the average 23 months follow-up observation period. Although the follow-up observation period was short, it was found that the rate of chronic pain of the two groups was not different.
In conclusion, the authors performed laparoscopic extraperitoneal herniorrhaphy without suprapubic port was performed on 24 patients. In regard to postsurgical complications and recurrence, in the future, long-term prospective random controlled experiments on more subjects are required. Nonetheless, it is considered that the new herniorrhaphy is not different in comparison with conventional TEP herniorrhaphy, and although it was not statistically significant, it is considered to be a surgical procedure with the advantages in postsurgical pain, urinary retention, the hospitalization period after surgery, and the level of satisfaction with surgery.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Bassini E. Nuovo metodo per la cura radicale dell'ernia inguinale. Atti Congr Assoc Med Ital. 1887;2:179. [Google Scholar]
- 2.Kumar S, Wilson RG, Nixon SJ, Macintyre IM. Chronic pain after laparoscopic and open mesh repair of groin hernia. Br J Surg. 2002;89:1476–1479. doi: 10.1046/j.1365-2168.2002.02260.x. [DOI] [PubMed] [Google Scholar]
- 3.Memon MA, Cooper NJ, Memon B, Memon MI, Abrams KR. Meta-analysis of randomized clinical trials comparing open and laparoscopic inguinal hernia repair. Br J Surg. 2003;90:1479–1492. doi: 10.1002/bjs.4301. [DOI] [PubMed] [Google Scholar]
- 4.Heikkinen TJ, Haukipuro K, Koivukangas P, Hulkko A. A prospective randomized outcome and cost comparison of totally extraperitoneal endoscopic hernioplasty versus Lichtenstein hernia operation among employed patients. Surg Laparosc Endosc. 1998;8:338–344. [PubMed] [Google Scholar]
- 5.Liem MS, van der Graaf Y, van Steensel CJ, Boelhouwer RU, Clevers GJ, Meijer WS, et al. Comparison of conventional anterior surgery and laparoscopic surgery for inguinal-hernia repair. N Engl J Med. 1997;336:1541–1547. doi: 10.1056/NEJM199705293362201. [DOI] [PubMed] [Google Scholar]
- 6.Johansson B, Hallerbäck B, Glise H, Anesten B, Smedberg S, Román J. Laparoscopic mesh versus open preperitoneal mesh versus conventional technique for inguinal hernia repair: a randomized multicenter trial (SCUR Hernia Repair Study) Ann Surg. 1999;230:225–231. doi: 10.1097/00000658-199908000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Surgit O. Single-incision laparoscopic surgery for total extraperitoneal repair of inguinal hernias in 23 patients. Surg Laparosc Endosc Percutan Tech. 2010;20:114–118. doi: 10.1097/SLE.0b013e3181d848c3. [DOI] [PubMed] [Google Scholar]
- 8.He K, Chen H, Ding R, Hua R, Yao Q. Single incision laparoscopic totally extraperitoneal inguinal hernia repair. Hernia. 2010 May 14; doi: 10.1007/s10029-010-0674-z. [Epub]. DOI: 10.1007/s10029-010-0674-z. [DOI] [PubMed] [Google Scholar]
- 9.Agrawal S, Shaw A, Soon Y. Single-port laparoscopic totally extraperitoneal inguinal hernia repair with the TriPort system: initial experience. Surg Endosc. 2010;24:952–956. doi: 10.1007/s00464-009-0663-4. [DOI] [PubMed] [Google Scholar]
- 10.Koch CA, Grinberg GG, Farley DR. Incidence and risk factors for urinary retention after endoscopic hernia repair. Am J Surg. 2006;191:381–385. doi: 10.1016/j.amjsurg.2005.10.042. [DOI] [PubMed] [Google Scholar]
- 11.Winslow ER, Quasebarth M, Brunt LM. Perioperative outcomes and complications of open vs laparoscopic extraperitoneal inguinal hernia repair in a mature surgical practice. Surg Endosc. 2004;18:221–227. doi: 10.1007/s00464-003-8934-y. [DOI] [PubMed] [Google Scholar]
- 12.Classification of chronic pain. Descriptions of chronic painsyndromes and definitions of pain terms. Prepared by the International Association for the Study of Pain, Subcommittee on Taxonomy. Pain Suppl. 1986;3:S1–S226. [PubMed] [Google Scholar]
- 13.Nyhus LM, Codon RE. Hernia. 4th ed. Philadelphia: JB Lippincott; 1995. pp. 3–199. [Google Scholar]
- 14.Lichtenstein IL, Shore JM. Simplified repair of femoral and recurrent inguinal hernias by a "plug" technic. Am J Surg. 1974;128:439–444. doi: 10.1016/0002-9610(74)90189-5. [DOI] [PubMed] [Google Scholar]
- 15.Ger R, Mishrick A, Hurwitz J, Romero C, Oddsen R. Management of groin hernias by laparoscopy. World J Surg. 1993;17:46–50. doi: 10.1007/BF01655704. [DOI] [PubMed] [Google Scholar]
- 16.Hawasli A. Laparoscopic inguinal herniorrhaphy: the mushroom plug repair. Surg Laparosc Endosc. 1992;2:111–116. [PubMed] [Google Scholar]
- 17.Arregui ME, Davis CJ, Yucel O, Nagan RF. Laparoscopic mesh repair of inguinal hernia using a preperitoneal approach: a preliminary report. Surg Laparosc Endosc. 1992;2:53–58. [PubMed] [Google Scholar]
- 18.McKernan JB, Laws HL. Laparoscopic repair of inguinal hernias using a totally extraperitoneal prosthetic approach. Surg Endosc. 1993;7:26–28. doi: 10.1007/BF00591232. [DOI] [PubMed] [Google Scholar]
- 19.Youn SI, Kim BG, Cha SJ, Chang IT. The comparative analysis between laparoscopic inguinal herniorrhaphy and open inguinal herniorrhaphy. J Korean Surg Soc. 2005;69:166–171. [Google Scholar]
- 20.EU Hernia Trialists Collaboration. Laparoscopic compared with open methods of groin hernia repair: systematic review of randomized controlled trials. Br J Surg. 2000;87:860–867. doi: 10.1046/j.1365-2168.2000.01540.x. [DOI] [PubMed] [Google Scholar]
- 21.Juul P, Christensen K. Randomized clinical trial of laparoscopic versus open inguinal hernia repair. Br J Surg. 1999;86:316–319. doi: 10.1046/j.1365-2168.1999.01053.x. [DOI] [PubMed] [Google Scholar]
- 22.Esposito C. One-trocar appendectomy in pediatric surgery. Surg Endosc. 1998;12:177–178. doi: 10.1007/s004649900624. [DOI] [PubMed] [Google Scholar]
- 23.Piskun G, Rajpal S. Transumbilical laparoscopic cholecystectomy utilizes no incisions outside the umbilicus. J Laparoendosc Adv Surg Tech A. 1999;9:361–364. doi: 10.1089/lap.1999.9.361. [DOI] [PubMed] [Google Scholar]
- 24.Bailey HR, Ferguson JA. Prevention of urinary retention by fluid restriction following anorectal operations. Dis Colon Rectum. 1976;19:250–252. doi: 10.1007/BF02590913. [DOI] [PubMed] [Google Scholar]
- 25.Beadnell SW, Connaughton B, Farhood VW. Management of postoperative urinary retention. J Oral Maxillofac Surg. 1989;47:1307–1310. doi: 10.1016/0278-2391(89)90730-1. [DOI] [PubMed] [Google Scholar]
- 26.Ferzli G, Sayad P, Huie F, Hallak A, Usal H. Endoscopic extraperitoneal herniorrhaphy. A 5-year experience. Surg Endosc. 1998;12:1311–1313. doi: 10.1007/s004649900847. [DOI] [PubMed] [Google Scholar]
- 27.Vidović D, Kirac I, Glavan E, Filipović-Cugura J, Ledinsky M, Bekavac-Beslin M. Laparoscopic totally extraperitoneal hernia repair versus open Lichtenstein hernia repair: results and complications. J Laparoendosc Adv Surg Tech A. 2007;17:585–590. doi: 10.1089/lap.2006.0186. [DOI] [PubMed] [Google Scholar]
- 28.Koch CA, Grinberg GG, Farley DR. Incidence and risk factors for urinary retention after endoscopic hernia repair. Am J Surg. 2006;191:381–385. doi: 10.1016/j.amjsurg.2005.10.042. [DOI] [PubMed] [Google Scholar]
- 29.Kulaçoğlu H, Dener C, Kama NA. Urinary retention after elective cholecystectomy. Am J Surg. 2001;182:226–229. doi: 10.1016/s0002-9610(01)00703-6. [DOI] [PubMed] [Google Scholar]
- 30.Han MS, Lee SM, Choi SI, Joo SH, Hong SW. Comparison of laparoscopic totally extraperitoneal inguinal hernia repair and tension-free herniorrhaphy using perfix (R): short-term follow-up results. J Korean Surg Soc. 2009;77:189–194. [Google Scholar]