Abstract
Hemophagocytic lymphohistiocytosis (HLH) is a syndrome of pathologic immune activation, occurring as either a familial disorder or a sporadic condition, in association with a variety of triggers. This immune dysregulatory disorder is prominently associated with cytopenias and a unique combination of clinical signs and symptoms of extreme inflammation. Prompt initiation of immunochemotherapy is essential for survival, but timely diagnosis may be challenging because of the rarity of HLH, its variable presentation, and the time required to perform diagnostic testing. Therapy is complicated by dynamic clinical course, high risk of treatment-related morbidity, and disease recurrence. Here, we review the clinical manifestations and patterns of HLH and describe our approach to the diagnosis and therapy for this elusive and potentially lethal condition.
Introduction
Hemophagocytic lymphohistiocytosis (HLH) is a syndrome of pathologic immune activation characterized by clinical signs and symptoms of extreme inflammation. It was first recognized as a familial immune dysregulatory disorder of childhood, called “familial hemophagocytic reticulosis” in 1952.1 Later, HLH was described as both a familial disorder and as a sporadic one, in association with infections, malignancies, or rheumatologic disorders. The immunologic basis of HLH was suspected because of its inflammatory nature and the finding of cytotoxic deficiencies and other immune abnormalities in patients with HLH.2 The first genetic insight into the etiology of HLH came in 1999 with the discovery of perforin mutations in some affected patients.3 Subsequent animal studies demonstrated that cytotoxic deficiency leads to abnormal T-cell activation and inflammatory cytokine production, which drive disease development.4 Recent work with whole genome expression analyses suggests paradoxical down-regulation of various aspects of the immune response, including B-cell development and function, Toll-like receptor expression and signaling, and apoptosis induction.5,6
Diagnosing HLH
Despite increasing insights into its genetic and immunologic basis, HLH remains a syndromic disorder, defined and diagnosed by a unique pattern of clinical findings. Although the individual signs or symptoms of HLH may occur in a variety of clinical circumstances, the combination of these features, caused by pathologic inflammation, forms the pattern of HLH. Although disease-associated genetic defects are a part of common diagnostic criteria, genetic testing is most useful to confirm a clinical diagnosis, predict the risk of future recurrence in affected patients, and define HLH predisposition in asymptom-atic family members. As part of the HLH-94 clinical trial, the Histiocyte Society proposed a standard definition of HLH in 1994. The definition was later revised for the HLH-2004 trial and serves as a current de facto definition of HLH. These criteria are listed in Table 1 with some minor modifications.7
Table 1.
Diagnostic criteria for HLH used in the HLH-2004 trial*
| The diagnosis of HLH† may be established: |
|---|
| A. Molecular diagnosis consistent with HLH: pathologic mutations of PRF1, UNC13D, Munc18-2, Rab27a, STX11, SH2D1A, or BIRC4 |
| or |
| B. Five of the 8 criteria listed below are fulfilled: |
| 1. Fever ≥ 38.5°C |
| 2. Splenomegaly |
| 3. Cytopenias (affecting at least 2 of 3 lineages in the peripheral blood) |
| Hemoglobin < 9 g/dL (in infants < 4 weeks: hemoglobin < 10 g/dL) |
| Platelets < 100 × 103/mL |
| Neutrophils < 1 × 103/mL |
| 4. Hypertriglyceridemia (fasting, > 265 mg/dL) and/or hypofibrinogenemia (< 150 mg/dL) |
| 5. Hemophagocytosis in bone marrow, spleen, lymph nodes, or liver |
| 6. Low or absent NK-cell activity |
| 7. Ferritin > 500 ng/mL‡ |
| 8. Elevated sCD25 (α-chain of sIL-2 receptor)§ |
Adapted from Henter et al.7
In addition, in the case of familial HLH, no evidence of malignancy should be apparent.
Although the HLH-2004 protocol uses ferritin > 500 ng/mL, we generally view ferritin > 3000 ng/mL as concerning for HLH and ferritin > 10 000 as highly suspicious.8
Elevations above age-adjusted, laboratory-specific normal levels (defined as > 2 SD from the mean) appear more meaningful than the original designation of > 2400 U/mL because of variations between laboratories.17
Diagnosing HLH is the first critical step toward successful therapy but is challenging because of the rare occurrence, variable presentation, and nonspecific findings of this disorder. Based on the incidence of HLH at our institutions, we estimate that tertiary care pediatric hospitals should expect 1 case of HLH per 3000 inpatient admissions.8 Practical considerations for diagnosis include prompt assessment and recognition of the signs of HLH, especially in critically ill patients. Special studies, such as NK cell function and soluble CD25 (sCD25, also known as the α-chain of the IL-2 receptor) levels, should be ordered early because of the time required to obtain these results from specialty laboratories. In our experience, sCD25 is one of the most useful inflammatory markers, as it correlates with current disease activity more consistently than ferritin or other disease indices. However, ferritin may also be a valuable marker because levels > 10 000 g/dL were highly sensitive and specific for the diagnosis of HLH in an institutional series8 and sCD25 assays are not readily available at all institutions. Because not all patients have hemophagocytosis at disease onset, diagnosis should not be delayed looking for this single feature. Furthermore, as hemophagocytosis is neither sensitive nor specific for HLH, we consider this one of the less important diagnostic criteria.9 Whereas familial HLH commonly presents in young children, there are reports of adults as old as 62 years with proven molecular defects in perforin and other HLH-associated genes.10,11 The same diagnostic and therapeutic approach may apply to both children and adults, although special caution should be used in treating adults as they may experience significant comorbidity, especially related to high-dose steroid therapy.
Understanding the patterns of HLH
Diagnostic criteria for HLH (Table 1) were originally derived by retrospective analysis of patients categorized and treated for HLH decades ago, and updated by the Histiocyte Society after analysis of patients enrolled on the HLH-94 study.7 Although intended for the conduct of clinical trials, these diagnostic criteria have been widely used for diagnosing and treating patients regardless of whether they are enrolled on these trials. It should be noted, however, that these diagnostic criteria do not reflect all of the typical clinical or laboratory features of patients with HLH, many of which are helpful in making the diagnosis. For instance, in our experience, patients with HLH almost always have evidence of liver inflammation, which may range from very mild elevations of transaminases to fulminant liver failure. Thus, unexplained liver failure with concurrent cytopenias and elevated inflammatory indices should suggest HLH, whereas a diagnosis of HLH with normal liver indices should be considered unusual. In addition, neurologic findings are not part of current diagnostic criteria, even though they are relatively common and a distinctive clinical feature in many patients with HLH. Finally, for practical reasons, the HLH-2004 diagnostic criteria do not include all available molecular studies relevant to familial HLH pathogenesis. However, the results of newer clinical laboratory studies evaluating expression of HLH-associated proteins (perforin, SLAM-associated protein, or X-linked inhibitor of apoptosis protein) or measurement of surface CD107a exposure (indicative of genetic abnormalities affecting degranulation)12are now available with results rapid enough to assist in identifying immunologic defects and diagnosing HLH.
In our experience, the diagnosis of HLH is often delayed, to the detriment of patients. This delay is the result of a variety of factors, including the rarity of HLH, the complexity of diagnostic criteria, and concern regarding the specificity of current diagnostic criteria. Although there is no substitute for maintaining a high index of suspicion in appropriate patients, we think that a better understanding of the clinical patterns of HLH and how they appear to relate to the underlying pathophysiology would lead to more prompt and accurate diagnoses. Based on current understanding of HLH pathogenesis, we have categorized the diagnostic, typical, and unique features of patients with HLH in Table 2.
Table 2.
A pathophysiologic view of HLH patterns
| Category 1: predisposing immunodeficiency | Category 2: significant immune activation | Category 3: abnormal immunopathology |
|---|---|---|
| Low or absent NK-cell function* | Fever* | Cytopenias* |
| Genetic defect of cytotoxicity* | Splenomegaly*/hepatomegaly | Decreased fibrinogen or increased triglycerides* |
| Family history of HLH | Elevated ferritin* (> 3000 ng/mL) | Hemophagocytosis* |
| Prior episode(s) of HLH or unexplained cytopenias | Elevated sCD25* | Hepatitis |
| Markers of impaired cytotoxicity: decreased expression of perforin, SAP, XIAP, or mobilization of CD107a | Elevated sCD16393 | CNS involvement |
SAP indicates SLAM-associated protein; and XIAP, X-linked inhibitor of apoptosis protein.
The HLH-2004 diagnostic criteria.
As Table 2 indicates, some features of HLH are indicative of a predisposing immune deficiency, whereas others indicate the presence of significant immune activation or the development of abnormal immune-mediated pathologies (when the immune reaction itself causes tissue damage). Categorizing the relevant and diagnostic features of HLH in this way has several valuable implications. First, these categories reflect the current understanding of causality and sequence in HLH. Experimental studies indicate that normal cytotoxic function limits immune activation and thereby mitigates the development of severe immunopathology.4,13 This understanding of causality emphasizes the importance of underlying immune activation (category 2) for HLH to develop. This sequence also reflects the common clinical observation that hemophagocytosis may not be found in initial biopsies and yet may linger in later biopsies, even when other disease parameters appear to be improving. Second, these categories reflect the uniqueness of HLH as a syndrome. We have divided most of the acute features of HLH as either indicating immune activation or immune-mediated pathology because this reflects the essence of this disease process. Although patients with a variety of inflammatory conditions display immune activation, normal cytotoxic immune regulatory mechanisms tend to dampen immune activation before unusual or paradoxical immunopathology (category 3) develops. The combination of acute systemic immune activation and the specific findings listed in category 3 is largely what distinguishes HLH from other inflammatory disorders. Organ-specific infectious or autoimmune processes (such as hepatitis, meningitis, or aplastic anemia) do not tend to display the systemic inflammatory and/or multiorgan features of HLH. Systemic inflammatory processes (such as sepsis) do not tend to display the specific constellation of immunopathologies and/or evidence of T-cell activation, as seen in HLH.14 Furthermore, whereas rising neutrophil counts, platelet counts, and fibrinogen levels may all be viewed as evidence of acute inflammation, the paradoxical fall seen in HLH is better characterized as an unusual immunopathology or consequence of immune activation. In line with this schema of immune activation and immune-mediated pathology, we think that robust findings in both category 2 and category 3 should be essential for the diagnosis of HLH. Third, because this schema illustrates that inflammation is primary to most clinical manifestations of HLH, it reiterates the importance of monitoring inflammatory markers, such as sCD25 or ferritin, for assessing response to therapy. We find that these markers often rise before clinically apparent worsening of HLH. We favor redefining the formula for diagnosis of HLH (eg, a certain number of features in categories 2 and 3, with or without features in category 1) to facilitate prompt and accurate diagnosis, although formal redefinition of the diagnostic criteria for HLH will require further experimental validation and international consensus.
Variations in the HLH pattern
Primary versus secondary
HLH presents in a variety of clinical contexts and with a variety of etiologic associations. Patients are often categorized as having either “primary” or “secondary” HLH. Patients in the “primary HLH” category are those with clear familial inheritance or genetic causes, are usually infants or younger children, and are thought to have fixed defects of cytotoxic function (although this is not always the case). Such persons have a clear risk of HLH recurrence and are not likely to survive long-term without hematopoietic cell transplantation (HCT). Although HLH in these patients can be associated with infections (such as CMV or EBV) or vaccination, the immunologic trigger is often not apparent.
The term “secondary HLH” generally refers to older children (or adults) who present without a family history or known genetic cause for their HLH. These patients typically have concurrent infections/medical conditions that appear to trigger their HLH, such as EBV infection, malignancy, or rheumatologic disorders. The list of triggering stimuli for both familial and apparently nonfamilial HLH is extensive.15,16 Patients with presumed secondary HLH are sometimes reported as having immune studies, which normalize with disease resolution, although in our experience this is variable or unclear. Although mortality from HLH may be significant, the risk of recurrence in cases of secondary HLH is poorly defined. Recurrence of HLH, in the absence of autoimmune disease or malignancy, is generally considered to be good evidence that a patient has primary HLH. However, in our experience, categorizing patients as having either “primary” or “secondary” HLH at diagnosis is of limited value. Without a known genetic defect or family history, it is often not possible to make an initial diagnosis of “primary” or “secondary” HLH. Furthermore, a careful search for underlying disease triggers should be performed in all patients. Thus, initial treatment should not be delayed or altered based on these categories.
MAS
Macrophage activation syndrome (MAS) has long been recognized by the rheumatology community as the major, potentially lethal complication of systemic onset juvenile idiopathic arthritis. MAS is also associated with other autoimmune conditions, including systemic lupus erythematosus, and should be thought of as HLH associated with rheumatic diseases. The main manifestations include fever, hepatosplenomegaly, hepatitis, lymphadenopathy, and disseminated intravascular coagulation. Cytopenias are a late finding, as patients with systemic onset juvenile idiopathic arthritis typically exhibit elevated blood counts during active disease, including neutrophilia and thrombocytosis. In the context of rheumatologic disorders, hemophagocytosis in the bone marrow or other tissues is an important finding. MAS may be the first manifestation of systemic onset juvenile idiopathic arthritis, leaving it difficult to distinguish on a symptomatic basis from HLH. In patients with a diagnosis of systemic onset juvenile idiopathic arthritis, infections, flares of the underlying disease process, or changes in medication may trigger MAS.17,18 MAS also bears close immunologic and genetic resemblance to HLH. A majority of patients with MAS have depressed NK function, depressed expression of perforin, and elevated sCD25 and sCD163.19 Polymorphisms or heterozygous mutations in PRF1 or UNC13D have been identified in a significant proportion of MAS patients. Comparison of gene microarrays between patients with MAS and HLH indicates a unique early erythroid signature that may reflect the consumptive anemia observed in both conditions.5
In patients with MAS diagnosed in the context of rheumatologic disease, treatment with increased immunosuppression and high-dose intravenous immunoglobulin are often effective. More recently biologic agents directed against inflammatory cytokines IL-1 and IL-6 have been shown to be helpful in some patients.20 If patients clinically deteriorate with laboratory findings of worsening inflammation despite steroids, cyclosporine, or other disease-specific therapy, it is sometimes necessary to escalate treatment to include etoposide, other HLH salvage therapy, or HCT.
HLH and malignancy
HLH has been reported primarily with lymphomas or leukemias of the T or NK cell lineages, but associations with anaplastic large cell lymphoma, early B lineage lymphoblastic leukemia, myeloid leukemias, mediastinal germ cell tumors, and rarely other solid tumors are also found. Many of these patients simultaneously have a bacterial, viral, or fungal infection that may serve as a trigger for the HLH in the context of a dysfunctional immune system that has occurred because of chemotherapy for the malignancy or perhaps cytokine production by the malignant cells. CTs of the chest and abdomen, as well as the bone marrow aspirate and biopsy, at the time of presentation are helpful to evaluate possible underlying malignancy. O'Brien et al reported a series and reviewed the literature of children with HLH and leukemia.21 Only one of 11 T-cell leukemia/HLH patients lived as opposed to 5 of 9 B-cell leukemia/HLH patients. All but 2 of the latter also had a simultaneous infection. The majority of published cases of HLH and T- or B-cell lymphoblastic leukemia in pediatric patients occurred after the diagnosis of acute lymphoblastic leukemia. Another series of 6 patients with malignancy were reported, including 2 cases of acute lymphoblastic leukemia, 2 acute myeloid leukemia, 1 recurrent medulloblastoma, and 1 Ewing sarcoma.22 Two of these patients had received allogeneic stem cell transplants. Other cases of HLH after stem cell transplant have been reported with a fludarabine-based reduced intensity conditioning regimen.23,24 Peripheral T-cell lymphomas and HLH with or without EBV infection have also been reported.25,26 Rearrangements of T-cell receptor genes and large atypical cells are found along with prominent hemophagocytosis by benign-appearing histiocytes. A case of hepatosplenic γδ T-cell lymphoma was reported to respond well to therapy with etoposide and dexamethasone.27 The simultaneous presentation of aggressive NK cell leukemia/lymphoma or anaplastic large cell lymphomas has been reported by several groups.28–32 Two patients who died with mediastinal germ cell tumors and HLH have also been reported.33,34 Based on our own experiences as well as the case reports and case series described in this section, in patients with HLH driven by malignancy, we recommend initiating immunochemotherapy aimed at controlling inflammation first and then transition to disease-specific therapy once inflammatory markers normalize.
EBV and HLH
EBV is the most frequent infection associated with HLH. EBV-associated HLH varies widely from inflammation that resolves spontaneously to unrelenting disease requiring HCT. EBV infection may trigger HLH in patients with any form of familial disease, and patients with X-linked lymphoproliferative disease (XLP) are at particularly high risk.35–37 EBV-HLH has been associated with acute infections not only in B cells, but also in T cells and NK cells.36,38–41 Survival is improved if etoposide–containing therapy is initiated promptly on diagnosis.42 Serial quantitative PCR of EBV DNA in T/NK as well as B-cell subsets may be helpful to distinguish self-limiting infectious mononucleosis from progressive HLH or other EBV-related lymphoproliferative disorders.41,43 Because it can eliminate EBV-infected B cells, rituximab may be a beneficial addition to other therapies in patients with progressive EBV-HLH.44 Of note, some patients with apparently self-resolving HLH after primary EBV infection later develop aggressive recurrent HLH requiring immunochemotherapy and HCT, including patients without identified mutations in XLP genes.
Many genotypes, one phenotype
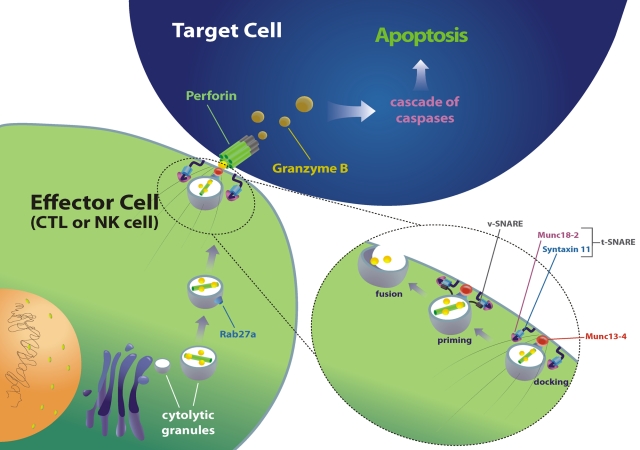
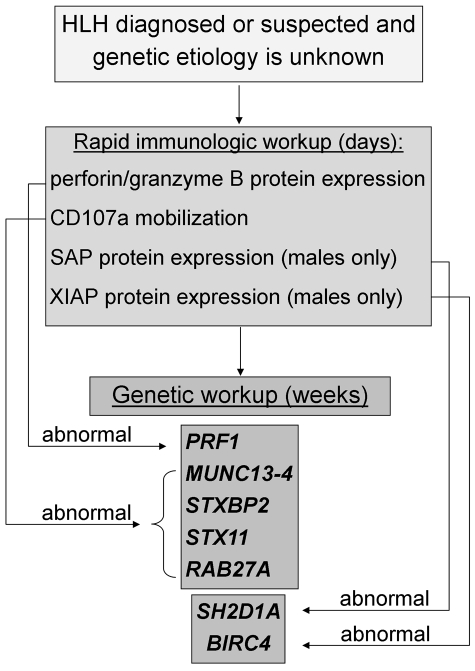
A variety of distinct genetic syndromes are associated with HLH. Although the gene defects underlying these syndromes (Table 3) are distinct, they all lead to the common phenotype of impaired cytotoxic function by NK and T cells, and a predisposition to develop HLH (Figure 1). Patients with more severe defects of cytotoxic function, as assessed by in vitro assays, tend to have earlier onset of disease and a more severe clinical course.45 Notably, the link between broad cytotoxic dysfunction and HLH is less clear for XLP1 and XLP2.35 Results of genetic testing for HLH in North America are displayed in Tables 4 and 5. Although there may be some referral bias because of the sequence of gene analysis studies and not all studies were performed on every patient, these data demonstrate the relative frequency of gene mutations and age or ethnic identity in North America. The frequency of specific genetic abnormalities may vary considerably by ethnic or national identity.46–48 An approach to evaluation of immune function and HLH-associated gene defects is described in Figure 2.
Table 3.
HLH-associated gene mutations
| Gene | Location | Disease |
|---|---|---|
| PRF1 | 10q21-22 | FHL2 |
| UNC13D | 17q25 | FHL3 |
| STX11 | 6q24 | FHL4 |
| RAB27A | 15q21 | Griscelli syndrome |
| STXBP2 | 19p13 | FHL5 |
| Unknown | 9q21.3-22 | FHL1 |
| SH2D1A | Xq24-26 | XLP1 |
| XIAP | Xq25 | XLP2/X-linked HLH |
| LYST | 1q42.1-42.2 | Chediak-Higashi syndrome |
Figure 1.
Mechanics of cytotoxic function revealed by HLH-associated gene mutations. HLH-associated genetic abnormalities (in the indicated genes) may affect granule-dependent lymphocyte cytotoxicity by impairing trafficking, docking, priming for exocytosis, or membrane fusion of cytolytic granules. The function of this pathway may also be severely impaired by loss of functional perforin, the key delivery molecule for proapoptotic granzymes. Diverse mutations in this pathway all give rise to similar clinical phenotypes (albeit of variable severity). Lyst (the gene affected in Chediak-Higashi syndrome) is not portrayed because its function is not entirely clear, although it appears to play an important role in the maintenance of normally sized (and functional) cytolytic granules.
Table 4.
Frequency of HLH-associated gene mutations by age in North American patients
| Age at referral | No. of HLH patients | PRF1 | UNC13D | STXBP2 | STX11 | RAB27A | Mutation identified, % |
|---|---|---|---|---|---|---|---|
| < 1 mo | 58 | 16 | 5 | 0 | 0 | 0 | 45 |
| 2 mo to 1 y | 100 | 23 | 15 | 1 | 0 | 0 | 39 |
| 1-2 y | 55 | 7 | 4 | 0 | 0 | 0 | 20 |
| > 2 y | 263 | 7 | 3 | 2 | 2 | 1 | 6 |
Data from Judith Johnson and Kejian Zhang.
Table 5.
Distribution of HLH-associated gene mutations, by ethnicity, in North American patients with identified genetic abnormalities
| Gene | White | Hispanic | Black | Arabic | Other/unknown |
|---|---|---|---|---|---|
| PRF1 | 20 (27) | 41 (71) | 44 (98) | 8 (36) | 22 (88) |
| UNC13D | 35 (47) | 10 (17) | 0 (0) | 6 (27) | 1 (4) |
| STX11 | 1 (2) | 4 (7) | 0 (0) | 2 (9) | 0 (0) |
| RAB27A | 2 (3) | 2 (3) | 0 (0) | 2 (9) | 1 (4) |
| STXBP2 | 16 (22) | 1 (2) | 1 (2) | 4 (18) | 1 (4) |
| Total | 74 | 58 | 45 | 22 | 25 |
Data from Judith Johnson and Kejian Zhang. Values in parentheses represent the percentage of patients with identified mutations who have an abnormality in the indicated gene.
Figure 2.
Immunologic and genetic workup of HLH. Rapid immunologic testing (which may be performed in 1-3 days) may support a diagnosis of HLH and provide etiologic data, whereas gene sequencing (typically requiring 3-8 weeks) may define the underlying genetic cause. Measurement of NK cytotoxic function and sCD25 may also support the diagnosis of HLH but is not included in the diagram because abnormalities in these assays do not suggest specific genetic lesions. Of note, whereas an abnormal test suggests an underlying gene abnormality, a normal immunologic test does not preclude genetic testing. Genetic testing should be pursued until biallelic (or hemizygous) mutations are found or until all 5 genes (or 7, in the case of males) are assayed. LYST gene sequencing is not currently commercially available.
Additional clinical features of HLH
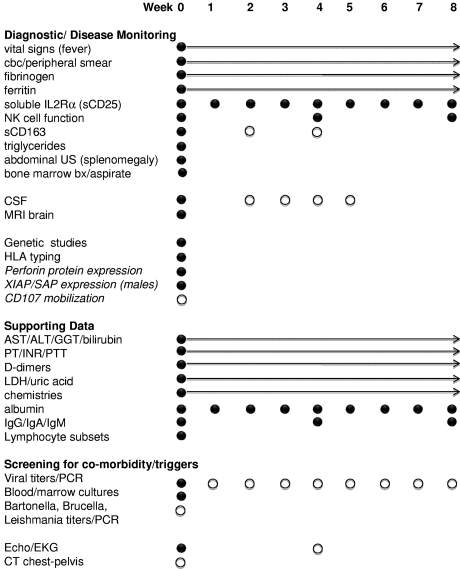
HLH is a syndrome that presents in many forms: fever of unknown origin (FUO), hepatitis/acute liver failure, sepsis-like, Kawasaki-like, and neurologic abnormalities. Not all of the HLH diagnostic criteria may be present initially, so it is important to follow clinical signs and laboratory markers of pathologic inflammation repeatedly to identify the trends. This section discusses common clinical findings in HLH patients. Our practices for initial evaluation are detailed in Figure 3.
Figure 3.
HLH diagnostic and induction surveillance strategy. A complete diagnostic evaluation, thorough search for underlying triggers (including infection or malignancy), and assessment of relevant immune studies are indicated in patients suspected to have HLH. In addition, ongoing reevaluation of inflammatory markers is essential to gauge the response to therapy. ● represents recommended studies; and ○, recommended studies with sufficient clinical suspicion. Arrows indicate recommendations for initial daily labs with decreasing frequency to one study per week as values normalize. Italicized studies are those that may facilitate diagnosis but are not directly part of current diagnostic criteria. CT or abdominal ultrasound may also facilitate diagnosis by documenting splenomegaly. sCD25 and sCD163 are useful markers of inflammation that may be more reliable measures of HLH disease activity than ferritin in some patients. CD107 mobilization may corroborate NK functional studies and quickly indicate a relevant degranulation defect. Careful monitoring of infection status is appropriate when persistent viral (or other infection) is found. Initial viral PCRs should assess EBV, CMV, adenovirus, and other relevant viruses. CSF studies are important to determine CNS involvement of HLH, although MRI may be substituted initially in coagulopathic patients. Pan-CT may be helpful in cases where there is concern for abscess or underlying malignancy. EKG/echocardiogram establish baseline organ function and screen for coronary artery vasculopathy in patients with overlapping symptoms of Kawasaki disease. We also recommend initiating HLA testing at the time of diagnosis to avoid delays in identifying donors for HCT.
Prolonged fever
FUO is a common diagnosis on general pediatric wards, and differentiating HLH from other causes of FUO may be challenging. In one series, patients ultimately diagnosed with HLH presented with fevers above 102° F (38.9°C) for a median of 19 days (range, 4-41 days).49 In patients with FUO, cytopenias, highly elevated ferritin (> 3000 g/dL), or sCD25 significantly above age-adjusted normal ranges, generally prompt us to pursue a complete HLH diagnostic evaluation.
Liver disease and coagulopathy
Most patients have variable evidence of hepatitis at presentation.49–51 HLH should be considered in the differential diagnosis of acute liver failure, especially if lymphocytic infiltrates are noted on biopsy. Autopsy evaluation of the liver has shown chronic persistent hepatitis with periportal lymphocytic infiltration in 22 of 27 patients with HLH.52 Neonates with HLH may present with hydrops fetalis and liver failure.53 Veno-occlusive disease may arise spontaneously in patients with HLH, and rates of veno-occlusive disease as high as 25% are reported after bone marrow transplantation.54 Nearly 95% of patients have features of disseminated intravascular coagulation and are at high risk for acute bleeding.49 Furthermore, patients with HLH resulting from degranulation defects may manifest platelet dysfunction.55
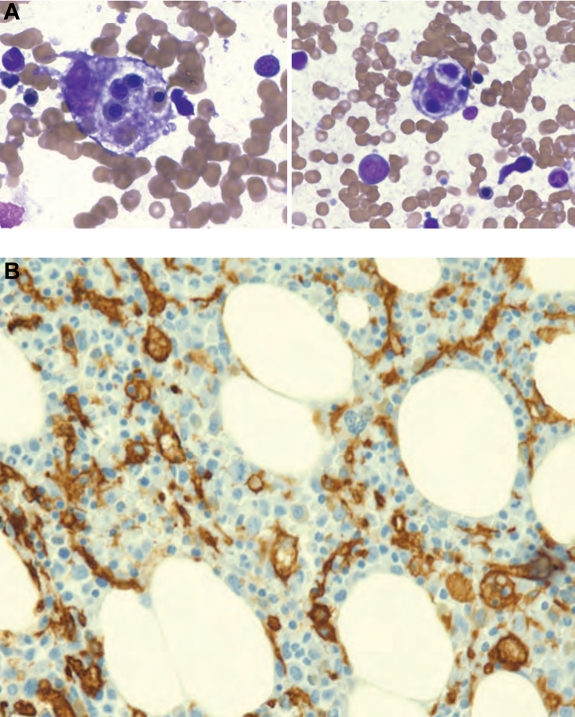
Bone marrow failure
Anemia and thrombocytopenia occur in > 80% of patients at the time of presentation with HLH.49,51 The cellularity of bone marrow aspirates varies from normocelluar to hypocellular or hypercellular. Prevalence of hemophagocytosis (examples in Figure 4) in association with HLH diagnosis ranges from 25%-100%, with ∼ 1-10 hemophagocytes per 500 cells in cases reported as positive.9 Although hemophagocytosis in bone marrow is associated with HLH, the morphologic phenomenon may also be induced by more common events, including blood transfusions, infection, autoimmune disease, and other forms of bone marrow failure or causes of red blood cell destruction.56–58 Despite the nomenclature of HLH, diagnosis should never be made or excluded solely on the presence or absence of hemophagocytosis. Infiltration of bone marrow or liver by activated macrophages, along with global clinical evaluation, may distinguish HLH from other causes of hemophagocytosis.
Figure 4.
Hemophagocytosis on bone marrow aspirate and biopsy. (A) Two examples of hemophagocytic macrophages identified on bone marrow aspiration (Wright-Giemsa stain). (B) CD163 staining of bone marrow biopsy section highlights hemophagocytosis (counterstained with hematoxylin). Images were taken on a Nikon Elipse microscope (panel A: 100×/10; panel B: 20×/10) without oil, with a Spot digital camera. Images are unmanipulated. Courtesy of Dr Jun Mo.
Skin manifestations
Patients may have a variety of skin manifestations, including generalized maculopapular erythematous rashes, generalized erythroderma, edema, panniculitis, morbilliform erythema, petechiae, and purpura.1,59 The incidence of skin manifestations ranges from 6%-65% in published series with highly pleomorphic presentations.50,60,61 Some patients may present with features suggestive of Kawasaki disease, including erythematous rashes, conjunctivitis, red lips, and enlarged cervical lymph nodes.62 Rashes may correlate with lymphocyte infiltration on skin biopsy, and hemophagocytosis may also be found.
Pulmonary dysfunction
Patients may develop pulmonary dysfunction that leads to urgent admission to the intensive care unit. In a review of the radiographic abnormalities in 25 patients, 17 had acute respiratory failure with alveolar or interstitial opacities, with fatal outcomes in 88% of those cases. Worsening pulmonary function is an ominous sign and should suggest inadequate control of HLH and/or infection.63
Brain, ophthalmic, and neuromuscular symptoms
More than one-third of patients will present with neurologic symptoms, including seizures, meningismus, decreased level of consciousness, cranial nerve palsy, psychomotor retardation, ataxia, irritability, or hypotonia.64 The cerebrospinal fluid (CSF) is abnormal in > 50% of HLH patients with findings of pleocytosis, elevated protein, and/or hemophagocytosis.64 MRI findings are variable, including discrete lesions, leptomeningeal enhancement, or global edema, and images correlate with neurologic symptoms.65 Retinal hemorrhages, swelling of the optic nerve, and infiltration of the choroid have been reported in infants with HLH.66–68 Diffuse peripheral neuropathy with pain and weakness secondary to myelin destruction by macrophages may also occur.69,70
Treating HLH
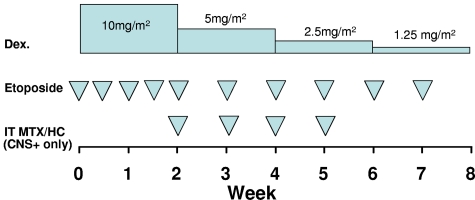
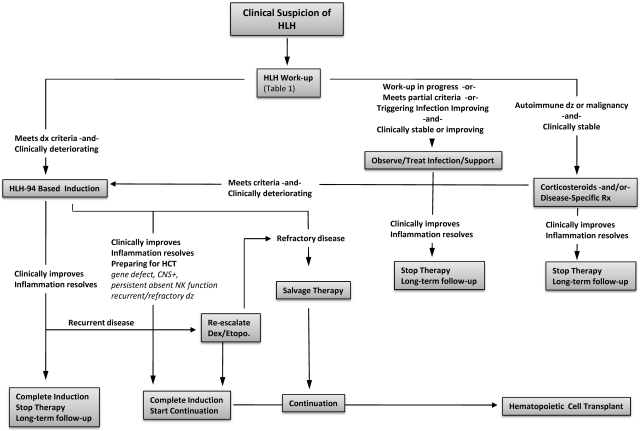
Without therapy, survival of patients with active familial HLH is ∼ 2 months.60,61 The first international treatment protocol for HLH was organized by the Histiocyte Society in 1994 and led to reported survival of 55%, with a median follow-up of 3.1 years.71 The HLH-94 protocol, as illustrated in Figure 5, included an 8-week induction therapy with dexamethasone, etoposide, and intrathecal methotrexate. The principal goal of induction therapy is to suppress the life-threatening inflammatory process that underlies HLH. At the end of 8 weeks, patients are either weaned off of therapy or transitioned to continuation therapy, which is intended only as a bridge to transplantation.
Figure 5.
Induction therapy for HLH. Based on the HLH-94 study, this approach should be considered standard of care for all patients not enrolled in clinical trials, based on published evidence of efficacy.71 Etoposide is dosed as 150 mg/m2 per dose. Alternatively, for patients weighing < 10 kg, consideration may be given to dosing etoposide as 5 mg/kg per dose. Dexamethasone (Dex.) is dosed as indicated and may be given orally or intravenously, although the latter is preferred at therapy initiation. Intrathecal methotrexate and hydrocortisone (IT MTX/HC) should be given to patients with evidence of CNS involvement, as early as LP may be safely performed (which may vary from the diagram) and dosed as follows: age < 1 year, 6/8 mg (MTX/HC); 1-2 years, 8/10 mg; 2-3 years, 10/12 mg; > 3 years, 12/15 mg. Weekly intrathecal therapy is generally continued until at least 1 week after resolution of CNS involvement (both clinical and CSF indices).
The Histiocyte Society opened a new trial in 2004, HLH-2004, which is currently enrolling patients. The major modifications from HLH-94 were to move cyclosporine dosing to the beginning of induction and add hydrocortisone to intrathecal therapy. An alternative approach to etoposide-based regimens, with comparable survival, was published as a single-center experience over 14 years in which all patients were treated with corticosteroids and antithymocyte globulin (ATG) followed (rapidly) by HCT.72 Until this immunotherapy approach can be compared with etoposide/dexamethasone in the setting of a clinical trial and until the results of the HLH-2004 study are published, our current practice is to treat patients who are not enrolled in a clinical study with a strategy based on HLH-94. Because the risks and benefits of adding cyclosporine to induction therapy are not yet defined, we do not use cyclosporine during induction, in patients who are not enrolled on HLH-2004.
Initial considerations
Often the principle challenge for treating patients with HLH is making a timely diagnosis. It is also critical to search for and treat underlying triggers of HLH, and institute specific antimicrobial therapy. Rituximab is often helpful in controlling EBV infection. Intravenous immunoglobulin is an appropriate adjunct for most viral infections. Although visceral leishmaniasis (which may closely resemble HLH) is not often seen in North America, it is readily treated and should be considered, especially in patients from endemic areas. In general, if the patient is stable and not severely ill, consideration can be given to treating the underlying trigger with disease-specific therapy with or without corticosteroids and close follow-up. However, in most cases, an aggressive therapeutic approach is warranted and may reasonably be initiated before obtaining final results for all diagnostic studies. Specifically, HLH therapy should not be withheld while awaiting results of genetic testing, as our understanding of HLH-associated gene defects remains incomplete. With the exception of autoimmune disease and malignancy, we do not differentiate initial therapy for patients with suspected familial or reactive HLH.
Many patients will be admitted to the ICU because of delay in diagnosis or complications of the disease. Although individual findings in HLH may mimic features of sepsis and multiorgan dysfunction, close follow-up is needed to define the diagnostic criteria for HLH. The degree of abnormality of inflammatory markers may help to distinguish these disorders. For example, in one study, the median ferritin was significantly higher in patients with HLH than in other inflammatory conditions, including shock and sepsis.8 Progressively increasing transaminases, bilirubin, coagulopathy, ferritin, and sCD25 levels as well as deteriorating respiratory status are poor prognostic signs.73
Induction therapy
The current standard of care consists of a decrescendo course of etoposide and dexamethasone, with or without intrathecal therapy (Figure 5). Ideally, critically ill patients should be treated at facilities familiar with care of cancer and bone marrow transplant patients. It is important to initiate therapy promptly, even in the face of unresolved infections, cytopenias, or organ dysfunction. Because etoposide is cleared by both renal and hepatic routes, we recommend dose reductions of 25% for creatinine clearance of 10-50 mL/minute, 50% for creatinine clearance of < 10 mL/minute, and 75% in case creatinine clearance is < 10 mL/minute and direct bilirubin is > 3 mg/dL.74,75 We do not dose reduce etoposide for isolated hyperbilirubinemia or neutropenia. HLA typing is sent at the start of induction therapy to avoid downstream delays in HCT.
After starting therapy, patients should be monitored closely for signs of improvement as well as potential complications and toxicities. An example strategy is outlined in Figure 6. Patients may follow a highly unpredictable and dynamic clinical course, which may require customization of therapy. For patients who respond well, with resolution of symptoms and normalization of inflammatory markers, therapy may be weaned per protocol. However, dexamethasone doses and etoposide frequency may need to be increased in response to disease reactivation (see “Salvage therapy”). Deterioration of liver function and blood counts as well as steady increases in serum ferritin, sCD25, and sCD163 tests may signal relapse of HLH disease activity.76 If patients do not display at least a partial response within 2-3 weeks of therapy initiation, salvage therapy should be considered. Recurrence of fever and increased inflammatory markers after an apparent response should also prompt a careful search for opportunistic infection.
Figure 6.
Treatment strategy for HLH. An algorithm for HLH treatment strategies in various clinical contexts.
CNS disease
Patients may present with CNS involvement or CNS inflammation may recur as treatment doses are being tapered. All patients should receive a careful neurologic examination, lumbar puncture, and brain MRI, even if asymptomatic, as soon as they can be safely performed. Changes in mental status at any time during therapy should be investigated urgently. Patients with proven CNS involvement should be treated with weekly intrathecal methotrexate and hydrocortisone until CSF abnormalities and symptoms normalize. Risk of posterior reversible encephalopathy syndrome appears to be significant during induction therapy.77 Although the etiology of posterior reversible encephalopathy syndrome is incompletely understood, it is more frequent in settings of hypertension and is also associated with cyclosporine use.78 Blood pressure should be aggressively managed during induction. Because CNS involvement suggests a genetic etiology and this disease feature is associated with substantial risks for long-term morbidity, we consider HCT for patients who develop this complication, especially in patients who do not have evidence of macrophage activation syndrome or underlying CNS infections.79
Supportive care
Infection
Supportive care guidelines for patients on therapy for HLH should be similar to standard practice for patients undergoing HCT, including acute care nursing, Pneumocystis jirovecii prophylaxis, fungal prophylaxis, intravenous immunoglobulin supplementation, and neutropenic precautions. Any new fever should be evaluated for HLH reactivation, as well as opportunistic infection, and empiric broad-spectrum antibiotic therapy initiated.
Bleeding
We do not recommend prophylactic heparin, which is sometimes used in acutely ill patients. Because of inflammation, consumptive coagulopathy, and intrinsic platelet defects in some patients, they are at very high risk of spontaneous bleeding.55,73,80 We aim to maintain platelet count > 50 × 109/L. Platelets, fresh frozen plasma, cryoprecipitate, and occasionally activated factor VII are required for acute bleeding. Depot leuprolide may be helpful in adolescent girls and women with menorrhagia.
Cardiac function
Patients may present with or develop acute cardiac dysfunction because of inflammation or possibly drug toxicity.81 We therefore evaluate baseline cardiac function at diagnosis. Furthermore, because of the inability to rule out concurrent vasculitis in patients with overlapping symptoms of Kawasaki disease, serial cardiac studies may be indicated in selected patients.82
Continuation therapy
Patients who can be weaned off of dexamethasone and etoposide without recurrence, recover normal immune function, and have no identified HLH-associated gene defects may stop therapy after the 8-week induction. HCT is generally recommended in patients with CNS involvement, recurrent/refractory disease, persistent NK cell dysfunction, or proven familial/genetic disease. Continuation according to HLH-94 consists of pulses of dexamethasone and etoposide (etoposide, 150 mg/m2, every 2 weeks; alternating with dexamethasone 10 mg/m2 per day × 3 days, every 2 weeks). Cyclosporine may be added in patients with stable blood pressure and adequate liver and kidney function. Patients on continuation therapy should proceed to HCT as quickly as possible because of the ongoing risks of infection, disease reactivation, or leukemia/MDS related to prolonged use of etoposide.
Salvage therapy
A significant number of patients with HLH will either fail to respond adequately to current therapies or relapse before HCT. Approximately 50% of patients treated on the HLH-94 study experienced a complete resolution of HLH, whereas 30% experienced a partial resolution and ∼ 20% died before HCT.71 Notably, most deaths occurred during the first few weeks of treatment and may reflect either preexisting morbidities or primary refractory disease. Although it is hoped that some patients will fare better with more prompt diagnosis of HLH, others remain unresponsive to standard therapy. Initial treatment with ATG (thymoglobulin, rabbit ATG) has been reported to give higher complete response rates; but in part the result of higher relapse rates, long-term outcomes do not appear superior.54 Although current therapy is effective, there is a need for new treatments for patients with refractory HLH.
At present, there are little data regarding potential second-line therapies. Case reports exist describing the use of infliximab, daclizumab, alemtuzumab, anakinra, vincristine, and other agents as salvage therapies for HLH.83–89 Because of the increasing recognition of the critical role of T cells in driving HLH pathogenesis, we began using alemtuzumab in 2006 to treat patients with refractory HLH.4 A recent analysis of our experience treating 25 patients found that alemtuzumab has significant activity against refractory HLH (Marsh, C.E.A., K.L.M., Weinstein, Washko, Skiles, Lee, Khan, Lawrence, Mo, Blessing, A.H.F., and M.B.J., manuscript submitted). Although refractory HLH appears to have a dismal prognosis, ∼ 70% of patients in our series survived. Because of its immunoablative qualities, alemtuzumab should be used with caution and by those with experience caring for profoundly immune-compromised patients. CMV reactivation and adenoviremia were frequent complications of this therapy.
In contrast to refractory patients, those patients who initially respond well to standard therapy but then relapse as treatment is tapered or withdrawn often respond to reintensification of therapy with standard agents. Our practice is to increase therapy back to initial levels, although this may need to be individualized. Because of the variability in patient responses, a critical aspect of initial or salvage therapy is close monitoring of the patients for improvement and potential toxicities, such as marrow suppression or infection.
HCT
Donor search should begin at the time of diagnosis because time to transplantation is a factor in morbidity and mortality from HLH, even though the precise etiology (eg, genetic defect) has not yet been defined. Generally, HCT is recommended in the case of documented familial HLH, recurrent or progressive disease despite intensive therapy, and CNS involvement.
Long-term disease-free survival after HCT was ∼ 50% to 65% before 2000, regardless of whether a matched sibling or closely matched unrelated donor was used.54,71,90 Most patients transplanted during that era died of “transplant-related” complications during the first 100 days after infusion. A significant proportion of fatal complications involved inflammatory conditions termed acute respiratory distress syndrome, veno-occlusive disease, and multisystem organ failure, unspecified. In rare cases, residual HLH was identified at autopsy, despite the use of myeloablative conditioning therapy. In contrast to the poor outcomes reported from the United States and Europe, an 86% long-term survival was achieved among 14 patients who underwent HCT for EBV-associated HLH in Japan.91
During the past decade, reduced intensity conditioning (RIC) regimens before HCT have been investigated after encouraging results from an institutional series.92 Most cases of RIC pretreatment have included alemtuzumab and demonstrated superior early posttransplantation survival. In a single-center analysis directly comparing HCT outcomes after myeloablative conditioning versus RIC, a statistically significant improvement was observed after RIC conditioning, with all patients surviving at 6 months after transplantation.93 At present, published data regarding outcome of RIC transplants using umbilical cord blood is not sufficient to draw conclusions regarding safety or efficacy. Donor choice should also take into account the possibility of an occult predisposition to HLH in siblings of patients without identified gene defects.
Much remains to be learned regarding the optimal application of alemtuzumab as well as other agents used before HCT. The timing of pretransplantation alemtuzumab impacts the probability of GVHD, mixed chimerism, and, in rare cases, rejection.93 Other factors, such as donor source, HLA match, cell dose, and patient condition with regard to HLH disease activity at time of conditioning, may all play a role in determining the likelihood of success after RIC HCT.
Because primary graft loss is common, we monitor total donor engraftment weekly in the early months after HCT. If total engraftment declines, especially approaching 50%-60% in the early posttransplantation months, it is possible to halt the decline in donor chimerism by the reduction or discontinuation of immunosuppression for GVHD prophylaxis. When this approach does not favorably impact declining donor chimerism, escalating doses of donor lymphocyte infusions may stabilize or increase donor chimerism. Full donor chimerism after transplantation is not required to suppress HLH disease in the majority of patients. Although very low levels of donor cells have been detected in healthy long-term survivors of HCT for HLH, the “safe” level of persistent total blood, or subset, chimerism is not known.
Patients with CNS HLH need close posttransplantation follow-up. We recommend examination of spinal fluid within 100 days of HCT, even in asymptomatic patients. Follow-up MRIs are recommended if pretransplantation abnormalities were present. In some patients with mixed or full hematopoietic donor chimerism, HLH disease activity in the CSF can be effectively treated with intrathecal therapy during the early posttransplantation months. CNS disease is subsequently controlled as donor immune reconstitution progresses.
Off therapy
If a patient is treated successfully and then weaned off of therapy because he is deemed to not need HCT, he should be monitored closely. Because the distinction between primary and secondary HLH is increasingly blurred, blanket recommendations for off-therapy patients are difficult to make and most follow-up decisions will have to be individualized. It appears that many patients who relapse do so within 1 year. In the absence of complicating medical issues, monthly follow-up once off therapy appears advisable during the first year, followed by annual follow-up thereafter.
New therapeutic approaches
As an alternative approach to etoposide-based approaches, ATG/prednisone have been used.54 Although a significant number of patients fail to respond adequately or completely to etoposide-based regimens, ATG-based regimens are complicated by relatively frequent and early relapse; median time to relapse reported by Ouachee-Chardin et al was 5.5 weeks.54 Thus, a rational combination of these approaches may improve outcomes by increasing initial responses and maintaining them until HCT can be obtained. Currently, a multicenter clinical trial, Hybrid Immunotherapy for HLH is underway in North America (http://clinicaltrials.gov/ct2/show/NCT01104025). In this approach, ATG and etoposide are incorporated into one regimen, but the etoposide dose intensity is decreased to minimize potential myelosuppression.
Although HLH appears to be a disease of excessive immune activation, the ideal form of immune suppression/anti-inflammatory therapy remains unknown. Although somewhat responsive to corticosteroids and clearly responsive to etoposide or anti-T-cell serotherapy (ATG or alemtuzumab), HLH remains difficult to treat. In the future, a variety of rationally designed immunosuppressive agents are likely to come into clinical use for transplantation or autoimmune disorders. Some of these agents may also prove to be useful for the treatment of HLH. Notably, interferon-γ was identified as an attractive therapeutic target in animal models of HLH, and anti–IFN-γ monoclonal antibodies will probably be tested in clinical trials involving patients with HLH.4,94 Future studies will focus on defining which immune-modulating strategies offer the best balance of safety and efficacy.
Acknowledgments
The authors thank Qian Wei, medical student at Duke University, and Dr Kejian Zhang, associate professor in the Division of Medical Genetics of Cincinnati Children's Hospital Medical Center, for creating Figure 1. This project was the result of discussions at the Texas Children's Cancer Center Histiocytosis Symposium, November 6-7, 2008, which was kindly supported by Ms Lisa Born.
This work was supported by the National Institutes of Health (R01HL091769; M.B.J.), the American Society of Hematology (C.E.A.), and the Hoag Foundation (C.E.A.).
Authorship
Contribution: All authors participated in conceptualizing, writing, and editing the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Kenneth L. McClain, Texas Children's Hospital, 6701 Fannin St, CC1410, Houston, TX 77030; e-mail: klmcclai@txccc.org; and Alexandra H. Filipovich, Cincinnati Children's Hospital Medical Center, 3333 Burnet Ave, Cincinnati, OH 45229; e-mail: lisa.filipovich@cchmc.org.
References
- 1.Farquhar JW, Claireaux AE. Familial haemophagocytic reticulosis. Arch Dis Child. 1952;27(136):519–525. doi: 10.1136/adc.27.136.519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Egeler RM, Shapiro R, Loechelt B, Filipovich A. Characteristic immune abnormalities in hemophagocytic lymphohistiocytosis. J Pediatr Hematol Oncol. 1996;18(4):340–345. doi: 10.1097/00043426-199611000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Stepp SE, Dufourcq-Lagelouse R, Le Deist F, et al. Perforin gene defects in familial hemophagocytic lymphohistiocytosis. Science. 1999;286(5446):1957–1959. doi: 10.1126/science.286.5446.1957. [DOI] [PubMed] [Google Scholar]
- 4.Jordan MB, Hildeman D, Kappler J, Marrack P. An animal model of hemophagocytic lymphohistiocytosis (HLH): CD8+ T cells and interferon gamma are essential for the disorder. Blood. 2004;104(3):735–743. doi: 10.1182/blood-2003-10-3413. [DOI] [PubMed] [Google Scholar]
- 5.Fall N, Barnes M, Thornton S, et al. Gene expression profiling of peripheral blood from patients with untreated new-onset systemic juvenile idiopathic arthritis reveals molecular heterogeneity that may predict macrophage activation syndrome. Arthritis Rheum. 2007;56(11):3793–3804. doi: 10.1002/art.22981. [DOI] [PubMed] [Google Scholar]
- 6.Sumegi J, Barnes MG, Nestheide SV, et al. Gene expression profiling of peripheral blood mononuclear cells from children with active hemophagocytic lymphohistiocytosis. Blood. 2011;117(15):e151–e160. doi: 10.1182/blood-2010-08-300046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Henter JI, Horne A, Arico M, et al. HLH-2004: diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2007;48(2):124–131. doi: 10.1002/pbc.21039. [DOI] [PubMed] [Google Scholar]
- 8.Allen CE, Yu X, Kozinetz CA, McClain KL. Highly elevated ferritin levels and the diagnosis of hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2008;50(6):1227–1235. doi: 10.1002/pbc.21423. [DOI] [PubMed] [Google Scholar]
- 9.Gupta A, Weitzman S, Abdelhaleem M. The role of hemophagocytosis in bone marrow aspirates in the diagnosis of hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2008;50(2):192–194. doi: 10.1002/pbc.21441. [DOI] [PubMed] [Google Scholar]
- 10.Clementi R, Emmi L, Maccario R, et al. Adult onset and atypical presentation of hemophagocytic lymphohistiocytosis in siblings carrying PRF1 mutations. Blood. 2002;100(6):2266–2267. doi: 10.1182/blood-2002-04-1030. [DOI] [PubMed] [Google Scholar]
- 11.Nagafuji K, Nonami A, Kumano T, et al. Perforin gene mutations in adult-onset hemophagocytic lymphohistiocytosis. Haematologica. 2007;92(7):978–981. doi: 10.3324/haematol.11233. [DOI] [PubMed] [Google Scholar]
- 12.zur Stadt U, Rohr J, Seifert W, et al. Familial hemophagocytic lymphohistiocytosis type 5 (FHL-5) is caused by mutations in Munc18-2 and impaired binding to syntaxin 11. Am J Hum Genet. 2009;85(4):482–492. doi: 10.1016/j.ajhg.2009.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lykens JE, Terrell CE, Zoller EE, Risma K, Jordan MB. Perforin is a critical physiologic regulator of T-cell activation. Blood. 2011;118(3):618–626. doi: 10.1182/blood-2010-12-324533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tang Y, Xu X, Song H, et al. Early diagnostic and prognostic significance of a specific Th1/Th2 cytokine pattern in children with haemophagocytic syndrome. Br J Haematol. 2008;143(1):84–91. doi: 10.1111/j.1365-2141.2008.07298.x. [DOI] [PubMed] [Google Scholar]
- 15.Fisman DN. Hemophagocytic syndromes and infection. Emerg Infect Dis. 2000;6(6):601–608. doi: 10.3201/eid0606.000608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Henter JI, Arico M, Egeler RM, et al. HLH-94: a treatment protocol for hemophagocytic lymphohistiocytosis. HLH study Group of the Histiocyte Society. Med Pediatr Oncol. 1997;28(5):342–347. doi: 10.1002/(sici)1096-911x(199705)28:5<342::aid-mpo3>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 17.Sawhney S, Woo P, Murray KJ. Macrophage activation syndrome: a potentially fatal complication of rheumatic disorders. Arch Dis Child. 2001;85(5):421–426. doi: 10.1136/adc.85.5.421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stephan JL, Kone-Paut I, Galambrun C, Mouy R, Bader-Meunier B, Prieur AM. Reactive haemophagocytic syndrome in children with inflammatory disorders: a retrospective study of 24 patients. Rheumatology (Oxford) 2001;40(11):1285–1292. doi: 10.1093/rheumatology/40.11.1285. [DOI] [PubMed] [Google Scholar]
- 19.Bleesing J, Prada A, Siegel DM, et al. The diagnostic significance of soluble CD163 and soluble interleukin-2 receptor alpha-chain in macrophage activation syndrome and untreated new-onset systemic juvenile idiopathic arthritis. Arthritis Rheum. 2007;56(3):965–971. doi: 10.1002/art.22416. [DOI] [PubMed] [Google Scholar]
- 20.Vastert SJ, Kuis W, Grom AA. Systemic JIA: new developments in the understanding of the pathophysiology and therapy. Best Pract Res Clin Rheumatol. 2009;23(5):655–664. doi: 10.1016/j.berh.2009.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.O'Brien MM, Lee-Kim Y, George TI, McClain KL, Twist CJ, Jeng M. Precursor B-cell acute lymphoblastic leukemia presenting with hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2008;50(2):381–383. doi: 10.1002/pbc.20950. [DOI] [PubMed] [Google Scholar]
- 22.Lackner H, Urban C, Sovinz P, Benesch M, Moser A, Schwinger W. Hemophagocytic lymphohistiocytosis as severe adverse event of antineoplastic treatment in children. Haematologica. 2008;93(2):291–294. doi: 10.3324/haematol.11704. [DOI] [PubMed] [Google Scholar]
- 23.Abe Y, Choi I, Hara K, et al. Hemophagocytic syndrome: a rare complication of allogeneic nonmyeloablative hematopoietic stem cell transplantation. Bone Marrow Transplant. 2002;29(9):799–801. doi: 10.1038/sj.bmt.1703554. [DOI] [PubMed] [Google Scholar]
- 24.Ferreira RA, Vastert SJ, Abinun M, et al. Hemophagocytosis during fludarabine-based SCT for systemic juvenile idiopathic arthritis. Bone Marrow Transplant. 2006;38(3):249–251. doi: 10.1038/sj.bmt.1705415. [DOI] [PubMed] [Google Scholar]
- 25.Falini B, Pileri S, De Solas I, et al. Peripheral T-cell lymphoma associated with hemophagocytic syndrome. Blood. 1990;75(2):434–444. [PubMed] [Google Scholar]
- 26.Su IJ, Wang CH, Cheng AL, Chen RL. Hemophagocytic syndrome in Epstein-Barr virus-associated T-lymphoproliferative disorders: disease spectrum, pathogenesis, and management. Leuk Lymphoma. 1995;19(5):401–406. doi: 10.3109/10428199509112197. [DOI] [PubMed] [Google Scholar]
- 27.Chin M, Mugishima H, Takamura M, et al. Hemophagocytic syndrome and hepatosplenic gammadelta T-cell lymphoma with isochromosome 7q and 8 trisomy. J Pediatr Hematol Oncol. 2004;26(6):375–378. doi: 10.1097/00043426-200406000-00008. [DOI] [PubMed] [Google Scholar]
- 28.Brodkin DE, Hobohm DW, Nigam R. Nasal-type NK/T-cell lymphoma presenting as hemophagocytic syndrome in an 11-year-old Mexican boy. J Pediatr Hematol Oncol. 2008;30(12):938–940. doi: 10.1097/MPH.0b013e31817e4b25. [DOI] [PubMed] [Google Scholar]
- 29.Petterson TE, Bosco AA, Cohn RJ. Aggressive natural killer cell leukemia presenting with hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2008;50(3):654–657. doi: 10.1002/pbc.21358. [DOI] [PubMed] [Google Scholar]
- 30.Tai CF, Chang LY, Lin DT, Lin KH, Jou ST, Yang YL. A case of natural killer cell lymphoma presenting with bilateral pleural effusions and hemophagocytic lymphohistocytosis. Pediatr Blood Cancer. 2009;52(5):666–669. doi: 10.1002/pbc.21943. [DOI] [PubMed] [Google Scholar]
- 31.Shimada A, Kato M, Tamura K, et al. Hemophagocytic lymphohistiocytosis associated with uncontrolled inflammatory cytokinemia and chemokinemia was caused by systemic anaplastic large cell lymphoma: a case report and review of the literature. J Pediatr Hematol Oncol. 2008;30(10):785–787. doi: 10.1097/MPH.0b013e318180bb33. [DOI] [PubMed] [Google Scholar]
- 32.Sovinz P, Lackner H, Schwinger W, Benesch M, Urban C, Beham-Schmid C. Anaplastic large cell lymphoma presenting as hemophagocytic syndrome in an adolescent. Pediatr Blood Cancer. 2007;49(7):1057. doi: 10.1002/pbc.21373. [DOI] [PubMed] [Google Scholar]
- 33.Myers TJ, Kessimian N, Schwartz S. Mediastinal germ cell tumor associated with the hemophagocytic syndrome. Ann Intern Med. 1988;109(6):504–505. doi: 10.7326/0003-4819-109-6-504. [DOI] [PubMed] [Google Scholar]
- 34.Urban C, Lackner H, Schwinger W, Beham-Schmid C. Fatal hemophagocytic syndrome as initial manifestation of a mediastinal germ cell tumor. Med Pediatr Oncol. 2003;40(4):247–249. doi: 10.1002/mpo.10127. [DOI] [PubMed] [Google Scholar]
- 35.Filipovich AH, Zhang K, Snow AL, Marsh RA. X-linked lymphoproliferative syndromes: brothers or distant cousins? Blood. 2010;116(18):3398–3408. doi: 10.1182/blood-2010-03-275909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McClain K, Gehrz R, Grierson H, Purtilo D, Filipovich A. Virus-associated histiocytic proliferations in children: frequent association with Epstein-Barr virus and congenital or acquired immunodeficiencies. Am J Pediatr Hematol Oncol. 1988;10(3):196–205. [PubMed] [Google Scholar]
- 37.Nichols KE, Ma CS, Cannons JL, Schwartzberg PL, Tangye SG. Molecular and cellular pathogenesis of X-linked lymphoproliferative disease. Immunol Rev. 2005;203:180–199. doi: 10.1111/j.0105-2896.2005.00230.x. [DOI] [PubMed] [Google Scholar]
- 38.Beutel K, Gross-Wieltsch U, Wiesel T, Stadt UZ, Janka G, Wagner HJ. Infection of T lymphocytes in Epstein-Barr virus-associated hemophagocytic lymphohistiocytosis in children of non-Asian origin. Pediatr Blood Cancer. 2009;53(2):184–190. doi: 10.1002/pbc.22037. [DOI] [PubMed] [Google Scholar]
- 39.Fox CP, Shannon-Lowe C, Gothard P, et al. Epstein-Barr virus-associated hemophagocytic lymphohistiocytosis in adults characterized by high viral genome load within circulating natural killer cells. Clin Infect Dis. 2010;51(1):66–69. doi: 10.1086/653424. [DOI] [PubMed] [Google Scholar]
- 40.Imashuku S. Treatment of Epstein-Barr virus-related hemophagocytic lymphohistiocytosis (EBV-HLH): update 2010. J Pediatr Hematol Oncol. 2011;33(1):35–39. doi: 10.1097/MPH.0b013e3181f84a52. [DOI] [PubMed] [Google Scholar]
- 41.Kasahara Y, Yachie A, Takei K, et al. Differential cellular targets of Epstein-Barr virus (EBV) infection between acute EBV-associated hemophagocytic lymphohistiocytosis and chronic active EBV infection. Blood. 2001;98(6):1882–1888. doi: 10.1182/blood.v98.6.1882. [DOI] [PubMed] [Google Scholar]
- 42.Imashuku S, Kuriyama K, Teramura T, et al. Requirement for etoposide in the treatment of Epstein-Barr virus-associated hemophagocytic lymphohistiocytosis. J Clin Oncol. 2001;19(10):2665–2673. doi: 10.1200/JCO.2001.19.10.2665. [DOI] [PubMed] [Google Scholar]
- 43.Heslop HE. How I treat EBV lymphoproliferation. Blood. 2009;114(19):4002–4008. doi: 10.1182/blood-2009-07-143545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Milone MC, Tsai DE, Hodinka RL, et al. Treatment of primary Epstein-Barr virus infection in patients with X-linked lymphoproliferative disease using B-cell-directed therapy. Blood. 2005;105(3):994–996. doi: 10.1182/blood-2004-07-2965. [DOI] [PubMed] [Google Scholar]
- 45.Schneider EM, Lorenz I, Muller-Rosenberger M, Steinbach G, Kron M, Janka-Schaub GE. Hemophagocytic lymphohistiocytosis is associated with deficiencies of cellular cytolysis but normal expression of transcripts relevant to killer-cell-induced apoptosis. Blood. 2002;100(8):2891–2898. doi: 10.1182/blood-2001-12-0260. [DOI] [PubMed] [Google Scholar]
- 46.My LT, Lien le B, Hsieh WC, et al. Comprehensive analyses and characterization of haemophagocytic lymphohistiocytosis in Vietnamese children. Br J Haematol. 2010;148(2):301–310. doi: 10.1111/j.1365-2141.2009.07957.x. [DOI] [PubMed] [Google Scholar]
- 47.Nagai K, Yamamoto K, Fujiwara H, et al. Subtypes of familial hemophagocytic lymphohistiocytosis in Japan based on genetic and functional analyses of cytotoxic T lymphocytes. PLoS One. 2010;5(11):e14173. doi: 10.1371/journal.pone.0014173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zur Stadt U, Beutel K, Kolberg S, et al. Mutation spectrum in children with primary hemophagocytic lymphohistiocytosis: molecular and functional analyses of PRF1, UNC13D, STX11, and RAB27A. Hum Mutat. 2006;27(1):62–68. doi: 10.1002/humu.20274. [DOI] [PubMed] [Google Scholar]
- 49.Palazzi DL, McClain KL, Kaplan SL. Hemophagocytic syndrome in children: an important diagnostic consideration in fever of unknown origin. Clin Infect Dis. 2003;36(3):306–312. doi: 10.1086/345903. [DOI] [PubMed] [Google Scholar]
- 50.Arico M, Janka G, Fischer A, et al. Hemophagocytic lymphohistiocytosis: report of 122 children from the International Registry. FHL Study Group of the Histiocyte Society. Leukemia. 1996;10(2):197–203. [PubMed] [Google Scholar]
- 51.Niece JA, Rogers ZR, Ahmad N, Langevin AM, McClain KL. Hemophagocytic lymphohistiocytosis in Texas: observations on ethnicity and race. Pediatr Blood Cancer. 2010;54(3):424–428. doi: 10.1002/pbc.22359. [DOI] [PubMed] [Google Scholar]
- 52.Ost A, Nilsson-Ardnor S, Henter JI. Autopsy findings in 27 children with haemophagocytic lymphohistiocytosis. Histopathology. 1998;32(4):310–316. doi: 10.1046/j.1365-2559.1998.00377.x. [DOI] [PubMed] [Google Scholar]
- 53.Stapp J, Wilkerson S, Stewart D, Coventry S, Mo JQ, Bove KE. Fulminant neonatal liver failure in siblings: probable congenital hemophagocytic lymphohistiocytosis. Pediatr Dev Pathol. 2006;9(3):239–244. doi: 10.2350/06-01-0005.1. [DOI] [PubMed] [Google Scholar]
- 54.Ouachee-Chardin M, Elie C, de Saint BG, et al. Hematopoietic stem cell transplantation in hemophagocytic lymphohistiocytosis: a single-center report of 48 patients. Pediatrics. 2006;117(4):e743–e750. doi: 10.1542/peds.2005-1789. [DOI] [PubMed] [Google Scholar]
- 55.Sandrock K, Nakamura L, Vraetz T, Beutel K, Ehl S, Zieger B. Platelet secretion defect in patients with familial hemophagocytic lymphohistiocytosis type 5 (FHL-5). Blood. 2010;116(26):6148–6150. doi: 10.1182/blood-2010-08-302943. [DOI] [PubMed] [Google Scholar]
- 56.Schaer DJ, Schaer CA, Schoedon G, Imhof A, Kurrer MO. Hemophagocytic macrophages constitute a major compartment of heme oxygenase expression in sepsis. Eur J Haematol. 2006;77(5):432–436. doi: 10.1111/j.1600-0609.2006.00730.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Biondi CS, Cotorruelo CM, Ensinck A, Racca LL, Racca AL. Use of the erythrophagocytosis assay for predicting the clinical consequences of immune blood cell destruction. Clin Lab. 2004;50(5):265–270. [PubMed] [Google Scholar]
- 58.Kraus MD, Bartlett NL, Fleming MD, Dorfman DM. Splenic pathology in myelodysplasia: a report of 13 cases with clinical correlation. Am J Surg Pathol. 1998;22(10):1255–1266. doi: 10.1097/00000478-199810000-00011. [DOI] [PubMed] [Google Scholar]
- 59.Morrell DS, Pepping MA, Scott JP, Esterly NB, Drolet BA. Cutaneous manifestations of hemophagocytic lymphohistiocytosis. Arch Dermatol. 2002;138(9):1208–1212. doi: 10.1001/archderm.138.9.1208. [DOI] [PubMed] [Google Scholar]
- 60.Henter JI, Elinder G, Soder O, Ost A. Incidence in Sweden and clinical features of familial hemophagocytic lymphohistiocytosis. Acta Paediatr Scand. 1991;80(4):428–435. doi: 10.1111/j.1651-2227.1991.tb11878.x. [DOI] [PubMed] [Google Scholar]
- 61.Janka GE. Familial hemophagocytic lymphohistiocytosis. Eur J Pediatr. 1983;140(3):221–230. doi: 10.1007/BF00443367. [DOI] [PubMed] [Google Scholar]
- 62.Palazzi DL, McClain KL, Kaplan SL. Hemophagocytic syndrome after Kawasaki disease. Pediatr Infect Dis J. 2003;22(7):663–666. [PubMed] [Google Scholar]
- 63.Fitzgerald N, McClain KL. Imaging characteristics of hemophagocytic lymphohistiocytosis. Pediatr Radiol. 2003;33:392–401. doi: 10.1007/s00247-003-0894-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Horne A, Trottestam H, Arico M, et al. Frequency and spectrum of central nervous system involvement in 193 children with haemophagocytic lymphohistiocytosis. Br J Haematol. 2008;140(3):327–335. doi: 10.1111/j.1365-2141.2007.06922.x. [DOI] [PubMed] [Google Scholar]
- 65.Goo HW, Weon YC. A spectrum of neuroradiological findings in children with haemophagocytic lymphohistiocytosis. Pediatr Radiol. 2007;37(11):1110–1117. doi: 10.1007/s00247-007-0569-z. [DOI] [PubMed] [Google Scholar]
- 66.Liao PM, Thompson JT. Ophthalmic manifestations of virus-associated hemophagocytic syndrome. Arch Ophthalmol. 1991;109(6):777. doi: 10.1001/archopht.1991.01080060033015. [DOI] [PubMed] [Google Scholar]
- 67.Park JK, Palexas GN, Streeten BW, Green WR. Ocular involvement in familial erythrophagocytic lymphohistiocytosis. Graefes Arch Clin Exp Ophthalmol. 1997;235(10):647–652. doi: 10.1007/BF00946941. [DOI] [PubMed] [Google Scholar]
- 68.Petersen RA, Kuwabara T. Ocular manifestations of familial lymphohistiocytosis. Arch Ophthalmol. 1968;79(4):413–416. doi: 10.1001/archopht.1968.03850040415009. [DOI] [PubMed] [Google Scholar]
- 69.Boutin B, Routon MC, Rocchiccioli F, et al. Peripheral neuropathy associated with erythrophagocytic lymphohistiocytosis. J Neurol Neurosurg Psychiatry. 1988;51(2):291–294. doi: 10.1136/jnnp.51.2.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.De Armas R, Sindou P, Gelot A, Routon MC, Ponsot G, Vallat JM. Demyelinating peripheral neuropathy associated with hemophagocytic lymphohistiocytosis: an immuno-electron microscopic study. Acta Neuropathol. 2004;108(4):341–344. doi: 10.1007/s00401-004-0897-0. [DOI] [PubMed] [Google Scholar]
- 71.Henter JI, Samuelsson-Horne A, Arico M, et al. Treatment of hemophagocytic lymphohistiocytosis with HLH-94 immunochemotherapy and bone marrow transplantation. Blood. 2002;100(7):2367–2373. doi: 10.1182/blood-2002-01-0172. [DOI] [PubMed] [Google Scholar]
- 72.Mahlaoui N, Ouachee-Chardin M, de Saint BG, et al. Immunotherapy of familial hemophagocytic lymphohistiocytosis with antithymocyte globulins: a single-center retrospective report of 38 patients. Pediatrics. 2007;120(3):e622–e628. doi: 10.1542/peds.2006-3164. [DOI] [PubMed] [Google Scholar]
- 73.Buyse S, Teixeira L, Galicier L, et al. Critical care management of patients with hemophagocytic lymphohistiocytosis. Intensive Care Med. 2010;36(10):1695–1702. doi: 10.1007/s00134-010-1936-z. [DOI] [PubMed] [Google Scholar]
- 74.Aronoff GR, Bennett WM, Berns JS. Dosing Guidelines for Adults and Children. 5th ed. Philadelphia, PA: American College of Physicians; 2007. Drug prescribing in renal failure. [DOI] [PubMed] [Google Scholar]
- 75.Joel SP, Shah R, Clark PI, Slevin ML. Predicting etoposide toxicity: relationship to organ function and protein binding. J Clin Oncol. 1996;14(1):257–267. doi: 10.1200/JCO.1996.14.1.257. [DOI] [PubMed] [Google Scholar]
- 76.Lin TF, Ferlic-Stark LL, Allen CE, Kozinetz CA, McClain KL. Rate of decline of ferritin in patients with hemophagocytic lymphohistiocytosis as a prognostic variable for mortality. Pediatr Blood Cancer. 2011;56(1):154–155. doi: 10.1002/pbc.22774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Thompson PA, Allen CE, Horton T, Jones JY, Vinks AA, McClain KL. Severe neurologic side effects in patients being treated for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2009;52(5):621–625. doi: 10.1002/pbc.21838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bechstein WO. Neurotoxicity of calcineurin inhibitors: impact and clinical management. Transpl Int. 2000;13(5):313–326. doi: 10.1007/s001470050708. [DOI] [PubMed] [Google Scholar]
- 79.Haddad E, Sulis ML, Jabado N, Blanche S, Fischer A, Tardieu M. Frequency and severity of central nervous system lesions in hemophagocytic lymphohistiocytosis. Blood. 1997;89(3):794–800. [PubMed] [Google Scholar]
- 80.Meeths M, Entesarian M, Al-Herz W, et al. Spectrum of clinical presentations in familial hemophagocytic lymphohistiocytosis type 5 patients with mutations in STXBP2. Blood. 2010;116(15):2635–2643. doi: 10.1182/blood-2010-05-282541. [DOI] [PubMed] [Google Scholar]
- 81.Creput C, Galicier L, Buyse S, Azoulay E. Understanding organ dysfunction in hemophagocytic lymphohistiocytosis. Intensive Care Med. 2008;34(7):1177–1187. doi: 10.1007/s00134-008-1111-y. [DOI] [PubMed] [Google Scholar]
- 82.Newburger JW, Takahashi M, Gerber MA, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Pediatrics. 2004;114(6):1708–1733. doi: 10.1542/peds.2004-2182. [DOI] [PubMed] [Google Scholar]
- 83.Bruck N, Suttorp M, Kabus M, Heubner G, Gahr M, Pessler F. Rapid and sustained remission of systemic juvenile idiopathic arthritis-associated macrophage activation syndrome through treatment with anakinra and corticosteroids. J Clin Rheumatol. 2011;17(1):23–27. doi: 10.1097/RHU.0b013e318205092d. [DOI] [PubMed] [Google Scholar]
- 84.Henzan T, Nagafuji K, Tsukamoto H, et al. Success with infliximab in treating refractory hemophagocytic lymphohistiocytosis. Am J Hematol. 2006;81(1):59–61. doi: 10.1002/ajh.20462. [DOI] [PubMed] [Google Scholar]
- 85.Imashuku S, Hibi S, Ohara T, et al. Effective control of Epstein-Barr virus-related hemophagocytic lymphohistiocytosis with immunochemotherapy: Histiocyte Society. Blood. 1999;93(6):1869–1874. [PubMed] [Google Scholar]
- 86.Kobayashi Y, Salih HM, Kajiume T, et al. Successful treatment with liposteroid followed by reduced intensity stem cell transplantation in an infant with perforin deficiency presenting with hemophagocytic lymphohistiocytosis. J Pediatr Hematol Oncol. 2007;29(3):178–182. doi: 10.1097/MPH.0b013e3180335030. [DOI] [PubMed] [Google Scholar]
- 87.Olin RL, Nichols KE, Naghashpour M, et al. Successful use of the anti-CD25 antibody daclizumab in an adult patient with hemophagocytic lymphohistiocytosis. Am J Hematol. 2008;83(9):747–749. doi: 10.1002/ajh.21236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Strout MP, Seropian S, Berliner N. Alemtuzumab as a bridge to allogeneic SCT in atypical hemophagocytic lymphohistiocytosis. Nat Rev Clin Oncol. 2010;7(7):415–420. doi: 10.1038/nrclinonc.2010.40. [DOI] [PubMed] [Google Scholar]
- 89.Tomaske M, Amon O, Bosk A, Handgretinger R, Schneider EM, Niethammer D. Alpha-CD25 antibody treatment in a child with hemophagocytic lymphohistiocytosis. Med Pediatr Oncol. 2002;38(2):141–142. doi: 10.1002/mpo.1294. [DOI] [PubMed] [Google Scholar]
- 90.Horne A, Janka G, Maarten ER, et al. Haematopoietic stem cell transplantation in haemophagocytic lymphohistiocytosis. Br J Haematol. 2005;129(5):622–630. doi: 10.1111/j.1365-2141.2005.05501.x. [DOI] [PubMed] [Google Scholar]
- 91.Ohga S, Kudo K, Ishii E, et al. Hematopoietic stem cell transplantation for familial hemophagocytic lymphohistiocytosis and Epstein-Barr virus-associated hemophagocytic lymphohistiocytosis in Japan. Pediatr Blood Cancer. 2010;54(2):299–306. doi: 10.1002/pbc.22310. [DOI] [PubMed] [Google Scholar]
- 92.Cooper N, Rao K, Gilmour K, et al. Stem cell transplantation with reduced-intensity conditioning for hemophagocytic lymphohistiocytosis. Blood. 2006;107(3):1233–1236. doi: 10.1182/blood-2005-05-1819. [DOI] [PubMed] [Google Scholar]
- 93.Marsh RA, Vaughn G, Kim MO, et al. Reduced-intensity conditioning significantly improves survival of patients with hemophagocytic lymphohistiocytosis undergoing allogeneic hematopoietic cell transplantation. Blood. 2010;116(26):5824–5831. doi: 10.1182/blood-2010-04-282392. [DOI] [PubMed] [Google Scholar]
- 94.Pachlopnik Sshmid J, Ho CH, Chretien F, et al. Neutralization of IFNgamma defeats haemophagocytosis in LCMV-infected perforin- and Rab27a-deficient mice. EMBO Mol Med. 2009;1(2):112–124. doi: 10.1002/emmm.200900009. [DOI] [PMC free article] [PubMed] [Google Scholar]