Abstract
Huntington disease (HD) is a dominantly inherited neurodegenerative disorder that is caused by a mutant huntingtin (HTT) gene encoding a version of the Htt protein with an expanded polyglutamine stretch. Although the HTT gene was discovered more than 18 years ago, the functions of normal Htt and the mechanisms by which mutant Htt causes disease are not well defined. In this issue of the JCI, Keryer et al. uncovered a novel function for normal Htt in ciliogenesis and report that mutant Htt causes hypermorphic ciliogenesis and ciliary dysfunction. These observations suggest that it is now critical to understand the extent to which ciliary dysfunction contributes to the different symptoms of HD and to determine whether therapeutic strategies designed to normalize ciliary function can ameliorate the disease.
Huntington disease (HD) is an autosomal-dominant disorder caused by expansion of a CAG repeat in the first exon of the huntingtin (HTT) gene (1). This repeat encodes an expanded stretch of polyglutamine residues at the amino terminus of the Htt protein. HD is predominantly an adult-onset disorder that is characterized by progressive neuronal cell death primarily in the striatum and deep layers of the cortex. Clinically, it is characterized by motor, cognitive, and neuropsychiatric abnormalities that cause a progressive loss of functional capacity and reduced life span (2). There are currently no effective treatments for this devastating neurodegenerative disease. This stems largely from an incomplete understanding of the cellular and molecular mechanisms by which mutant Htt causes disease.
Evidence obtained from cell culture and animal model studies supports the hypothesis that the polyglutamine expansion in mutant Htt confers on the protein both a toxic gain of function and a partial loss of normal function (3). More than 100 Htt-interacting proteins have been identified, implicating Htt as a participant in a diverse array of cellular processes (4). One of the most predominant of these processes is microtubule-based transport of vesicles and organelles. The role of Htt in intracellular transport is mediated by its direct interaction with the dynein intermediate chain within the dynein microtubule motor complex (5) and by an indirect interaction with dynein via its association with a complex containing huntingtin-associated protein 1 (HAP1) and dynactin (6). In the presence of mutant Htt, dynein function is compromised, perturbing vesicle and organelle transport along microtubules.
In this issue of the JCI, Keryer and colleagues have linked the function of Htt in intracellular transport to ciliogenesis (7). As mutant Htt was found to cause hypermorphic ciliogenesis and ciliary dysfunction, it is possible that several symptoms of HD might be caused, at least in part, by ciliary dysfunction.
Cilia and ciliopathies
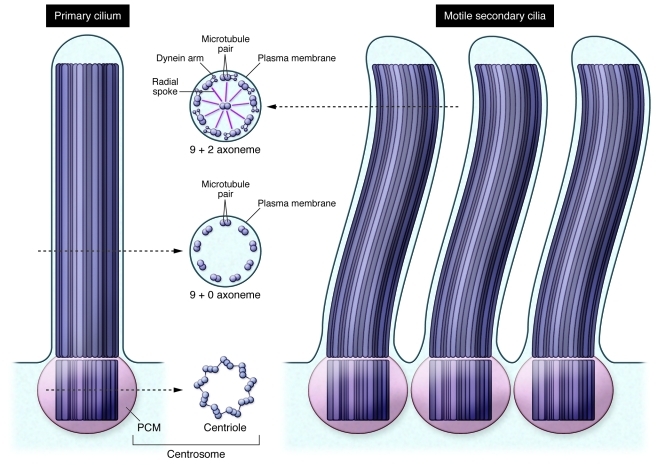
Primary cilia are single hair-like protrusions 1–5 μm in length that are present on virtually all cells, including neurons and glia (8, 9). Primary cilia are nonmotile and have a microtubule skeleton consisting of nine microtubule pairs (9 + 0 axoneme), whereas motile secondary cilia have the same outer nine microtubule pairs, but include inner and outer dynein arms and a pair of central microtubules (9 + 2 axoneme) (Figure 1). Primary cilia in mammalian neurons are derived from a centriole within the centrosome and are located on the soma or proximal portion of the apical dendrite. They are thought to be involved in sensing the extracellular environment and in signal transduction of the various sensory modalities. Motile secondary cilia in the brain (such as those found on ependymal cells lining the lateral ventricles) are critical for maintaining the flow of cerebrospinal fluid (CSF) through the ventricles and sensing the composition of the CSF.
Figure 1. Structure of primary and motile secondary cilia.
Primary and motile secondary cilia differ in the structure of their axoneme. Primary cilia have an axoneme composed of nine pairs of microtubules (9 + 0 axoneme), whereas the axoneme of motile secondary cilia also includes a central pair of microtubules (9 + 2 axoneme). Each of the nine outer pairs of microtubules in the axoneme of motile secondary cilia have inner and outer dynein arms that connect with an adjacent pair of outer microtubules and radial spokes connecting them with the central pair of microtubules. At the base of primary cilia is a basal body composed of a centrosome (centriole plus surrounding PCM). Motile secondary cilia also have basal bodies consisting of centrioles and PCM.
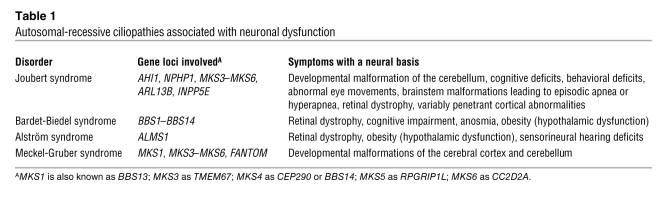
There are several known genetic disorders that are caused by defects in primary cilium formation, structure, and function; these conditions are known as ciliopathies (8). Among these are a group of autosomal-recessive developmental disorders — including Joubert, Bardet-Biedel, and Meckel-Gruber syndromes — that include nervous system dysfunction among their many symptoms (Table 1). Abnormalities in primary cilia have also been observed recently in a mouse model of the adult-onset neurodegenerative disorder familial amyotrophic lateral sclerosis (10). These observations, together with the data generated by Keryer et al. indicating that the mutant Htt protein underlying HD can drive ciliary dysfunction (7), suggest that aberrant cilia function might contribute to the pathogenesis of other adult-onset neurodegenerative disorders.
Table 1 .
Autosomal-recessive ciliopathies associated with neuronal dysfunction
A novel function for Htt in ciliogenesis
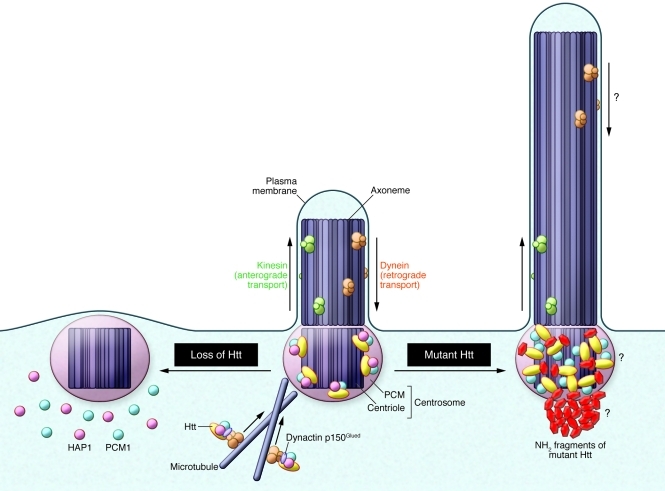
Using both in vitro and in vivo systems, Keryer et al. provide evidence of a functional role for Htt in ciliogenesis (7). They found that Htt and HAP1 regulated ciliogenesis by transporting pericentriolar material 1 protein (PCM1) to the centrosome (Figure 2). In the absence of Htt or HAP1 expression, mislocalization of PCM1 reduced primary cilium formation in neurons and glia in culture and led to hypomorphic motile secondary cilia in ependymal cells. The latter contributed to hydrocephalus in an Htt loss-of-function mouse model.
Figure 2. Mutant Htt and loss of normal Htt have opposing effects on ciliogenesis.
Keryer and colleagues showed that mutant Htt drives increased ciliogenesis and the formation of hypermorphic primary cilia, whereas loss of Htt results in reduced ciliogenesis (7). These results suggest that normal Htt acts as a molecular scaffold in dynein/dynactin/HAP1-mediated transport of PCM1 to the centrosome. In the absence of Htt, dynein-mediated transport of PCM1 to the centrosome is impaired, and a primary cilium is not formed. In contrast, the presence of mutant Htt causes accumulation of PCM1 at the centrosome, increased ciliogenesis, and lengthening of the primary cilium. It is not yet known in HD whether dynein-mediated intraflagellar transport is affected, whether PCM1 is associated in a complex with mutant Htt and/or HAP1 at the centrosome, or whether aggresome formation can affect ciliary function.
In contrast to the hypomorphic ciliogenesis phenotype observed when normal Htt expression was reduced, Keryer et al. found that mutant Htt expression had the opposite effect on ciliogenesis (ref. 7 and Figure 2): excess PCM1 accumulated at the centrosome, the percentage of neurons and glia with primary cilia was increased in vitro, and ependymal cell cilia were lengthened in a mouse model of HD. In the model of HD, this phenotype led to abnormal CSF flow that affected neuroblast migration from the subventricular zone to the olfactory bulb. In addition, the authors observed an increase in PCM1 and N-acetylated tubulin (a marker of cilia) immunoreactivity in postmortem brains of individuals with HD.
Cilia dysfunction and HD symptoms
The work of Keryer et al. (7) suggests that several symptoms of HD may be caused, at least in part, by dysfunctional primary and secondary cilia. Their data suggest that defects in ependymal motile cilia impair CSF flow, resulting in an abnormal rostral migratory stream (RMS). Adult neurogenesis in the subventricular zone generates neuroblasts that migrate through the RMS into the olfactory bulb, where they differentiate into interneurons. Normal CSF circulation is required to orient the neuroblasts in the RMS, and the dysfunctional ependymal cilia observed by Keryer et al. in the mouse model of HD led to reduced CSF flow, affecting neuroblast migration (7). The authors speculate that a defective RMS may contribute to the olfactory deficits experienced by HD patients and that reduced CSF flow in HD may also affect brain homeostasis by altering the clearance of brain catabolites.
Neurons expressing olfactory receptors also have nonmotile secondary cilia that are important for normal function (11). In Bardet-Biedel syndrome, for example, defective cilia function in olfactory receptor neurons can cause anosmia in humans (12). Although not examined by Keryer and colleagues, it will be interesting to see whether hypertrophic cilia are observed in the olfactory epithelia of HD mouse models and patients, and if so, whether this structural abnormality affects olfactory receptor neuronal function.
The dentate gyrus region of the hippocampus contains adult neuronal stem and progenitor cells with primary cilia in both rodents and humans (13–15). Given that Keryer et al. identified defects in ependymal motile cilia and neuronal primary cilia (7), it will be important in future studies to determine whether adult neuronal stem cells in the brains of rodents and humans with HD have hypertrophic cilia and whether this phenotype correlates with deficits in adult neuronal stem cell function in HD. This may have direct relevance to cognitive dysfunction in HD, as it has previously been shown that adult hippocampal neurogenesis in rodents is involved in learning and memory (16).
The increased ciliogenesis in HD mouse model astrocytes observed by Keryer et al. (7) could also contribute to the deficits in astrocyte function that are observed in HD (17). Astrocytes have a critical role in maintaining neuronal homeostasis, and the increased ciliogenesis observed in HD may perturb the ability of astrocytes to sense and respond to changes in its environment, thus affecting neuronal survival.
How does mutant Htt affect cilia function?
Although aggregation of PCM1 in the choroid plexus and ependymal cell layer of the lateral ventricles was detected by Keryer et al. as early as 5 months of age in a mouse model of HD, abnormal cilia were only observed later, at 12 months of age (7). This phenotype appears to differ from the classic autosomal-recessive ciliopathies that exhibit early developmental abnormalities (Table 1), instead resembling the slow progression of degeneration that is characteristic of HD.
A neuropathological hallmark of HD is the accumulation of aggregated amino-terminal fragments of mutant Htt in the cytoplasm (neuropil inclusions) and nuclei (nuclear intranuclear inclusions). Small cytoplasmic Htt aggregates can be transported to the centrosome, where they coalesce to form an aggresome that can protect cells from the buildup of misfolded protein (18). The work of Keryer et al. (7) leads us to wonder whether the formation of the aggresome affects cilia function in the HD brain. The authors’ observations also raise a number of other important questions: How does the aggregation of PCM1 affect ciliogenesis, ciliary maintenance, ciliary signaling, or some combination thereof? Are other ciliary cargos affected? Is transport along the axoneme (intraflagellar transport) also affected? These are critical questions, as the answers have direct relevance to the design of therapeutic strategies aimed at restoring the function of primary and motile cilia in HD patients.
In addition to perturbing HAP1 and dynein function (3), mutant Htt affects membrane trafficking by interfering with the activities of Rab8 and Rab11, two small GTPases that function in ciliogenesis (19–21). Mutant Htt expression disrupts both Rab8 and Rab11 activity by affecting normal localization of Rab8 on Golgi membranes (20) and by impairing guanine nucleotide exchange factor activity on Rab11, resulting in reduced recycling of cargo proteins (21). Expression of a constitutively active form of Rab11 in primary neurons from an HD mouse model ameliorates deficits in extracellular cysteine uptake by restoring cell surface levels of the glutamate transporter EAAC1 (22), and overexpression of Rab11 in a Drosophila model of HD rescues neurodegeneration and extends lifespan (23). Thus, it is possible that manipulating the activity and expression levels of HAP1, dynein, Rab8, and Rab11 might ameliorate at least some aspects of ciliary dysfunction in HD.
Therapeutic perspectives for treating cilia dysfunction in HD
The present study by Keryer and colleagues has uncovered a mechanism underlying HD pathogenesis that may provide a new therapeutic target for the disease (7). Although not all pathological events in HD can be explained by defective ciliogenesis and abnormal ciliary function, amelioration of those symptoms caused by abnormal primary and secondary ciliary function should improve the quality of life for patients with HD and may provide relief for symptoms that do not yet exhibit an obvious link to ciliary dysfunction. Moreover, as morphological and functional criteria for primary and secondary cilia already exist, the establishment of cell culture–based high-throughput screens for small molecules able to rescue the effects of mutant Htt on ciliogenesis and ciliary function should be feasible.
Acknowledgments
The authors thank Emily Andre for comments and suggestions. This work was supported in part by the NIH (NINDS NS043466) and by CHDI Foundation Inc.
Footnotes
Conflict of interest: The authors have declared that no conflict of interest exists.
Citation for this article: J Clin Invest. 2011;121(11):4237–4241. doi:10.1172/JCI60243.
See the related article beginning on page 4372.
References
- 1.The Huntington’s Disease Collaborative Research Group. A novel gene containing a trinucleotide repeat that is expanded and unstable on Huntington’s disease chromosomes. Cell. 1993;72(6):971–983. doi: 10.1016/0092-8674(93)90585-E. [DOI] [PubMed] [Google Scholar]
- 2. Hayden MR.Huntington’s Chorea . New York, New York, USA: Springer-Verlag; 1981. [Google Scholar]
- 3.Zuccato C, Valenza M, Cattaneo E. Molecular mechanisms and potential therapeutical targets in Huntington’s disease. Physiol Rev. 2010;90(3):905–981. doi: 10.1152/physrev.00041.2009. [DOI] [PubMed] [Google Scholar]
- 4.Harjes P, Wanker EE. The hunt for huntingtin function: interaction partners tell many different stories. Trends Biochem Sci. 2003;28(8):425–433. doi: 10.1016/S0968-0004(03)00168-3. [DOI] [PubMed] [Google Scholar]
- 5.Caviston JP, Zajac AL, Tokito M, Holzbaur EL. Huntingtin coordinates the dynein-mediated dynamic positioning of endosomes and lysosomes. Mol Biol Cell. 2011;22(4):478–492. doi: 10.1091/mbc.E10-03-0233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rong J, Li SH, Li XJ. Regulation of intracellular HAP1 trafficking. J Neurosci Res. 2007;85(14):3025–3029. doi: 10.1002/jnr.21326. [DOI] [PubMed] [Google Scholar]
- 7.Keryer G, et al. Ciliogenesis is regulated by a huntingtin-HAP1-PCM1 pathway and is altered in Huntington disease. J Clin Invest. 2011;121(11):4372–4382. doi: 10.1172/JCI57552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gerdes JM, Davis EE, Katsanis N. The vertebrate primary cilium in development, homeostasis, and disease. Cell. 2009;137(1):32–45. doi: 10.1016/j.cell.2009.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Louvi A, Grove EA. Cilia in the CNS: the quiet organelle claims center stage. Neuron. 2011;69(6):1046–1060. doi: 10.1016/j.neuron.2011.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ma X, Peterson R, Turnbull J. Adenylyl Cyclase type 3, a marker of primary cilia, is reduced in primary cell culture and in lumbar spinal cord in situ in G93A SOD1 mice. BMC Neurosci. 2011;12:71. doi: 10.1186/1471-2202-12-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Elsaesser R, Paysan J. The sense of smell, its signalling pathways, and the dichotomy of cilia and microvilli in olfactory sensory cells. BMC Neurosci. 2007;8(suppl 3):S1. doi: 10.1186/1471-2202-8-S3-S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kulaga HM, et al. Loss of BBS proteins causes anosmia in humans and defects in olfactory cilia structure and function in the mouse. Nature Genet. 2004;36(9):994–998. doi: 10.1038/ng1418. [DOI] [PubMed] [Google Scholar]
- 13.Alvarez-Buylla A, Seri B, Doetsch F. Identification of neural stem cells in the adult vertebrate brain. Brain Res Bull. 2002;57(6):751–758. doi: 10.1016/S0361-9230(01)00770-5. [DOI] [PubMed] [Google Scholar]
- 14.Quinones-Hinojosa A, et al. Cellular composition and cytoarchitecture of the adult human subventricular zone: a niche of neural stem cells. J Comp Neurol. 2006;494(3):415–434. doi: 10.1002/cne.20798. [DOI] [PubMed] [Google Scholar]
- 15.Han Y-G, Alvarez-Buylla A. Role of primary cilia in brain development and cancer. Curr Opin Neurobiol. 2010;20(1):58–67. doi: 10.1016/j.conb.2009.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Deng W, Aimone JB, Gage FH. New neurons and new memories: how does adult hippocampal neurogenesis affect learning and memory? Nat Rev Neurosci. 2010. 11 5 339 350 . 10.1038/nrn2822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bradford J, et al. Mutant huntingtin in glial cells exacerbates neurological symptoms of Huntington disease mice. J Biol Chem. 2010;285(14):10653–10661. doi: 10.1074/jbc.M109.083287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Johnston JA, Ward CL, Kopito RR. Aggresomes: a cellular response to misfolded proteins. J Cell Biol. 1998;143(7):1883–1898. doi: 10.1083/jcb.143.7.1883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Knodler A, et al. Coordination of Rab8 and Rab11 in primary ciliogenesis. Proc Natl Acad Sci U S A. 2010;107(14):6346–6351. doi: 10.1073/pnas.1002401107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.del Toro D, et al. Mutant huntingtin impairs post-Golgi trafficking to lysosomes by delocalizing optineurin/Rab8 complex from the Golgi apparatus. Mol Biol Cell. 2009;20(5):1478–1492. doi: 10.1091/mbc.E08-07-0726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li X, et al. Mutant huntingtin impairs vesicle formation from recycling endosomes by interfering with Rab11 activity. Mol Cell Biol. 2009;29(22):6106–6116. doi: 10.1128/MCB.00420-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li X, et al. Aberrant Rab11-dependent trafficking of the neuronal glutamate transporter EAAC1 causes oxidative stress and cell death in Huntington’s disease. J Neurosci. 2010;30(13):4552–4561. doi: 10.1523/JNEUROSCI.5865-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Richards P, et al. Dendritic spine loss and neurodegeneration is rescued by Rab11 in models of Huntington’s disease. Cell Death Differ. 2011;18(2):191–200. doi: 10.1038/cdd.2010.127. [DOI] [PMC free article] [PubMed] [Google Scholar]