The results of renal transplantation in black recipients have been conflicting. Many reports have described inferior graft survival in blacks.1-12 Other reports have shown no difference between black and white recipients.13-17 The reason for these disparate findings is not clear. Speculation has centered around the response to cyclosporine,10 HLA and Lewis antigen matching differences,7,10,12 and the center effect.11,13
Two other important issues in renal transplantation concern organ allocation and immunosuppressive management. In 1986, the point system was implemented at the University of Pittsburgh to provide end-stage renal disease (ESRD) patients with equal access to cadaver kidneys.18 The system, developed in Pittsburgh and since adopted by the United Network for Organ Sharing (UNOS), takes into account waiting time, number of HLA antigens matched, and the degree of sensitization. Medical urgency and logistical factors play a much smaller role. A recipient for a given kidney is selected according to rank on the list as determined by these objective criteria. Since race does not enter into consideration, the point system is formally color blind.
In our most recent analyses of graft and patient survival after the introduction of the point system into clinical practice, we noted and confirmed the important effect of the immunosuppressive regimen.19,20 The three-drug combination of cyclosporine, azathioprine, and prednisone was associated with a 10 to 15% improvement in graft survival when compared with cyclosporine and prednisone alone. This observation held up in all subgroup analyses, including those of sensitized patients. In this article, we present our experience with renal transplantation, looking specifically at the question of patient and graft survival in black and white recipients. We concern ourselves specifically with the 2½-year period after the introduction of the point system.
Patients and Methods
Five hundred forty-nine renal transplantations were performed at the University of Pittsburgh Hospitals (Presbyterian-University Hospital and Children's Hospital of Pittsburgh) between January 1, 1986, and June 30, 1988. Eight of the kidneys were from living related donors and were excluded from analysis. Similarly excluded were 11 cases of cadaver kidney transplantation in conjunction with a liver or a heart transplant. There were thus 530 consecutive cases available for analysis. Seventy-five (14.2%) kidneys were transplanted into black recipients; the total number of Hispanic and Asian recipients was less than 1% of the total recipient population. These figures are in close proportion to the local referral base in Pittsburgh.
Of the 450 adults, 383 (85.1%) were white and 67 (14.9%) were black. They received 413 and 71 transplants, respectively. The mean age was 42.2 ± 12.9 years and 43.1 ± 12.6 years, respectively. The most common disease of the native kidneys was chronic glomerulonephritis. Ninety-five (23%) of the white adult recipients and 10 (14%) of the black adult recipients were diabetics, almost all type I.
Three black children received 4 transplants, whereas 37 white children received 42 transplants: 3 of the black children and 23 of the white children were 10 to 18 years old, and no black children and 14 white children were 6 months to 9 years old.
Twenty-seven (5.1%) of the kidneys came from black donors, and 503 (94.9%) were from white donors.
Tissue Typing
The HLA typing for all donors and all recipients was carried out in an accredited laboratory in which all class I and class II antigens can be measured. Antidonor antibodies were systematically looked for, and crossmatches with recipient sera were performed in every case.
Point Allocation System
The Pittsburgh allocation system ranks potential recipients of a given kidney on the basis of several factors.18 Waiting time, defined as beginning with the date of referral, can account for up to 10 points. Each class I or class II antigen match between donor and recipient counts for 2 points, for a potential total of 12 if there is complete HLA identity. Every 10% of panel reactive antibody (PRA) counts for 1 point, for a potential total of 10 points, if there are antibodies against all the lymphocyte test panel (100% PRA). Finally, medical urgency or logistic factors can add points, although these are rarely used. Thus, the system gives priority to those who have waited the longest, those with the best antigen match, and those with the greatest degree of presensitization who have a negative crossmatch.
Immunosuppression
During 1986, all patients were managed initially with cyclosporine and prednisone. In 1987, just under half of the recipients were started on cyclosporine, azathioprine, and prednisone. In 1988, all patients were induced with the three-drug regimen. Variations of this triple-drug regimen were described in 1984 at the International Transplantation Society, or shortly thereafter.21-24 Earlier, the combination of cyclosporine and azathioprine had been tested in primates by Reitz et al,25 and synergism was demonstrated in rats and dogs by Squifflet et al,26 By the time of the 1986 meeting in Helsinki of the International Transplantation Society, more than a dozen papers describing the advantages of three-drug or four-drug therapy were presented.
OKT3 was used for steriod-resistant rejection episodes.27 In some highly sensitized patients or cases of multiple retransplantation, OKT3 was used for induction.
Statistical Methods
Actuarial patient and graft survivals were calculated for the 2-year period. Statistical analysis was performed using BMDP software. Significance was assessed by the Mantel-Cox or the Breslow test.
Results
Patient Survival and Causes of Death
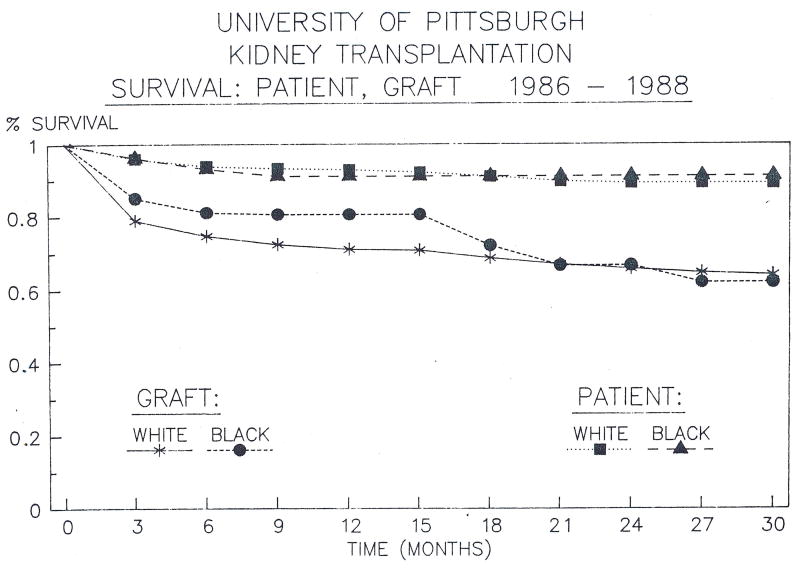
Seventy black patients received 75 kidneys, and 420 white patients received 455 kidneys. The actuarial patient survival at 1 and 2 years was 91% in black patients; for white recipients it was 93% and 90% (Fig 1). Five (7.1%) black and 35 (8.4%) white recipients have died. The causes of death for black and white recipients are listed in Table 1. In 80% of the cases, there had been difficulty in maintaining good renal graft function (Table 1), either early, because of acute rejection, or later because of chronic rejection or other factors. Apart from this factor, the most common principal cause of the events leading to death was infection, usually caused by opportunistic organisms or viruses.
Fig 1. Overall patient and graft survival in blacks and whites under the point system, 1986-1988.
Table 1. Causes of Death After Renal Transplantation.
| Cause of Death | Graft Functioning | Graft Removed or Nonfunctioning | Total | |||
|---|---|---|---|---|---|---|
| B | W | B | W | B | W | |
| Infection | 0 | 1 | 4 | 10 | 4 | 11 |
| Cardiovascular | 0 | 4 | 0 | 5 | 0 | 9 |
| Gastrointestinal | 0 | 1 | 1 | 3 | 1 | 4 |
| Respiratory | 0 | 0 | 0 | 2 | 0 | 2 |
| Malignancy | 0 | 0 | 0 | 1 | 0 | 1 |
| Technical | 0 | 0 | 0 | 1 | 0 | 1 |
| Miscellaneous (D.I.C., multiple organ failure, hyperkalemia, bleed after biopsy, motor vehicle accident) | 0 | 2 | 0 | 3 | 0 | 5 |
| Unknown | 0 | 0 | 0 | 2 | 0 | 2 |
|
|
|
|
|
|
|
|
| Total | 0 | 8 | 5 | 27 | 5 | 35 |
| Grand total | 8 (20%) | 32 (80%) | 40 | |||
Graft Survival
In black recipients, 1- and 2-year actuarial graft survival was 80% and 66%; the corresponding figures in the white population were 72% and 67%. These percentages were not statistically different (Fig 1). Although the sophisticated examination of tissue typing was not part of the study, there was no obvious effect of tissue matching (Table 2). The incidence of success was about the same in both blacks and whites with all levels of compatibility. Graft survival has been 4-30 months.
Table 2. Matching in 491 Cases in Which There Was Adequate Donor/Recipient Typing.
| No. of Antigens Matched | Black | White | Total |
|---|---|---|---|
| 6 | 0 | 5/6 (83%) | 5/6 (83%) |
| 5 | 0 | 3/5 (60%) | 3/5 (60%) |
| 4 | 2/2 (100%) | 12/17 (71%) | 14/19 (74%) |
| 3 | 4/6 (67%) | 41/67 (61%) | 45/73 (62%) |
| 2 | 13/16 (81%) | 81/113 (72%) | 94/129 (73%) |
| 1 | 19/24 (79%) | 96/138 (70%) | 115/162 (71%) |
| 0 | 13/23 (57%) | 47/74 (64%) | 60/97 (62%) |
|
|
|
|
|
| 51/71 (72%) | 285/420 (68%) | 336/491 (68%) |
Because some of the patients received more than one graft during the 1986 to 1988 study period, the actual number of patients represented by the 530 cadaveric transplantations was 490. Of the 490 patients, 450 (92%) are alive and 362 (74%) are off dialysis (Table 3). The percentages for blacks and whites are nearly identical. Thus, a higher percentage of patients have a good result after renal transplantation than is indicated by actuarial graft survival.
Table 3. Fate of 70 Black Recipients of 75 Grafts and 420 White Recipients of 455 Grafts.
| Black | White | Total | |
|---|---|---|---|
| Alive | 65 (92.9%) | 385 (91.7%) | 450 (91.8%) |
| Off dialysis | 52 (74.3%) | 310 (73.8%) | 362 (73.9%) |
| On dialysis | 13 (18.6%) | 75 (17.9%) | 88 (17.9%) |
| Dead | 5 (7.1%) | 35 (8.3%) | 40 (8.2%) |
Donor Effect
Twenty-seven kidneys from black donors were transplanted into 3 black and 24 white recipients. One-year graft survival was 100% and 58.3%, respectively (Table 4). Five hundred three kidneys from white donors were transplanted into 72 black and 431 white recipients. One-year graft survival was 79.2% and 72.2%, respectively. These figures were not statistically different.
Table 4. The Donor Effect: Number of Kidneys Transplanted and Percent Surviving at 1 Year (by Race of Recipient).
| Race of Donor | Race of Recipient | |||
|---|---|---|---|---|
| Number of Kidneys | 1-Year Graft Survival | |||
| Black | White | Black | White | |
| Black | 3 | 24 | 100% | 58.3% |
| White | 72 | 431 | 79.2% | 72.2% |
Adults vs Children
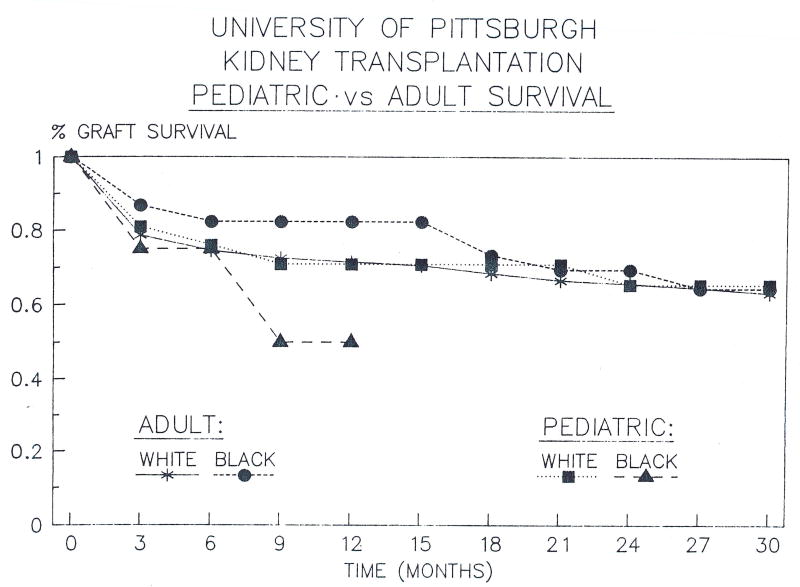
Black and white adults and children did not differ significantly in overall graft survival (Fig 2). None of 3 black children and 4 of 37 (10.8%) white children had died, with a mortality similar to that of adults.
Fig 2. Graft survival, pediatric and adult blacks and whites.
Primary Transplantation vs Retransplantation
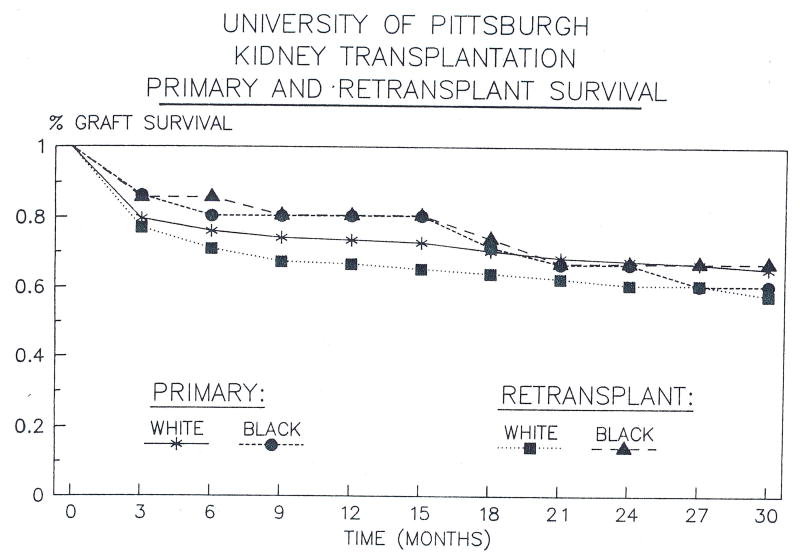
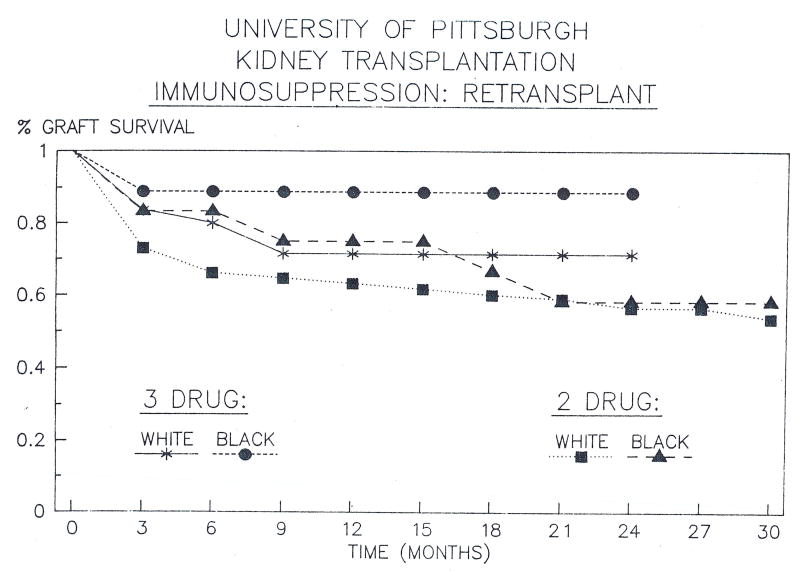
The results in transplanting patients for the first time were slightly but not significantly better than the results with retransplantation (Fig 3). Again, there was no difference between black and white recipients.
Fig 3. Graft survival, primary transplantation and retransplantatlon in blacks and whites.
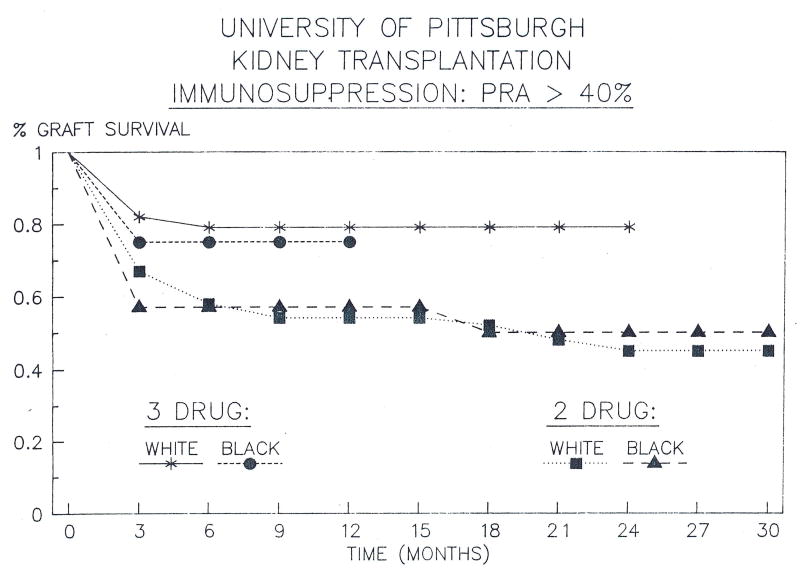
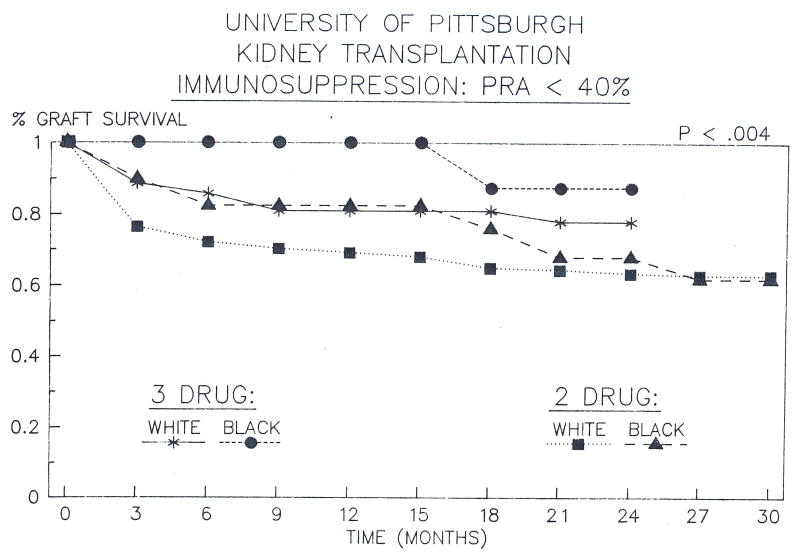
Transplantation to Unsensitized vs Sensitized Patients
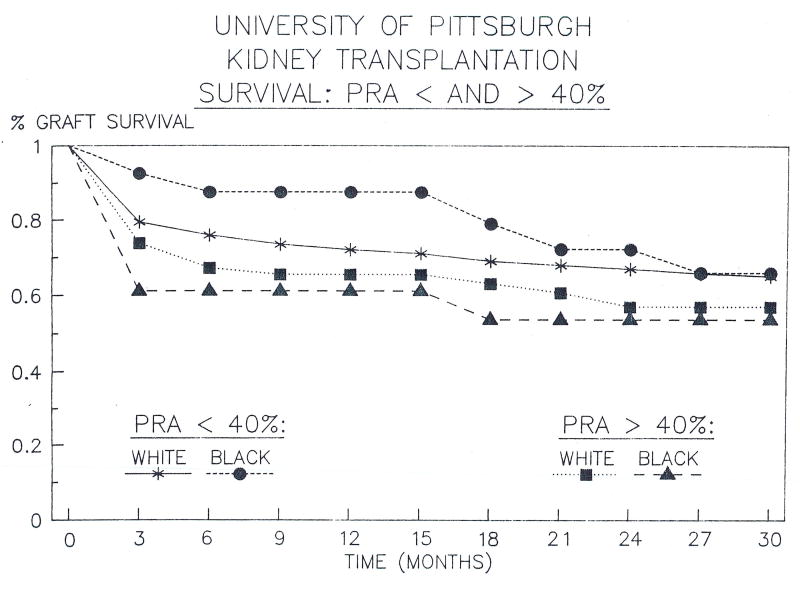
Black patients with a PRA less than 40% had a significantly (p < 0.05) better survival than did blacks with a PRA greater than 40% (Fig 4). Similar results were noted in white recipients. This observation has been noted in most series.
Fig 4. Graft survival, PRA <40% and >40% in blacks and whites.
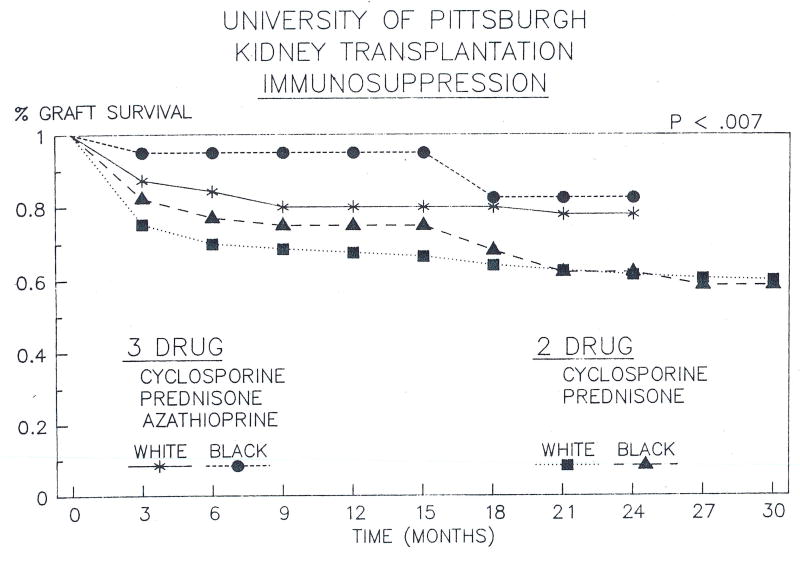
Effect of Triple- vs Double-Drug Immunosuppression
Beginning in January 1987, a subgroup of patients was treated with cyclosporine, azathioprine, and prednisone, and graft survival was found to be significantly better than with the cohort of patients receiving cyclosporine and steroids alone. Since January 1988, all patients have received triple-drug immunosuppression, and the initially favorable results have continued. In the triple therapy group, actuarial 1-year graft survival has been 95% and 80% in blacks and whites, respectively, and in those receiving double therapy, the corresponding figures are 75% and 68% (p < 0.007) (Fig 5).
Fig 5. Graft survival, three-drug and two-drug immunosuppression in blacks and whites.
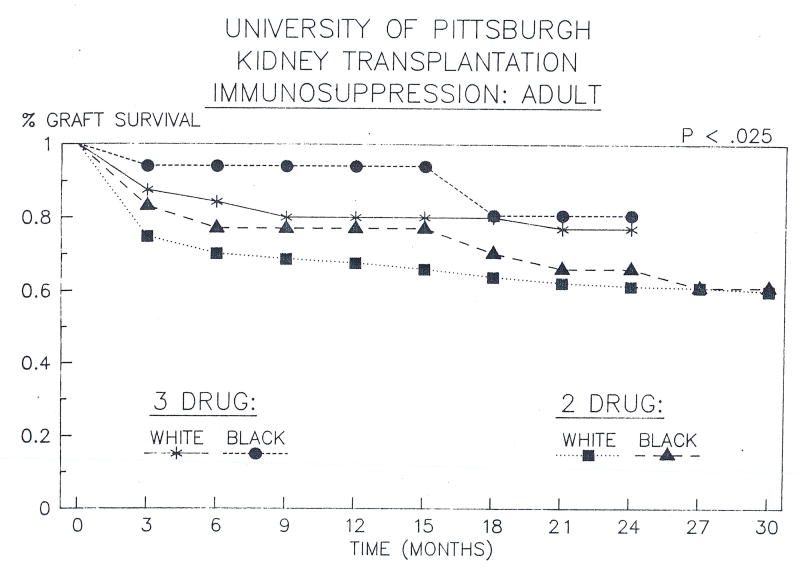
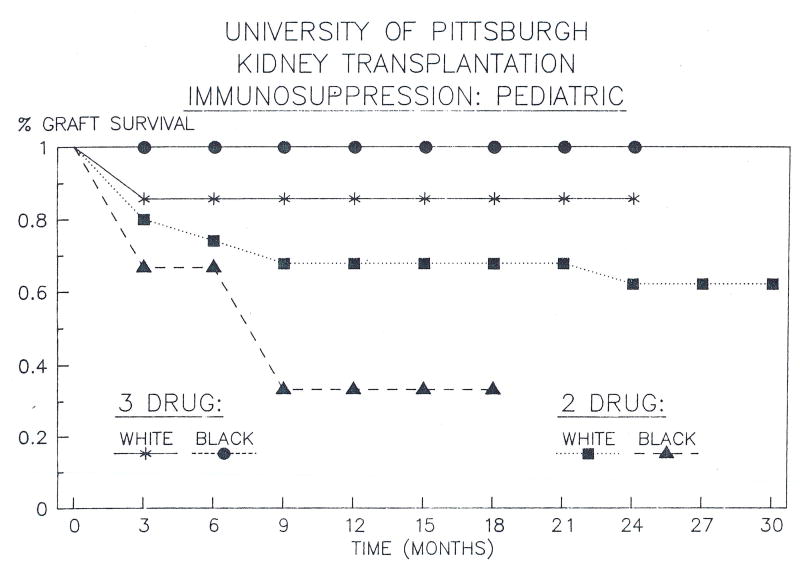
Adults vs Children
The advantage of triple-drug therapy was approximately the same whether the recipients were in the black or white adult or pediatric population (Figs 6 and 7), although the numbers in the pediatric group were too small to show statistical significance.
Fig 6. Graft survival, three-drug and two-drug immunosuppression in black and white adults.
Fig 7. Graft survival, three-drug and two-drug immunosuppression in black and white children.
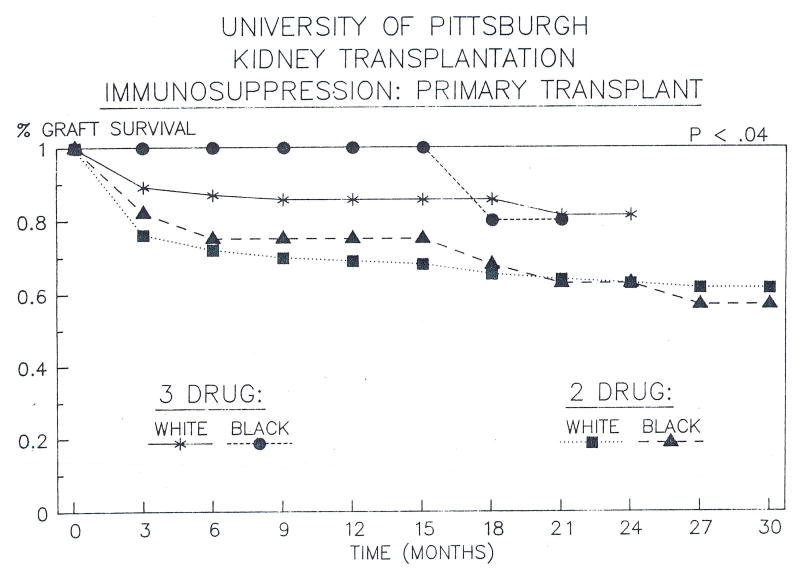
Primary Transplantation vs Retransplantation
In both black and white recipients, triple-drug immunosuppression was associated with improved 1-year graft survival in primary grafts (p < 0.04) (Fig 8). There also appeared to be improved survival in retransplantation, although the numbers were too small to show statistical significance (Fig 9). Again, there was no difference between blacks and whites.
Fig 8. Graft survival, three-drug and two-drug Immunosuppression for primary transplantations in blacks and whites.
Fig 9. Graft survival, three-drug and two-drug immunosuppression for retransplantation in blacks and whites.
Low vs High PRA
Triple-drug therapy seemed to be somewhat advantageous for sensitized black and white patients. Actuarial 1-year graft survival was 75% and 79%, respectively, compared to 57% and 55% under double-drug treatment. Black and white recipients with low PRAs had an actuarial 1-year survival of 100% and 81%, respectively, under triple-drug immunosuppression compared to 83% and 70% with double-drug treatment (Figs 10 and 11) (p < 0.004). There was no difference between black and white recipients. Thus triple-drug therapy upgraded survival in both the favorable and immunologically unfavorable patient categories.
Fig 10. Graft survival, three-drug and two-drug Immunosuppression in blacks and whites with PRA >40%.
Fig 11. Graft survival, three-drug and two-drug immunosuppression in blacks and whites with PRA <40%.
Discussion
Many articles have been published describing inferior renal allograft survival in black recipients.1-7, 9-13 Multiple explanations have been offered. A few articles have demonstrated equivalent graft survival rates between blacks and writes.13-17 In a review combining the results of many centers. Terasaki et al claim that the inferior graft survival in blacks was merely a center effect and that there was in fact no racial difference.11,13 Specifically, they pointed out that if centers with “excellent” results, there were no differences between blacks and whites. In centers with “fair” results, graft survival in blacks was inferior. The fact that more black recipients were transplanted in centers with fair results accounts for the overall poorer graft survival seen in blacks.
Our experience under the point system demonstrated at least equivalent graft survival between black and white recipients. There was, in fact, a trend toward superior results in black recipients, but this difference was not statistically significant. The implications are reassuring in several different ways. Critics of the point system have argued that the goal of transplantation should be to maximize graft survival and the way to accomplish this is to transplant the “best” recipients, ie, those who are young and healthy and have low PRAs.28 Kjellstrand's analysis has shown how this ad hoc selection process systematically excluded blacks from the “best” designation.29 In our previous reports of experience with the point system, we noted and confirmed that excellent patient and graft survival could be obtained under a system that ensured equal access to donor organs. In this regard, the important advantage of three-drug over two-drug immunosuppression was emphasized. An equitable allocation system ensures that black recipients will come to transplantation as often as white recipients. Our results indicate that black and white recipients have equally good results under such a system. Furthermore, the effect of immunosuppressive protocol was seen in both blacks and whites.
The results seen in renal transplantation in blacks have generated enough controversy to lead to this conference. It is our hope that the demonstration of equally good results in black and white recipients with the point system will help to settle this issue.
Acknowledgments
We thank the renal transplant coordinators, Lisa Streb, RN, Loraine Kaminski, RN, Regina Fenton, RN, Joan Murray, RN, and Deborah Good, RN, for their care of the patients and their help with data collection; Dr Robert D. Gordon, Sandi Mitchell, MSIS, and Jeanne Kowalski for their help with the data analysis; Donna Ross for typing this article; Robert Karausky and Terry Trees, PhD, for fashioning the tables and graphs; and Toni Pratt for her help with the data organization and entry.
Supported by Research Grants from the Veterans Administration and Project Grant No. DK 29961 from the National Institutes of Health.
References
- 1.Opelz G, Mickey MR, Terasaki PI. Transplant Proc. 1977;9:137. [PubMed] [Google Scholar]
- 2.Stuart FP, Hill LJ, Reckard CR, et al. Arch Surg. 1979;114:416. doi: 10.1001/archsurg.1979.01370280070010. [DOI] [PubMed] [Google Scholar]
- 3.Opelz G, Terasaki PI. 8th Histocompatibility Workshop Study on Renal Transplantation. 1980:592. [Google Scholar]
- 4.Pfaff WW, Morehead RA, Fennell RS, et al. Ann Surg. 1980;191:617. doi: 10.1097/00000658-198005000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spees EK, Vaughn WK, Niblack G, et al. Transplant Proc. 1981;13:155. [PubMed] [Google Scholar]
- 6.Oriol R, Le Pendu J, Chun C. Transplantation. 1982;33:22. doi: 10.1097/00007890-198201000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Pfaff WW, Howard RJ, Ireland J, et al. Transplant Proc. 1983;15:1139. [Google Scholar]
- 8.Krakauer H, Grauman JS, McMullan MR, et al. N Engl J Med. 1983;308:1558. doi: 10.1056/NEJM198306303082603. [DOI] [PubMed] [Google Scholar]
- 9.Weller JM, Wu SC, Ferguson W, et al. Am J Kidney Dis. 1987;9:191. doi: 10.1016/s0272-6386(87)80054-9. [DOI] [PubMed] [Google Scholar]
- 10.Barger BO, Hudson SL, Shroyer TW, et al. Clin Transplants. 1988:217. [PubMed] [Google Scholar]
- 11.Kondo K, Shibue T, Iwaki Y, et al. Clin Transplants. 1988:339. [PubMed] [Google Scholar]
- 12.Diethelm AG, Blackstone EH, Naftel DC, et al. Ann Surg. 1988;207:538. doi: 10.1097/00000658-198805000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Perdue ST, Terasaki PI. Transplantation. 1982;34:75. doi: 10.1097/00007890-198208000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Mittal VK, Toledo-Pereyra LH, Baskin S, et al. Am Surgeon. 1983;49:436. [PubMed] [Google Scholar]
- 15.Krakauer H, Spees EK, Vaughn WK, et al. Transplantation. 1983;36:372. doi: 10.1097/00007890-198310000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Garvin PJ, Castaneda M, Codd JE, et al. Arch Surg. 1983;118:1441. doi: 10.1001/archsurg.1983.01390120061016. [DOI] [PubMed] [Google Scholar]
- 17.Ward HJ, Koyle MA, Terasaki PI, et al. Transplant Proc. 1987;19:1546. [PubMed] [Google Scholar]
- 18.Starzl TE, Hakala T, Tzakis A, et al. JAMA. 1987;257:3073. [PMC free article] [PubMed] [Google Scholar]
- 19.Shapiro R, Tzakis AG, Hakala TR, et al. Contrib Nephrol. 1989;70:30. doi: 10.1159/000416901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shapiro R, Tzakis AG, Hakala TR, et al. Clin Transplants. 1989:181. [PMC free article] [PubMed] [Google Scholar]
- 21.Illner WD, Land W, Habersetzer R, et al. Transplant Proc. 1985;17:1181. [Google Scholar]
- 22.Slapak M, Goeghegan T, Digard N, et al. Transplant Proc. 1985;17:1222. [Google Scholar]
- 23.Fries D, Kechrid C, Charpentier B, et al. Transplant Proc. 1985;17:1231. [Google Scholar]
- 24.Simmons RL, Canafax DM, Strand M, et al. Transplant Proc. 1985;17:266. [PubMed] [Google Scholar]
- 25.Reitz BA, Bieber CP, Raney AA, et al. Transplant Proc. 1981;13:393. [PubMed] [Google Scholar]
- 26.Squifflet JP, Sutherland DER, Rynasiewicz JJ, et al. Transplantation. 1982;34:315. doi: 10.1097/00007890-198212000-00001. [DOI] [PubMed] [Google Scholar]
- 27.Fung JJ, Demetris AJ, Porter KA, et al. Nephron. 1987;96:19. doi: 10.1159/000184431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fryd DS. JAMA. 1988;259:840. doi: 10.1001/jama.1988.03720060012012. [DOI] [PubMed] [Google Scholar]
- 29.Kjellstrand CM. Arch Intern Med. 1988;148:1305. [PubMed] [Google Scholar]