Abstract
Purpose
To evaluate a panel of pretreatment clinical and laboratory parameters in metastatic melanoma (MM) in order to verify their impact on response and survival in a single prospective multi-institutional phase III study comparing out-patient chemotherapy (CT) vs bioCT.
Methods
A total of 176 patients were randomised to receive CT (cisplatin, dacarbazine, optional carmustine) or bioCT (the same CT followed by subcutaneous IL-2 plus intramuscular α-IFN-2b). Pretreatment total leucocytes, lymphocytes, eosinophyls, C-reactive protein (CRP), lactate dehydrogenase (LDH), erytrosedimentation rate (ESR), and fibrinogen were analyzed. Some clinical parameters (performance status, age, sex, and disease site) were also considered. As we found a positive trend for bio-CT with no statistical significance in OR (25.3% vs 20.2%) and OS (11 Mo vs 9.5 Mo), all analyses are stratified by treatment arm.
Results
In univariate analysis, higher value of lymphocytes percentage (P < .0001), lower value of total leucocytes (P=.005), CRP (P=.003), LHD (P < .0001), ESR (P < .027), fibrinogen (P < .0001), and no liver disease were strongly related to a better survival. In a multivariate analysis, using the Cox proportional hazards model, only fibrinogen (P=.004), LDH (P=.009) and liver disease (P=.04) were found to have an independent role on clinical outcome in metastatic melanoma patients.
Conclusion
Liver disease and higher LDH and fibrinogen levels had an important impact on survival in MM patients. In particular, fibrinogen has been recently reconsidered both for its determinant role in the host hemostatic system, and for its capability to provide protection against NK and LAK-cell-induced lysis. These observations could have some important implications for therapeutic approaches, in particular when immunological strategies are used.
Introduction
The incidence of melanoma has increased more rapidly over the last half century than that of all other forms of cancer, except for lung cancer in female smokers. Earlier diagnosis of primary disease has resulted in an increased frequency of surgical cure with a 5 years survival rate of 80–100%, but in patients in which melanoma recurs, life expectancy at 3 years is less than 10%, with a median survival of about 7 months [1,2].
The efficacy of adding immunotherapy to chemotherapeutic regimens in metastatic melanoma (MM) is questionable. The first few published phase III trials seem to indicate a greater efficacy of combined chemoimmunotherapy as far as response rates are concerned, but toxicity and quality of life seem to worsen and overall survival rate is not always higher [3,4].
Several studies have attempted to identify factors that have an important impact on response and survival in metastatic melanoma (MM) patients. All these studies resulted in opportunities for stratification of patients for clinical trials using some clinical and laboratory parameters. In fact, the current American Joint Committee on Cancer (AJCC) staging system distinguishes in M category three different prognostic groups according to metastatic sites and serum levels of lactate dehydrogenase [5].
Among clinical parameters, the number and the pattern of metastatic disease were found to be two statistically significant prognostic factors that strongly correlated with survival [6-9]. For instance patients with liver involvement have a very poor prognosis similar to those with central nervous system disease [10]. Soft tissue and/or single visceral organ metastases were independent positive predictors for survival [9,11]. Also poor performance status and the presence of symptoms (reduced appetite, fever, nausea/vomiting), and sex (male patients) were associated with a poorer survival [6-8,10,11]. On the contrary, period of enrollment (enrollment late in the decade) and prior immunotherapy were associated with an improved prognosis [9,11].
In patients treated with interleukin-2-based immunotherapy, visceral metastases were again correlated with a poorer clinical response [12]. In addition, in patients treated with high-dose intravenous bolus IL-2, the presence of only subcutaneous and/or cutaneous metastases was associated to a higher response rate (53.6 %) with respect to other sites of disease (12.4%). Moreover, responding patients developed long-term immunologic side effects such as abnormal thyroid function tests and vitiligo [13].
A series of laboratory parameters has been also correlated with response and survival in MM patients. Pre-treatment high level of LDH and low levels of albumin showed the capability of predicting survival behaviour in a significant and adequate way. [7-9,11]. Also abnormal baseline values of alkaline phosphatase, and platelets were found prognostic for a poorer survival [9]. C-reactive protein (CRP) together with clinically defined group (patients with superficial or visceral metastases) were found to be indipendent predictors on multifactorial analysis in patients treated with IL-2 containing therapy. Thus, patients with high levels of CRP and/or visceral organ involvement could be unlikely to respond to IL-2 therapy [12].
Most data regarding pretreatment values of total lymphocytes and lymphocyte subsets in cancer patients have been recently published, but their real impact on clinical outcome and prognosis is still unclear [14]. Among patients treated with high-dose intravenous bolus IL-2, responding patients developed a higher maximum lymphocytes count immediately after therapy with respect to non-responding patients but baseline lymphocytes seem to have no impact on survival [13].
Finally, the role of fibrinogen in the metastatic potential of tumor cells has been recently reconsidered both for its determinant role in the host hemostatic system, and for its capability to providing protection against NK and LAK-cell-induced lysis [15-17].
In our single prospective multi-institutional phase III study comparing out-patient chemotherapy (CT) versus bioCT, we analyzed a panel of pretreatment laboratory and clinical factors to verify their impact on response and survival. Among the laboratory parameters we considered: total leucocytes, lymphocytes, eosinophyls, C-reactive protein (CRP), lactate dehydrogenase (LDH), erytrosedimentation rate (ESR), and fibrinogen. Finally, we evaluated also some clinical parameters: performance status (PS), age, sex, and disease site.
Patients and Methods
Patients and treatment
We carried out a multicentric randomized study to compare the standard polychemotherapeutic scheme including DTIC and CDDP with a chemo-immunotherapeutic scheme adding low dose of IL-2 and α-IFN subcutaneously, as immunomodulants. The participating centres had the choice of adding carmustine (BCNU) to the chemotherapeutic schedule for all their patients, obviously in both arms and for the whole duration of the treatment.
Patients with histologically proven advanced melanoma were enrolled in the study between March 1st 1997 and December 31st 1999. Patient characteristics are listed in Table 1. Detailed analyses of these clinical characteristics have been reported previously [18].
Table 1.
Patient Characteristics
| CT | BioCT | |||
| No. | % | No. | % | |
| No. patients | 89 | 87 | ||
| Sex | ||||
| Male | 57 | 64.0 | 48 | 55.2 |
| Female | 32 | 36.0 | 39 | 44.8 |
| Age | ||||
| Median | 59 | 56 | ||
| Range | 26–76 | 25–77 | ||
| Performance status (ECOG) | ||||
| 0 | 60 | 67.4 | 59 | 67.8 |
| 1 | 23 | 25.8 | 24 | 27.6 |
| 2 | 6 | 6.7 | 4 | 4.6 |
| Site of primary melanoma | ||||
| Head and neck | 16 | 18.0 | 16 | 18.4 |
| Body | 35 | 39.3 | 36 | 41.4 |
| Arms | 34 | 38.2 | 34 | 39.1 |
| Not referred | 4 | 4.5 | 1 | 1.1 |
| Sites of disease | ||||
| Liver +/- others | 30 | 33.7 | 32 | 36.8 |
| Viscera +/- others | 29 | 32.6 | 31 | 35.6 |
| Bone + soft tissue and lymph nodes | 4 | 4.5 | 2 | 2.3 |
| Soft tissue and lymph nodes | 26 | 29.2 | 22 | 25.3 |
Before each cycle clinical examination, determination of complete blood count and biochemical analysis were performed; after every two cycles during therapy and every three months thereafter until progression, the patients received a chest CT-scan or x-ray, liver CT scan or ultrasonography examination.
All patients gave their informed written consent to receive treatment and the study was examined and approved by the Ethical committees of every Local Health and Social Service of each center included in the study in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki.
All patients were randomized to receive treatment with either chemotherapy (CT) or chemoimmunotherapy (bioCT). The treatment scheme used is the following: on day 1 all patients received 75 mg/m2 CDDP i.v. with the usual hydrating scheme, 800 mg/m2 DTIC i.v. and optionally 100 mg/m2 BCNU i.v.. The patients who were allocated in the bioCT arm received exactly the same regimen as the CT arm, with the addition of IL-2 and α-IFN as immunomodulants. The dose of IL-2 used was 4,500,000 IU given subcutaneously from day 3 to 5 and 8 to 12. α-IFN-2b was given intramuscularly at the dose of 3,000,000 U on days 3, 5 and then 3 times a week. The treatment was repeated every 21 days for six cycles or until progression or severe toxicity. After the sixth cycle, the bioCT arm patients continued to receive IL-2 and α-IFN alone up to the twelfth month or until progression or severe toxicity. Response evaluations and toxicity were assessed according to WHO criteria as previously reported [18].
Clinical and laboratory parameters
All patients were characterized according to some pre-treatment clinical and laboratory parameters. Basal clinical evaluations included performance status, age, sex, and site of disease (liver versus no liver disease).
Finally a panel of laboratory parameters were also evaluated before starting treatment and subsequently before each treatment cycle. Data showed in this paper refer to baseline evaluation only. Pre-treatment bio-humoral parameters included total leukocytes (normal range up to 8500 cells/mm3), eosinophils (normal range up to 4% of the total WBC) and lymphocytes (normal range 20%-40% of the total WBC), CRP (normal range up to 1.5 mg/dl), LDH (normal range, up to 460 U/L), erytrosedimentation rate (ESR) (normal range up to 20 mm), and fibrinogen (normal range, up to 450 mg/dl). CRP was assayed by a rate immunonephelometric technique on a protein system analyser; for fibrinogen a quantitative assay standardized photo-optical method was used; finally LDH determination was performed using a UV-assay standardized method.
Assessment of Clinical Response
Tumor sites were objectively evaluated by physical examination and radiologic tests after every two cycles of therapy and than every three months.
Standard definitions of complete and partial objective response were used, as previously reported (18). Survival was defined as the time interval between randomization and death of the patient for any cause or the last follow-up. Time to progression (TTP) was defined as the time interval between the date of randomization and the date of disease progression or last follow-up.
Statistical analysis
The overall survival (OS), objective response (OR), TTP, the toxicity profile, and quality of life (QoL) of patients were evaluated in the eligible "intention to treat" (ITT) population. Sample size was determined a priori in agreement to the primary end point of the randomised study. OS and TTP curves for the two arms were estimated by the Kaplan and Meier method and then compared using the Logrank test. As regards the response analysis, 95% confidence interval (95%CI) of response rate was calculated, and comparison between groups was assessed using Fisher's exact test.
As we only found a positive trend for bio-CT pts vs CT with no statistical significance in OR and OS, all analyses regarding the parameters considered are stratified by treatment arm. Univariate and multivariate analyses were performed. In multivariate analyses the Cox proportional hazards model was used to study the effects of different variables on survival. This model was carried out on 129 patients who had available all pre-treatment variables considered. Statistical significance was defined at P less than .05 for univariate and multivariate analyses.
Since patients with liver involvement have a very poor prognosis and in order to avoid a bias due to liver disease impact on the laboratory parameters evaluated in the study, we also considered this variable (liver disease yes or not). As the explorative intent of this analysis, no P values were adjusted for the multiplicity of the performed tests. All P values were based on two-sided testing and statistical analyses were carried out with SAS Statistical software (SAS/STAT User's Guide, version 6, SAS Institute, Cary NC, 1990).
Results
Survival and Response to treatment
A total of 178 patients were enrolled from 27 Italian centres; two of these patients were excluded from the study because they were not eligible and 176 patients were evaluable for the efficacy analysis.
Median follow-up was 18 and 16 months for the CT and bioCT groups respectively. Most relevant clinical results included a median survival time of 1.5 months longer for bioCT treated patients than for the CT group (11 vs 9.5 months), although no statistically significant difference was found between the two treatment arms (HR = 0.888, logrank = 0.442, p = 0.506). TTP was quite similar for the two arms with a median TTP of 3.6 months for the bioCT group and 3 months for CT treated patients (HR = 0.791, logrank = 2.216, p = 0.137); finally the response rate was 25.3% and 20.2 respectively.
Clinical parameters
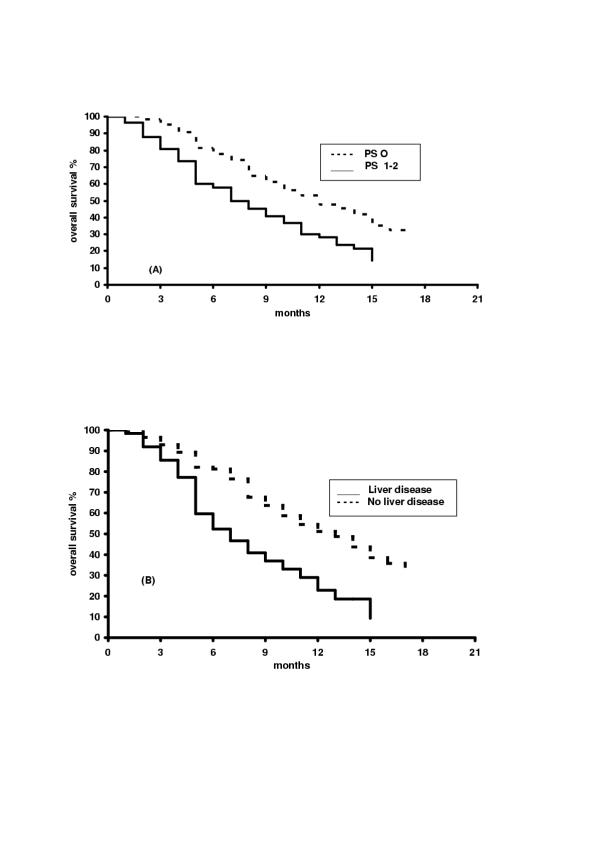
Among clinical parameters considered (age, sex, PS, presence or not of liver disease), only PS and liver disease were found to have an important impact on patient survival (Table 2). Patients with PS 0 had a median OS of 11.6 months compared with patients with PS 1–2 who had a median OS of 6.9 months (P=.001). The presence of liver disease had a stronger impact on patient survival with a median OS of 12 months for patients without liver disease with respect to 6.3 months in patients with liver disease (P < .0001) (Figure 1).
Table 2.
Univariate Survival Analysis According To Clinical Characteristics
| Clinical Variable | No. Of patients | Median Survival, Months (CI) | Odds Ratio | Log-Rank P |
| Liver Disease | ||||
| Yes | 114 | 12 (9.7–14.6) | 2.4 (1.64–3.53) | |
| No | 62 | 6.3 (4.8–8.6) | 0.0001 | |
| PS | ||||
| 0 | 119 | 1.6 (9.2–14.4) | 1.85 (1.27–2.67) | 0.001 |
| 1–2 | 57 | 6.9 (4.7–10.1) | ||
| Age | ||||
| <60 years | 99 | 9.2 (7.3–12.7) | 0.97 (0.7–1.4) | 0.85 |
| ≥ 60 years | 77 | 10.7 (8.2–13.2) | ||
| Sex | ||||
| Male | 105 | 9.3 (7.8–11) | 0.78 (0.54–1.12) | 0.178 |
| Female | 71 | 12 (7.9–14.6) |
Figure 1.
Kaplan-Meier survival curves according to PS (A) and presence or not of liver disease (B).
The patient age and sex did not influence both the overall response and survival.
Laboratory parameters
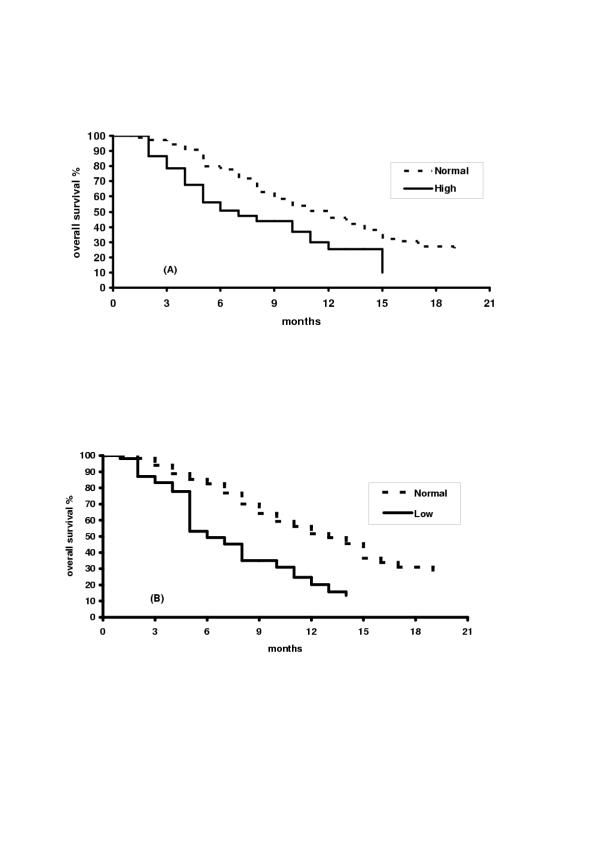
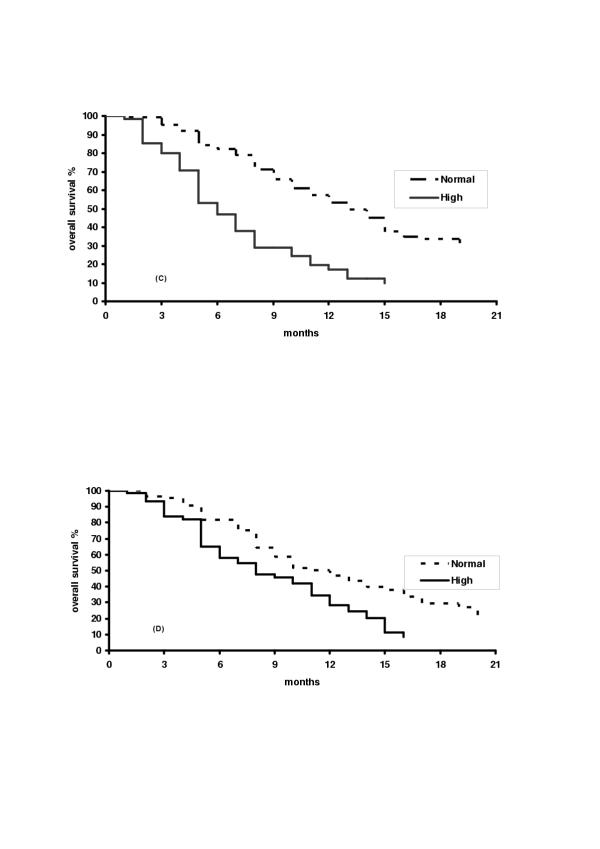
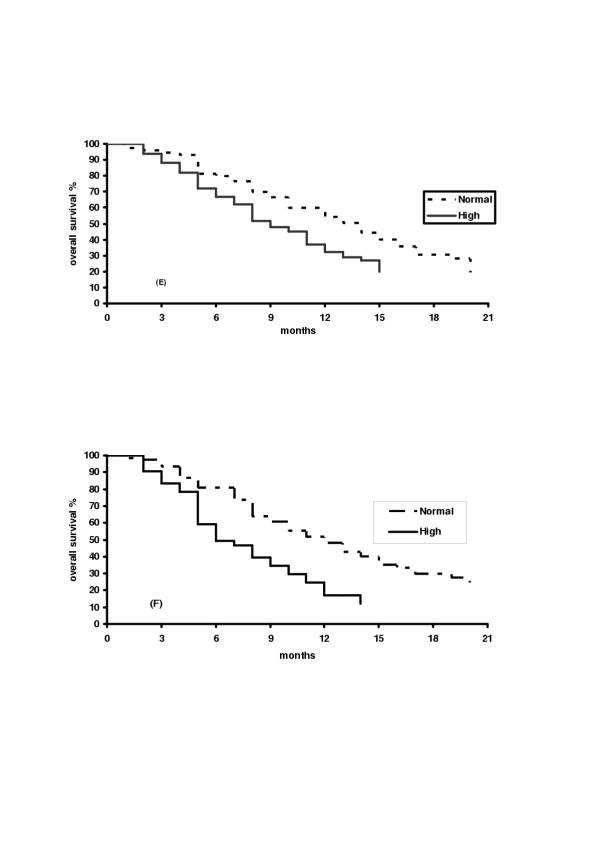
Regarding laboratory parameters, in univariate analysis, pretreatment higher value of lymphocytes (P=.004 for absolute lymphocyte count, and P < .0001 for the percentage count), lower value of CRP (P=.003), LDH (P < .0001), ESR (P=.02), fibrinogen (P < .0001) and WBC (P=.005) were related to a better survival (Table 3) (Figure 2). On the contrary, none of these factors was found to correlate with response. A multivariate analysis, using the Cox proportional hazards model, was carried out on 129 patients; in order to avoid a bias due to liver disease, we also considered this variable (liver disease yes/no). From an initial model, using a backward selection procedure, a final parsimonious model was obtained. Only fibrinogen (P=.0001), LDH (p=.009) and liver disease (P=.04) were found to have independent impact on survival (Table 4).
Table 3.
Univariate Survival Analysis According To Laboratory Parameters
| Laboratory Parameters | No. Of patients | Median Survival, Months (CI) | Odds Ratio | Log-Rank P |
| White Blood Count | ||||
| Normal | 137 | 12 (8.7–13.2) | 1.8 (1.18–2.8) | 0.0057 |
| High | 37 | 6 (4–10.5) | ||
| Lymphocytes | ||||
| Normal | 100 | 12 (9.5–14.8) | 1.67 (1.16–2.4) | 0.0049 |
| Low | 72 | 7.8 (6.5–10.1) | ||
| Lymphocytes (%) | ||||
| Normal | 118 | 9.1 (9.7–14.7) | 2.26 (1.5–3.3) | 0.0001 |
| Low | 54 | 5.4 (4.4–7.9) | ||
| Eosinofili | ||||
| Normal | 171 | 10 (8.2–11.9) | 1.82 (0.66–5.03) | 0.23 |
| High | 5 | 4.3 (3–15.2) | ||
| Eosinofili (%) | ||||
| Normal | 126 | 9.2 (7.8–11.6) | 0.77 (0.45–1.3) | 0.32 |
| High | 25 | 13.2 (9.5–15.4) | ||
| LDH | ||||
| Normal | 121 | 12.4 (10.5–14.6) | 2.77 (1.91–4.02) | 0.0001 |
| High | 55 | 5.4 (4.2–7) | ||
| CRP | ||||
| Normal | 84 | 10.7 (8.5–14.7) | 1.80 (1.2–2.67) | 0.0031 |
| High | 62 | 7.4 (5.1–10.4) | ||
| ESR | ||||
| Normal | 70 | 13.2 (9.5–15.5) | 1.57 (1.06–2.31) | 0.022 |
| High | 83 | 8.5 (7–10.7) | ||
| Fibrinogen | ||||
| Normal | 107 | 11.8 (9.2–14.3) | 2.37 (1.58–3.54) | 0.0001 |
| High | 42 | 5.4 (4.7–8.3) |
Figure 2.
Kaplan-Meier survival curves according to White Blood Count (A), Lymphocytes percentage (B).
Table 4.
Multivariate Survival Analysis According To Clinical and Laboratory Parameters.
| Variable | Hazard Ratio | IC 95% Hazard ratio | P |
| Liver Disease (yes vs no) | 1.68 | 1.025–2.75 | 0.04 |
| LDH (high vs normal) | 1.89 | 1.17–3.06 | 0.009 |
| Fibrinogen (high vs normal) | 1.99 | 1.24–3.19 | 0.004 |
Evaluated 129 pts (parameters considered: PS, liver disease, lymphocytes, LDH, ESR, PCR, Fibrinogen and WBC)
Discussion
Commonly used treatment options for MM patients have included chemotherapy alone or combined to immunotherapy. Unfortunately, these treatments are effective in only a minority of patients. Indeed, the prognosis for patients with metastatic melanoma still seems to be more influenced by disease caracteristics than any particular therapy.
Metanalyses carried out recently have demonstrated that the association of chemotherapy with immunotherapy including IL-2 and/or α-IFN, offers the highest response percentage and long-term survival rates in MM patients [19-21]. In our trial we only found a positive trend for bio-CT pts versus CT with no statistical significance in OR (25.3% vs 20.2%), TTP (3.6 vs. 3.0 months) and OS (11 vs 9.5 months).
Of interest is that some simple laboratory parameters such as LDH, Fibrinogen, CRP, albumin are able to predict survival behaviour, supplanting more complex or subjective factors, including sites of disease and patient PS [7,11].
Our analysis of potential prognostic factors confirmed the importance of some laboratory known unfavourable parameters (high LDH, ESR, CRP) and some clinical aspects (poor basal PS and the presence of liver disease). On the contrary, none of these factors was found correlated to response. Two interesting new aspects which emerged noticeably from this trial were the prognostic value of the basal number of lymphocytes and the fibrinogen level, which seem to be discriminating factors between a good or bad survival prognosis.
CRP is an acute-phase protein produced in the liver in response to cyokines such as IL-6. In vivo, CRP seems mainly to reflect IL-6 secretion [22] as supported by high correlation demonstrated between serum CRP and the IL-6 concentrations in melanoma patients [12]. Discordances observed in some studies between CRP and IL-6 concentration may be explained by differences in kinetics of secretion, since the increase of IL-6 is sometimes transient and occurs before CRP production. Also the action of other cytokines could explain the discordance of CRP/IL-6 levels [23,24]. Other Authors have also shown that elevated pretreatment values of a specific inflammatory markers, such as CRP and erythrosedimentation rate are frequent in advanced cancer patients with poor prognostic characteristics, such as cachexia [25]. Moreover, pretreatment high levels of CRP predicts lack of IL-2 activity on tumour objective response and its efficacy on overall survival in metastatic cancer patients [26]. However, these findings have not been confirmed by others [13,27].
The impact of pretreatment values of total lymphocytes and lymphocyte subsets in cancer patients remains questionable yet [14]. Lynphocytopenia [28] and/or a lower lynphocyte percentage [29,30] seem to be independent predictive factors for short survival in cancer patients, whereas a higher lymphocyte number is related to longer survival in patients with different neoplasms including lung cancer [28], colorectal cancer [31], gastric cancer [32].
In stage I-III melanoma patients, lower levels of total lymphocytes and of T-lymphocyte subset have been shown to have a negative prognostic value when compared to patients with normal values both in term of disease free survival and overall survival [33]. As known, lymphocytes play a fundamental role in mediating tumor cell destruction [34] and the rebound lymphocytosis represents the typical biomarker of immune activation to IL-2 immunotherapy [35]. In fact, a higher lymphocyte rebound has been observed after IL-2 therapy in responding patients with metastatic renal cell cancer [36,37] and metastatic melanoma [13]. In cancer patients receiving immunotherapy, the relative amount of CD4+, CD8+, and natural killer cells have been found to correlate with a better survival [14]. Moreover, it has been recently advanced that one of the underlying mechanisms responsible for the compromised host immune response, could in part be explained by a low production of endogenous IL-2 caused by a decreased number and/or functionality of lymphocytes [37,38].
Recently, fibrinogen has been reconsidered as an important determinant of the metastatic potential of tumor cells [17]. A specific association between human cancer and the hemostatic system has been recognized for more time. Many significant hemostatic abnormalities have been described in cancer patients including disseminated intravascular coagulation, hemorrhagic events, and migratory thrombophlebitis [39]. Many tumor cells possess strong procoagulant activities that promote the local activation of the coagulation cascade resulting in both the formation of tumor stroma and the promotion of hematogenous metastases. Fibrin matrices also promote neovascularization. Moreover, fibrin degradation products have also been shown to display powerful chemotactic, immune-modulatory, as well as angiogenic properties. Finally, the formation of platelet-fibrin-tumor aggregates may be causally related to endothelial adhesion and metastatic potential. The generation of viable mouse lines with selected deficits in key hemostatic factors has provided the opportunity to directly examine the role of fibrinogen in tumor progression and spread. Using fibrinogen-deficient and plasminogen-deficient transgenic mice and transplantable murine tumor cell lines, it has been demonstrated that fibrinogen deficiency strongly diminished the metastatic capability of tumor cells with a significant reduction in the number of surface pulmonary metastases, although fibrinogen deficiency did not reduce the growth rate of transplanted tumor cells [17]. This indicates that initial establishment of metastatic foci, but not tumor growth itself, was impaired in fibrinogen-deficient mice.
Moreover, many detailed experimental in vitro studies have demonstrated that melanoma cells with a highly metastatic potential are able to utilize the host hemostatic system for protection against the host immune system using a covalent attachment to fibrinogen, either directly or after its conversion into fibrin [16]. Interestingly, cytotoxicity experiments showed that the fibrinogen coating on melanoma cells provided protection against LAK-cell-induced lysis and that brief trypsinization restored the susceptibility of the cells to lysis, due to removal of the fibrinogen coating [15,16].
Lee et al [40] studied the role of fibrinogen covalently associated with cell membrane in blood-borne lung tumor colony formation of murine mammary carcinoma cells in mice. Interestingly, in mice with hyperfibrinogenemia, induced by prednisolone administration or fibrinogen infusion of syngeneic mice, the coagulation time was significantly accelerated and the number of lung tumor colonies significantly increased. On the contrary, low fibrinogen levels induced by rabbit antisyngenic mouse fibrinogen immunoglobulins or heparin infusion, markedly delayed coagulation time and reduced the numbers of blood-borne lung tumor colonies of the tumor cells. Also these Authors reported that the fibrinogen coating on tumor cells provides protection against LAK-cell-induced lysis. These observations could have potential implications for tumor metastasis studies and therapeutic approaches, in particular when immunologic strategies are used.
In conclusion, patient prognostic subgroups and the different treatments they should receive could be better identified on the basis of proven predictive factors. This prospect might change if or when innovative therapeutic strategies and different therapeutic options are available.
In summary, the current study represents one of the largest single experience regarding prognostic factors in MM patients. Our findings carried out in 176 consecutive MM patients homogeneously treated in a single trial with chemo or bio-chemotherapy, confirm that some laboratory and clinical factors are strongly related to survival in MM patients, and they introduce a new simple laboratory parameter, the fibrinogen, that could be utilized to better identify patients with different prognosis.
Figure 3.
Kaplan-Meier survival curves according to LDH (C), CRP (D).
Figure 4.
Kaplan-Meier survival curves according to ESR (E), Fibrinogen (F).
Acknowledgments
Acknowledgments
We thank IMI participants and authors (Laura Ridolfi, Department of Medical Oncology, Pierantoni Hospital, Forlì; Roberta Redelotti, Grazia Artioli, Department of Medical Oncology, Busonera Hospital, Padua; Vito Lorusso, Department of Medical Oncology, Oncology Institute of Bari, Bari; Lucia Tanganelli, 4 Medical Oncology Unit, S. Chiara Hospital, Pisa; Paola Poletti, Medical Oncology Unit, Riuniti Hospital, Bergamo; Stella Porrozzi, Enrichetta Corgna, Medical Oncology Unit, Monteluce Polyclinic, Perugia; Giuseppe Lo Presti, Carmelo Iacono, Department of Medical Oncology, Ragusa Hospital, Ragusa; Anna Chiara, Giovanna Luchena, Medical Oncology Center, Sant'Anna Hospital, Como; Elvira Scelzi, Paolo Manente, Medical Oncology Unit, S. Giacomo Apostolo Hospital, Castelfranco Veneto; Laura Scaltriti, Fabrizio Artioli, Oncology Outpatient Clinic, B. Ramazzini Hospital, Carpi (Modena); Sergio Palmeri, Salvatore Miceli, Department of Medical Oncology and Oncohematology, University of Palermo, Palermo; Antonio Muggiano, Department of Medical Oncology, A. Businco Hospital, Cagliari; Sergio Montanara, Sergio Cozzi, Department of Oncology, Castelli Hospital, Verbania; Franca Pari, Enrico Aitini, Department of Medical Oncology and Hematology, Mantova; Vittorio Mascia, Daniele Farci, Department of Medical Oncology III, A. Businco Hospital, Cagliari; Angelo Gambi, Maria Cristina Cappelli, Oncology Unit, per gli Infermi Hospital, Faenza; Domenico De Toma, Anna Giacobone, Oncology I, Polyclinic Institute San Donato Milanese, Milan; Maurizio Bertuccelli, Oncology Center, Riuniti Hospital, Livorno; Guido Biasco, Simona Casadei, Institute of Hematology and Medical Oncology, University of Bologna, Bologna; Salvatore Toma, Department of Oncology, Biology and Genetics, University of Genoa, National Institute for Cancer Research, Genoa) for their partecipation to the study and Silvana Valerio for her technical assistance in the preparation of this manuscript.
Contributor Information
Michele Guida, Email: micguida@libero.it.
Alessandra Ravaioli, Email: a.ravaioli@ausl.fo.it.
Vanna Chiarion Sileni, Email: mgaliz@tiscalinet.it.
Antonella Romanini, Email: a.romanini@med.unipi.it.
Roberto Labianca, Email: labianca@libero.it.
Antonio Freschi, Email: freschi@libero.it.
Salvatore Brugnara, Email: brugnara@libero.it.
Addolorata Casamassima, Email: a.casamassima@oncologico.bari.it.
Vito Lorusso, Email: vitolorusso@inwind.it.
Oriana Nanni, Email: o.nanni@ausl.fo.it.
Ruggero Ridolfi, Email: r.ridolfi@ausl.fo.it.
the Italian Melanoma Intergroup (IMI), Email: micguida@libero.it.
References
- Parker SL, Tong T, Bolden S, et al. Cancer statistics 1996. CA Cancer J Clin. 1996;46:5–25. doi: 10.3322/canjclin.46.1.5. [DOI] [PubMed] [Google Scholar]
- Greenlee RT, Hill-Harmon MB, Murray T, et al. Cancer statistics, 2001. CA Cancer J Clin. 2001;51:15–36. doi: 10.3322/canjclin.51.1.15. [DOI] [PubMed] [Google Scholar]
- Eton O, Legha SS, Bedikian AY, et al. Sequential biochemotherapy versus chemotherapy for metastatic melanoma: results from a phase III randomized trial. J Clin Oncol. 2002;20:2045–2052. doi: 10.1200/JCO.2002.07.044. [DOI] [PubMed] [Google Scholar]
- Rosenberg SA, Yang JC, Schwrtzentruber DJ, et al. Prospective randomised trial of the treatment of patients with metastatic melanoma using chemotherapy with cisplatin, dacarbazine, and tamoxifene alone or in combination with interleukin-2 and interferonalpha-2b. J Clin Oncol. 1999;17:968–975. doi: 10.1200/JCO.1999.17.3.968. [DOI] [PubMed] [Google Scholar]
- Balch C, Buzaid AC, Soong SJ, et al. Final version of the AJCC staying system for cutaneous melanoma. J Clin Onc. 2001;19:3635–3649. doi: 10.1200/JCO.2001.19.16.3635. [DOI] [PubMed] [Google Scholar]
- Balch CM, Soong S, Shaw HM, et al. An analysis of prognostic factors in 8500 patients with cutaneous melanoma. In: Balch CM, Houghton AN, Milton GW, editor. in: Cutaneous Melanoma. 2. Philadelphia. PA. Lippincott; 1992. pp. 180–186. [Google Scholar]
- Sirott MN, Bajorin DF, Wong GYC, et al. Prognostic factors in patients with metastatic melanoma: A multivvariate analysis. Cancer. 1993;73:3091–3098. doi: 10.1002/1097-0142(19931115)72:10<3091::aid-cncr2820721034>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- Keilholz U, Scheibenbogen C, Sommer M, et al. Prognostic factors for response and survival in patients with metastatic melanoma receiving immunothrapy. Mel Res. 1996;6:173–178. doi: 10.1097/00008390-199604000-00013. [DOI] [PubMed] [Google Scholar]
- Manola J, Atkins M, Ibrahim J, Kirkwood J. Prognostic factors in metastatic melanoma: a pooled analysis of Eastern Cooperative Oncology Group trials. J Clin Oncol. 2000;15:18–22. doi: 10.1200/JCO.2000.18.22.3782. [DOI] [PubMed] [Google Scholar]
- Ryan L, Kramar A, Borden E. Prognostic factors in metastatic melanoma. Cancer. 1993;71:2995–3005. doi: 10.1002/1097-0142(19930515)71:10<2995::aid-cncr2820711018>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- Eton O, Legha SS, Moon TE, et al. Prognostic factors for survival of patients treated systemically for disseminated melanoma. J Clin Oncol. 1998;16:1103–1111. doi: 10.1200/JCO.1998.16.3.1103. [DOI] [PubMed] [Google Scholar]
- Tartour E, Blay JY, Dorval T, et al. Predictors of clinical response to interleukin-2-based immunotherapy in melanoma patients: A French multiinstitutional study. J Clin Oncol. 1996;14:1697–1703. doi: 10.1200/JCO.1996.14.5.1697. [DOI] [PubMed] [Google Scholar]
- Phan GP, Attia P, Steinberg SM, et al. Factors associated with response to high-dose interleukin-2 in patients with metastatic melanoma. J Clin Oncol. 2001;19:3477–3482. doi: 10.1200/JCO.2001.19.15.3477. [DOI] [PubMed] [Google Scholar]
- Hernberg M. lymphocyte subsets as prognostic markers for cancer patients receiving immunomodulative therapy. Med Oncol. 1999;16:145–153. doi: 10.1007/BF02906126. [DOI] [PubMed] [Google Scholar]
- Gunji Y, Gorelik E. Role of fibrin coagulation in protection of murine tumor cells from destruction by cytotoxic cells. Cancer Res. 1988;48:5216–5221. [PubMed] [Google Scholar]
- Cardinali M, Uchini R, Chung SI. Interaction of fibrinogen with murine melanoma cells: covalent association with cell membranes and protection against recognition by lymphokine activated killer cells. Cancer Res. 1990;50:8010–8016. [PubMed] [Google Scholar]
- Palumbo JS, Kombrinck KV, Drew AF, et al. Fibrinogen is an important determinant of the metastatic potential of circulating tumor cells. Blood. 2000;96:3302–3309. [PubMed] [Google Scholar]
- Ridolfi R, Chiaron-Sileni V, Guida M, et al. Cisplatin, dacarbazine with or without subcutaneous interleukin-2 and alfa interferon phase III randomized trial: results of an Italian multicentric study in advanced melanoma out-patients. J Clin Onc. 2002;20:1600–1607. doi: 10.1200/JCO.20.6.1600. [DOI] [PubMed] [Google Scholar]
- Allen IE, Kupelnick B, Kumashiro M. Efficacy of interleukin-2 in the treatment of metastatic melanoma-systemic review and metastasis-analysis. Cancer Ther. 1998;1:168–173. [Google Scholar]
- Keilholz U, Conradt C, Legha SS. Results of interleukin-2-based treatment in advanced melanoma: A case record-base analysis of 631 patients. J Clin Oncol. 1998;16:2921–2929. doi: 10.1200/JCO.1998.16.9.2921. [DOI] [PubMed] [Google Scholar]
- Huncharek M, Caubet JF, McGarry R'01. Single-agent DTIC versus combination chemotherapy with or without immunotherapy in metastatic melanoma: a meta-analysis of 3273 patients from 20 randomized trials. Melanoma Res. 2001;11:75–81. doi: 10.1097/00008390-200102000-00009. [DOI] [PubMed] [Google Scholar]
- Klein B, Wijdenes J, Zhang XG, et al. Murine anti-interleukin 6 monoclonal antibody therapy in myeloma. Blood. 1991;78:1198–1204. [PubMed] [Google Scholar]
- Baumann H, Gauldie J. The acute phase response. Immunol Today. 1994;15:74–80. doi: 10.1016/0167-5699(94)90137-6. [DOI] [PubMed] [Google Scholar]
- Gogard A, Fauchet F, Raher S, et al. Generation of monoclonal antibodies against HILDA/LIF and their use in the quantitative assay of the cytokine. Cytokine. 1993;5:16–23. doi: 10.1016/1043-4666(93)90019-2. [DOI] [PubMed] [Google Scholar]
- Scott HR, McMillan DC, Crilly A, et al. The relationship between weight loss and interleukin-6 in non-small cell lung cancer. Br J Cancer. 1996;73:1560–1562. doi: 10.1038/bjc.1996.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blay JY, Negrier S, Combaret V, et al. Serum level of interleukin 6 as a prognosis factor in metastatic renal cell carcinoma. Cancer Res. 1992;52:3317–3322. [PubMed] [Google Scholar]
- Walther MM, Johnson B, Culley D, et al. Serum interleukin-6 levels in metastatic renal cell carcinoma before treatment with interleukin-2 correlates with paraneoplastic syndromes but not patient survival. J Urol. 1998;159:718–722. [PubMed] [Google Scholar]
- Stanley KE. Prognostic factors for survival in patients with inoperable lung cancer. J Natl Cancer Inst. 1980;65:25–32. [PubMed] [Google Scholar]
- Riesco A. Five-year cancer cure: relation to total amount of peripheral lymphocyles and neutrophils. Cancer. 1970;25:135–140. doi: 10.1002/1097-0142(197001)25:1<135::aid-cncr2820250120>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- Maltoni M, Pirovano M, Nanni O, et al. Biological indices predictive of survival in 519 italian terminally ill cancer patients. J Paain Symptom Manage. 1997;13:1–9. doi: 10.1016/S0885-3924(96)00265-5. [DOI] [PubMed] [Google Scholar]
- Kim US, Papatestas AE, Aufses AH. Prognostic significance of peripheral lymphocyte counts and carcinoembryonic antigens in colorectal carcinoma. J Surg Oncol. 1976;8:257–62. doi: 10.1002/jso.2930080312. [DOI] [PubMed] [Google Scholar]
- Lavin P, Bruckner HW, Plaxe SC. Studies in prognostic factors relating to chemotherapy for advanced gastric cancer. Cancer. 1982;50:2016–2023. doi: 10.1002/1097-0142(19821115)50:10<2016::aid-cncr2820501007>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- Bernengo MG, Lisa F, Meregalli M, et al. The prognostic value of T-lymphocyte levels in malignant melanoma. A five year follow-up. Cancer. 1983;52:1841–1848. doi: 10.1002/1097-0142(19831115)52:10<1841::aid-cncr2820521014>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- Grimm EA, Mazumder A, Zhang HZ, Rosenberg SA. Lyinphokine-activated killer cell phenomenon. J Exp Med. 1982;155:1823–1841. doi: 10.1084/jem.155.6.1823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmer PA, Atzpodien J, Philip T, Negrier S, et al. A comparison of 2 modes of administration of rIL-2: continuous intravenous infusion alone versus subcutaneous administration plus IFN-a in patients with advanced renal cell carcinoma. Cancer Biother. 1993;8:123–136. doi: 10.1089/cbr.1993.8.123. [DOI] [PubMed] [Google Scholar]
- Gohring B, Riemann D, Rebmann U, et al. Prognostic value of immunomonitoring of patients with renal cell carcinoma under therapy with IL-2/IFN-alpha in combination with 5-FU. Urol Res. 1996;24:297–3031. doi: 10.1007/BF00304780. [DOI] [PubMed] [Google Scholar]
- Fumagalli L, Lissoni P, Di Felice G, et al. Pretreatment serum markers and lymphocyte response to interleukin-2 therapy. Brit J Cancer. 1999;80:407–411. doi: 10.1038/sj.bjc.6690371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monson JRT, Ramsden C, Guillou PJ. Decreased IL-2 production in patients with gastrointestinal cancer. Br J Surg. 1986;73:483–486. doi: 10.1002/bjs.1800730620. [DOI] [PubMed] [Google Scholar]
- Dvorak HF. Thombosis and cancer. Hum Pathol. 1987;18:275–281. doi: 10.1016/s0046-8177(87)80010-2. [DOI] [PubMed] [Google Scholar]
- Lee SY, Park LO, Suk SH. role of fibrinogen covalently associated with cell membrane in blood-borne lung tumor colony formation of murine mammary carcinoma cells. Oncology. 2000;59:238–244. doi: 10.1159/000012167. [DOI] [PubMed] [Google Scholar]