Abstract
The control of HIV and other sexually transmitted infections (STI) is a challenge in China, with female sex workers (FSW) and male clients suspected as bridge groups. This study used a 2006 national probability survey of 2,707 adult men. Among men 15–49 years old, the prevalence of FSW contacts last year was 4.2% (95% CI, 3.3–5.2) overall, with 7.2% (CI, 5.9–8.7) in urban and 1.8% (CI, 1.0–3.3) in rural areas. In urban areas, the men most at risk for FSW were high income, often traveled, engaged in business entertaining, ages 25–39, and had early sex histories. When compared to men with only wife or stable sex partner, those most likely to report STI last year also reported FSW sex of any type (aOR,13.10; CI, 5.87–29.42). Additionally, when compared to men reporting consistent condom use with FSW, men with inconsistent condom use had elevated STI (aOR, 3.71; CI, 1.18–11.66). Additional efforts are needed for high income men in urban areas, and on consistent condom use with FSW.
The control of human immunodeficiency virus (HIV) infection and other sexually transmitted infections (STIs) is a significant challenge in China, with infection increasingly transmitted through heterosexual contact, including wives infected by husbands who visit female sex workers (FSWs) [1, 2]. Biomarker studies among FSW clients have found the prevalence of HIV infection to be as high as 6.0% and that of STIs to be as high as 23% [1, 3–7]. Information about national levels of infection and significant risk groups is limited by a scarcity of studies, many of which are based on convenience samples [3–7]. Some descriptive studies suggest high risk among high-income men, including those who use sex for business networking [8–10]. Other studies have examined higher risks among rural-to-urban migrant men [11, 12]. The risk for other types of partners remains uncertain. This study moves toward firmer answers for some of these questions with the use of a 2006 nationally representative survey of adult men.
DATA AND METHODS
Sample
The 2006 Sexuality Survey of China used a stratified, multistage cluster sample [13]. In each of the urban and rural strata, official administrative units were selected with probability proportional to size, in which larger administrative units were more likely to be picked on the basis of a random number generator. Sampling proceeded through the following stages: (1) In the urban stratum, 75 primary sampling units (PSUs) were selected from a list that included all urban districts (in larger cities) as well as whole towns and small cities. From all rural counties, 47 counties were picked. (2) A single administrative neighborhood (jiedao) was selected from each urban PSU and a single administrative subunit, be it township (xiang) or town (zhen), was selected from each rural PSU. (3) Two resident’s committees (juwei hui) were selected from each urban neighborhood and one village (cun) level unit was selected from each township/town. (4) At the lowest level, individuals 18–60 years old from the local household register (for both permanent and temporary residents) were listed. In urban neighborhoods lacking a complete register of migrants, the list of residents was supplemented by local registration officials providing both an estimate of the number of unregistered migrants and sites (peddlers, small stores, and construction sites) where migrants worked. These sites were enumerated by the survey team and then added to list of residents. This complete list was sampled by using a random number generator to pick a starting point and then picking every nth person after that point (with the nth gap chosen to produce the requisite number of eligible persons for that locale).
Participants were interviewed not at home but in a nearby meeting place—hotel, school, or neighborhood office—with family members absent. The questionnaire was in a laptop computer, with a same-sex interviewer initially controlling the computer and then the participant controlling the computer during the last, more sensitive part of the interview. In urban areas, the proportions of men who needed help in using the computer during the sensitive portion of the questionnaire were as follows: never, 54%; sometimes, 42%; and constantly, 4%. In rural areas, these percentages were 40%, 50%, and 11%, respectively. The study procedures were approved by a Renmin University human subjects committee, and participants gave informed consent prior to beginning the interview.
In the initial sample of 10 203 individuals, 2650 (26%) could not be found at the address where they were registered, leaving 7553 individuals who had the potential to be interviewed. Excluding refusals, temporary absences, computer glitches, and faked interviews, 5404 interviews were completed and available for analysis. Or, compared with the 7553 individuals who could potentially be interviewed, the response rate was 71.5%.
Some questions were not answered because of a few participants breaking off the interview before getting to questions near the end of the interview, because of computer glitches, or because of errors in data cleaning. The implications for analysis samples were as follows: First, the cross-national analysis sample for all men 18–49 years of age was reduced from an initial 2231 men to 2222 men. Second, through deletion of observations that lacked information on either outcomes or risk factors, the sample of urban men 18–60 years of age was reduced from an initial 2079 men to 2066 men in the analysis of risk factors for FSW visits and to 2068 men for the analysis of risk factors for STIs.
Weighting and Analysis
Except where raw numbers are indicated, all results were adjusted both by population weights and by corrections for the effects of clustered sampling by use of the svy procedures in Stata statistical software (version 11.2) [14]: (1) Population (sampling) weights were the inverse of the probability that this observation was included in the sample. These weights were produced by first calculating the number of people in cells produced by the intersection of age, sex, and urban or rural residence, starting with the total population in the census and then for the effective sample. Then, the numbers in the census cells were divided by the numbers in the sample cells to yield population weights. (2) To adjust for additional variability introduced at the first stage of selecting a modest number of PSUs, the analysis used Huber–White corrections [15].
In the analysis of risk factors, the adjusted odds ratio (aOR) column was derived from a multivariate equation (constant not shown) that included the effects of all the other risk factors in the same equation. The selection of risk factors was guided by the literature on high-income men who travel and entertain [8–10] and the literature on rural-to-urban migrants [11, 12]. The organization of risk factors was influenced by the literature on conditions encouraging infidelity and other forms of risky sexual behavior, including freedom from surveillance and early sexual experiences (eg, premarital sex) [16, 17].
Measures
Two outcome measures were asked in the self-administered part of the questionnaire: (1) commercial sex and (2) STI. Commercial sex was defined as paid sex with a FSW, excluding sex merely in exchange for gifts or favors. The precise question was about sex (even if only oral sex or a so-called hand job) with a “Miss” (xiaojie)—slang for a prostitute—with the initial question about “Miss” adding prostitute (jinu) in parentheses. The occurrence of STI was based on self-reports that a doctor had told a man that he had syphilis, gonorrhea, chlamydia, and/or genital herpes during the past 12 months; STI was coded 1 for any infection and 0 for none.
Risk factors included 4 items from the self-administered part of the questionnaire: (1) masturbation that had begun by age 17 years, (2) premarital sex, (3) type of partner, and (4) consistent condom use. Masturbation that had begun by age 17 was coded 1 if the participant reported (near the end of the interview) an age of first masturbation that was ≤17 years. Premarital sex was coded 1 if a man reported any sexual experience before his first marriage or, if never married, any sexual experience ever. Otherwise, it was coded 0. Type of partner in the past 12 months was determined from a series of questions about types of sexual partners, producing a summary typology of commercial partner, short-term partner, spouse or stable partner, and none. Short-term partners were for nonmarital relationships that lasted <6 months. Nonmarital stable partnerships were for nonmarital relationships, including cohabiting and other sexual relationships that had lasted for at least 6 months. If a man reported more than one type of relationship during the year, the riskiest (most likely to have STI) was coded. Consistent condom use was determined from questions about condom use with sex workers during the previous year.
Risk factors that were not self-administered included the following: (1) travel for at least 1 week during the past year, (2) social life, (3) migration, (4) income, and (5) occupation. Travel for at least 1 week during the past year was determined from the question, “During the past 12 months, regardless of reason, how many days did you leave home and travel on your own? (Only overnight stays count.)” Social life (without regular partner) more than monthly was determined from the question, “During the past 12 months, how often did you participate in social activities (shehui jiaowang huodong) outside work? (Including social/business activities, parties, visiting friends, group traveling, etc, but excluding activities with family or relatives.)” Migration (rural-to-urban without urban registration) was determined from items asking urban residents where they lived at age 14 years and the location of their official household registration (hukou), an internal passport system. Income was the participant’s own monthly income during the past year. Occupation was one’s current occupation, with a division between managers or owners of larger enterprises and self-employed individuals (geti hu) who worked alone or by hiring no more than 7 workers.
Other Countries
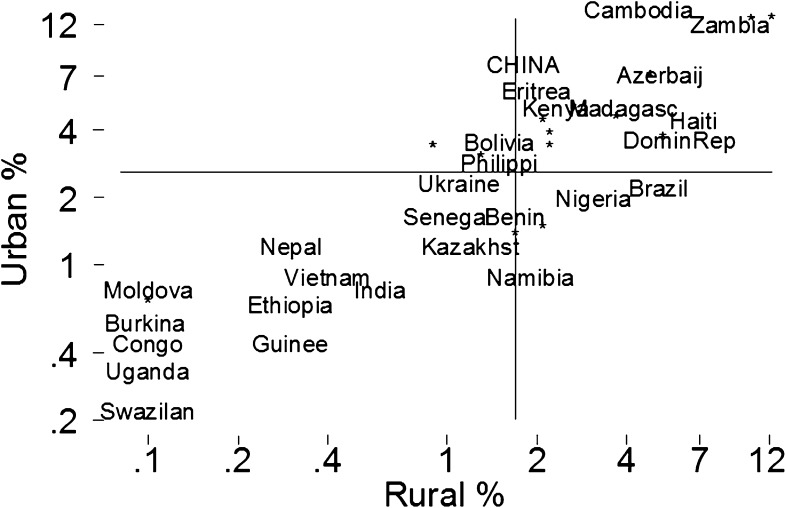
Comparisons to other countries were made for paid (not just gifts and favors) sex with a dedicated sex worker (prostitute) among men aged 15–49 years in the most recent survey for each country, with a median survey date of 2003 [18–20]. In addition to the countries with separate urban and rural statistics reported in Figure 1, data included the national data for Australia, France, Greece, Italy, the Netherlands, Norway, Portugal, Singapore, Spain, Switzerland, Thailand, and the United Kingdom. To make the Chinese sample of men more comparable with those of the other countries, the Chinese averages for men age aged 18–49 years were recalculated for a hypothetical age range of 15–49 years, using the assumption that unobserved Chinese men aged 15–17 years had no commercial sex in the previous 12 months.
Figure 1.
Percentage of men aged 15–49 years reporting commercial sex during the past 12 months. Axes are on a logarithmic scale. Solid lines indicate the median percentage for each axis. For readability, the following 14 countries are identified only by asterisks, in descending order on the rural axis: Mozambique, Tanzania, Malawi, Togo, Zimbabwe, Liberia, Uzbekistan, Cameroon, Armenia, Ghana, Mali, Botswana, Chad, and Rwanda [18, 19]. Chinese data are from the 2006 Sexuality Survey of China.
RESULTS
Descriptive Statistics
Lifetime Commercial Sex.
Among men aged 18–49 years, the percentages reporting that they had commercial sex at least once during their lifetimes were 6.9% nationally, with 10.1% urban and 4.4% rural. Among 185 men reporting lifetime commercial sex, the unadjusted median time of onset was 27 years, with a 25th–75th percentile range of 23–33 years.
Frequency and Cost.
Among the 139 men reporting payment at the last visit (some of which occurred >1 year ago), prices for commercial sex ranged from a few yuan to >1000 yuan, with a median price of 100 yuan (US $13 in 2006). This median payment was 10% (95% confidence interval [CI], 3%–36%) of the monthly income of gainfully employed men. Among the 120 urban men 18–49 years old reporting commercial sex in the past year, the number of sex worker visits during the year were distributed as follows: 1 visit, 25% of men, 2–3 visits, 26% of men, 4–6 visits, 27% of men, and 7–60 visits, 21% of men.
Prevalence in Past 12 Months.
For men 15–49 years old, the estimated rural prevalence of Chinese men’s commercial sex of 1.8% was near the median for rural areas in other countries (Figure 1, horizontal axis). In contrast, China’s estimated urban prevalence of 7.2% was greater than the urban median of other countries (Figure 1, vertical axis) and was exceeded by that of only 4 countries (Cambodia, Zambia, Mozambique, and Tanzania) with urban data.
The addition of CIs (Table 1) shows that China’s rural CI overlapped the rural median of other societies. China’s CIs for both urban and national data exceeded the median levels for other countries. For example, in national level statistics, China’s median prevalence of 4.2% (95% CI, 3.5%–5.2%) exceeded the median of 2.4% among 55 other countries.
Table 1.
Prevalence of Male Commercial Sex During the Past 12 Months
| Group level | China |
Other countries |
||
| No. of participants (prevalence) | 95% CI | No. of countries (prevalence in median country) | IQR | |
| National | 2222 (4.2) | 3.3–5.2 | 55 (2.4) | 1.1–4.6 |
| Urban | 1728 (7.2) | 5.9–8.7 | 42 (2.6) | 0.8–4.0 |
| Rural | 494 (1.8) | 1.0–3.3 | 41 (1.7) | 0.6–3.9 |
For men aged 15–49 years, including sexually inactive men [18, 20]. Chinese data are from the 2006 Sexuality Survey of China; see the text for the calculations. Prevalence, % of men reporting commercial sex in past 12 months.Abbreviations:CI, confidence interval; IQR, interquartile range (25th–75th percentile).
Risk Factors
Commercial Sex.
The remaining analysis was based on the higher-prevalence urban sample and on the full sample age range of 18–60 years (Table 2). Several risk factors stood out in the initial descriptive analysis, including premarital sex (13.0%), regular social life without spouse (12.4%), high income (12.5%), being an enterprise manager or owner (29.7%), cohabitation (15.2%), and age of 25–39 years (10.9%). In the final multivariate analysis, 3 groups of risk factors stood out, namely, sexual history (eg, aOR for premarital sex, 2.93), the additional opportunities provided by income (aOR for the highest income group, 2.03), the occupation of manager or owner (aOR, 3.03), and the opportunities provided by an active social life outside the home (aOR, 2.12).
Table 2.
Commercial Sex in the Past 12 Months and Risk Factors Among Urban Men Aged 18–60 Years
| Risk factors | No. of participants with commercial sex/total no. of participants (weighted %) (N = 2066) | OR (95% CI) | aOR (95% CI) |
| All participants | 143/2066 (6.8) | ||
| Sexual history | |||
| Masturbation began by age 17 | |||
| Yes | 71/727 (9.6) | 1.92 (1.30–2.82)a | 1.81 (1.22–2.70)a |
| No | 72/1339 (5.3) | ||
| Premarital sex (before first marriage) | |||
| Yes | 95/719 (13.0) | 3.98 (2.78–5.68)a | 2.93 (2.01–4.28)a |
| No | 48/1347 (3.6) | ||
| Opportunity, surveillance relaxed | |||
| Travel for at least 1 week during the year (without regular partner) | |||
| Yes | 72/671 (10.7) | 2.28 (1.51–3.44)a | 1.62 (1.03–2.55)a |
| No | 71/1395 (5.0) | ||
| Social life (without regular partner) | |||
| More than monthy | 77/622 (12.4) | 3.03 (2.04–4.51)a | 2.12 (1.36–3.32)a |
| Monthly or less | 66/1444 (4.4) | ||
| Migrant status (rural-to-urban without urban registration) | |||
| Yes | 20/289 (6.9) | 1.01 (0.59–1.73) | 0.97 (0.47–1.98) |
| No | 123/1777 (6.8) | ||
| Opportunity, resources and work | |||
| Income, amount per month | |||
| 1500 rmb (US $180 or more) | 71/564 (12.5) | 5.72 (2.75–11.88)a | 2.03 (1.03–4.00)a |
| 1000–1499 rmb (US $120–$180) | 38/530 (7.1) | 3.08 (1.49–6.36)a | 1.63 (0.88–3.04) |
| 500–999 rmb (US $60–$120) | 22/497 (4.3) | 1.81 (0.87–3.75) | 1.12 (0.59–2.13) |
| 0–499 rmb (reference) | 12/475 (2.4) | 1.00 | 1.00 |
| Occupation | |||
| Administrator (government, etc) | 1/38 (2.3) | 0.47 (0.06–3.90) | 0.27 (0.03–2.15) |
| Manager or owner (enterprise) | 18/60 (29.7) | 8.28 (3.59–19.12)a | 3.31 (1.34–8.14)a |
| Professional or technical | 14/108 (13.3) | 3.01 (1.51–6.02)a | 1.86 (0.85–4.04) |
| Clerical | 26/328 (7.8) | 1.67 (0.86–3.23) | 1.13 (0.52–2.47) |
| Sales or service | 23/285 (7.9) | 1.68 (0.89–3.15) | 1.43 (0.72–2.85) |
| Self-employed (with ≤7 workers) | 28/343 (8.4) | 1.79 (0.94–3.40) | 1.12 (0.56–2.26) |
| Manual labor (reference) | 18/380 (4.8) | 1.00 | 1.00 |
| Farmer | 1/29 (3.2) | 0.64 (0.12–3.41) | 0.81 (0.14–4.84) |
| Other | 4/69 (5.8) | 1.20 (0.47–3.08) | 0.65 (0.25–1.71) |
| Not working (including students) | 10/426 (2.2) | 0.44 (0.17–1.14) | 0.89 (0.29–2.69) |
| Demographic information | |||
| Marital status | |||
| Single (includes virgins) | 18/415 (4.1) | 0.57 (0.34–0.94)a | 0.83 (0.42–1.65) |
| Cohabiting | 13/86 (15.2) | 2.41 (1.19–4.90)a | 1.31 (0.55–3.13) |
| Married (reference) | 99/1421 (6.9) | 1.00 | 1.00 |
| Remarried | 6/54 (10.6) | 1.60 (0.66–3.88) | 1.96 (0.81–4.73) |
| Divorced or widowed | 7/90 (7.2) | 1.04 (0.48–2.25) | 1.29 (0.57–2.90) |
| Age, years | |||
| 18–25 | 15/386 (3.9) | 0.70 (0.30–1.62) | 0.45 (0.16–1.33) |
| 26–39 | 92/839 (11.0) | 3.28 (1.82–5.91)a | 1.58 (0.73–3.38) |
| 40–49 | 27/501 (5.7) | 1.62 (0.81–3.21) | 1.22 (0.56–2.65) |
| 50–60 (reference) | 9/340 (2.4) | 1.00 | 1.00 |
The total number and number of participants with commercial sex are for numbers of observations. The adjusted odds ratio (aOR) includes the effects of all risk factors in the column.
Abbreviations: CI, confidence interval; OR, odds ratio; rmb, Chinese renminbi currency.
P < .05.
A check was performed on the robustness of our results. Some young never-married men were coded as having premarital sex only because they had commercial sex, thereby artificially inflating the premarital sex relationship to commercial sex. When this artifact was removed by restricting the analysis to men who were no longer single (either ever married or living with a cohabiting partner), the aOR for the final equation was smaller but still robust (aOR, 2.40; 95% CI, 1.57–3.66).
STI in Past 12 Months.
Self-reported STIs averaged 1.4% (Table 3). That prevalence rose to 10.3% among men reporting any commercial sex and to 19.4% among men reporting inconsistent condom use during commercial sex. In a Wald test, the aOR for inconsistent condom use was statistically greater than the aOR for consistent use at P = .02. Alternatively, rerunning the final equation of Table 3 with consistent condom use as the reference category produced an aOR of 3.71 (95% CI, 1.18–11.66) for inconsistent condom use. Sex with a short-term partner was associated with a 1.8% prevalence, which in this sample was statistically no greater than faithful sex with a spouse or stable partner (aOR, 2.53; CI, 0.72–8.83). When added to the final multivariate equation one at a time, education and occupation were nonsignificant (P > .05).
Table 3.
Sexually Transmitted Infection in the Past 12 Months by Type of Sexual Partner and Age Among Urban Men Aged 18–60 Years
| Risk factors | Any commercial sex |
Commercial sex and condom use |
|||
| No. of participants with STI/total no. of participants (weighted %) (N = 2068) | OR (95% CI) | aOR (95% CI) | OR (95% CI) | aOR (95% CI) | |
| All participants | 31/2068 (1.4) | ||||
| Type of partner in past 12 months | |||||
| Commercial | |||||
| Any | 15/144 (10.3) | 15.13 (6.96–32.9)a,b | 13.10 (5.87–29.42)a,b | ||
| Condom use | |||||
| Inconsistent | 8/41 (19.4) | 31.88 (11.83–85.90)a,b | 29.40 (10.51–82.26)a,b | ||
| Consistent | 7/103 (6.7) | 9.44 (3.68–24.18)a | 7.92 (3.14–19.97)a | ||
| Short term (<6 months) | 3/149 (1.8) | 2.47 (0.68–8.94) | 2.53 (0.72–8.83) | 2.47 (0.68–8.94) | 2.52 (0.72–8.80) |
| Wife or stable partner (≥6 months; reference) | 11/1386 (0.8) | 1.00 | 1.00 | 1.00 | 1.00 |
| No partner | 2/389 (0.5) | 0.72 (0.18–2.79) | 1.62 (0.29–8.87) | 0.72 (0.18–2.79) | 1.62 (0.29–8.95) |
| Age, years | |||||
| 18–25 | 1/384 (0.2) | 0.44 (0.04–5.00) | 0.32 (0.02–6.11) | 0.44 (0.04–5.00) | 0.34 (0.02–6.23) |
| 26–39 | 23/839 (2.8) | 4.99 (1.47–16.90)a | 3.03 (0.89–10.26) | 4.99 (1.47–16.90)a | 3.26 (0.98–10.79) |
| 40–49 | 5/503 (0.9) | 1.68 (0.32–8.71) | 1.29 (0.25–6.57) | 1.68 (0.32–8.71) | 1.33 (0.27–6.49) |
| 50–60 (reference) | 2/342 (0.6) | 1.00 | 1.00 | 1.00 | 1.00 |
The total number and number of participants with commercial sex are for numbers of observations. The adjusted odds ratio (aOR) includes the effects of all risk factors in the column.
Abbreviations: CI, confidence interval; OR, odds ratio.
P < .05.
P ≤ .05 in a Wald test comparing the next OR in the same column.
Concurrency occurred among different types of partners. Among men who had any type of commercial sex in the past 12 months, 88.6% (95% CI, 83.2%–92.5%) also had a wife or stable partner and 32.5% (95% CI, 25.8%–40.0%) had a noncommercial, short-term partner. In addition, among men who had a short-term partner, 88.3% (95% CI, 82.7%–92.3%) had a wife or stable partner.
DISCUSSION
China faces increasing challenges in slowing the spread of HIV infection and other STIs, particular through contact with FSWs [1, 2]. Based on the nationally representative data on men’s self-reported FSW contacts and STIs in 2006, the results in this paper are consistent with those in reports about both the high prevalence of men’s commercial sex and the degree to which unprotected commercial sex increased STIs [1–7]. The Chinese prevalence of commercial sex was either similar to (rural) or greater than (urban and national) the median prevalence for other countries (Figure 1; Table 1).
STIs
The data on self-reported STIs illustrate the high risk of commercial sex and the protective value of consistent condom use. Short-term partners were not of exceptional risk for STI. Commercial partners were of exceptional risk, particularly when commercial sex involved inconsistent condom use (Table 3). Among men reporting commercial sex, concurrency was high: about nine-tenths of men who had commercial sex also had a wife or stable partner, and another one-third had a noncommercial short-term partner. These data were consistent with the conclusion that FSWs and their clients are a major bridge group and therefore worthy of efforts to promote consistent condom use during commercial sex [1, 2].
Risk Groups
The analysis of risk groups suggests 4 conclusions. First, the results were consistent with arguments that rich men who often travel and socialize are a significant risk group [8–10]. In a multivariate analysis, the aORs were large and significant for income, active social life, and work as owner or manager of a larger business (Table 3). Second, the men most at risk were not young but 25–39 years of age. Third, although it is typically not noted in the extant literature for China, men were particularly prone to FSW visits when they reported an early sexual history, including early masturbation and premarital sex. Fourth, as here measured, migrant men differed little from other urbanites. This contravenes some of the results in the extant literature on migrant men [11, 12].
Limitations
First, self-reports in the absence of biomarkers could have produced 2 problems: (1): the overall STI prevalence could be understated, both because of asymptomatic STIs and because of a hesitancy to reveal infections [4]; and (2) differential reporting could have produced artifactual relationships between risk factors and outcomes–for example, this might have happened if owners or managers of larger firms were more both more forthright in reporting FSW visits and more likely to see a doctor and then to report STI diagnoses.
Second, the sampling was problematic, particularly for rural-to-urban migrants and the increasingly mobile urban young. Third, comparisons with other countries were vulnerable to differences in methods used in each country. As in China, most of the surveys in other countries used interviewers who were the same sex as the participant and also separated the participant from other people before asking sensitive questions [19]. However, unlike in China, the data from other countries lacked confidential responses to sensitive questions, which could have skewed reports below Chinese levels.
Conclusion
The results for China in 2006 suggest that men’s sex with FSWs remains a challenge for efforts to control HIV infection and other STIs. FSWs and their clients seem to be a major bridge group in the spread of STIs. The prevalence in men’s use of FSWs remains high, and inconsistent condom use needs further attention.
Notes
Acknowledgments.
This work was supported by the Ministry of Science and Technology of People's Republic of China (grant 2008ZX10001-003 to Wang Ning [subcontract]); the Ford Foundation (grants 1065-0331 and 1070-0226 to S.P.); and the National Institutes of Health (grant R24 HD056670 to Gail Henderson [subcontract]).
Potential conflicts of interest.
All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Rou K, Sullivan SG, Liu P, Wu Z. Scaling up prevention programmes to reduce the sexual transmission of HIV in China. Int J Epidemiol. 2010;39(suppl 2):ii38–46. doi: 10.1093/ije/dyq211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.China CDC, National Centre for AIDS/STD Control and Prevention. Gender analysis of data on HIV epidemic and response in six provinces (Guangdong, Guangxi, Yunnan, Henan, Hubei and Chongqing) Beijing: NCAIDS, China CDC; 2010. http://www.unaids.org.cn/pics/20101210091816.pdf. Accessed 30 August 2011. [Google Scholar]
- 3.Xu JJ, Wang N, Lu L, et al. HIV and STIs in clients and female sex workers in mining regions of Gejiu City, China. Sex Transm Dis. 2008;35:558–65. doi: 10.1097/OLQ.0b013e318165926b. [DOI] [PubMed] [Google Scholar]
- 4.Hong Y, Fang X, Zhou Y, Zhao R, Li X. Factors associated with sexually transmitted infection underreporting among female sex workers in China. J Womens Health. 2011;20:129–36. doi: 10.1089/jwh.2010.2139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yang C, Latkin C, Luan R, Wang C, Nelson K. HIV, syphilis, hepatitis C, and risk behaviours among commercial sex male clients in Sichuan province, China. Sex Transm Infect. 2010;86:559–64. doi: 10.1136/sti.2009.041731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jin X, Smith K, Chen RY, et al. HIV prevalence and risk behaviors among male clients of female sex workers in Yunnan, China. J Acquir Immune Defic Syndr. 2010;52:131–5. doi: 10.1097/QAI.0b013e3181b3552a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pan S, Huang Y, Wang J, Liu Z. “Nan ke” de aizi bing fengxian ji ganyu. Chinese male clients: report on HIV risks and prevention. Zhongguo sexuality yanjiu xilie, 012. Gaoxiong Shi: Wanyou chuban she; 2008. [Google Scholar]
- 8.Uretsky E. “Mobile men with money”: the socio-cultural and politico-economic context of “high-risk” behaviour among wealthy businessmen and government officials in urban China. Cult Health Sex. 2008;10:801–14. doi: 10.1080/13691050802380966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang E. Goudui and the state: constructing entrepreneurial masculinity in two cosmopolitan areas of post-socialist china. In: Hodgson DL, editor. Gendered modernities: ethnographic perspectives. New York, NY: Palgrave; 2001. pp. 235–65. [Google Scholar]
- 10.Zheng T. Cool masculinity: male clients’ sex consumption and business alliance in urban China’s sex industry. J Contemp China. 2006;15:161–82. [Google Scholar]
- 11.Chen X, Stanton B, Li X, Fang X, Lin D, Xiong Q. A comparison of health-risk behaviors of rural migrants with rural residents and urban residents in China. Am J Health Behav. 2009;33:15–25. doi: 10.5993/ajhb.33.1.2. [DOI] [PubMed] [Google Scholar]
- 12.Huang Y, Pan S, Du J. Liudong, xing, aizi bing fangzhi: Xiangmu baogao. Reports on mobility, sexuality and HIV/AIDS prevention. Zhongguo sexuality yanjiu xilie, 013. Gaoxiong Shi: Wanyou chuban she; 2008. [Google Scholar]
- 13.Levy PS, Lemeshow S. Sampling of populations: methods and applications. New York, NY: Wiley; 1999. [Google Scholar]
- 14.StataCorp LP. College Station, TX: StataCorp LP; 2009. Stata survey data reference manual: release 11. [Google Scholar]
- 15.White H. Estimation, inference and specification analysis. New York, NY: Cambridge University Press; 1994. [Google Scholar]
- 16.Treas J, Giesen D. Sexual infidelity among married and cohabiting Americans. J Mar Fam. 2000;62:48–60. [Google Scholar]
- 17.Atkins DC, Baucom DH, Jacobson NS. Understanding infidelity: correlates in a national random sample. J Fam Psych. 2001;15:735–49. doi: 10.1037//0893-3200.15.4.735. [DOI] [PubMed] [Google Scholar]
- 18.DHS (MEASURE DHS, StatCompiler) Statistics compiled from demographic and health surveys. Calverton, MD: Macro International Inc; 2010. http://www.measuredhs.com/hivdata/. Accessed 15 February 2010. [Google Scholar]
- 19.DHS (MEASURE DHS+) Training guidelines for DHS surveys. Calverton, MD: Macro International Inc; 2000. http://www.measuredhs.com/pubs/pdf/DHSM3/DHS_Training_Guidelines.pdf. Accessed 29 August 2010. [Google Scholar]
- 20.Caraël M, Slaymaker E, Lyerla R, Sarkar S. Clients of sex workers in different regions of the world: hard to count. Sex Transm Infect. 2006;82:iii26–33. doi: 10.1136/sti.2006.021196. [DOI] [PMC free article] [PubMed] [Google Scholar]