Abstract
One-fifth of all public treatment admissions are emerging adults, and few studies have considered whether treatments are developmentally appropriate. This study compares outcomes between substance use-disordered adolescents and emerging adults that received the Adolescent Community Reinforcement Approach (A-CRA). Propensity score matching was used to create a weighted comparison group of adolescents (n=151) that had similar demographic characteristics, clinical severity, and treatment retention as the group of emerging adults (n=152). We examined age differences in abstinence and other psychosocial outcomes at the last available follow up. Emerging adults and adolescents both reduced their substance use at follow-up. However, emerging adults were less likely to be abstinent and in remission, and had more days of alcohol use when compared to adolescents. This study’s findings are consistent with prior work on emerging adults. Additional research should examine features of interventions that are most effective in addressing the developmental needs of emerging adults.
Keywords: Emerging Adults, Adolescents, Drug Abuse Treatment, Propensity Score Matching
1. Introduction
Until recently, substance use disorder (SUD) treatments developed for adults have been delivered to adolescents with few modifications (Dennis, Dawud-Noursi, Muck, & McDermeit, 2003; Muck et al., 2001). Although many sophisticated adolescent trials have been conducted in the last decade (Becker & Curry, 2008; Waldron & Turner, 2008), the emphasis on testing developmentally appropriate treatments has not extended to emerging adults (EAs) aged 18–25 (Arnett, 2000). This is unfortunate as EA aged 18–25 represent nearly 20% of all publicly funded treatment admissions (Substance Abuse and Mental Health Services Administration, 2007), the peak prevalence of SUD and other mental health problems occurs during EA (Blanco et al., 2008; Substance Abuse and Mental Health Services Administration, 2008), emerging adults have lower treatment motivation and higher psychiatric comorbidity than other age groups (Chan, Dennis, & Funk, 2008; DiClemente, Doyle, & Donovan, 2009; Mason & Luckey, 2003), and EAs with SUD have poorer outcomes when compared to older adults (Satre, Mertens, Areán, & Weisner, 2003; Satre, Mertens, Arean, & Weisner, 2004). With few exceptions (Carroll et al., 2006), EA outcome studies do not generalize to typical SUD outpatient settings and mainly involve brief alcohol screening interventions in college or non-traditional settings (Dimeff, Baer, Kivlahan, & Marlatt, 1999; Doumas & Andersen, 2009; Juarez, Walters, Daugherty, & Radi, 2006; Monti et al., 1999; Monti et al., 2007; Saitz et al., 2007).
This study tests whether or not EAs receiving the Adolescent Community Reinforcement Approach (A-CRA; Godley et al., 2001) have different outcomes compared to adolescents. Few studies have enough variation in age to answer such a question, leading some to conclude that interventions with generally robust efficacy findings should be assumed to work with special populations such as EAs (Miller, Villanueva, Tonigan, & Cuzmar, 2007). However, if age moderates treatment response, additional research with EAs may be warranted.
1.1. Differences between emerging adults (EAs) and adolescents
Arnett (2000) argued that emerging adulthood (EA) is a unique developmental stage, because of demographic trends that delay the onset of adult roles (i.e., committed romance, career job). When EAs are asked about whether or not they have reached adult status, the modal reply is yes and no (Arnett, 2003). EAs enjoy fewer limits (i.e., less social control from parents, bosses, romantic partners) than adolescents, which permits greater identity exploration compared to adolescents (Arnett, 2000). EA is distinguished from the onset of adulthood, because nationally we see fewer 18–25 year olds reaching the traditionally accepted adulthood milestones (Shanahan, Porfeli, Mortimer, & Erickson, 2005).
1.1.2. Clinical samples
Little work exists on whether attending to the proposed developmental aspects of EA would lead to substance use remediation (Arnett, 2005). In the absence of empirical investigations on whether developmental variables moderate the effect of age on treatment outcomes, it is difficult to know the utility of this work for designing EA treatments. An important first step, however, would be to document whether treatment responses vary by age.
Unfortunately, very few studies have directly compared the characteristics of EAs and adolescents in treatment for SUD (Chan et al., 2008; Dennis, White, & Ives, 2009), a few have compared EAs to older adults (Mason & Luckey, 2003; Satre et al., 2003; Satre et al., 2004), and many studies comparing adolescents to adults do not distinguish between EAs and the rest of the adult sample (Handelsman, Stein, & Grella, 2005). Dennis and colleagues (2009) pooled data across 113 adolescent treatment programs funded by the Substance Abuse and Mental health Services Administration (SAMHSA). Although these treatment programs focused on adolescents ages 12–17 (n = 13,625), emerging adults (n=1149) comprised 8% of total admissions. At clinical intake, and compared to adolescents, EAs were less likely to be in school, have early onset substance use (i.e., < age 15), have been victimized, engage in violent or criminal behaviors, have past year psychiatric problems, or have peers that used substances on a weekly basis. They were, however, more likely than their adolescent counterparts to use alcohol and drugs other than marijuana weekly, live with someone that used drugs on a weekly basis, be employed, have prior treatment episodes, perceive their substance use to be problematic, and be involved with the child welfare system. Several studies have noted that EAs have lower treatment motivation compared to older adults (DiClemente et al., 2009; Mason & Luckey, 2003; Melnick, De Leon, Hawke, Jainchill, & Kressel, 1997; Satre et al., 2003; Sinha, Easton, & Kemp, 2003). Compared to adolescents, one study showed that EAs had less pressure from family and friends to quit (Smith, Cleeland, & Dennis, 2010). Finally, Satre and colleagues (2004) showed differences in outcomes between EAs and older adults in alcohol or drug treatment, which were moderated by characteristics more common to EAs like poor retention and being surrounded by those that encourage substance use.
Alcohol and drug-involved leisure activities and dense substance using social networks are negatively correlated with treatment outcomes and positively correlated with substance use for both adolescents and EAs (Andrews, Tildesley, Hops, & Li, 2002; Borsari & Carey, 2006; Delucchi, Matzger, & Weisner, 2008; Godley, Kahn, Dennis, Godley, & Funk, 2005). No study to date, however, has investigated whether age differences in social network composition exists after receipt of SUD treatment. It is possible that EAs social networks may be more difficult to alter since the peak prevalence of substance use occurs during EA.
1.2. The Adolescent Community Reinforcement Approach (A-CRA)
The Adolescent Community Reinforcement Approach (A-CRA) is an operant behavioral approach that attempts to make an alcohol and drug-free lifestyle more rewarding than continued use (Godley et al., 2001). It is a slight adaptation of the adult CRA treatment (Meyers & Smith, 1995), shown to be efficacious for treating substance use disorders in numerous metaanalyses (Finney & Monahan, 1996; Holder, Longabaugh, Miller, & Rubonis, 1991; Miller et al., 1995; Miller & Wilbourne, 2002; Roozen et al., 2004). A-CRA outcomes may differ for EAs because some adolescent components were added while some adult components were omitted.
1.3. Summary and hypotheses
Based on prior research, we hypothesized that substance use outcomes, especially alcohol use outcomes, will be poorer for EAs. Although there is no literature to guide us, we expected that EAs social networks would be less malleable than those of adolescents. Finally, due to prior research showing CRA to have a larger impact on depression among EAs (Slesnick et al., 2007) we examined whether mental health outcomes would be better for EAs than for adolescents.
2. Materials and methods
2.1. Participants and setting
Data were obtained from 28 SAMHSA-funded outpatient treatment sites that implemented A-CRA. IRB approval was obtained locally by each participating project. Coded data were shared with the first author after a data request was made, sites were allowed to comment and/or opt out, and a HIPAA-compliant data sharing agreement was executed.
At the time of this study, over two thousand adolescents and emerging adults (N=2400) were enrolled in the study. Adolescents (n=1922) and emerging adults (n=152) with baseline data and either three or six month follow up data (86% of total sample) were included in the analysis. Out of this larger pool of adolescents, a smaller sample with equivalent baseline characteristics (n =151) was derived using propensity score matching (see below). Participants in the weighted analysis sample (see Table 1) were racially diverse and mostly male (71.7%).
Table 1.
Demographic Characteristics and Diagnostic Severity of Analysis Sample
|
Adolescents (n = 151) |
EA (n = 152) |
Total (n = 303) |
|
|---|---|---|---|
| (% or M (SD)) | (% or M (SD)) | (% or M (SD)) | |
| Demographic Characteristics | |||
| Gender | |||
| Male | 71.6% | 70.4% | 71.7% |
| Female | 28.4% | 29.6% | 28.3% |
| Age* | 15.6 (1.22) | 18.4 (.88) | 17.1 (1.6) |
| Race/Ethnicity | |||
| Caucasian | 29.8% | 30.3% | 30.0% |
| African-American | 19.2% | 23.7% | 21.5% |
| Hispanic | 24.3% | 28.5% | 26.4% |
| Native American | 2.0% | 3.3% | 2.6% |
| Other/Biracial | 19.3% | 19.8% | 19.5% |
| Substance Use Disorders | |||
| Past Year Dependence | 50.3% | 57.9% | 54.1% |
| Lifetime Substance Use Disordera | 83.0% | 93.0% | 88.0% |
| Drug for which most DSM criteria met, highest frequency of use, or most recent use | |||
| Alcohol* | 19.9% | 27.6% | 23.8% |
| Marijuana* | 60.9% | 49.3% | 55.1% |
| Amphetamines | 11.9% | 15.1% | 13.5% |
| Cocaine | 0.7% | 0.0% | 0.3% |
| Opioids | 2.0% | 3.9% | 3.0% |
| Other | 4.6% | 4.3% | 4.3% |
p<.05
Includes both substance dependence and substance abuse diagnoses.
2.3. Treatment and data collection monitoring
Treatment centers sent staff members to A-CRA training with the model’s developers, submitted digital session recordings until certification status was reached, and used common outcome measures. Sites elected at least one individual to receive training as an A-CRA supervisor so that on-going adherence monitoring was sustained locally. Staff members were also certified in standardized data collection using the Global Appraisal of Individual Needs (GAIN; Dennis, Titus, White, Unsicker, & Hodgkins, 2002).
2.4. Measures
All outcome measures were from the Global Appraisal of Individuals Needs (GAIN). Below we provide an overview of the GAIN, as well as details on the independent, dependent, and matching variables. (A detailed description (i.e., psychometrics, scoring interpretation) of all variables and scales used to develop the propensity score is available from the first author and also at http://chestnut.org/LI/gain/index.html #Supporting psychometrics, scales, and crosswalks.)
The GAIN is a reliable and valid semi-structured interview measure for which core scales exhibit excellent internal consistency, good agreement with blind psychiatric diagnoses (Jasiukaitis & Shane, 2001) and timeline followback (Dennis, Funk, Godley, Godley, & Waldron, 2004), good concordance with urine tests (Buchan, Dennis, Tims, & Diamond, 2002), and the ability to differentiate among adolescents treated in various levels of care (Dennis, Scott, Godley, & Funk, 1999). The GAIN contains items consistent with the DSM IV (American Psychiatric Association, 2000) criteria for all substance use disorders and many common Axis I mental health diagnoses (i.e., ADHD, Major Depression, Generalized Anxiety). Furthermore, the GAIN has over 100 scales and indices to inform complex level of care placements (Mee-Lee, Gartner, Miller, Shulman, & Wilford, 2001), or for use in developing propensity scores.
2.4.1 Independent and Dependent Measures
We used age in years (mean = 17.1, SD = 1.6) to code whether participants were adolescents or EAs. Adolescents under age 18 were coded 0, and emerging adults aged 18-25 were coded 1. The majority of the participants in the EA group, however, (77%) were 18.
2.4.2 Dependent Measures: Substance Use Outcomes
Five variables were used to measure substance use outcomes. First, a dichotomous (0 = no, 1 = yes) variable indicated whether the participant was abstinent and in early remission, as indicated by no past month substance use or SUD criteria, while residing in the community (i.e., vs. a controlled environment). This outcome variable has been used in other major clinical trials (Dennis et al, 2004), prevents substance use outcomes from being unduly influenced by time spent in controlled environments (Godley, Dennis, Godley, & Funk, 2004), and avoids a narrow focus on a single substance of abuse in a polysubstance using sample (Rounsaville, Petry, & Carroll, 2003). Next, Substance use frequency was measured with the Substance Frequency Scale (SFS), indicating the average proportion of days (out of the past 90) of any drug use, heavy drug use, days of problems due to use and days of alcohol, marijuana, crack (or powder) cocaine, or heroin use. Values are expressed as decimal values ranging from zero to one with higher values indicating more frequent use (and problems resulting from use) across a variety of substances. Third, we also used two indicators of past 90 day alcohol use, one asking on how many days participants drank any alcohol and another asking about binge alcohol use (i.e., got drunk or had five or more drinks). Finally, Substance-related problems were measured using the Substance Problem Scale (SPS; past month version), which contains sixteen yes/no items that measure the DSM IV criteria for substance abuse (4 items) and dependence (7 items), as well as other health and social consequences due to use (5 items).
2.4.3 Dependent Measures: Social Network Variables
Three measures were used to measure participants’ social networks. First, two items asked participants for the number of days they spent in the past 90 days (Range = 0 to 90) participating in formal recreational activities where others present were or were not using alcohol or other drugs. Second, we used the Social Risk Index, which asks participants to indicate how many peers (seven items, 1= none to 4 = all) attend school or work, have frequent verbal or physical conflicts, use drugs or alcohol, have been in treatment, or consider themselves to be in recovery (reversed). Higher scores indicate more risky peer environments.
2.4.3 Dependent Measures: Mental Health Functioning
The Emotional Problem Scale is a measure of days of functional impairment from mental health problems out of the past 90 days. Similar to the SFS, it is a proportional measure out of 90 days (range = 0-1) of days of being bothered by and/or kept from responsibilities due to emotional problems, days of experiencing traumatic memories, and days of having difficulty paying attention and/or controlling one’s impulses. The baseline means and standard deviations for all dependent variables appear at the bottom of Table 2.
Table 2.
Baseline Differences on Clinically Relevant Variables Prior to and After Propensity Score Matching
| Prior to Propensity Score Matching | After Propensity Score Matching | |||||
|---|---|---|---|---|---|---|
|
Adolescents (n = 1922) |
EA (n = 152) |
Total (n = 2074)a |
Adolescents (n = 151) |
EA (n = 152) |
Total (n = 303) |
|
| (% (n) or M (SD)) | (% (n) or M (SD)) | (% (n) or M (SD)) | (% (n) or M (SD)) | (% (n) or M (SD)) | (% (n) or M (SD)) | |
| Clinical Severity and Treatment Motivation | ||||||
| Number of Substance Use Disorders | .78 (.86) | .93 (.96)** | .78 (.87) | .83 (.94) | .93 (.96) | .88 (.95) |
| Years of Substance Use | 2.9 (2.1) | 4.6 (2.8)** | 3.1 (2.2) | 4.0 (2.8) | 4.7 (2.8)** | 4.3 (2.8) |
| Problem Orientation Scale | .67(1.5) | .99 (1.7)** | .69 (1.5) | .79 (1.6) | .99 (1.7) | .89 (1.6) |
| Conduct Disorder Scale (CDS) | 3.4 (3.2) | 2.8 (2.9)** | 3.4 (3.1) | 2.8 (2.9) | 2.8 (2.9) | 2.8 (2.9) |
| Crime and Violence Scale (CVS) | 7.3 (5.8) | 6.4 (5.4)** | 7.3 (5.7) | 6.3 (5.2) | 6.4 (5.4) | 6.3 (5.3) |
| Anxiety and Fear Severity Scale (AFSS) | 2.2 (2.5) | 2.7 (3.2)** | 2.2 (2.6) | 2.4 (2.8) | 2.7 (3.2) | 2.6 (3.0) |
| Depression Symptom Scale (DSS) | 2.8 (2.6) | 3.3 (2.9)* | 2.8 (2.6) | 3.0 (2.8) | 3.2 (2.9) | 3.1 (2.9) |
| Traumatic Stress Scale (TSS) | 2.2 (3.4) | 2.8 (3.7)** | 2.2 (3.5) | 2.4 (3.7) | 2.8 (3.7) | 2.6 (3.7) |
| General Victimization Scale (GVS) | 3.1(3.1) | 3.7 (3.5)** | 3.1 (3.1) | 3.4 (3.2) | 3.7 (3.5) | 3.5 (3.3) |
| Treatment Process | ||||||
| %Young Adults at Treatment Site | 7.1 (7.6) | 16.9 (9.1)** | 7.8 (8.1) | 14.7 (9.9) | 16.9 (9.1)** | 15.8 (9.6) |
| Length of Treatment (in days) | 180.4 (99.8) | 162.8 (77.7)** | 179.1 (98.4) | 164.4 (86.8) | 162.8 (77.7) | 163.6 (82.2) |
| Environmental Factors | ||||||
| Days in Controlled Environment | 6.5 (16.9) | 4.2 (14.2)** | 6.4 (16.7) | 4.7 (13.7) | 4.2 (14.2) | 4.4 (13.9) |
| Living Risk Index | 10.7 (2.9) | 11.3 (3.5)* | 10.8 (3.0) | 11.0 (3.1) | 11.3 (3.5) | 11.2 (3.3) |
| Baseline Values of Outcomes | ||||||
| Abstinent and in the Community | 24.9% (477) | 19.7% (30) | 24.5% (507) | 23.2% (35) | 19.7% (30) | 21.4% (65) |
| Substance Problem Scale | 2.9 (3.6) | 3.2 (4.2) | 3.1 (3.9) | 3.2 (3.7) | 3.2 (4.2) | 3.2 (3.9) |
| Substance Frequency Scale | .13 (.14) | .17 (.17)** | .13 (.14) | .15 (.15) | .17 (.17) | .16 (.16) |
| Days of alcohol use | 6.0 (11.6) | 9.3 (16.2)** | 6.3 (12.1) | 7.8 (13.9) | 9.3 (16.1) | 8.6 (15.1) |
| Days of binge alcohol use | 3.2 (8.2) | 5.6 (12.2)** | 3.4 (8.6) | 4.5 (11.1) | 5.5 (12.1) | 5.0 (11.6) |
| Days of AODA-free activities* | 10.8 (19.6) | 8.1 (15.1)** | 10.6 (19.3) | 8.8 (17.4) | 8.1 (15.1) | 8.4 (16.2) |
| Days of AODA-involved activities | 9.2 (17.8) | 11.0 (19.0)** | 9.4 (17.9) | 10.5 (20.2) | 11.0 (19.0) | 10.6 (19.5) |
| Social Risk Index | 13.3 (4.3) | 13.9 (4.4) | 13.6 (4.4) | 13.4 (4.2) | 13.9 (4.4) | 13.7 (4.3) |
| Emotional Problem Scale | .25 (.19) | .25 (.19) | .25 (.19) | .24 (.20) | .25 (.19) | .25 (.19) |
p<.10,
p<.05,
Actual n differs by variable due to missing data. On average, 1.5% of responses were missing (range = 0 to 4.9% missing)
2.4.4 Variables used in Propensity Matching
In addition to baseline measures of the dependent variables, as well as gender and minority status, 34 variables were considered for use in creating a propensity score to control for baseline differences in confounding variables between EAs and adolescents. These variables (e.g., substance use and psychiatric severity, treatment utilization, motivation for treatment) were examined due to their associations with treatment outcomes in prior studies, and were included in the propensity score if they were correlated with outcome variables and significant differences existed between age groups at baseline (i.e., p < .10). Out of 34 variables, 13 (38%) met these criteria and were used to develop the propensity score. Table 2 shows baseline values of these variables prior to and after calculating the propensity score (Rosenbaum & Rubin, 1983).
2.5. Data analysis procedures
Following procedures used in other investigations (Smith et al., 2010; Subramaniam, Ives, Stitzer, & Dennis, 2010), propensity score weighting was used to create comparison groups of equal size while controlling for differences between age cohorts on select variables. The propensity score was calculated using a combination of logistic regression and discriminant function analysis to predict age group membership as a function of variables mentioned above. The weight was then calculated as the propensity score times the sample size of the EA group over the sum of the adolescent weights. Adding the latter (a constant) does not affect the match but creates equal sample sizes per group and creates a slightly more conservative test. The final weighted groups were approximately the same size (151 adolescents, 152 emerging adults).
After weighting, we used logistic (one outcome; abstinence and in remission) or linear regression (eight outcomes) to predict outcomes at participants’ last available follow up (3 or 6 months post-intake), entering age group as the independent variable and controlling for the number of days to the follow up interview. To understand the magnitude of any differences, we also calculated effect sizes (Cohen’s d) by subtracting adolescents’ follow-up scores from those of EAs, and dividing by the standard deviation for the adolescent group.
3. Results
3.1. Equivalence of groups prior to and after matching
Prior to developing the propensity score, there were several significant differences between emerging adults and adolescents on factors known to correlate with substance misuse treatment outcomes. Specifically, at baseline adolescents exhibited significantly lower problem recognition (POS), endorsed a higher number of conduct disorder symptoms (CDS), exhibited more criminal and violent behavior (CVS), and spent more time in controlled environments. On average, adolescents’ lengths of stay were 20 days longer than those for EAs. Not surprisingly due to their longer lengths of substance use, EAs were found to be significantly more impaired on many measures of psychosocial functioning, which included more frequent use of substances in the past 90 days, higher number of unique substance use disorders, higher means on all internalizing disorder scales (i.e., depression, anxiety, and traumatic stress), higher levels of victimization (i.e., physical, sexual, emotional), more days of any or binge use of alcohol, fewer days of substance-free recreational activities and more days of substance-involved ones, and higher proportions of individuals in their households who were using drugs or engaging in antisocial behaviors. Furthermore, EAs were more likely to report being treated at facilities that treated a higher percentage of EAs as a percent of total admissions. This is important as, for whatever unobserved reason (e.g., staff expertise), this variable was negatively correlated with our dependent measures.
After matching, differences on baseline severity and treatment process variables largely disappeared, with two exceptions. First, EAs still had more experience (in years) using substances (mean = 4.7 vs. 4.0 for adolescents). However, the difference was largely diminished, with the average adolescent in the larger unmatched sample using substances for only 2.8 years. Additionally, EAs were still treated in facilities that included a higher proportion of their age mates as a percent of total admissions (mean percent at site = 16.9% vs. 14.7% for adolescents). Again, however, we find that the mean difference was much smaller than that found for the unmatched sample (mean difference matched = 2.2% versus mean difference unmatched = 9.8%). (Our models that controlled for these two variables were not substantively different, and below we present unadjusted analyses.) Overall, the matched sample of adolescents was equivalent in size, demographic characteristics and clinical severity when compared to the EA sample.
3.2. Outcomes at last available follow-up
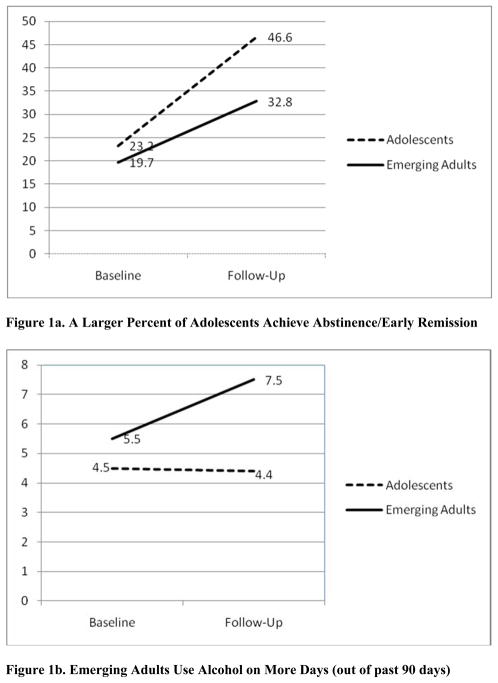
Table 3 presents the means, standard deviations, and effect sizes for follow up outcome differences between emerging adults and adolescents. Age group was a significant predictor of two substance use outcomes, being abstinent and SUD symptom-free while residing in the community (Hosmer and Lemeshow χ2 = 4.3, ns; Nagelkerke R2 = .03; Odds Ratio (95% CI) = .58 (.36, .92); p = .02), as well as days of any alcohol use in the past 90 days (df = 1, 298; B = 2.78; R2 = .02; p =.04). For the abstinence/remission measure, a moderate effect was detected. Whereas more participants in both age groups were abstinent at follow up (Figure 1a), the slopes for days of any alcohol use were flat and positive for adolescents and emerging adults, respectively (Figure 1b). In other words, the group average for adolescents remained the same over time, and the average use increased for emerging adults from baseline to follow up. Although age group did not significantly predict the three other substance use outcomes (i.e., binge drinking, substance problems, or substance use frequency), emerging adults were worse on all these scales with small effects (Cohen’s d’s greater than .20) present for two out of three measures. The small effect for substance use frequency (Cohen’s d’s = .25, p = .058) approached statistical significance.
Table 3.
Means, Standard Deviations and Effect Sizes for Follow-Up Outcomes
| Outcome (Range) | Adolescents (n = 151)a (% or M (SD)) |
EA (n = 152) (% or M (SD)) |
Effect Size (OR or d) |
|---|---|---|---|
|
Substance Use Outcomes
| |||
| Abstinent (EA=1, Adolescent=0)b | 46.6% | 32.8% | .58* |
|
| |||
| Substance Problem Scale (0–16) | 1.5 (2.8) | 1.8 (1.8) | .11 |
| Substance Frequency Scale (0–1) | .07 (.12) | .10 (.13) | .25 c |
| Days of Alcohol Use (0–90) | 4.4 (10.1) | 7.4 (13.1) | .30* |
| Binge Drinking Days (0–90) | 2.6 (8.2) | 4.3 (10.5) | .21 |
| Social Environment Outcomes | |||
| AODA-Involved Activities (0–90) | 5.3 (12.2) | 7.4 (16.5) | .17 |
| AODA-Free Activities (0–90) | 8.1 (17.3) | 7.8 (17.4) | −.02 |
| Social Risks (0–28) | 12.4 (4.4) | 12.9 (4.2) | .11 |
| Mental Health Outcomes | |||
| Emotional Problem Scale (0–1) | .16 (.15) | .18 (.18) | .13 |
p < .05
Actual n differs by variable due to missing data. On average, 1.5% of responses were missing (range = 0 to 4.9% missing)
Percent of sample indicating they had not used any substances in the past month, were living in the community, and had no past month DSM IV criteria for SUDs. This effect size is an Odds Ratio (95% CI: .36 to .92). All other effect sizes are reported as Cohen’s d.
p = .058
Figure 1.
Age group was not a significant predictor of any of the social network or mental health outcomes. Although emerging adults reported slightly more social risks and days of emotional problems, as well as fewer days of alcohol and drug free recreational activities, these differences appear negligible. One non-significant trend worth noting, however, was that emerging adults reported, on average, 2.1 more days of being involved in alcohol and drug related recreational activities. This approached a small effect (Cohen’s d =.17).
4. Discussion
The study findings indicate that after controlling for numerous potential confounds via propensity matching, emerging adults fared poorer on two separate substance use outcomes when compared to younger adolescents receiving A-CRA. Specifically, a higher percent of adolescents (46.6% vs. 32.8% of emerging adults) achieved early full symptom remission and abstinence at follow up while residing in the community. This difference is important given the heavy use (Mean AOD use at follow up =32.1 days) among those adolescents and EA that did not achieve SUD symptom-remission and abstinence. On average, emerging adults also drank alcohol on three more days (out of the past 90) when compared to adolescents. We found no differences on social network or mental health outcomes.
It is not clear why differences between adolescents and emerging adults were not robust across multiple outcome variables in this study. We only found significant differences on two of five substance use measures. It is possible that this is due to the large number of 18 year olds in our emerging adult sample. On average, our EAs (mean age =18.4 years) were only 2.8 years older than the adolescents. This pattern of mixed findings could also be due to differences in the measures. For example, the two summary measures of abstinence/remission and substance frequency that account for multiple substance use may have been more sensitive to heterogeneity in substances used in this sample. In supplemental analyses we found an inconsistent pattern where emerging adults used some drugs more frequently and vice versa. (Results from these analyses are available upon request from the first author.) Although these differences were not statistically significant for any single substance, findings for our abstinence/remission measure (Odds Ratio =.58, p<.05) and the substance frequency scale (d = .25, p=.058) both reveal poorer outcomes for emerging adults. It would not seem, however, that Substance Problem Scale outcomes would be explained by heterogeneous use patterns, and the lack of differences on this continuous measure of DSM IV SUD criteria remains a mystery. Notwithstanding this mixed pattern of findings, the differences in abstinence/remission detected here appear clinically significant given the heavy AOD use (mean =32.1 days) of participants that did not achieve this milestone through the six month follow up wave.
Also, unlike one study comparing emerging adults to older adults (Sarte et al., 2004), we found no evidence that emerging adults social environment risks would be more severe at follow up. The A-CRA treatment was equally effective in reducing AOD-involved activities for both age groups. Again, it is possible this is due to the smaller age differences separating these developmental periods, given the larger age range in the Sarte et al (2004) study. However, in this study, provision of A-CRA did not result in increases of AOD-free activities for either group. (See tables 2 and 3). Thus, adolescents and emerging adults may both benefit from additional strategies to increase prosocial, AOD-free recreation.
We did not replicate findings that CRA has a stronger influence on emerging adults’ internalizing symptoms (Slesnick, Prestopnik, Meyers, & Glassman, 2007). This may have been due to differences in measures used in Slesnick et al (2007) and the present study. That is, our measure of emotional problems does not focus on depression symptoms, but rather on days of impairment across multiple mental health domains in addition to depression (e.g., traumatic stress, externalizing behaviors). Nevertheless, in supplemental analyses (not shown), we found no differences in days of impairment from depression/anxiety between adolescents and EA. A second possibility is that differences in mental health outcomes between adolescents and emerging adults are negligible. Additional research is needed to clarify whether CRA has differential impacts on emerging adults’ depression outcomes.
This study’s limitations should be considered when interpreting its findings. First, emerging adults only comprised a small percent (8%) of the total treatment sample at these predominantly adolescent treatment sites. Thus, the effects observed here are for emerging adults that were admitted to predominantly adolescent programs. Also, while we were able to account for some site level variables (i.e., percent of EA at each site) the statistical analyses used did not fully account for the nesting of clients within therapists and within sites. Second, the sample of emerging adults in this study was skewed toward 18 year olds, as only 23% of the emerging adult subset was age 19 or older. Thus, findings may not generalize to populations of older emerging adults around 25 years of age. Further, it is possible that the truncated age range of the EA subsample accounts for the small differences we observed here between EAs and adolescents. However, the study does call attention to an important clinical issue--that individuals aged 18 are either placed in adolescent or adult programs, neither of which may be specifically tailored to their needs. Here we see that when emerging adults are admitted to adolescent outpatient programs implementing an empirically-supported adolescent treatment, they fare poorer in terms of the percent achieving early full symptom remission and abstinence while residing the community. Results also only generalize to emerging adults and adolescents within a certain range of clinical severity, and adolescents in the matching sample of this study exhibited higher severity than the adolescents not selected for matching. It is also important to note that this comparison of adolescent and EA outcomes is only for one type of treatment. Also, the follow-up period of 3- and 6- months is relatively short and many individuals were still in treatment at those time points. Next, we note that we did not have access to urine test data to corroborate self reported substance use at follow up. Finally, we relied on some single item outcome indicators, days of alcohol and drug free (or AOD-involved) recreational activities, and these items have not been validated in previous outcome studies as stand-alone measures.
5. Conclusion
Although findings were mixed, preliminary evidence provided here suggests that evidence based treatments should be tested specifically with EAs. We could only locate one community clinic-based study that tested the comparative efficacy of different interventions with EAs (Carroll et al., 2006). Studies are needed that manipulate components of treatments thought to be developmentally relevant to EAs. Unmeasured developmental variables (e.g., identity development, feeling in between adulthood and adolescence) on which adolescents and emerging adults differ, may account for differences in substance use outcomes observed here. Further, several hypotheses exist about how the developmental features defining emerging adulthood should relate to substance abuse (Arnett, 2005), but they have not been subjected to empirical testing. In sum, it is important for future studies to randomize emerging adults to treatment conditions that vary in exposure to components thought to meet their specific developmental needs.
Acknowledgments
The development of this article was supported by NIAAA Grant # 1K23AA017702 - 01A2 (Smith). The opinions, however, are those of the authors and do not reflect official positions of NIAAA or the federal government. An earlier version of this manuscript was presented at the 2010 meeting of the Research Society on Alcoholism in San Antonio, Texas.
Footnotes
Author’s Note: Dr. Smith is Assistant Professor of Social Work.
Contributor Information
Douglas C. Smith, University of Illinois at Urbana-Champaign
Susan H. Godley, Chestnut Health Systems, Bloomington, IL
Mark D. Godley, Chestnut Health Systems, Bloomington, IL
Michael L. Dennis, Chestnut Health Systems, Bloomington, IL
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders, text revision. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Andrews JA, Tildesley E, Hops H, Li F. The influence of peers on young adult substance use. Health Psychology. 2002;21(4):349–357. doi: 10.1037//0278-6133.21.4.349. [DOI] [PubMed] [Google Scholar]
- Arnett JJ. Emerging adulthood: A theory of development from the late teens through the twenties. American Psychologist. 2000;55(5):469–480. [PubMed] [Google Scholar]
- Arnett JJ. Conceptions of the transition to adulthood among emerging adults in American ethnic groups. New Directions in Child and Adolescent Development. 2003;100:63–75. doi: 10.1002/cd.75. [DOI] [PubMed] [Google Scholar]
- Arnett JJ. The developmental context of substance use in emerging adulthood. Journal of Drug Issues. 2005;35(2):235–254. [Google Scholar]
- Becker SJ, Curry JF. Outpatient interventions for adolescent substance abuse: A quality of evidence review. Journal of Consulting and Clinical Psychology. 2008;76(4):531–543. doi: 10.1037/0022-006X.76.4.531. [DOI] [PubMed] [Google Scholar]
- Blanco C, Okuda M, Wright C, Hasin DS, Grant BF, Liu S, Olfson M. Mental health of college students and their non-college-attending peers: Results from the national epidemiologic study on alcohol and related conditions. Arch Gen Psychiatry. 2008;65(12):1429–1437. doi: 10.1001/archpsyc.65.12.1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsari B, Carey K. How the quality of peer relationships influences college alcohol use. Drug & Alcohol Review. 2006;25(4):361–370. doi: 10.1080/09595230600741339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchan BJ, Dennis ML, Tims FM, Diamond GS. Cannabis use: Consistency and validity of self-report, on-site urine testing and laboratory testing. Addiction. 2002;97:98–108. doi: 10.1046/j.1360-0443.97.s01.1.x. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Easton CJ, Nich C, Hunkele KA, Neavins TM, Sinha R, Rounsaville BJ. The use of contingency management and motivational/skills-building therapy to treat young adults with marijuana dependence. Journal of Consulting and Clinical Psychology. 2006;74(5):955–966. doi: 10.1037/0022-006X.74.5.955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan Y, Dennis ML, Funk RR. Prevalence and comorbidity of major internalizing and externalizing problems among adolescents and adults presenting to substance abuse treatment. Journal of Substance Abuse Treatment. 2008;34(1):14–24. doi: 10.1016/j.jsat.2006.12.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delucchi KL, Matzger H, Weisner C. Alcohol in emerging adulthood: 7-year study of problem and dependent drinkers. Addictive Behaviors. 2008;33(1):134–142. doi: 10.1016/j.addbeh.2007.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis ML, White MK, Ives ML. Individual characteristics and needs associated with substance misuse of adolescents and young adults in addiction treatment. In: Leukefeld C, Gullotta T, Stanton Tindall M, editors. Handbook on adolescent substance abuse prevention and treatment: Evidence-based practice. New London, CT: Child and Family Agency Press; 2009. pp. 45–72. [Google Scholar]
- Dennis ML, Dawud-Noursi S, Muck RD, McDermeit M. The need for developing and evaluating adolescent treatment models. In: Stevens S, Morral A, editors. Adolescent substance abuse treatment in the united states: Exemplary models from a national evaluation study. New York: The Haworth Press; 2003. pp. 3–34. [Google Scholar]
- Dennis ML, Funk R, Godley SH, Godley MD, Waldron H. Cross-validation of the alcohol and cannabis use measures in the global appraisal of individual needs (GAIN) and timeline followback (TLFB; form 90) among adolescents in substance abuse treatment. Addiction. 2004;99:120–128. doi: 10.1111/j.1360-0443.2004.00859.x. [DOI] [PubMed] [Google Scholar]
- Dennis ML, Scott CK, Godley MD, Funk R. Comparisons of adolescents and adults by ASAM profile using GAIN data from the drug outcome monitoring study (DOMS): Preliminary data tables 1999 [Google Scholar]
- Dennis ML, Titus JC, White MK, Unsicker JI, Hodgkins D. Global appraisal of individual needs (GAIN): Administration guide for the GAIN and related measures. Bloomington, IL: Chestnut Health Systems; 2002. [Google Scholar]
- DiClemente CC, Doyle SR, Donovan D. Predicting treatment seekers' readiness to change their drinking behavior in the COMBINE study. Alcoholism: Clinical and Experimental Research. 2009;33(5):879–892. doi: 10.1111/j.1530-0277.2009.00905.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimeff LA, Baer JS, Kivlahan DR, Marlatt GA. Brief alcohol screening and intervention for college students (BASICS): A harm reduction approach. New York, NY, US: Guilford Press; 1999. [Google Scholar]
- Doumas DM, Andersen LL. Reducing alcohol use in first-year university students: Evaluation of a web-based personalized feedback program. Journal of College Counseling. 2009;12(1):18–32. [Google Scholar]
- Finney JW, Monahan SC. The cost-effectiveness of treatment for alcoholism: A second approximation. Journal of Studies on Alcohol. 1996;57(3):229–243. doi: 10.15288/jsa.1996.57.229. [DOI] [PubMed] [Google Scholar]
- Godley MD, Kahn JH, Dennis ML, Godley SH, Funk RR. The stability and impact of environmental factors on substance use and problems after adolescent outpatient treatment for cannabis abuse or dependence. Psychology of Addictive Behaviors. 2005;19(1):62–70. doi: 10.1037/0893-164X.19.1.62. [DOI] [PubMed] [Google Scholar]
- Godley SH, Dennis ML, Godley MD, Funk RR. Thirty-month relapse trajectory cluster groups among adolescents discharged from out-patient treatment. Addiction. 2004;99:129–139. doi: 10.1111/j.1360-0443.2004.00860.x. [DOI] [PubMed] [Google Scholar]
- Godley SH, Meyers RJ, Smith JE, Karvinen T, Titus JC, Godley MD, Kelberg P. The adolescent community reinforcement approach for adolescent cannabis users, cannabis youth treatment (CYT) series, volume 4. Silver Spring, MD: Substance Abuse and Mental Health Services Administration; 2001. [Google Scholar]
- Handelsman L, Stein JA, Grella CE. Contrasting predictors of readiness for substance abuse treatment in adults and adolescents: A latent variable analysis of DATOS and DATOS-A participants. Drug and Alcohol Dependence. 2005;80(1):63–81. doi: 10.1016/j.drugalcdep.2005.03.022. [DOI] [PubMed] [Google Scholar]
- Holder H, Longabaugh R, Miller WR, Rubonis AV. The cost effectiveness of treatment for alcoholism: A first approximation. Journal of Studies on Alcohol. 1991;52(6):517–540. doi: 10.15288/jsa.1991.52.517. [DOI] [PubMed] [Google Scholar]
- Jasiukaitis P, Shane P. Discriminant analysis with GAIN-I psychological indices reproduces staff psychiatric diagnoses in an adolescent substance abusing sample. Persistent Effects of Treatmetn Study of Adolescents Analytic Cross-Site Meeting.2001. [Google Scholar]
- Juarez P, Walters ST, Daugherty M, Radi C. A randomized trial of motivational interviewing and feedback with heavy drinking college students. Journal of Drug Education. 2006;36(3):233–246. doi: 10.2190/753N-8242-727T-G63L. [DOI] [PubMed] [Google Scholar]
- Mason MJ, Luckey B. Young adults in alcohol-other drug treatment: An understudied population. Alcoholism Treatment Quarterly. 2003;21(1):17–32. [Google Scholar]
- Mee-Lee D, Gartner L, Miller MM, Shulman G, Wilford B. Patient placement criteria, second edition-revised (ASAM PPC-2R) Annapolis Junction, MD: American Society of Addiction Medicine; 2001. [Google Scholar]
- Melnick G, De Leon G, Hawke J, Jainchill N, Kressel D. Motivation and readiness for therapeutic community treatment among adolescents and adult substance abusers. American Journal of Drug and Alcohol Abuse. 1997;23(4):485–506. doi: 10.3109/00952999709016891. [DOI] [PubMed] [Google Scholar]
- Meyers RJ, Smith JE, editors. Clinical guide to alcohol treatment: The community reinforcement approach. New York, NY: Guilford Press; 1995. [Google Scholar]
- Miller WR, Brown JM, Simpson TL, Handmaker NS, Bien TH, Luckie LF, Tonigan J. What works? A methodological analysis of the alcohol treatment outcome literature. In: Hester RK, Miller WR, editors. Handbook of alcoholism treatment approaches: Effective alternatives. 2nd. Needham Heights, MA: Allyn & Bacon; 1995. pp. 12–44. [Google Scholar]
- Miller WR, Wilbourne PL. Mesa grande: A methodological analysis of clinical trials of treatment for alcohol use disorders. Addiction. 2002;97(3):265–277. doi: 10.1046/j.1360-0443.2002.00019.x. [DOI] [PubMed] [Google Scholar]
- Miller WR, Villanueva M, Tonigan JS, Cuzmar I. Are special treatments needed for special populations? Alcoholism Treatment Quarterly. 2007;25(4):63. doi: 10.1300/J020v25n04_05. [DOI] [Google Scholar]
- Monti PM, Barnett NP, Colby SM, Gwaltney CJ, Spirito A, Rohsenow DJ, Woolard R. Motivational interviewing versus feedback only in emergency care for young adult problem drinking. Addiction. 2007;102(8):1234–1243. doi: 10.1111/j.1360-0443.2007.01878.x. [DOI] [PubMed] [Google Scholar]
- Monti PM, Colby SM, Barnett NP, Spirito A, Rohsenow DJ, Myers M, Lewer W. Brief intervention for harm reduction with alcohol-positive older adolescents in a hospital emergency department. Journal of Consulting and Clinical Psychology. 1999;67(6):989–994. doi: 10.1037/0022-006X.67.6.989. [DOI] [PubMed] [Google Scholar]
- Muck R, Zempolich KA, Titus JC, Fishman M, Godley MD, Schwebel R. An overview of the effectiveness of adolescent substance abuse treatment models. Youth & Society. 2001;33(2):143–168. [Google Scholar]
- Roozen HG, Boulogne JJ, Van Tulder MW, Van Den Brink W, De Jong CAJ, Kerkhof AJFM. A systematic review of the effectiveness of the community reinforcement approach in alcohol, cocaine and opioid addiction. Drug and Alcohol Dependence. 2004;74(1):1–13. doi: 10.1016/j.drugalcdep.2003.12.006. [DOI] [PubMed] [Google Scholar]
- Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70(1):41–55. doi: 10.1093/biomet/70.1.41. [DOI] [Google Scholar]
- Rounsaville BJ, Petry NM, Carroll KM. Single versus multiple drug focus in substance abuse clinical trials research. Drug and Alcohol Dependence. 2003;70(2):117–125. doi: 10.1016/s0376-8716(03)00033-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saitz R, Palfai TP, Freedner N, Macdonald A, Ozonoff AL, Dejong W, Winter MR. Screening and brief intervention online for college students: The iHealth study. Alcohol and Alcoholism. 2007;42(1):28–36. doi: 10.1093/alcalc/agl092. [DOI] [PubMed] [Google Scholar]
- Satre DD, Mertens J, Areán PA, Weisner C. Contrasting outcomesof older versus middle-aged and younger adult chemical dependency patients in a managed care program. Journal of Studies on Alcohol. 2003;64:520–530. doi: 10.15288/jsa.2003.64.520. [DOI] [PubMed] [Google Scholar]
- Satre D, Mertens J, Arean P, Weisner Five-year alcohol and drug treatment outcomes of older adults versus middle-aged and younger adults in a managed care program. Addiction. 2004;99(10):1286–1297. doi: 10.1111/j.1360-0443.2004.00831.x. [DOI] [PubMed] [Google Scholar]
- Shanahan MJ, Porfeli EJ, Mortimer JT, Erickson LD. Subjective age identity and the transition to adulthood. In: Settersten RA Jr, Furstenberg FF Jr, Rumbaut RG, editors. On the frontier of adulthood: Theory, research and public policy. Chicago: University of Chicago Press; 2005. [Google Scholar]
- Sinha R, Easton C, Kemp K. Substance abuse treatment characteristics of probation-referred young adults in a community-based outpatient program. American Journal of Drug and Alcohol Abuse. 2003;29(3):585–597. doi: 10.1081/ADA-120023460. [DOI] [PubMed] [Google Scholar]
- Slesnick N, Prestopnik JL, Meyers RJ, Glassman M. Treatment outcome for street-living, homeless youth. Addictive Behaviors. 2007;32(6):1237–1251. doi: 10.1016/j.addbeh.2006.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith DC, Cleeland L, Dennis ML. Reasons for quitting among emerging adults and adolescents in substance-use-disorder treatment. Journal of Studies on Alcohol and Drugs. 2010;71(3):400–409. doi: 10.15288/jsad.2010.71.400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramaniam GA, Ives ML, Stitzer ML, Dennis ML. The added risk of opioid problem use among treatment-seeking youth with marijuana and/or alcohol problem use. Addiction. 2010;105(4):686–698. doi: 10.1111/j.1360-0443.2009.02829.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Treatment episode data set (TEDS): 1992–2005 : Concatenated data [computer file] 2007 [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the2007 national survey on drug use and health: National findings (office of applied studies, NSDUH series H-34, DHHS publication no. SMA 08-4343) Rockville, MD: Author; 2008. [Google Scholar]
- Waldron HB, Turner CW. Evidence-based psychosocial treatments for adolescent substance abuse. Journal of Clinical Child and Adolescent Psychology. 2008;37(1):238–261. doi: 10.1080/15374410701820133. [DOI] [PubMed] [Google Scholar]