Abstract
Objective
Osteoarthritis (OA) clinical practice guidelines identify a substantial therapeutic role for physical activity but objective information about the physical activity of this population is lacking. We objectively measured physical activity levels of adults with knee OA and report the prevalence of meeting public health physical activity guidelines.
Methods
Cross-sectional accelerometer data from 1111 adults with radiographic knee OA aged 49 to 84 years participating in Osteoarthritis Initiative accelerometer monitoring ancillary study were assessed for meeting the aerobic component of the 2008 Physical Activity Guidelines for Americans (≥150 minutes/week in episodes≥10 minutes). Quantile regression was used to test median gender differences in physical activity levels.
Results
Aerobic physical activity guidelines were met by 12.9% of men and 7.7% of women with knee OA. A substantial 40.1% of men and 56.5% of women were inactive, doing no moderate-to-vigorous (MV) activity over 7 days that lasted 10 minutes or more. Although men engaged in significantly more MV intensity activity (20.7 vs. 12.3 average daily minutes) they also spent more time in no or very light intensity activity (608.2 vs. 585.8 average daily minutes) than women.
Conclusion
Despite substantial health benefits from physical activity, adults with knee OA were particularly inactive based on objective accelerometer monitoring. The percentages of men and women who met public health physical activity guidelines were substantially less than previous reports based on self-reported activity in arthritis populations. These findings support intensified public health efforts to increase physical activity levels among persons with knee OA.
INTRODUCTION
Osteoarthritis (OA) is a major debilitating disease affecting more than 27 million persons in the United States (U.S.)1 This number is expected to increase due to the growing obesity epidemic and the greater numbers of adults who are reaching older ages, when the prevalence of arthritis is highest2–4. OA affecting the knee is currently a leading cause of disability in adults1,5,6.
OA clinical practice guidelines identify a substantial therapeutic role for physical activity in bone and joint health.7 Recent federal guidelines now include people with arthritis in the physical activity recommendations.8 Among persons with knee OA, physical activity conveys disease-specific benefits. Randomized clinical trials show that physical activity programs are effective to reduce pain, improve physical performance, reduce depressive symptoms, and prevent or delay disability in knee OA.9–11 In addition, physical activity conveys general health benefits.12 Randomized clinical trials in the general adult population show that physical activity reduces mortality and risk of various chronic diseases and can improve disease-related symptoms and complications such as pain, fatigue, functional limitation, and impaired sleep.8,13
Despite important health benefits of being physically active, persons with arthritis are particularly inactive and are at risk for poor health outcomes.14,15 In a national U.S. survey 44% of persons with arthritis were classified as inactive (i.e. reporting no sustained 10 minute periods of moderate or vigorous physical activity in a typical week) compared to 36% of adults without arthritis.16 These estimates were based on self-reported activity, which is prone to overestimated activity intensity and time spent in physical activity.17 Thus, currently available information may overestimate physical activity levels among adults with arthritis. Objective evidence on the physical activity experience of this population is needed to better understand the magnitude of the problem. The primary purpose of this study is to assess objectively-measured physical activity levels of adults with knee OA and report the prevalence of this population meeting public health physical activity guidelines. A secondary purpose is to assess the effects of gender, age, and body mass index on physical activity levels.
METHODS
Study Population
The participants for this physical activity study were a subcohort from the Osteoarthritis Initiative (OAI), a prospective study investigating risk factors and biomarkers associated with the development and progression of knee OA in men and women aged 45–79 years at enrollment, with or at high risk to develop knee OA. Annual OAI evaluations began in 2004 at four clinical sites: Baltimore Maryland, Columbus Ohio, Pittsburgh Pennsylvania, and Pawtucket Rhode Island and are currently ongoing.18 Institutional review board approval was obtained the participating OAI sites and at Northwestern University. Each participant provided written informed consent. The OAI excluded individuals with rheumatoid or inflammatory arthritis; severe joint space narrowing in both knees on the baseline knee radiograph, or unilateral total knee replacement and severe joint space narrowing in the other knee; bilateral total knee replacement or plans to have bilateral knee replacement in the next 3 years; inability to undergo a 3.0T magnetic resonance imaging (MRI) exam of the knee because of contraindications; positive pregnancy test; inability to provide a blood sample; use of ambulatory aides other than a single straight cane for more than 50% of the time during ambulation; comorbid conditions that might interfere with the ability to participate in a 4-year study; current participation in a double-blind randomized trial. All OAI participants underwent knee radiography at baseline using a “fixed-flexion” knee radiography protocol19 including bilateral, standing, posteroanterior knee films with knees flexed to 20–30° and feet internally rotated 10° using a plexiglass positioning frame. .Baseline films were assessed by clinic readers for OARSI atlas20 grades of tibiofemoral osteophytes and joint space narrowing. The baseline visit identified 2679 participants with radiographic evidence of knee OA (i.e., definite joint space narrowing, or OARSI atlas20 grade 1 or higher, osteophytes) in one or both knees from the total OAI enrollment of 4796 persons.
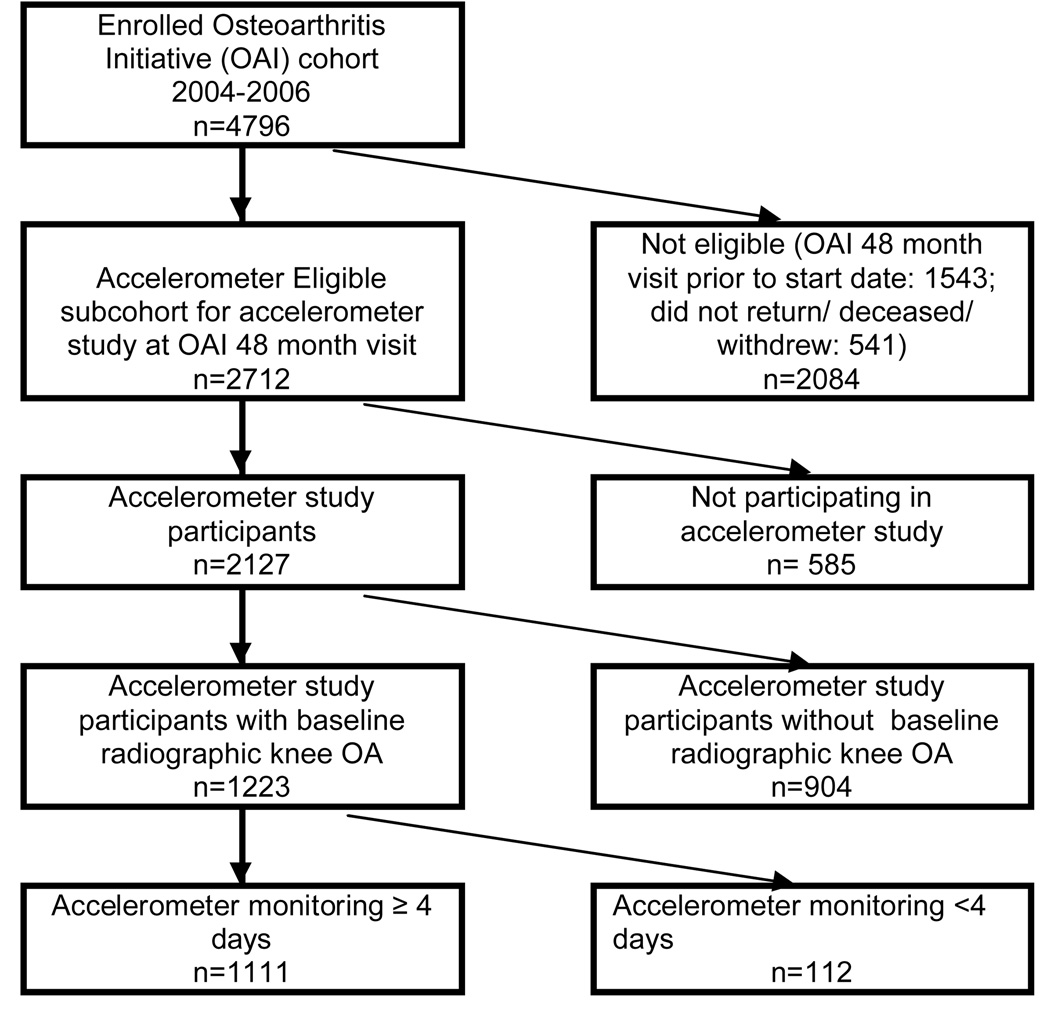
A physical activity study collected accelerometer data on a subcohort of OAI participants with and without radiographic OA at the scheduled 48-month follow-up visit. Eligibility required a scheduled OAI 48-month follow-up visit between August 2008 and July 2010, with staggered starting months across the OAI sites. A total of 2127 persons consented to participate in accelerometer monitoring representing 78.4% of eligible participants (2712). (Another 1543 OAI participants had visits that preceded the physical activity study start date and 541 were deceased/did not return at 48 months/ withdrew from OAI study). This report included 1223 participants with baseline radiographic knee OA (see Figure 1). Accelerometer data were merged with OAI public data (from baseline to the 48-month visit) containing information on participant characteristics.
Figure 1.
Flow chart of accelerometer study analytic sample of Osteoarthritis Initiative participants
Outcomes
Physical activity was measured at the OAI 48-month follow-up visit using a GT1M Actigraph accelerometer, a small uniaxial accelerometer that measures vertical acceleration and deceleration21. Uniaxial accelerometer validation studies against whole-body indirect calorimetry showed high correlation with metabolic equivalent (r=0.93) and total energy expenditure (r=0.93)22. The accuracy (walking speed23) and test-retest reliability24 of Actigraph accelerometers under field conditions have been established in many populations including persons with OA25. Accelerometer output is an activity count, which is the weighted sum of the number of accelerations measured over a time period (e.g. in this case 1 minute), where the weights are proportional to the magnitude of measured acceleration.
Trained research personnel initialized each accelerometer and gave instructions at an in-person visit, on how to position and wear the accelerometer. Participants were given uniform scripted instructions to wear the unit on a belt at the natural waistline on the right hip in line with the right axilla upon arising in the morning and continuously until retiring at night, except during water activities, for seven consecutive days. Participants maintained a daily log to record time spent in water and cycling activities, which may not be fully captured by accelerometers. At the end of the 7-day monitoring period, participants returned the accelerometers to the research center; data were downloaded using the manufacturer’s software, and were checked for valid data recording.
Covariates
Covariates were measured at the OAI 48 month visit. Demographic factors included race/ethnicity (African-American, White, or other), age, and gender. Body mass index (BMI) was calculated from measured height and weight [weight (kg)/height (m)2]. If BMI was missing at the 48-month visit, BMI from the 36-month OAI visit (4 participants, 0.4% cases) was used. Persons were classified as normal weight (BMI 18.5–24.9), overweight (BMI=25.0–29.9), or obese (BMI ≥ 30).
Pain measures included assessments of both current and chronic pain. Self-reported current knee pain was measured by a 5-point Likert scale (0=none, 1=slight, 2=moderate, 3=severe, 4=extreme) in the past 7 days from the WOMAC (Western Ontario and McMaster University OA Index, Likert version, 3.1, modified in the OAI to ask about the right and left knee symptoms separately26). The WOMAC pain score range was 0–20; a higher number represents worse symptoms. Current pain was the maximum of the left and right knee WOMAC pain scores. The presence of chronic knee pain symptoms was ascertained from a positive response to “Do you have pain, aching, or stiffness on most days of at least one month during the past 12 months.” If 48-month knee pain information was not available, information from the 36-month OAI visit (2 participants, 0.2% cases) was used.
Statistical analysis
Accelerometer data from each participant were analytically filtered to identify non-wear periods (a period the monitor was potentially removed) during a day and days with sufficient wear time to be analyzed. Non-wear periods were defined as ≥90 minutes with zero activity counts (allowing for two interrupted minutes with counts<100)27. A valid day of monitoring was defined as 10 or more wear hours in a 24-hour period.17 Although three days is the minimal period needed to provide a reliable estimate of physical activity,28 for this study, we conservatively included only participants who had four or more valid days of monitoring. These methods are consistent with accelerometer methodology used in the general population and have been validated in patients with rheumatic disease17,27,29.
Accelerometer data were scored for the purposes of standardization. We applied intensity thresholds used by the National Cancer Institute (NCI)17 on a minute-by-minute basis to classify accelerometer counts into four intensity levels: none to very light (0–99 counts), light (100–2019 counts), moderate (2020–5998 counts), and vigorous (5999 counts). Due to the low frequency of vigorous activity in this sample, only moderate-to-vigorous (MV) activity (≥ 2020 counts) is reported. MV activity increases both heart and breathing rates and is generally equivalent, at minimum, to brisk walking as when late to an appointment; while light activity typically does not produce an increase in breathing or heart rate and is generally equivalent to leisurely walking as in a grocery store.30 Total daily time (minutes) was summed for each intensity level. In addition, we calculated daily minutes of MV physical activity occurring in bouts; a bout was defined as 10 or more consecutive minutes above the 2020 count threshold, with allowance for interruptions of 1 or 2 min below threshold, consistent with NCI methodology.17 Weekly totals were summed from the daily totals or estimated as 7 times the average daily total for persons with 4 to 6 valid days of monitoring. Each person was classified according to the 2008 Physical Activity Guidelines for Americans27 physical activity levels: Meeting Recommendations (≥ 150 bouted MV activity minutes per week), Low Active (1–149 bouted MV activity minutes per week) or Inactive (zero bouted MV activity minutes per week)31. In addition, we examined the frequency of Very Active (≥ 300 bouted MV activity minutes per week), which is a level of activity associated with additional health benefits including weight loss31. Of note, the “inactive” classification is based on of the absence of MV activity bouts (i.e., zero MV activity that occurred in bouts lasting at least 10 minutes over 7 days). Therefore we evaluate time spent in specific activity intensities including no/very low intensity activities, such as sitting and standing.
Descriptive analyses of physical activity outcomes (time spent in physical activity intensity categories and meeting Guidelines) are presented separately for men and women because of recognized gender differences in physical activity patterns17. Group differences in percentages (noted in text by p-values) were tested using logistic regression. For physical activity outcomes, we utilized nonparametric quantile regression to test differences in group medians by gender due to asymmetrically distributed outcomes.32 Spearman’s rank correlation was used to calculate correlation coefficients between intensity outcomes. Recognizing that systematic differences between the participating (n=1223) and non-participating (n=1456) OAI radiographic knee OA cohort could influence our findings, we performed weighted analyses recommended by Hogan33 and Robins (findings available on request).34 Because results were very similar and trends were identical for weighted and unweighted analyses, for simplicity unweighted analyses were reported. All analyses were performed using SAS software version 9.2.
RESULTS
A total of 1223 persons aged 45–79 years with radiographic knee OA (67.8% of these had definite joint space narrowing, or the equivalent of Kelgren-Lawrence grade 3 or 4) at the baseline OAI visit consented to physical activity measurement using accelerometers at the 48 month OAI visit. Participants in this physical activity ancillary study compared to the non-participating OAI radiographic knee OA cohort had similar baseline age (62.1 versus 62.7 years), BMI (29.0 versus 29.9 kg/m2), but were more frequently male (45.4% vs. 39.0%), White (82.7% versus 74.6%), with slightly less pain (mean WOMAC pain 3.5 versus 4.5).
The analytic sample n=1111 (91.0%) used in this report had at least 4 valid days of accelerometer data (of these, 98.1% and 93.3% had at least 5 and at least 6 valid monitoring days, respectively). Characteristics of these study participants at the physical activity assessment (48 month visit) are shown in Table 1 by age and gender. Adults with knee OA in the under 70 year age groups were generally obese (40.7% men, 48.1% women) or overweight (45.6% men, 31.1% women). Among the oldest group, 70 years or older, obesity was less common (33.1% men, 26.7% women) than in the younger groups, but the frequency of overweight remained high (46.3% men, 42.5% women). Chronic knee pain was frequently reported (48.0% of men and 46.8% of women). The mean WOMAC pain score was 3.2 for both men and women.
Table 1.
Characteristics n=1111 physical activity study participants‡ with radiographic knee OA
| Characteristics | 49–59 years | 60–69 years | 70 years or older | ||||
|---|---|---|---|---|---|---|---|
| Male | Female | Male | Female | Male | Female | ||
| N | 163 | 146 | 166 | 214 | 175 | 247 | |
| Age in years: mean(SD) | 54.9 (2.9) | 54.3 (3.0) | 64.2 (3.0) | 64.9 (2.8) | 75.8 (3.8) | 75.7 (3.7) | |
| Race/Ethnicity: White (%) | 82.2% | 74.0% | 88.0% | 73.4% | 91.4% | 86.6% | |
| African American (%) | 15.3% | 22.6% | 9.6% | 24.3% | 6.9% | 11.3% | |
| Other (%) | 2.5% | 3.4% | 2.4% | 2.3% | 1.7% | 2.0% | |
| BMI: mean (SD) | 29.4 (4.3) | 30.0 (5.9) | 29.3 (4.1) | 30.3 (5.4) | 28.6 (3.9) | 27.5 (4.3) | |
| Normal† | 13.5% | 23.3% | 13.9% | 19.2% | 20.6% | 30.8% | |
| Overweight†† | 47.9% | 32.9% | 43.4% | 29.9% | 46.3% | 42.5% | |
| Obese††† | 38.7% | 43.8% | 42.8% | 50.9% | 33.1% | 26.7% | |
| Current knee pain mean (SD) | 3.3 (3.6) | 3.8 (4.2) | 2.9 (3.2) | 3.3 (3.8) | 3.3 (3.7) | 2.8 (3.4) | |
| Chronic knee symptoms (%) | 50.3% | 50.7% | 48.2% | 50.5% | 45.7% | 41.3% | |
Physical activity study conducted at the Osteoarthritis Initiative 48 month evaluation using accelerometer monitoring
Normal body mass index (BMI): 18.5–24.9 (includes 6 participants with BMI 17.2–18.4),
Overweight BMI: 25.0–29.9,
Obese BMI: >=30
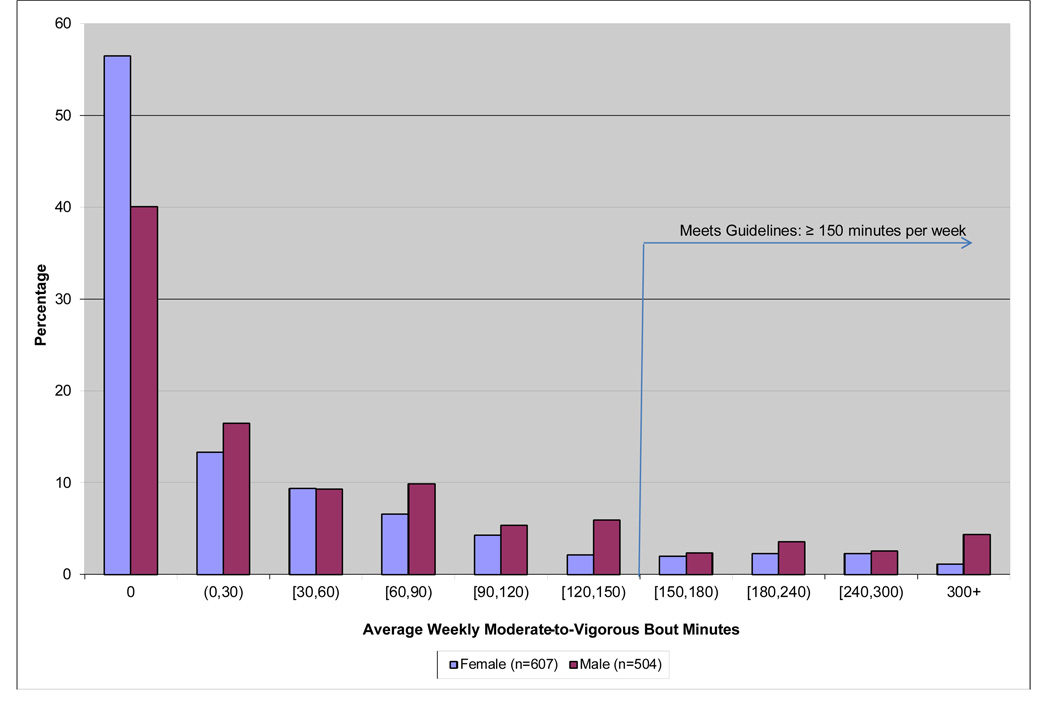
Time spent in activities of MV intensity that occur in episodes (i.e., bouts) lasting 10 minutes or longer is the metric on which physical activity guidelines are based. The distribution of bouted MV daily activity per week is shown by gender in Figure 2. Women were substantially more likely than men (56.5% versus 40.1%) not to participate in any bouts of MV activity over one week. In addition, men generally demonstrated more MV activity than women, including MV amounts that meet Guidelines (at least 150 bouted MV minutes per week).
Figure 2.
Distribution moderate-to-vigorous (MV) physical activity for men (n=504) and women (n=607) with radiographic knee OA having 4 or more valid days of accelerometer monitoring
Physical activity levels based on Guidelines are summarized in Table 2. Men are significantly more likely than women to meet Guidelines (12.9% vs. 7.7%, p=.005) or be in the Low Active group (47.0% vs. 35.8%, p<.001). Women are significantly more likely to be Inactive than men (56.5% vs. 40.1%, p<.001), accumulating no bouts of MV activity during the week. Significant gender differences persisted after controlling for age, BMI, current knee pain, and chronic knee pain (not shown). Further analyses found no interaction between gender, age, or BMI with current or chronic knee pain in relation to physical activity levels. For both men and women, the prevalence of meeting Guidelines decreased with increasing BMI. Prevalence of meeting Guidelines was similar for age groups under age 70 years (age 49–59: 12.0%, age 60–69: 11.3%), but markedly lower after age 70 (7.6%). Sensitivity analyses in the accelerometer study group without knee OA at baseline (n=826 with 4 or more valid days of accelerometer monitoring) also showed that Guidelines were met more frequently by men (22.0%) than women (10.8%).
Table 2.
Physical activity levels based on the 2008 Physical Activity Guidelines for Americans among men (n=504‡) and women (n=607‡) with radiographic knee OA
| Characteristics | Sample Size |
Inactive (No bouts of MV‡‡ min/week) |
Low Active (<150 bouted MV min/week) |
Active, meeting Guidelines (≥150 bouted MV min/week) |
Very Active (≥300 bouted MV min/week) |
|
|---|---|---|---|---|---|---|
| Men | ||||||
| n | % [95% CI] | % [95% CI] | % [95% CI] | % [95% CI] | ||
| Overall | 504 | 40.1 [35.8, 44.4] | 47.0 [42.6, 51.4] | 12.9 [10.0, 15.8] | 4.4 [2.6, 6.2] | |
| Age in years | ||||||
| 49–59 | 163 | 25.2 [18.5, 31.9] | 60.1 [52.6, 67.6] | 14.7 [9.3, 20.1] | 6.1 [2.4, 9.8] | |
| 60–69 | 166 | 34.3 [27.1, 41.5] | 50.6 [43.0, 58.2] | 15.1 [9.7, 20.5] | 4.8 [1.5, 8.1] | |
| >=70 | 175 | 59.4 [52.1, 66.7] | 31.4 [24.5, 38.3] | 9.1 [4.8, 13.4] | 2.3 [0.1, 4.5] | |
| BMI | ||||||
| Normal† | 81 | 30.9 [20.8, 41.0] | 46.9 [36.0, 57.8] | 22.2 [13.1, 31.3] | 8.6 [2.5, 14.7] | |
| Overweight†† | 231 | 34.2 [28.1, 40.3] | 50.7 [44.3, 57.1] | 15.2 [10.6, 19.8] | 4.3 [1.7, 6.9] | |
| Obese††† | 182 | 51.0 [43.9, 58.1] | 42.7 [35.7, 49.7] | 6.3 [2.9, 9.7] | 2.6 [0.3, 4.9] | |
| Women | ||||||
| Overall | 607 | 56.5 [52.6, 60.4] | 35.8 [32.0, 39.6] | 7.7 [5.6, 9.8] | 1.2 [0.3, 2.1] | |
| Age in years | ||||||
| 49–59 | 146 | 43.8 [35.8, 51.8] | 47.3 [39.2, 55.4] | 8.9 [4.3, 13.5] | 2.1 [−0.2, 4.4] | |
| 60–69 | 214 | 49.5 [42.8, 56.2] | 42.1 [35.5, 48.7] | 8.4 [4.7, 12.1] | 0.5 [−0.4, 1.4] | |
| >=70 | 247 | 70.0 [64.3, 75.7] | 23.5 [18.2, 28.8] | 6.5 [3.4, 9.6] | 1.2 [−0.2, 2.6] | |
| BMI | ||||||
| Normal# | 151 | 39.1 [31.3, 46.9] | 45.7 [37.8, 53.6] | 15.2 [9.5, 20.9] | 2.0 [−0.2, 4.2] | |
| Overweight | 217 | 54.8 [48.2, 61.4] | 35.9 [29.5, 42.3] | 9.2 [5.4, 13.0] | 1.4 [−0.2, 3.0] | |
| Obese | 239 | 69.0 [63.1, 74.9] | 29.3 [23.5, 35.1] | 1.7 [0.1, 3.3] | 0.4 [−0.4, 1.2] | |
4 or more valid days of accelerometer monitoring;
Moderate-to-Vigorous physical activity occurring in activity bouts of 10 minutes or more;
Normal body mass index (BMI): 18.5–24.9;
Overweight BMI: 25.0–29.9;
Obese BMI: >=30;
includes 6 participants with BMI 17.2–18.4.
Recognizing that the classification of inactivity is solely based on the absence of bouts of MV activity, we further investigated time spent non-bouted MV minutes, as well as in lower intensity activities. Table 3 summarizes the time spent per day in no/very light, light, and MV (non-bouted) intensity activities for men and women, respectively. Men spent significantly more time per day than women (608.2 vs. 585.8 average daily minutes) in no/very light activity, but less time in light intensity activity (262.2 vs. 288.2 average daily minutes). Men also spent significantly more time in both non-bouted MV activity (20.7 vs. 12.3 average daily minutes) and bouted MV activity (9.2 vs. 5.4 average daily minutes) compared to women. As expected, Table 3 also demonstrates that time spent in light and MV activity tended to decrease while no/very low activity time increased with older age and higher BMI. Time spent in no/very light activity was more strongly correlated with light activity time (r =−0.48) than MV time (r=−0.21) or bouted MV time (r=−0.11) (not shown). Because accelerometers were removed for water activities and may underestimate activities such as cycling, further analyses examined diary information (completed by 98.0% of participants) to determine the extent of these activities. Participants spent a median time of 0 minutes per day (interquartile range 0 to 3.6 minutes) in such activities, which indicates that non-monitored or underestimated activity was negligible.
Table 3.
Time per day spent in physical activity, by intensity, among 504 men‡ and 607 women‡ with radiographic OA
| Baseline Characteristics |
n | No to Very Light Intensity Activity a Mean Daily Minutes (SD) |
Light Intensity Activity b Mean Daily Minutes (SD) |
Moderate-to- Vigorous (MV) Intensity Activityc Mean Daily Minutes (SD) |
MV Intensity Activity boutsd Mean Daily Minutes (SD) |
|
|---|---|---|---|---|---|---|
| Men | ||||||
| Men Overall | 504 | 608.2 (90.9) | 262.2 (75.2) | 20.7 (20.7) | 9.2 (14.7) | |
| Age in years | ||||||
| 49–59 | 163 | 599.4 (96.0) | 278.0 (75.1) | 28.6 (22.7) | 11.6 (15.6) | |
| 60–69 | 166 | 601.6 (89.9) | 275.5 (66.4) | 22.2 (18.9) | 10.1 (13.7) | |
| >=70 | 175 | 622.7 (85.4) | 234.9 (75.8) | 11.9 (16.7) | 6.0 (14.2) | |
| Weight Status | ||||||
| Normal† | 81 | 604.7 (93.3) | 271.1 (81.8) | 25.6 (25.4) | 13.0 (19.0) | |
| Overweight†† | 231 | 603.2 (85.9) | 268.9 (69.9) | 22.9 (19.7) | 10.5 (13.5) | |
| Obese††† | 192 | 615.8 (95.5) | 250.4 (77.3) | 16.0 (18.7) | 6.0 (13.3) | |
| Women | ||||||
| Women Overall | 607 | 585.8 (95.6) | 288.2 (80.6) | 12.3 (14.3) | 5.4 (10.9) | |
| Age in years | ||||||
| 49–59 | 146 | 570.1 (102.7) | 319.8 (82.6) | 19.8 (14.8) | 7.1 (11.5) | |
| 60–69 | 214 | 579.5 (92.1) | 297.5 (73.5) | 11.9 (11.7) | 5.6 (9.5) | |
| >=70 | 247 | 600.4 (92.6) | 261.5 (76.9) | 8.3 (14.4) | 4.2 (11.6) | |
| Weight Status | ||||||
| Normal# | 151 | 590.1 (93.0) | 282.8 (68.2) | 17.1 (17.8) | 9.4 (14.8) | |
| Overweight | 217 | 587.8 (95.7) | 292.0 (81.9) | 12.5 (14.5) | 5.7 (10.9) | |
| Obese | 239 | 581.1 (97.4) | 288.2 (86.5) | 9.0 (10.3) | 2.5 (6.3) | |
4+ valid days of accelerometer monitoring;
counts 0–99/minute;
counts 100–2019/minute;
counts≥2020/minute not restricted to bouts;
bouts of 10 or more consecutive minutes above the 2020 count threshold;
Normal body mass index (BMI): 18.5–24.9;
Overweight BMI: 25.0–29.9;
Obese BMI: ≥30
includes 6 participants with BMI 17.2–18.4.
Table 4 reports gender differences in time engaged in different intensities of physical activity controlling for factors (BMI, WOMAC pain, chronic knee pain, demographic characteristics) that may affect physical activity level. Men with knee OA spent significantly more time in no/very light activity (28.9 average daily minutes) and MV activity (4.6 average daily minutes) than women. However, women spent more time in light activity (33.4 average daily minutes) than men. Further analyses examined gender differences within age and BMI weight groups. Across all age groups and BMI categories, women spent significantly more time in light activity while men spent more time in MV activity. In addition, men spent more time in no/very light activities than women; those differences were statistically significant or achieved borderline significance. Sensitivity analyses that further controlled for radiographic OA severity from the baseline visit (results not shown) yielded almost identical results.
Table 4.
Men versus Women: Median difference in physical activity minutes per day by intensity level, adjusted for age, race, body mass index (BMI), current pain severity, and chronic pain symptoms among n=1111‡ persons with radiographic knee OA
| Men vs. Women Difference |
n | No to Very Low Intensity Activitya Adjusted Difference Minutes/day (95% CI‡‡) |
Light Intensity Activity b Adjusted Difference Minutes/day (95% CI) |
Moderate-to- Vigorous (MV) Intensity Activityc Adjusted Difference Minutes/day (95% CI) |
MV Intensity Activity boutsd Adjusted Difference Minutes/day (95% CI) |
|---|---|---|---|---|---|
| Overall * | 1111 |
28.9 (16.1, 41.6) |
−33.4 (−42.4, −24.4) |
4.6 (3.2, 6.1) |
1.1 (0.6, 1.5) |
| Age Groups ** | |||||
| 49–59 | 309 | 18.7 (−3.8, 41.3) |
−36.4; (−58.4, −14.4) |
6.3 (1.5, 11.2) |
3.6 (2.9, 4.4) |
| 60–69 | 380 |
35.2 (8.4, 61.9) |
−21.7 (−35.5, −8.0) |
9.8 (6.2, 13.4) |
1.9 (1.2, 2.6) |
| 70+ | 422 |
31.0 (13.8, 48.2) |
−29.2 (−53.1, −5.3) |
2.5 (1.2, 3.8) |
0.5 (−0.2, 1.1) |
| Weight Status *** | |||||
| Normal† | 232 | 23.1 (−2.9, 49.0) |
−24.1 (−49.1, 0.9) |
4.4 (0.6, 8.2) |
0.6 (0.1, 1.0) |
| Overweight †† | 448 | 18.8 (−0.3, 38.0) |
−30.3 (−41.4, −19.2) |
7.4 (4.7, 10.0) |
1.6 (1.2, 2.1) |
| Obese††† | 431 |
40.7 (19.3, 62.0) |
−37.7 (−54.1, −21.4) |
1.8 (0.1, 3.6) |
0.6 (−0.1, 1.3) |
counts 0–99/minute;
counts 100–2019/minute;
counts≥2020/minute not restricted to bouts of activity;
bouts of 10 or more consecutive minutes above the 2020 count threshold;
4+ valid days of accelerometer monitoring
A 95% confidence interval that excludes 0 indicates a statistically significant gender difference.
Men versus women median difference adjusted for age, weight status, race, knee symptoms, and pain with associated 95% confidence interval (CI) estimated from quantile regression
Men versus women median difference in average daily minutes adjusted for weight status, race, knee symptoms, and pain with associated 95% CI estimated from quantile regression; statistical significance is indicated by CIs that exclude 0, which are bolded
Men versus women median difference in average daily minutes adjusted for age, race, knee symptoms, and pain with associated 95% CI estimated from quantile regression
Normal BMI: 18.5–24.9 (includes 6 participants with BMI 17.2–18.4),
Overweight BMI: 25.0–29.9,
Obese BMI≥30
DISCUSSION
These findings report on the prevalence of meeting the Physical Activity Guidelines for Americans aerobic recommendations and on time spent in different physical activity intensity levels using objectively measured accelerometer data among adults with radiographic knee OA. Despite substantial evidence showing that health benefits are related to physical activity, persons with knee OA participated in little physical activity. Less than one of seven men and one of twelve women with knee OA accumulated sufficient physical activity to meet the Guidelines. More than one-third of men and more than half the women were completely inactive, doing no sustained MV activity that lasted 10 minutes or more. Although men compared to women engaged in significantly more daily minutes of MV intensity activity they also accrued significantly more time engaged in no/very light intensity activities than women. These findings point to the urgent need for widespread dissemination of public health interventions to reduce the sedentary lifestyle of the 27 million adults with knee OA.
This study based on objectively measured physical activity using accelerometers found that 12.9% of men and 7.7% of women with radiographic knee OA met the current Guidelines. This finding indicates the vast majority of adults with knee OA are not participating in guideline recommendations to benefit overall health (e.g. mortality reduction from cardiovascular disease). National data on self-reported physical activity from the 2002 National Health Interview Survey (NHIS) found that 30% of adults age 18+ with self-reported doctor-diagnosed arthritis met physical activity recommendations.16 Self-reported physical activity information from the 2000 and 2001 Behaviors Risk Factor Surveillance Survey (BRFSS) state surveys showed that 22%-40% of adults age 45+ with self-reported doctor-diagnosed arthritis met recommended levels.35,36 One clinical study that objectively assessed physical activity using accelerometers (n=259) found that 30% of adults aged 35–65 years with confirmed early knee OA accumulated at least 30 minutes/day MV activity. However that study did not assess bouted MV activity, the metric for public health recommendations, which comprises less than one-half of overall MV activity in adults over age 40.17 Our results applying the current Guidelines (at least 150 bouted minutes MV activity per week) to objective accelerometer assessments from a knee OA cohort indicated that a much lower proportion met physical activity recommendations than these previous reports in arthritis populations. Consistent with these knee OA findings, a sensitivity analysis using the OAI accelerometer sample without baseline knee OA showed a lower proportion met current Guidelines (15.7%) based on objective assessment than estimates from the 2002 NHIS sample without arthritis (38% met recommendations) based on self-reported physical activity.16
There may be several reasons why our prevalence estimates of meeting physical activity recommendations among adults with arthritis are lower than previous prevalence estimates. First and arguably the strongest contributor to differences is that these previous population-based estimates used self-reports of physical activity to assess if physical activity guidelines were met, in contrast to the current study based on objectively measured physical activity. Self-reports of physical activity have been shown to overestimate objectively measured physical activity in the general population, particularly in older, obese individuals.37;38 Second, prior to the 2008 Guidelines, meeting physical activity recommendations required stricter criteria based on engaging in 30 minutes or more per day of bouted [episodes lasting at least 10 minutes] moderate intensity activity on 5 or more days of the week (5×30) or 20 minutes of vigorous intensity activity on 3 or more days per week (3×20).39 Persons that did some moderate intensity or vigorous intensity activity but not enough to meet either the 5×30 or the 3×20 criteria would be classified as not meeting physical activity recommendations. In practice, this issue likely has little effect since we summed all moderate and vigorous intensity activity before applying the 150 minutes/week Guideline recommendation and still found very low rates of meeting recommendations. Third, the case definition of arthritis used in national health surveys such as the NHIS and BRFSS include persons with OA, rheumatoid arthritis, lupus, fibromyalgia, and gout, while our study used a strict case definition of radiographic knee OA. It is not known how much the prevalence of meeting physical activity recommendations varies among different types of arthritis. However, OA is the most common type of arthritis in the US and would be the predominant type of arthritis represented in those national samples. Last, the NHIS national health survey included adults with arthritis as young as 18 years, while our study evaluated participants aged 49+ who may be less active than younger adults. However 30% of that NHIS arthritis population met physical activity guidelines, which is comparable to the 22%–40% of the BRFSS arthritis population of adults age 45+ meeting guidelines, so it is likely that differences due to a wider age span are small.
A substantial 40.1% of men and 56.5% of women were classified inactive, having no MV episodes that lasted 10 minutes or longer. These results are consistent with the 2002 NHIS findings that classified 40.0% of men and 45.8% of women with arthritis as inactive based on their self-reported activity.16 Our study confirms these previous estimates using an objective measure of activity. Although no minimum dose of MV activity that results in health benefits has been identified for adults with arthritis specifically, just moving from inactive to low active (1–149 bouted MV minutes per week) has been shown to have substantial benefits including reduced mortality and risk for incident coronary heart disease, hypertension and diabetes. For example, as little as 60–90 minutes per week of MV physical activity lowers the risk of premature mortality by approximately 25%.27 This health benefit, coupled with the fact that moderate, low impact exercise has been proven safe and effective for adults with arthritis, affirms the Healthy People 2020 recommendation that adults with OA should be counseled to be as physically active as possible (i.e., avoid inactivity) even if they may never intend to engage in sufficient activity to meet recommendations.40 Indeed, the avoidance of time spent in no or very light activity may be the first realistic goal for those with knee pain/mobility issues.
Research on physical activity has largely concentrated on time spent in MV activity. However that focus neglects the potential health benefits of time spent in light-intensity activities over no or very light intensity activity such as sitting. Physiologically, unbroken absence of activity suppresses skeletal muscle lipoprotein lipase (LPL) activity and reduces glucose uptake41,42. Time spent no/very light activity is associated with a larger waist circumference, poor 2-hour plasma glucose levels, triglyceride profiles, and increased metabolic risk scores.43,44 Being sedentary can have adverse effects even among otherwise physically active people. In a study of over 4000 adults from the Australian Diabetes, Obesity, and Lifestyle study, longer television time was significantly associated with larger waist circumference, higher systolic blood pressure and 2-hour plasma glucose, even among active adults who reported activity levels compatible with guidelines.44 We found a negative correlation between no/very light activity time and light activity in this knee OA cohort (r=−0.48), which was stronger than its correlation with MV activity time. Trading sitting activities for light intensity activities such as gardening or leisurely walking may be an intermediate step to change undesirable behaviors mediated through improved self-efficacy. This strategy may be particularly helpful for adults with arthritis who fear their symptoms will become worse through increased activity levels. Once they have been successful at replacing time spent in no/very light intensity activities with light activity, counseling efforts can be targeted to increasing the intensity of activity. In addition, any movement beyond lying or sitting contributes to total daily energy expenditure; increased activity when coupled with dietary caloric restriction may produce weight loss. These potential benefits motivate the promotion of light to moderate intensity activities in persons with knee OA as a feasible approach to reduce no/very light activity time and possibly improve health outcomes.
This study had substantial strengths which include the large sample size, the objective accelerometer assessment of physical activity, radiographic verification of knee OA, and the age and gender diversity of this OA cohort. There are limitations to acknowledge in the present study. Accelerometers do not provide qualitative information on context of the physical activity (e.g., household, transportation, outdoor location), information which may be helpful to target interventions. While accelerometer information could assess the aerobic component of the physical activity guideline recommendation, it is not known if that activity was accomplished using low impact activities as advised for people with arthritis; nor could it assess the muscle-strengthening component of the recommendation. The accelerometer model used in this study cannot capture water activities and may underestimate upper body movement or vertical acceleration/deceleration activities, such as cycling. Diary information indicated that the median time this sample spent in water and cycling activities was 0 minutes/day, so the potential underestimate is negligible. It is possible that wearing an accelerometer may made individuals more aware of activity, providing a stimulus to participate in physical activity. To minimize such effects the accelerometer provided no feedback to the participant on monitored activity. If participation rates were inflated due to the presence of the monitor, the true day to day physical activity levels would be even lower than those observed. Radiographic data on joint damage were only available from baseline, 4 years prior to the current study. Sensitivity analyses that controlled for baseline radiographic status showed similar statistical differences to the reported findings. Last, it is recognized that adults not measured in the OAI physical activity ancillary study were more likely to be female, African American, and had greater baseline pain than study participants. Because these differential characteristics are associated with lower levels of physical activity, our findings represent a conservative upper bound on physical activity levels for adults with knee OA. However sensitivity analyses that accounted for these differential characteristics among the unmeasured group yielded similar estimates and identical trends, suggesting that any bias in our findings is small.
CONCLUSION
Despite substantial health benefits related to physical activity, adults with radiographic knee OA were particularly inactive. Only 12.9% of men and 7.7% of women met public health physical activity guidelines based on objective assessment; these estimates were substantially below previous reports based on self-reported activity in arthritis populations. Although men compared to women engaged in significantly more MV intensity activity, they also spent significantly more time in no/very light intensity activity. A substantial 40.1% of men and 56.5% of women were classified as inactive, participating in no episodes of MV activity lasting over 10 minutes. These findings demonstrate the critical need to intensify public health efforts to increase physical activity and reduce sedentary time in both men and women with knee OA.
ACKNOWLEDGEMENTS
This study is supported in part by National Institute for Arthritis and Musculoskeletal Diseases (grant no. P60-AR48098, R01-AR055287, R01-AR054155, and R21-AR059412) and the Falk Medical Research Trust. The OAI is a public-private partnership comprised of five contracts (N01-AR-2-2258; N01-AR-2-2259; N01-AR-2-2260; N01-AR-2-2261; N01-AR-2-2262) funded by the National Institutes of Health, a branch of the Department of Health and Human Services, and conducted by the OAI Study Investigators. Private funding partners include Merck Research Laboratories; Novartis Pharmaceuticals Corporation, GlaxoSmithKline; and Pfizer, Inc. Private sector funding for the OAI is managed by the Foundation for the National Institutes of Health. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the OAI.
References
- 1.Lawrence RC, Felson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008 Jan;58(1):26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. U.S. Obesity Trends. [Accessed April 11, 2011]; http://www.cdc.gov/obesity/data/trends.html.
- 3.U.S. Department of Commerce. Unprecedented Global Aging Examined in New Census Bureau Report Commissioned by the National Institute on Aging. [Accessed April 11, 2011];U.S. Census Bureau News. http://www.nih.gov/news/health/jul2009/nia-20.htm.
- 4.Hootman JM, Helmick CG. Projections of US prevalence of arthritis and associated activity limitations. Arthritis Rheum. 2006 Jan;54:226–229. doi: 10.1002/art.21562. [DOI] [PubMed] [Google Scholar]
- 5.Yelin E. Cost of musculoskeletal diseases: impact of work disability and functional decline. J Rheumatol Suppl. 2003 Dec;68:8–11. [PubMed] [Google Scholar]
- 6.Felson DT, Lawrence RC, Dieppe PA, et al. Osteoarthritis: new insights. Part 1: the disease and its risk factors. Ann Intern Med. 2000 Oct 17;133:635–646. doi: 10.7326/0003-4819-133-8-200010170-00016. [DOI] [PubMed] [Google Scholar]
- 7.American College of Rheumatology Subcommittee on Osteoarthritis Guidelines. Recommendations for the medical management of osteoarthritis of the hip and knee: 2000 update. Arthritis Rheum. 2000 Sep;43(9):1905–1915. doi: 10.1002/1529-0131(200009)43:9<1905::AID-ANR1>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 8.Physical Activity Guidelines Advisory Committee. Physical Activity Guidelines Advisory Committee Report. Washington, DC: U.S. Department of Health and Human Services; 2008. [DOI] [PubMed] [Google Scholar]
- 9.Deyle GD, Henderson NE, Matekel RL, Ryder MG, Garber MB, Allison SC. Effectiveness of manual physical therapy and exercise in osteoarthritis of the knee. A randomized, controlled trial. Ann Intern Med. 2000 Feb 1;132(3):173–181. doi: 10.7326/0003-4819-132-3-200002010-00002. [DOI] [PubMed] [Google Scholar]
- 10.Ettinger WH, Jr, Burns R, Messier SP, et al. A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis. The Fitness Arthritis and Seniors Trial (FAST) Jama. 1997 Jan 1;277:25–31. [PubMed] [Google Scholar]
- 11.Penninx BW, Rejeski WJ, Pandya J, et al. Exercise and depressive symptoms: a comparison of aerobic and resistance exercise effects on emotional and physical function in older persons with high and low depressive symptomatology. J Gerontol B Psychol Sci Soc Sci. 2002 Mar;57:P124–P132. doi: 10.1093/geronb/57.2.p124. [DOI] [PubMed] [Google Scholar]
- 12.Nelson ME, Rejeski WJ, Blair SN, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007 Aug;39(8):1435–1445. doi: 10.1249/mss.0b013e3180616aa2. [DOI] [PubMed] [Google Scholar]
- 13.King AC, Oman RF, Brassington GS, Bliwise DL, Haskell WL. Moderate-intensity exercise and self-rated quality of sleep in older adults. A randomized controlled trial. Jama. 1997 Jan 1;277(1):32–37. [PubMed] [Google Scholar]
- 14.Fontaine KR, Heo M, Bathon J. Are US adults with arthritis meeting public health recommendations for physical activity? Arthritis Rheum. 2004 Feb;50:624–628. doi: 10.1002/art.20057. [DOI] [PubMed] [Google Scholar]
- 15.Keysor JJ. Does late-life physical activity or exercise prevent or minimize disablement? A critical review of the scientific evidence. Am J Prev Med. 2003 Oct;25:129–136. doi: 10.1016/s0749-3797(03)00176-4. [DOI] [PubMed] [Google Scholar]
- 16.Shih M, Hootman JM, Kruger J, Helmick CG. Physical activity in men and women with arthritis National Health Interview Survey, 2002. Am J Prev Med. 2006 May;30:385–393. doi: 10.1016/j.amepre.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 17.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008 Jan;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 18.Lester G. Clinical research in OA--the NIH Osteoarthritis Initiative. J Musculoskelet Neuronal Interact. 2008 Oct–Dec;8(4):313–314. [PubMed] [Google Scholar]
- 19.Peterfy C, Li J, Zaim S, et al. Comparison of fixed-flexion positioning with fluoroscopic semi-flexed positioning for quantifying radiographic joint-space width in the knee: test-retest reproducibility 3. Skeletal Radiol. 2003 Mar;32:128–132. doi: 10.1007/s00256-002-0603-z. [DOI] [PubMed] [Google Scholar]
- 20.Altman RD, Hochberg M, Murphy WA, Jr, Wolfe F, Lequesne M. Atlas of individual radiographic features in osteoarthritis. Osteoarthritis Cartilage. 1995 Sep;3 Suppl A:3–70. [PubMed] [Google Scholar]
- 21.Matthews CE, Ainsworth BE, Thompson RW, Bassett DR., Jr Sources of variance in daily physical activity levels as measured by an accelerometer. Med Sci Sports Exerc. 2002 Aug;34:1376–1381. doi: 10.1097/00005768-200208000-00021. [DOI] [PubMed] [Google Scholar]
- 22.Kumahara H, Schutz Y, Ayabe M, et al. The use of uniaxial accelerometry for the assessment of physical-activity-related energy expenditure: a validation study against whole-body indirect calorimetry. The British journal of nutrition. 2004 Feb;91(2):235–243. doi: 10.1079/BJN20031033. [DOI] [PubMed] [Google Scholar]
- 23.Brage S, Wedderkopp N, Franks PW, Andersen LB, Froberg K. Reexamination of validity and reliability of the CSA monitor in walking and running. Med Sci Sports Exerc. 2003 Aug;35(8):1447–1454. doi: 10.1249/01.MSS.0000079078.62035.EC. [DOI] [PubMed] [Google Scholar]
- 24.Welk GJ, Schaben JA, Morrow JR., Jr Reliability of accelerometry-based activity monitors: a generalizability study. Med Sci Sports Exerc. 2004 Sep;36(9):1637–1645. [PubMed] [Google Scholar]
- 25.Farr JN, Going SB, Lohman TG, et al. Physical activity levels in patients with early knee osteoarthritis measured by accelerometry. Arthritis Rheum. 2008 Sep 15;59(9):1229–1236. doi: 10.1002/art.24007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McGrory BJ, Harris WH. Can the western Ontario and McMaster Universities (WOMAC) osteoarthritis index be used to evaluate different hip joints in the same patient? 7. J Arthroplasty. 1996 Oct;11:841–844. doi: 10.1016/s0883-5403(96)80184-7. [DOI] [PubMed] [Google Scholar]
- 27.Hootman JM. Planned periodic CDC revision of phyblic health recommendations. Chicago IL: 2010. [Google Scholar]
- 28.Trost SG, McIver KL, Pate RR. Conducting accelerometer-based activity assessments in field-based research. Med Sci Sports Exerc. 2005 Nov;37(11 Suppl):S531–S543. doi: 10.1249/01.mss.0000185657.86065.98. [DOI] [PubMed] [Google Scholar]
- 29.Semanik P, Song J, Chang RW, Manheim L, Ainsworth B, Dunlop D. Assessing physical activity in persons with rheumatoid arthritis using accelerometry. Med Sci Sports Exerc. 2010 Aug;42(8):1493–1501. doi: 10.1249/MSS.0b013e3181cfc9da. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ainsworth BE, Haskell WL, Whitt MC, et al. Compendium of physical activities: an update of activity codes and MET intensities 9 Suppl. Med Sci Sports Exerc. 2000 Sep;32:S498–S504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 31.Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans. Department of Health and Human Services USA; 2008. Oct, 2008. [Google Scholar]
- 32.Buchinsky M. Recent Advances in Quantile Regression Models: A Practical Guideline for Empirical Research. The Journal of Human Resources. 1998 Winter;33:88–126. [Google Scholar]
- 33.Hogan JW, Roy J, Korkontzelou C. Handling drop-out in longitudinal studies. Stat Med. 2004 May 15;23(9):1455–1497. doi: 10.1002/sim.1728. [DOI] [PubMed] [Google Scholar]
- 34.Robins JM, Rotnitzky A, Zhao LP. Analysis of semiparametric regression models for repeated outcomes in the presence of missing data. Journal of the American Statistical Association. 1995;90:106–121. [Google Scholar]
- 35.Hootman JM, Macera CA, Ham SA, Helmick CG, Sniezek JE. Physical activity levels among the general US adult population and in adults with and without arthritis. Arthritis Rheum. 2003 Feb 15;49:129–135. doi: 10.1002/art.10911. [DOI] [PubMed] [Google Scholar]
- 36.Fontaine KR, Heo M. Changes in the prevalence of US adults with arthritis who meet physical activity recommendations, 2001–2003. J Clin Rheumatol. 2005 Feb;11:13–16. doi: 10.1097/01.rhu.0000152143.25357.fe. [DOI] [PubMed] [Google Scholar]
- 37.Conway JM, Seale JL, Jacobs DR, Jr, Irwin ML, Ainsworth BE. Comparison of energy expenditure estimates from doubly labeled water, a physical activity questionnaire, and physical activity records 3. Am J Clin Nutr. 2002 Mar;75:519–525. doi: 10.1093/ajcn/75.3.519. [DOI] [PubMed] [Google Scholar]
- 38.Irwin ML, Ainsworth BE, Conway JM. Estimation of energy expenditure from physical activity measures: determinants of accuracy 9. Obes Res. 2001 Sep;9:517–525. doi: 10.1038/oby.2001.68. [DOI] [PubMed] [Google Scholar]
- 39.Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007 Aug;39(8):1423–1434. doi: 10.1249/mss.0b013e3180616b27. [DOI] [PubMed] [Google Scholar]
- 40.U.S. Department of Health and Human Services. Healthy People 2010:Understanding and improving health (2nd edition) Washington, D.C: 2003. [Google Scholar]
- 41.Bey L, Hamilton MT. Suppression of skeletal muscle lipoprotein lipase activity during physical inactivity: a molecular reason to maintain daily low-intensity activity. The Journal of physiology. 2003 Sep 1;551(Pt 2):673–682. doi: 10.1113/jphysiol.2003.045591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hamilton MT, Hamilton DG, Zderic TW. Exercise physiology versus inactivity physiology: an essential concept for understanding lipoprotein lipase regulation. Exerc Sport Sci Rev. 2004 Oct;32(4):161–166. doi: 10.1097/00003677-200410000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Healy GN, Dunstan DW, Salmon J, et al. Objectively measured light-intensity physical activity is independently associated with 2-h plasma glucose. Diabetes Care. 2007 Jun;30(6):1384–1389. doi: 10.2337/dc07-0114. [DOI] [PubMed] [Google Scholar]
- 44.Healy GN, Wijndaele K, Dunstan DW, et al. Objectively measured sedentary time, physical activity, and metabolic risk: the Australian Diabetes, Obesity and Lifestyle Study (AusDiab) Diabetes Care. 2008 Feb;31(2):369–371. doi: 10.2337/dc07-1795. [DOI] [PubMed] [Google Scholar]