Abstract
Background
The primary aim of this study was to compare the effects of pentoxifylline (PTX) versus placebo on the histological features of NASH.
Methods
55 adults with biopsy-confirmed NASH were randomized to receive PTX at a dose of 400mg three times a day (n=26) or placebo (n=29) over 1 year. The primary efficacy endpoint was defined as improvement on histological features of NASH through reduction in steatosis, lobular inflammation, and/or hepatocellular ballooning as reflected by a decrease of ≥ 2 points in the NAFLD activity score (NAS).
Results
After 1 year, intention-to-treat analysis showed a decrease of >=2 points in the NAS in 38.5% of patients on PTX vs 13.8% of those on placebo (p=0.036). Per protocol analysis, a decrease of ≥ 2 points in the NAS from baseline was observed in 50% of the patients on PTX versus 15.4% of those on placebo (p=0.01). The mean change in NAS score from baseline was −1.6 in the PTX group, vs −0.1 in the placebo group (p<0.001). PTX significantly improved steatosis (mean change in score −0.9 vs −0.04 with placebo, p<0.001) and lobular inflammation (median change −1 vs 0 with placebo, p=0.02). No significant effects in hepatocellular ballooning were observed. PTX also improved liver fibrosis (mean change in fibrosis score was −0.2 among those on PTX versus +0.4 among those on placebo, p=0.038). Although not statistically significant (p=0.17), improvement in fibrosis was observed in a greater proportion (35%) of patients in the PTX group compared to placebo (15%). Adverse effects were similar in both groups.
Conclusion
PTX improved histological features of NASH compared to placebo. PTX was well tolerated in patients with NASH (ClinicalTrials.gov number NCT00590161).
Keywords: nonalcoholic fatty liver disease, pentoxifylline, clinical trials, liver fibrosis
Approximately 60 million adults in the United States have nonalcoholic fatty liver disease (NAFLD)1. The histologic spectrum of NAFLD spans from simple steatosis to nonalcoholic steatohepatitis (NASH), characterized by hepatocellular injury, inflammation, and fibrosis that can eventually progress to cirrhosis2,3.. Until recently, no therapy had been definitely proven beneficial for patients with NASH. A recent study showed some benefits of therapy with vitamin E in a proportion of patients with NASH4, however, there is still a need for additional and more effective therapies for patients with NASH.
Multiple factors and pathways are involved in the pathogenesis and progression of NAFLD and NASH. Imbalances in inflammatory cytokines, oxidative stress, and insulin resistance are some of the proposed mechanisms involved in NASH pathogenesis and progression5–8. Cytokines including tumor necrosis factor alpha (TNF-alpha)9,10, a pro-inflammatory cytokine, and adiponectin, an anti-inflammatory cytokine9, are believed to play an important role in hepatocellular damage, inflammation and fibrogenesis in NASH11. In mice, fatty liver disease is improved by inhibition of hepatic TNF-alpha production12 and by infusion of anti-TNF-alpha neutralizing antibody13,14.
Pentoxifylline (PTX) is a methylxanthine derivative known to increase red blood cell flexibility, reduce blood viscosity, and decrease platelet aggregation15,16. There is evidence supportive of a potential role for PTX in NASH. PTX inhibits a number of pro-inflammatory cytokines including TNF alpha17–19. In addition, PTX may have hepatoprotective effects17,20. It increases hepatic glutathione levels in mice with steatohepatitis induced by a methionine choline deficient diet17 and reduces the production of oxygen radicals induced by prolonged ischemia time in rat livers21. Potential antifibrogenic effects of PTX have been suggested by in vitro studies on hepatic stellate cells22,23, and in a rat model of biliary duct occlusion24. Therefore, PTX has a number of mechanisms that may provide therapeutic benefit to NASH patients.
Pilot studies of PTX in patients with NASH have been conducted and their results have suggested possible benefits of PTX in NASH25,26. However, to date, published studies have had significant limitations, predominantly uncontrolled design, small sample sizes, and lack of histological follow up evaluation.
The primary aim of this study was to compare the effectiveness of PTX over one year with placebo in patients with NASH. The primary outcome measure was defined as an improvement of 2 or more points in the NAFLD activity score (NAS)27. Other aims were to compare the effects of PTX compared to placebo on serum transaminases; to assess the effect of PTX on insulin sensitivity; to assess the effect of PTX on hepatocyte apoptosis; and to assess the effect of therapy with PTX on serum levels of TNF alpha and adiponectin. We also aimed to compare the rate of adverse events in patients with NASH receiving PTX compared with placebo.
Patients and Methods
Selection of Patients
Patients were recruited at two medical centers in Cleveland, OH, the Louis Stokes Cleveland Veterans Affairs Medical Center, and the Cleveland Clinic. Patients were considered for the study if they had a well established diagnosis of NASH based on liver biopsy performed within six months of entry into the study.
Other inclusion criteria were (1) daily alcohol intake of <30 g for males and <15 g for females; (2) appropriate exclusion of other liver diseases; (3) age between 18 and 70 years and (4) the ability to give informed consent. Patients with diabetes mellitus type 2 (DM) were included only if their therapeutic regimen was limited to oral agents including sulfonylureas (e.g. glipizide and glyburide) and/or biguanides (e.g. metformin), was stable (defined by no changes in oral agents or their dose for at least 6 months), and with relatively adequate glucose control as defined by HgbA1C < 8%.
Patients were excluded if they had a history of past excessive alcohol drinking (as defined above) for a period longer than 2 years at any time in the past 10 years; positive testing for hepatitis B virus or hepatitis C virus; any other suspected cause of liver disease by history, blood tests or clinical findings; patients were also excluded if they were taking medications known to cause steatosis; or taking medications that have shown benefits in previous NASH pilot studies, including vitamin E, Betaine, S-adenosylmethionine (SAM-e), thiazolidinediones, and alpha-glucosidase inhibitors. Patients with cirrhosis defined by stage 4 fibrosis on liver biopsy or by unequivocal clinical evidence consistent with underlying cirrhosis were also excluded. Patients with a history of hypersensitivity to PTX or the methylxanthines (caffeine, theophylline, theobromine) were excluded, as well as those with a history of cerebral or retinal hemorrhage. Patients taking theophylline or coumadin were excluded because of potential interactions with PTX.
Study Design and Organization
The study was designed as a double-blinded, randomized, placebo-controlled trial. The study was approved by the institutional review boards at all involved institutions. The study conduction, progress and data were overseen by an independent Data and Safety Monitoring Board, and an independent Regulatory Compliance and Data Integrity Monitor. Enrollment occurred between December 2006 and February 2009. A computer-generated randomization table was kept by the research pharmacy at each site and only pharmacy study personnel had access to it. Double-blinding was maintained throughout the duration of the randomization phase. The trial was completed in April of 2010.
Patients were assigned to one of two study groups. Patients on the treatment arm received an oral dose of 400 mg three times per day of PTX for one year. In the placebo arm, identical placebo was substituted for PTX. Both formulations were white, oblong capsules with no markings, no discernible odor, and no difference to taste.
Evaluation and Monitoring of Patients
Clinical history and physical examination were completed at entry and at 1 year. Follow up liver biopsy was obtained after 12 months of taking the study medication and prior to discontinuation. Laboratory studies done at entry and at 12 months included liver enzymes, basic metabolic panel, complete blood count, prothrombin time, hemoglobin A1C, fasting insulin, C-peptide, lipid panel, TNF-alpha, and adiponectin. Liver enzymes were also tested at 3, 6, and 9 months.
Weight and height for body mass index (BMI) calculation, and waist measurement were obtained at entry and at study completion. Individualized nutritional counseling for adequate caloric intake and recommended lifestyle modifications were provided to all study subjects.
Compliance and adverse effects were formally evaluated at one month, three months, six months, nine months, and twelve months into the study. Compliance was assessed by direct questioning of the subjects. In addition, patients were asked to return remaining pills at the time of each refill, and pill count was performed.
Assessment of Liver Histology
Liver pathologists at each center (PG at the Cleveland VAMC site, and LY at the Cleveland Clinic site) established the presence of histological diagnosis of NASH required for entry.
Adequacy of the liver biopsy specimens for evaluation was performed by the study pathologists and the aggregate biopsy length of the specimens was recorded. Subsequently, all entry and end of study liver biopsies (from both centers) were formally reviewed and scored by a dedicated liver pathologist blinded to treatment arm and who is experienced with the NAS (LY). Per study design, final analysis was based on the results of this formal review. The NAS27 grades NAFLD based on the individual scores for steatosis, inflammation and ballooning. Fibrosis at entry and at the end of trial was staged 0 to 4 (0 –absent; 1 –perisinusoidal or portal/periportal only; 2 –perisinusoidal and periportal; 3 –bridging fibrosis; 4 –cirrhosis).
Assessment of insulin sensitivity
Assessment of insulin sensitivity was done at entry and at study completion by the frequently sampled intravenous glucose tolerance test (FSIVGTT) 28–30. The 5 study subjects with DM were asked not to take their oral hypoglycemic medications for the 36 hours prior to initiation of the test. The FSIVGTT test was completed by expert nursing personnel at the Clinical Research Units located at University Hospitals Case Medical Center (for patients enrolled at the Cleveland VA) and at the Cleveland Clinic (for patients enrolled at the Cleveland Clinic). Samples were processed by laboratory personnel at the Clinical Research Units. Testing was performed by a skilled team at the Human Specimen Laboratory Core of the Case Western Reserve University Clinical & Translational Science Collaborative located in University Hospitals Case Medical Center. YSI 2300 STAT Plus Glucose analyzer (Yellow Springs, OH) was used to measure glucose. Insulin was measured using the Human Insulin Specific assay, Millipore (Catalog #HI-14K, Billerica, MA). Insulin sensitivity and insulin secretory capacity were assessed using the MINMOD analysis program30,31 by a collaborator with expertise (JK). In addition, fasting glucose and insulin were used to calculate insulin resistance according to the homeostasis model assessment technique (HOMA-IR) at entry and at study completion.
Assessment of serum cytokines
Serum cytokines were measured by expert personnel at the Human Specimen Laboratory Core. TNF-alpha in serum at entry and at study completion was measured with the Human TNF-α/TNFSF1A HS assay (R&D Systems, Catalog #HSTA00C, Minneapolis, MN). Adiponectin was measured using the Human Adiponectin assay (Millipore, Catalog #EZHADP-61K, Billerica, MA).
Assessment of hepatocyte apoptosis
Hepatocyte apoptosis in liver sections obtained at baseline and at one year were quantitated using the TUNEL assay32 by a collaborator with expertise (AEF). Quantitation was done by counting the number of TUNEL-positive cells in 30 random microscopic fields (x400) as previously described33. The ApopTag InSitu apoptosis detection kit (Millipore, product #S7111) and ApopTag TdT enzyme (Millipore, product #S7107) were used.
Sample Size Calculation and Statistical Analyses
The primary outcome measure was defined as an improvement of ≥2 points in the NAS. A sample size of 52 subjects (26 per study arm) was estimated to provide 80% power to detect a significant difference (delta=40%) between groups in achieving the primary endpoint at an alpha level of 0.05. To allow for a potential dropout rate of 20%, a sample total sample size of 64 patients was projected. However, study enrollment was stopped at 55 patients. This decision was partly due to slower than projected accrual and prolonged study duration, but also to a significantly lower than expected dropout rate. By the time 55 patients had been enrolled, over 60% of the goal sample size had completed the study timeline and the dropout rate had been 10%. Eventually the dropout rate was 11% overall.
The primary endpoint of the study regarding efficacy was improvement by ≥ 2 points in the NAFLD activity score (NAS). Intention-to-treat (ITT) analyses and per-protocol analyses of the primary endpoint were performed. For subjects who did not undergo end-of-study liver biopsy the primary endpoint was imputed as treatment failure for the ITT analysis. Analysis of all other efficacy and safety endpoints was performed with subjects for whom data was available. Continuous data were analyzed by the student t test if normally distributed and by non-parametric tests otherwise. Distribution of all continuous and ordinal variables was assessed using the Kolmogorov-Smirnov test as well as normal probability plots. Categorical data were analyzed by the χ2 test or Fisher exact test. The proportion of subjects in each treatment arm for whom there was improvement in histologic features as assessed by the NAFLD Activity Score (NAS) was compared using Pearson’s chi-square tests. The direct estimates of treatment effects were also obtained by calculating the contrast in mean change in NAS and fibrosis stage between treatment groups along with 95% confidence intervals. In addition, because the standardized difference of the baseline values for AST and ALT exceeded 15%, an adjusted analysis was performed. Logistic regression models and ANCOVA were used for efficacy endpoints. For each model, treatment group and baseline value of the endpoint were included as independent variables. Multivariable modeling was used to adjust for relevant variables when indicated. Given the number of patients who had improvement in the NAS, we were limited to assessing treatment with PTX plus one additional variable at a time. Multivariable analysis was done to adjust for those variables that were of clinical relevance and found to be associated with NAS improvement by univariate analysis. All statistical tests were two-sided. A p-value < 0.05 was considered statistically significant and all analyses were carried out using SAS version 9.2 (The SAS Institute, Cary, NC).
Results
Study Patients
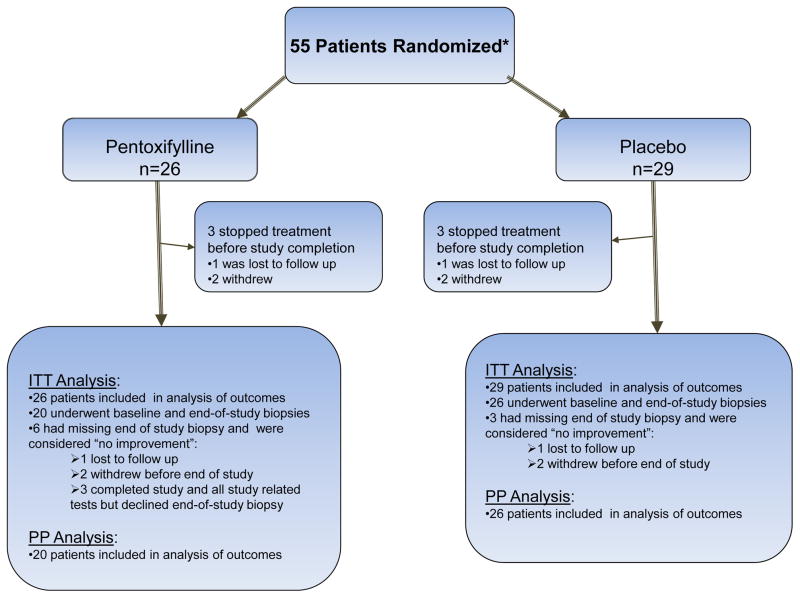
Fifty-five patients were enrolled in the study. Twenty-six patients were assigned to the PTX group and 29 to the placebo group (Fig. 1). In the PTX group, 23 patients completed the trial, and in the placebo group 26 patients completed the trial. Among the 3 PTX patients who stopped treatment before study completion, one stopped after 4 weeks because he did not wish to continue in the study after his liver tests normalized; the second one stopped after six months because of personal reasons; and the third was lost to follow up. Among the 3 placebo patients who stopped treatment before study completion, one stopped after one day because changed her mind; the second one stopped after three months because could not commit to the study; and the third one was lost to follow up.
Figure 1.
Patient flow diagram illustrating the two study groups.
Both groups were comparable at entry regarding demographics, anthropomorphic measurements, prevalence of relevant co-morbidities, and histological features on liver biopsy (Table 1). Both groups were also comparable at entry regarding most laboratory tests. However, higher aspartate aminotransferease (AST) and alanine aminotransferase (ALT) at baseline were observed in the PTX group compared to the placebo group. Because of this, appropriate adjustments were made at the time of statistical analysis.
Table 1.
Baseline Characteristics of Subjects
| Factor | N | Pentoxifylline (N=26) | Placebo (N=29) | Total (N=55) |
|---|---|---|---|---|
| Demographic and metabolic | . | |||
| Age (yrs) | 55 | 50.5 ± 12.7 | 49.6 ± 9.6 | 50.0 ± 11.1 |
| Male | 55 | 18 (69.2) | 20 (69.0) | 38 (69.1) |
| White | 55 | 25 (96.2) | 26 (89.7) | 51 (92.7) |
| BMI (kg/m2) | 55 | 32.9 ± 4.6 | 34.0 ± 5.4 | 33.5 ± 5.0 |
| Waist circumference (cm) | 44 | 112.4 ± 20.1 | 111.8 ± 12.7 | 112.1 ± 16.6 |
| Diabetes Type 2 | 55 | 1 (3.8) | 4 (13.8) | 5 (9.1) |
| Hypertension | 48 | 15 (65.2) | 13 (52.0) | 28 (58.3) |
| Hyperlipidemia | 48 | 15 (65.2) | 10 (40.0) | 25 (52.1) |
| Laboratory tests | . | |||
| AST (U/L) | 55 | 58.0 [37.0, 72.0] | 43.0 [34.0, 56.0] | 48.0 [35.0, 63.0] |
| ALT (U/L) | 55 | 81.5 [58.0, 108.0] | 55.0 [44.0, 80.0] | 67.0 [50.0, 93.0] |
| Alkaline Phosphate (U/L) | 55 | 72.5 [56.0, 96.0] | 63.0 [51.0, 83.0] | 67.0 [53.0, 91.0] |
| Total bilirubin (mg/dL) | 55 | 0.7 ± 0.3 | 0.8 ± 0.4 | 0.7 ± 0.4 |
| Fasting glucose (mg/dL) | 55 | 91.0 [83.0, 97.0] | 95.0 [85.0, 107.0] | 92.0 [83.0, 102.0] |
| HOMA-IR | 55 | 5.3 ± 2.5 | 6.1 ± 3.0 | 5.7 ± 2.8 |
| HgbA1C (%) | 48 | 5.8 ± 0.7 | 5.8 ± 0.5 | 5.8 ± 0.6 |
| C-Peptide(ng/mL) | 55 | 2.8 [1.9, 3.7] | 3.4 [2.1, 3.7] | 2.9 [1.9, 3.7] |
| Total cholesterol (mg/dL) | 55 | 193.5 ± 44.7 | 184.3 ± 27.3 | 188.6 ± 36.5 |
| HDL (mg/dL) | 54 | 40.5 ± 10.0 | 41.1 ± 10.4 | 40.8 ± 10.1 |
| Triglycerides (mg/dL) | 54 | 158.5 [123.0, 194.0] | 110.5 [96.5, 163.5] | 139.5 [102.0, 191.0] |
| TNFa (pg/mL) | 55 | 7.6 ± 1.7 | 7.4 ± 2.0 | 7.5 ± 1.9 |
| Adiponectin (ug/mL) | 55 | 5.9 ± 2.4 | 5.4 ± 2.3 | 5.7 ± 2.4 |
| Liver biopsy features | . | |||
| Aggregate Biopsy length (mm) | 20.0 ± 9.1 | 23.5 ± 10.2 | 21.8 ± 9.8 | |
| NAFLD Activity Score | 55 | 5.7 ± 1.3 | 5.4 ± 1.5 | 5.6 ± 1.4 |
| Steatosis | 55 | |||
| 1–33% | 3 (11.5) | 6 (20.7) | 9 (16.4) | |
| 34–66% | 11 (42.3) | 13 (44.8) | 24 (43.6) | |
| >66% | 12 (46.2) | 10 (34.5) | 22 (40.0) | |
| Lobular Inflammation | 55 | |||
| No/minimal | 0 (0.0) | 1 (3.4) | 1 (1.8) | |
| Mild | 4 (15.4) | 9 (31.0) | 13 (23.6) | |
| Moderate | 18 (69.2) | 16 (55.2) | 34 (61.8) | |
| Severe | 4 (15.4) | 3 (10.3) | 7 (12.7) | |
| Ballooning | 55 | |||
| None | 0 (0.0) | 1 (3.4) | 1 (1.8) | |
| Few | 16 (61.5) | 11 (37.9) | 27 (49.1) | |
| Many | 10 (38.5) | 17 (58.6) | 27 (49.1) | |
| Fibrosis Stage | 55 | |||
| 0 | 0 (0.0) | 5 (17.2) | 5 (9.1) | |
| 1 | 11 (42.3) | 7 (24.1) | 18 (32.7) | |
| 2 | 10 (38.5) | 8 (27.6) | 18 (32.7) | |
| 3 | 5 (19.2) | 9 (31.0) | 14 (25.5) | |
| TUNEL(+)cells/hpf | 2.7 [1.3, 3.3] | 1.9 [1.0, 2.7] | 2.3 [1.0, 3.3] |
N is total subjects with non-missing data
Data presented as Mean +/−SD, Median [25th, 75th percentiles] or N (%).
Insulin resistance was calculated using the homestatis model assessment for insulin resistance (HOMA-IR) according to the following formula: [glucose (mg/dL) × insulin (uU/mL)]/405.
NAFLD Activity Score (NAS) was assessed on a scale of0 to 8 with higher scores indicating more severe disease. NAS is obtained by adding steatosis (assessed on a scale of 0 to 3), inflammation (assessed on a scale of 0 to 3) and ballooning (assessed on a scale of 0 to 2). Fibrosis stage is assessed on a scale of 0 to 4 with higher values indicating more severe disease.
Primary Outcome
Nine subjects (6 who stopped treatment before study completion and 3 who completed the study but declined the end of study liver biopsy) did not have end of study liver histology available. For the intention-to-treat (ITT) analysis, the primary outcome for those nine subjects was imputed as lack of improvement. As shown in Table 2, per ITT analysis, a decrease of >=2 points in the NAS from baseline was observed in 38.5% of patients on PTX versus 13.8% of those on placebo (p=0.036). Per protocol (PP) analysis (assessed in subjects with both biopsies available), a decrease of ≥ 2 points in the NAS from baseline was observed in 50% of the patients on PTX versus 15.4% of those on placebo (p=0.01).
Table 2.
Primary Outcome and Improvement in Histologic Features
| Factor | Pentoxifylline | Placebo | p-value* |
|---|---|---|---|
| Primary Outcome | |||
| No. of subjects randomly assigned | 26 | 29 | |
| NAS decreased by 2+ points (ITT) | 10 (38.5) | 4 (13.8) | 0.036 |
| Other Histologic Features | |||
| No. of subjects with both biopsies | 20 | 26 | . |
| NAS | |||
| Mean Change from baseline | −1.6 ± 1.1 | −0.1 ± 1.4 | <0.001 |
| NAS decreased by 2+ points (Per-protocol) | 10 (50.0) | 4 (15.4) | 0.011 |
| Steatosis | |||
| Mean Change from baseline | −0.85 ± 0.6 | −0.04 ± 0.7 | |
| Median Change from baseline | −1.0 [−1.0, −0.5] | 0.0 [0.0, 0.0] | <0.001 |
| Patients with improvement | 15 (75.0) | 5 (19.2) | <0.001 |
| Lobular Inflammation | |||
| Mean Change from baseline | −0.45 ± 0.7 | 0.08 ± 0.8 | |
| Median Change from baseline | −1.0 [−1.0, 0.0] | 0.0 [0.0, 1.0] | 0.023 |
| Patients with improvement | 11 (55.0) | 6 (23.1) | 0.026 |
| Ballooning | |||
| Mean Change from baseline | −0.25 ± 0.7 | −0.15 ± 0.5 | |
| Median Change from baseline | 0.0 [−1.0, 0.0] | 0.0 [0.0, 0.0] | 0.70 |
| Patients with improvement | 6 (30.0) | 6 (23.1) | 0.60 |
| Fibrosis | |||
| Mean Change from baseline | −0.2 ± 0.7 | 0.4 ± 0.9 | 0.038 |
| Patients with improvement | 7 (35.0) | 4 (15.4) | 0.17 |
Data presented as Mean +/−SD, Median [25th, 75th percentiles] or N (%).
Primary outcome was improvement in NAFLD Activity Score (NAS) by at least 2 points. Nine subjects (6 in Pentoxifylline group, 3 in placebo group) did not have end of study biopsy done; primary outcome for these was imputed as lack of improvement in NAS. Other histologic features are assessed in the 46 subjects with both biopsies available. NAS was assessed on a scale of 0 to 8 with higher scores indicating more severe disease.
Improvement in fibrosis, steatosis, inflammation or ballooning is defined as a decrease of at least 1 point.
p-values for % improvement were calculated using Fisher’s Exact Test for fibrosis and Pearson’s chi-square tests otherwise.
As shown in Figure 2, all patients in the PTX group had improvement (n=17) or no change (n=3) on the NAS score by the end of the study, whereas the changes on the NAS of those patients on placebo were widely variable. The mean change in NAS score from baseline was −1.6 (±1.1) in the PTX group, compared to a mean change of −0.1(±1.4) in the placebo group (p<0.001). The direct estimate of PTX treatment effect on the NAS score was −1.4 (95% CI −2.2, −0.67).
Figure 2.
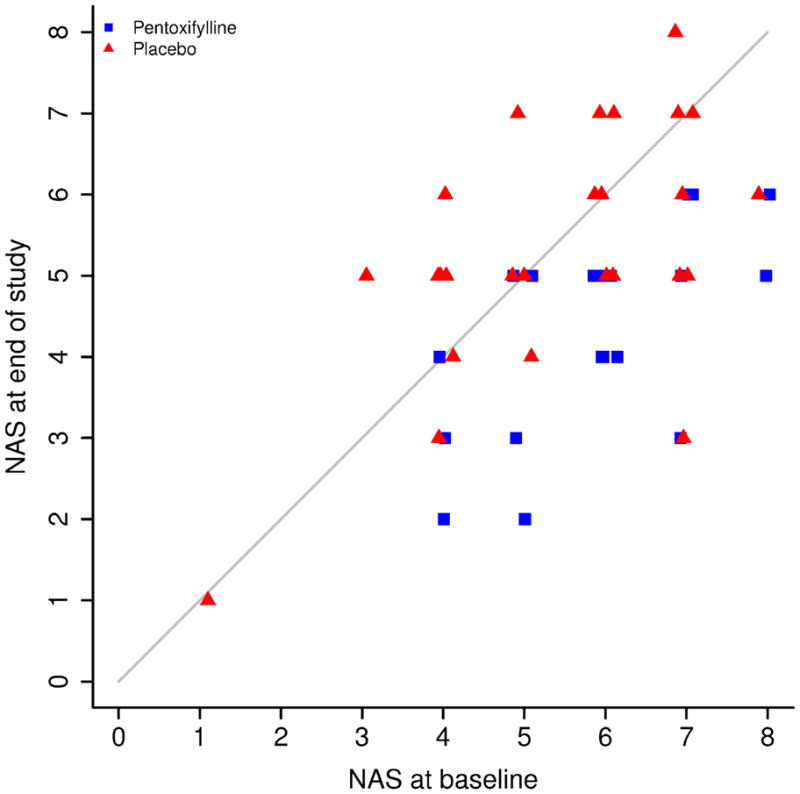
Change in NAFLD Activity Score from Baseline to End of Study. The diagonal line represents no change between start and end of study; values above the line represent increases in NAS (worsening of histological disease) while those below the line represent improvement in NAS. The data was jittered along the x-axis to break ties. The graphic shows that 17 subjects in the PTX group had histological improvement (decrease in NAS score) while the remaining three had no change in NAS score. In contrast, in the placebo group, changes in NAS score are strewn all over the graph showing 9 subjects had histological worsening of disease, 8 had no change, and 9 had histological improvement.
Secondary Outcomes
Histologic Features
As shown in Table 2, PTX significantly improved steatosis (mean change in score −0.9 vs −0.04 with placebo, p<0.001) and lobular inflammation (median change in score −1 vs 0 with placebo, p=0.02). However, no significant effects in hepatocellular ballooning were observed.
PTX was also associated with improvement of fibrosis score. The difference in mean change in fibrosis score was −0.2 among those on PTX compared to +0.4 among those on placebo (p=0.038). The direct estimate of treatment effect on the fibrosis score was −0.5 (95% CI −1.0, −0.04).
Analyses were performed to investigate and adjust for associations between potentially relevant variables and NAS improvement. No association by univariate analysis was demonstrated between NAS improvement and several variables including gender; age; presence or absence of DM, hypertension or hyperlipidemia; or changes in HOMA, TNF alpha, insulin, acute insulin response to glucose, disposition index, insulin sensitivity index, or glucose effectiveness, among others. Treatment group (PTX), change in BMI, and change in Hgb A1C were associated with NAS improvement by univariate analysis. At the end of the study, a change from baseline in BMI of −0.28 kg/m2 (±1.0) was observed in the PTX group compared to 0.52 kg/m2 (±1.8) in the placebo group (p=0.052). The final multivariable model (whole model test p<0.0001) showed that only treatment group (PTX) and change with BMI remained significantly associated with NAS improvement. The effect of PTX on NAS improvement was independent of change in BMI. The odds ratio for NAS improvement [with 95% CI] for PTX treatment was 7.1 [1.5, 34.3], p=0.015; and for BMI it was 0.49 [0.24, 0.99], p=0.049.
There was no significant association between change in BMI and improvement in fibrosis. The only variable significantly associated with improvement in fibrosis was treatment with PTX. Of the 46 NASH study patients who had follow up biopsies, at the end of the study 40 (87%) still had NASH and 6 (13%) did not have NASH. Among patients on the PTX arm, 5 of 20 (25%) with NASH at entry had no NASH at the end of the study. Among patients on the placebo arm, 1 of 26 (3.9%) with NASH at entry had no NASH at the end of the study (p=0.03).
Change in Aminotransferases
Normalization or improvement of 30% or more in ALT levels from baseline was observed in 57% of the subjects taking PTX compared to 23% of those taking placebo (p=0.016). Regarding AST, the difference between treatment groups regarding normalization or improvement of 30% or more from baseline did not reach statistical significance. The decision to incorporate patients who had normalization of values in the group with 30% improvement was made in order to include patients with normalization of transaminases even if it required less than 30% decrease in baseline levels. Regarding ALT, there was no difference between the number of patients that had 30% improvement and those with normalization (all 19 patients had at least 30% improvement). Continuous AST and ALT values were the only relevant laboratory test showing imbalances at baseline between treatment arms and after adjusting for these imbalances the mean changes between groups were not significantly different.
Changes in Insulin Resistance, serum TNF-alpha and Adiponectin, and Hepatocyte Apoptosis
As shown in Table 3, there was no evidence to suggest a significant association between treatment with PTX and mean changes in several measurements of insulin resistance; serum levels of TNF-alpha and adiponectin; or hepatocyte apoptosis.
Table 3.
Changes from Baseline in Secondary Outcomes*
| Factor | Pentoxifylline (N=23) | Placebo (N=26) | p-value* |
|---|---|---|---|
| Measurements of Insulin Resistance/Sensitivity | |||
| Acute Insulin Response to Glucose (AIRg) | −75.8 ± 77.6 | 58.1 ± 70.8 | 0.21 |
| Disposition Index (DI) | −75.1 ± 142.4 | 86.2 ± 130.0 | 0.41 |
| Insulin Sensitivity Index (SI) | 0.09 ± 0.24 | −0.05 ± 0.22 | 0.67 |
| Glucose effectiveness(Sg) | 0.0018 ± 0.001 | 0.0001 ± 0.001 | 0.36 |
| Change in HOMA-IR | 0.8 [−0.2, 3.7] | 1.1 [−2.5, 1.7] | 0.39 |
| Measurement of Hepatocyte Apoptosis | |||
| Change in TUNEL(+) cells/hpf | −0.3 [−1.7, 0.5] | −0.2 [−1.0, 0.5] | 0.54 |
| Serum cytokines measurements | |||
| Change in TNFa | −0.1 ± 0.9 | 0.2 ± 1.5 | 0.38 |
| Change in adiponectin | 0.1 [−1.1, 0.8] | −0.0 [−1.0, 0.2] | 0.60 |
Data presented as Mean +/−SD, Median [25th, 75th percentiles] or N (%).
Changes in AIRg, DI, SI, and Sg were available for 45 subjects; HOMA and C-peptide for 47; Change in TUNEL was available for 36;and TNFa and adiponectin for 46. AIRg, DI, SI and Sg were adjusted for baseline values. P-values were calculated using t-tests or Wilcoxon rank sum tests were indicated.
Safety and Adverse Events
The occurrence of adverse experiences was monitored and recorded throughout the study. Table 4 presents the subjects in each treatment arm that experienced side effects during the treatment period. There was no statistically significant difference in the occurrence of side effects overall between groups. However, nausea and vomiting were reported more frequently by patients on PTX compared to those on placebo. Three (12.5%) subjects on the PTX treatment arm had to decrease the medication dose from TID to BID because of nausea. With dose change the symptom was adequately controlled. No study drug related severe adverse events occurred. No patients discontinued therapy as a result of adverse events.
Table 4.
Side Effects
| Pentoxifylline (N=25) | Placebo (N=28) | p-value* | |
|---|---|---|---|
| Any side effects | 11 (44.0) | 14 (50.0) | 0.78 |
| Nausea | 6 (24.0) | 4 (14.3) | 0.37 |
| Vomiting | 2 (8.0) | 0 (0.0) | 0.13 |
| Dose change due to nausea/vomiting | 3 (12.5) | 0 (0.0) | 0.063 |
| Bloating | 2 (8.0) | 3 (10.7) | 0.74 |
| Abdominal pain | 0 (0.0) | 2(7.1) | 0.17 |
| Headache | 2 (8.0) | 1 (3.6) | 0.49 |
| Lightheadedness | 1 (4.0) | 3 (10.7) | 0.36 |
| Diarrhea | 1 (4.0) | 3 (10.7) | 0.36 |
| Chest pain | 0 (0.0) | 2 (7.1) | 0.17 |
| Chest palpitations | 0 (0.0) | 1 (3.6) | 0.34 |
| Fatigue | 0 (0.0) | 2 (7.1) | 0.17 |
| Vasovagal pre/post biopsy | 1 (4.0) | 1 (3.6) | 0.93 |
Data presented as n (%).
One subject in each treatment arm was lost to follow up and had no information on safety endpoints
p-values were calculated using Pearson’s chi-square test for presence of any side effect and Fisher’s Exact tests otherwise
Discussion
The results of this randomized placebo controlled trial show that PTX improved histological features of NASH, and liver fibrosis, in patients with NASH. The rising prevalence of NAFLD, and therefore NASH, together with the recognition of patient subsets at higher risk of increased severity and progression of disease, highlight the need for an effective treatment. Although a recent important study showed benefits of vitamin E in a significant portion of patients with NASH4, the majority of NASH patients treated with vitamin E in that trial did not respond to the treatment. Also, the possibility that high doses of vitamin E may increase cardiovascular risk and mortality is an additional concern that should be kept in mind34. Therefore, the need for additional effective therapies for NASH remains.
In this study, therapy with PTX for one year resulted in significant improvement of histological features of NASH compared to placebo. Among patients with both biopsies available, achievement of the primary outcome was observed in 50% of the patients on PTX versus 15.4% of those on placebo (p=0.01). These results substantiate the benefits of PTX in NASH suggested by previous pilot studies25,26. The histological improvements associated with PTX treatment in this study were clearly independent of changes on insulin resistance or sensitivity measures. In addition, other potential underlying mechanisms were explored. Although PTX is known to inhibit TNF-alpha, we were unable to demonstrate changes in TNF-alpha associated with PTX treatment or with histological improvement in patients on PTX. However, we need to acknowledge that the lack of changes in circulating levels of this cytokine may not correlate with hepatic levels35. Similarly, changes on hepatocyte apoptosis measured by TUNEL were not associated with PTX treatment in this study. However, TUNEL is not a robust test to track changes in apoptosis longitudinally, and it also lacks in specificity and sensitivity36. Future studies to investigate further the potential underlying mechanistic aspects of these observations, including better characterization of the potential effects of PTX on hepatic TNF-alpha and on apoptotic pathways in NASH, will be needed. Other potential mechanisms by which PTX may exert its protective effect and that should be investigated in future studies include modulation of the inflammatory response16,37, as well as antioxidant effects21,38.
Interesting observations of this study relate to the results suggesting that PTX may improve liver fibrosis among patients with NASH. This is of particular importance because liver fibrosis is the main histological feature that correlates with adverse clinical outcomes in NASH. Although mechanistic explanations of the observations regarding liver fibrosis are beyond the scope of this manuscript, there is some data that may support this potential effect of PTX. In vitro studies have showed an antifibrogenic effect of PTX on dermal fibroblasts39,40 and on activated hepatic stellate cells22,23, and this effect appears to be partly mediated by extracellular collagen degradation22. In rats with biliary duct occlusion, PTX reduces liver collagen and key fibrogenic cytokines24. Interestingly, like caffeine, PTX is also a methylxanthine, and there is recent evidence that increased caffeine intake may be associated with decreased liver fibrosis41. Future studies may help characterize this further.
There was no statistically significant difference in the rate of adverse events between treatment groups. However, nausea and vomiting was observed at a more clinically significant frequency among patients taking PTX compared to placebo. Nausea and vomiting are well recognized potential side effects of PTX. These effects are known to be dose-related and dosage-form related, with nausea and vomiting reported more frequently with higher doses and in patients taking immediate-released preparations compared to controlled-release preparations42. We used a controlled-release preparation for this study. This, together with the lower dose used (1200 mg per day), may explain the lower rate of nausea and vomiting in our patient cohort compared to previous pilot studies that used a higher dose25. Although nausea was reported by 6 (24%) of patients on PTX, only 3 (12.5%) patients had to change the dose from TID to BID in order to control the symptom. No patient on the PTX arm had to stop taking PTX due to drug related adverse effects. Although this study was not powered to assess safety, the overall safety profile of PTX has been well established for decades, plus our data now indicates that in patients with NASH it appears to be safe and relatively well tolerated. Furthermore, its affordability as a generic drug is an attractive factor for both patients and governments particularly given the increasing prevalence of NAFLD -and therefore NASH- in the general population, and the knowledge that medical therapy of NASH will likely have to be long term.
Despite the very encouraging results observed regarding the effectiveness of PTX on the liver histology of patients with NASH, we acknowledge the limitations of the study. The limitations regarding the measurement of circulating TNF-alpha and the use of TUNEL to quantitate apoptosis were acknowledged above. Similarly acknowledged above was the fact that our sample size provided adequate power to assess the main outcomes of interest, but was not designed to formally assess safety measures. An additional limitation of the study is that the number of patients with DM included was very small. This was partly due to strict inclusion criteria that allowed only type 2 DM not on insulin and on stable regimens and well controlled blood glucose to be included, and also to the fact that a separate trial targeting NASH patients with DM was being conducted simultaneously at one of the recruiting institutions. Because of the resulting small number of DM patients included, no conclusions can be made specifically regarding the response to PTX treatment among NASH patients with co-existing DM. NASH patients with cirrhosis were also excluded from the study, therefore the conclusions cannot be extrapolated to that patient population. Future studies can study the effects of PTX specifically in the subsets of NASH patients with DM or with cirrhosis. Finally, as with any clinical trial in NASH patients where liver biopsy histology is the main outcome measure, the subjectivity of the interpretation of the liver histology is a limitation. The use of a single pathologist (LY) who has special training and significant experience with the CRN NAS system27 and who was blinded to treatment allocation lessened this limitation.
In conclusion, this trial demonstrated that PTX improves NASH and may impact the progression of liver fibrosis in NASH. PTX was overall well tolerated in patients with NASH. These observations, together with PTX’s long term safety data and its affordability as a generic, may support the use of PTX in patients with NASH, but larger studies will be needed, especially to corroborate the effects on liver fibrosis and to further characterize underlying mechanisms.
Acknowledgments
This work was supported by the American College of Gastroenterology Junior Faculty Career Development Award to Dr. Claudia Zein. Dr. Claudia Zein is also supported by Grant Number KL2 RR024990 from the National Center for Research Resources (NCRR), a component of the NIH and NIH Roadmap for Medical Research. This project was supported by Grant Number M01 RR00080 and Grant Number UL1 RR024989 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH). The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH.
The authors would like to thank the nurses, laboratory personnel, nutrition staff and other personnel at the Clinical Research Units at the University Hospitals Case Medical Center and the Cleveland Clinic for their valuable role as part of this project.
Abbreviations
- NAFLD
Nonalcoholic Fatty Liver Disease
- NASH
Nonalcoholic Steatohepatitis
- PTX
pentoxifylline
- DM
type 2 diabetes mellitus
- BMI
body mass index
- SD
standard deviation
- OR
odds ratio
Footnotes
This work was presented, in part, at the Annual Meeting of the American College of Gastroenterology (ACG), October 2010, San Antonio, TX
References
- 1.Browning JD, Szczepaniak LS, Dobbis R, et al. Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology. 2004;40:1387–95. doi: 10.1002/hep.20466. [DOI] [PubMed] [Google Scholar]
- 2.Adams LA, Lymp JF, St Sauver J, et al. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterolgy. 2005;129:113–121. doi: 10.1053/j.gastro.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 3.Matteoni CA, Younossi ZM, Gramlich T, et al. Nonalcoholic fatty liver disease: An spectrum of clinical and pathological severity. Gastroenterology. 1999;116:1413–1419. doi: 10.1016/s0016-5085(99)70506-8. [DOI] [PubMed] [Google Scholar]
- 4.Sanyal AJ, Chalasani N, Kowdley KV, et al. Pioglitazone, vitamin E or placebo for nonalcoholic steatohepatitis. N Engl J Med. 362(18):1675–1685. doi: 10.1056/NEJMoa0907929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Day CP, James OF. Steatohepatitis: A Tale of Two “Hits”. Gastroenterology. 1998;114:842–845. doi: 10.1016/s0016-5085(98)70599-2. [DOI] [PubMed] [Google Scholar]
- 6.Bruix J, Llovet JJ. Is bacterial ash the flash that ignites NASH? Gut. 2001;48:148–153. doi: 10.1136/gut.48.2.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sanyal AJ, Campbell-Sargent C, Mirshahi F, et al. Nonalcoholic steatohepatitis: association of insulin resistance and mitochondrial abnormalities. Gastroenterology. 2001;120:1183–92. doi: 10.1053/gast.2001.23256. [DOI] [PubMed] [Google Scholar]
- 8.Weltman MD, Farrell GC, Hall P, et al. Hepatic cytochrome P450 2E1 is increased in patients with nonalcoholic steatohepatitis. Hepatology. 1998;27:128–33. doi: 10.1002/hep.510270121. [DOI] [PubMed] [Google Scholar]
- 9.Hui JM, Hodge A, Farrell GC, et al. Beyond insulin resistance in NASH: TNFα or adiponectin? Hepatology. 2004;40:46–54. doi: 10.1002/hep.20280. [DOI] [PubMed] [Google Scholar]
- 10.Katsuki A, Sumida Y, Murashima S, et al. Serum levels of tumor necrosis factor-alpha are increased in obese patients with noninsulin-dependent diabetes mellitus. J Clin Endocrinol Metab. 1998;83:859–862. doi: 10.1210/jcem.83.3.4618. [DOI] [PubMed] [Google Scholar]
- 11.Tilg H, Diehl AM. Cytokines in alcoholic and nonalcoholic steatohepatitis. N Engl J Med. 2000;343:1467–76. doi: 10.1056/NEJM200011163432007. [DOI] [PubMed] [Google Scholar]
- 12.Lin HZ, et al. Metformin reverses fatty liver disease in obese, leptin-deficient mice. Nat Med. 2000;6:998–1003. doi: 10.1038/79697. [DOI] [PubMed] [Google Scholar]
- 13.Li Z, Yang S, Lin H, et al. Probiotics and antibodies to TNF inhibit inflammatory activity and improve nonalcoholic fatty liver disease. Hepatology. 2003;37:343–50. doi: 10.1053/jhep.2003.50048. [DOI] [PubMed] [Google Scholar]
- 14.Koppe SW, Sahai A, Malladi P, et al. Pentoxifylline attenuates steatohepatitis induced by the methionine choline deficient diet. J Hepatol. 2004;41:592–8. doi: 10.1016/j.jhep.2004.06.030. [DOI] [PubMed] [Google Scholar]
- 15.Ward A, Clissold SP. Pentoxifylline. A review of its pharmacodynamic and pharmacokinetic properties, and its therapeutic efficacy. Drugs. 1987;34:50–97. doi: 10.2165/00003495-198734010-00003. [DOI] [PubMed] [Google Scholar]
- 16.Matzky R, Darius H, Schror K. The release of prostacyclin (PGI2) by pentoxifylline from human vascular tissue. Arzneimittelforschung. 1982;32:1315–1318. [PubMed] [Google Scholar]
- 17.Koppe SW, Sahai A, Malladi P, et al. Pentoxifylline attenuates steatohepatitis induced by the methionine choline deficient diet. J Hepatol. 2004;41:592–598. doi: 10.1016/j.jhep.2004.06.030. [DOI] [PubMed] [Google Scholar]
- 18.Hernandez E, Correa A, Bucio L, et al. Pentoxifylline diminished acetaldehyde-induced collagen production in hepatic stellate cells by decreasing interleukin-6 expression. Pharmacol Res. 2002;46:435–443. doi: 10.1016/s1043661802002025. [DOI] [PubMed] [Google Scholar]
- 19.Balibrea JL, Arias-Diaz J, Garcia C, Vara E. Effect of pentoxifylline and somatostatin on tumour necrosis factor production by human pulmonary macrophages. Circulatory Shock. 1994 Jun;43(2):51–6. [PubMed] [Google Scholar]
- 20.Abdel Salam OM, Aiuomy AR, El-Shenawy SM, et al. Effect of pentoxifylline on hepatic injury caused in the rat by the administration of carbon tetrachloride or acetaminophen. Pharmacol Rep. 2005;57:596–603. [PubMed] [Google Scholar]
- 21.Kozaki K, Egawa H, Bermudez L, et al. Effects of pentoxifylline pretreatment on Kupffer cells in rat liver transplantation. Hepatology. 1995;21:1079–82. [PubMed] [Google Scholar]
- 22.Romaneli RG, Caligiuri A, Carloni V, et al. Effect of pentoxifylline on the degradation of procollagen type I produced by hepatic stellate cells in response to transforming growth factor-beta 1. Br J Pharmacol. 1997;122:1047–54. doi: 10.1038/sj.bjp.0701484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Preaux AM, Mallat A, Rosenbaum J, et al. Pentoxifylline inhibits growth and collagen synthesis of cultured human hepatic myofibroblast-like cells. Hepatology. 1997;122:1047–54. doi: 10.1002/hep.510260210. [DOI] [PubMed] [Google Scholar]
- 24.Raetsch C, Jia JD, Boigk G, et al. Pentoxifylline downregulates profibrogenic cytokines and procollagen I expression in rat secondary biliary fibrosis. Gut. 2002;50:241–247. doi: 10.1136/gut.50.2.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Adams LA, Zein CO, Angulo P, Lindor KD. A pilot trial of pentoxifylline in nonalcoholic steatohepatitis. Am J Gastroenterol. 2004;99:2365–2368. doi: 10.1111/j.1572-0241.2004.40064.x. [DOI] [PubMed] [Google Scholar]
- 26.Satapathy S, Garg S, Chauhan R, et al. Beneficial effects of tumor necrosis factor-α inhibition by pentoxifylline on clinical, biochemical, and metabolic parameters of patients with nonalcoholic steatohepatitis. Am J Gastroenterol. 2004;99:1946–1952. doi: 10.1111/j.1572-0241.2004.40220.x. [DOI] [PubMed] [Google Scholar]
- 27.Kleiner DE, Brunt EM, Van Natta M, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41:1313–1321. doi: 10.1002/hep.20701. [DOI] [PubMed] [Google Scholar]
- 28.Bergman RN, Ider YZ, Bowden CR, Cobelli C. Quantitative estimation of insulin sensitivity. Am J Physiol. 1979;236:E667–77. doi: 10.1152/ajpendo.1979.236.6.E667. [DOI] [PubMed] [Google Scholar]
- 29.Welch S, Gebhart SS, Bergman RN, Phillips LS. Minimal model analysis of intravenous glucose tolerance test-derived insulin sensitivity in diabetic subjects. J Clin Endocrinol Metab. 1990;71:1508–1518. doi: 10.1210/jcem-71-6-1508. [DOI] [PubMed] [Google Scholar]
- 30.Boston RC, Stefanovski D, Moate PJ, et al. MINMOD Millennium: a computer program to calculate glucose effectiveness and insulin sensitivity from the frequently sampled intravenous glucose tolerance test. Diabetes Technol Ther. 2003;5:1003–15. doi: 10.1089/152091503322641060. [DOI] [PubMed] [Google Scholar]
- 31.Bergman RN, Prager R, Volund A, Olefsky JM. Equivalence of the insulin sensitivity index in man derived by the minimal model method and the euglycemic glucose clamp. J Clin Invest. 1987;79:790–800. doi: 10.1172/JCI112886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Loo DT, Rillema JR. Measurement of cell death. Methods Cell Biol. 1998;57:251–264. doi: 10.1016/s0091-679x(08)61583-6. [DOI] [PubMed] [Google Scholar]
- 33.Feldstein AE, Canbay A, Angulo P, et al. Hepatocyte apoptosis and Fas Expression are prominent features of human nonalcoholic steatohepatitis. Gastroenterology. 2003;125:437–443. doi: 10.1016/s0016-5085(03)00907-7. [DOI] [PubMed] [Google Scholar]
- 34.Miller ER, III, Pastor-Barriuso R, Dalal D, Riemersma RA, et al. Meta-analysis: high-dosage vitamin E supplementation may increase all-cause mortality. Ann Intern Med. 2005;142:37–46. doi: 10.7326/0003-4819-142-1-200501040-00110. [DOI] [PubMed] [Google Scholar]
- 35.Carter-Kent C, Zein NN, Feldstein AE. Cytokines in the pathogenesis of fatty liver and disease progression to steatohepatitis: implications for treatment. Am J of Gastroenterol. 2008;103:1036–1042. doi: 10.1111/j.1572-0241.2007.01709.x. [DOI] [PubMed] [Google Scholar]
- 36.Galluzi L, Aaronson SA, Abrams J, et al. Guidelines for the use and interpretation of assays for monitoring cell death in higher eukaryotes. Cell Death and Differentiation. 2009;16:1093–1107. doi: 10.1038/cdd.2009.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sekut L, Yarnall D, Sitmpson SA, et al. Anti-inflammatory activity of phosphodiesterase (PDE)-IV inhibitors in acute and chronic models of inflammation. Clin Exp Immunol. 1995;100:126–32. doi: 10.1111/j.1365-2249.1995.tb03613.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vircheva S, Alexandrova A, Georgieva A, et al. In vivo effects of pentoxifylline on enzyme and non-enzyme antioxidant levels in rat liver after carrageenan-induced paw inflammation. Cell Biochem Funct. 2010;28:668–72. doi: 10.1002/cbf.1705. [DOI] [PubMed] [Google Scholar]
- 39.Berman B, Duncan MR. Pentoxifylline inhibits the proliferation of human fibroblasts derived from keloid, scleroderma and morphoe skin and their production of collagen, glycosaminoglycans and fibronectin. Br J Dermatol. 1990;123:339–46. doi: 10.1111/j.1365-2133.1990.tb06294.x. [DOI] [PubMed] [Google Scholar]
- 40.Duncan MR, Hasan A, Berman B. Pentoxifylline, pentifylline, and interferons decrease type I and type III procollagen mRNA levels in dermal fibroblasts: evidence for mediation by nuclear factor I down-regulation. J Invest Dermatol. 1995;104:282–6. doi: 10.1111/1523-1747.ep12612819. [DOI] [PubMed] [Google Scholar]
- 41.Modi AA, Feld JJ, Park Y, et al. Increased caffeine consumption is associated with reduced hepatic fibrosis. Hepatology. 2010;51:201–9. doi: 10.1002/hep.23279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pentoxifylline DRUGDEX Evaluations. [Accessed on April 7, 2011];Micromedex® 2.0. http://www.thompsonhc.com/micromedex2.