Abstract
Prevalence of depression is high among individuals with type 2 diabetes (T2D). The objective of the current study was to identify the socio-demographic, psychosocial, cultural, and clinical risk factors that predispose to depression, and resources that protect from depression among low income Latinos with T2D. Participants (N = 211) were interviewed in their homes upon enrollment. Multivariate logistic regression was used to identify factors associated with depressive symptoms based on a score of ≥21 on the Center for Epidemiological Studies Depression scale. Lower household income, interference of diabetes with daily activities, and more T2D clinical symptoms were associated with depression risk in the multivariate analyses. At each level of food insecurity the risk of depression was lower the higher the level of social support (P < 0.05). Findings suggest that social support buffers against the negative influence of household food insecurity on depression risk. A comprehensive approach is necessary to address the mental health needs of low income Latinos with T2D.
Keywords: Depression, Type 2 diabetes, Latinos, Social support, Food insecurity, Low socio-economic status
Introduction
Gallo and Matthews propose that the association between lower socio-economic position and negative mood may be partially explained by frequent, intense, and chronic stress exposure attributable to the social environments where low-income individuals live [1]. They further posit that low socio-economic status (SES) may also be related to having fewer opportunities to develop and replenish health promoting resources [1]. In this context, resources may be tangible, such as access to food, interpersonal, such as social support or cultural integration, or intrapersonal, such as quality of life. National data suggests that low income families are especially vulnerable to food insecurity [2]. Food insecurity could be viewed as a chronic stressor because of the psychological, physical and socio-familial implications associated with it [3]. Low-income households are especially vulnerable to food insecurity. US Census Bureau data suggests that in 2008, 15% (17 million) of US households did not have access to nutritionally adequate and safe food for at least some time during the year. Among these, 39% of households (6.7 million) suffered from severe household food insecurity [2].
Pearlin’s stress process model suggests that even though new and existing stressful events may lead to mental stress, effect modifiers such as social support from family or friends could decrease the individual’s vulnerability to them [4]. Thus, on this basis we should expect that social support would protect low-income Latinos with diabetes from depression even in the presence of other stressors such as household food insecurity.
While it has been demonstrated that diabetes, and low SES are each individual risk factors for depression, it is largely unknown what factors predispose to, and protect from depression in the presence of these risk factors [5, 6]. Therefore, the purpose of this study was to identify risk factors associated with elevated depressive symptoms, and to determine if social support protects against depressive symptoms in the presence of risk factors (e.g., household food insecurity) in a sample of low income Latinos with T2D.
Methods
Study Participants
The baseline data of DIALBEST, a randomized controlled longitudinal trial involving peer-counselors (community health workers) in the diabetes care of low income Latino adults with T2D, was used for these analyses [7]. Participants were recruited from a ‘Metabolic Syndrome clinic’ at Hartford Hospital’s Brownstone Clinic. A baseline screening was conducted with the help of an electronic medical database designed to identify eligible candidates who were contacted in person by recruiters on their clinical appointment day at the clinic. A total of 211 participants were enrolled from December 2006 to February 2009. Participants were included if they: (1) were >21 years of age, (2) were living in Hartford County, CT, (3) had HbA1c levels ≥7%, and (4) had no medical conditions that completely limited their ability to perform physical activity. The objective of the DIALBEST study was to develop, implement and evaluate a best-practice model to support the management of type 2 diabetes among inner-city Latinos through peer-counselors. Participants were randomly assigned into either control (n = 106) or treatment group (n = 105). The treatment group received home visits from peer-counselors for 12 months in addition to the usual care available from the clinic. Data were collected at baseline, 3, 6, 12 and 18 months post-enrollment. The analyses presented in this article are derived from the baseline data.
Assessment
After obtaining participants’ written informed consent, one of three bicultural/bilingual interviewers conducted a face to-face interview. The survey modules in the questionnaires were either previously validated and used by other researchers [8–10] or by our own group among Latinos with type 2 diabetes [11]. Before starting data collection with DIALBEST participants, the survey was pre-tested among five bi-cultural/bi-lingual (Spanish and English) staff at the Hispanic Health Council, Hartford. Additionally, the English and Spanish versions were tested with five English and five Spanish speaking DIALBEST participants. As shown by the post-hoc Cronbach’s alpha results from the baseline sample (see below) the internal consistency of the scales was adequate supporting the validity of the survey instrument used in this study. The interviews were conducted in English or Spanish according to participant’s preference. This study was approved by the Institutional Review Boards of all collaborating institutions.
Dependent Variable: Elevated Depressive Symptoms
Depressive symptoms were measured using the Center for Epidemiologic Studies (CES-D) Scale [12], a reliable and valid tool among Latinos including Puerto Ricans [13]. The scale consists of 20 items that ask how often each of a series of depressive symptoms was experienced over the past week. Response options range from 0 = “none of the time” to 3 = “most or all the time”, with total scores ranging from 0 to 60 (Cronbach alpha = 0.88). As recommended for populations with T2D [14, 15] the CES-D cut-off score ≥21 was used to designate elevated depressive symptoms.
Independent Variables
Demographic and Socio-Economic Variables
Demographic variables included age, gender, ethnicity, marital status, smoking status, and household size. Socioeconomic variables included monthly income, education, employment status, and food security. Food security was assessed with a previously validated [8] short form of the US household food security supplement module [US-HFSSM] module [16]. The score ranged from 0 to 5, with five indicating extreme food insecurity (Cronbach alpha = 0.89).
Psychosocial Variables
Social support was measured using an 11 item-questionnaire that asks about the support given by family and friends [17]. The three-point scale response options ranged from “never available” to “always available”, with the total social support score ranging from 0 to 22 (Cronbach alpha = 0.87).
Perceived interference of diabetes on the respondent’s ability to engage in particular activities was assessed using the modified Interference subscale of Multi Dimensional Diabetes Questionnaire [18]. Out of the nine original questions, five original questions (Questions 1, 4, 7, 8 and 15), and an additional question on the perceived interference on making/having enough money were used in the current study. The responses were recorded on a four-point scale ranging from “not at all” to “a lot” (Cronbach alpha = 0.77).
Cultural Variables
Acculturation was assessed with a modified 21-item version of the Acculturation Rating Scale for Mexican Americans-II (ARSMA), scale 1 [19]. Although this scale was originally developed for Mexican Americans, Cuellar et al. [19] suggested that it may be used among other Latino groups. This scale has indeed been successfully used with Puerto-Ricans [9] and is one of the most comprehensive and commonly used Latino acculturation scales [20]. Using ARSMA’s recommended method, we generated cut-off scores to classify individuals into five acculturation categories ranging from strongly Mexican oriented to strongly Anglo oriented. Amount of time respondent had lived in the US was also measured.
Clinical Variables
Clinical factors included health insurance status, fasting plasma glucose (FPG), glycosylated hemoglobin (HbA1c) levels, body mass index (calculated from weight and height measurements), diabetes related clinical symptoms, self-reported health status, insulin use and number of medications consumed.
Fasting blood (2 mL) was collected and fasting plasma glucose (FPG) was measured using a YSI-2300 stat plus glucose & lactate analyzer (YSI life sciences, Yellow Springs, OH) in duplicate. HbA1c was measured from capillary blood using an FDA approved and National Glycohemoglobin Standardization Program certified instrument that accurately measures HbA1c in home settings—‘A1cNow INView’ device (Metrika Inc., Sunnyvale, CA).
Self rated health was assessed by asking the standard question ‘how would you rate your overall health?’ [21]. Response options were (1) excellent, (2) very good, (3) good, (4) fair, and (5) poor. In the current study, the first four categories were grouped together and classified as ‘fair to excellent health’, and the fifth category remained labeled as ‘poor health’ in order to adjust the multivariate analyses for this potential confounder, as poor health has been previously associated with both depression and food insecurity.
Diabetes-related symptoms were measured on the basis of, presence or absence of six clinical symptoms: extreme thirst, extreme hunger, frequent urination, blurred vision, pain in legs, and tingling or numbness in extremities.
Details of all prescription and non-prescription medications used by participants were collected from which numbers of medications by type consumed per day were computed. Participants were further classified based on whether or not they used insulin.
Statistical Analyses
Data were analyzed using the Statistical Program for the Social Sciences for Windows (SPSS v.19.0; IBM Corporation, New York). Comparisons between participants with elevated and non-elevated depressive symptoms were conducted using t test for continuous variables and Chi-square test for categorical variables. Variables that were found to be significantly (P ≤ 0.05) associated with elevated depressive symptoms were entered into multivariate logistic regression model. In addition, variables with proven theoretical association with depression symptoms such as gender, HbA1c levels, body mass index, and insulin use were entered into the model as covariates. In order to test our a priori hypothesis that higher social-support buffers the effects of food insecurity on elevated depression symptoms, a social support × food insecurity interaction was also included in the model. To interpret the interaction results, the logistic regression parameters were used to predict the probability of depression for each level of food insecurity (range: 0–5) as a function of social support status [low (score = 0), middle (score = 12), high (score = 22)]. Similar effects were found with linear multivariate analyses using depression score as a continuous variable with regard to diabetes interference score, diabetes related clinical symptoms and social support × food insecurity interaction. Thus, only logistic regression results are presented.
Results
Participants Characteristics
The majority of respondents were middle aged (mean = 56.4 years), women (74%) of Puerto-Rican origin (94%). About 43% of participants were separated, divorced or widowed. About two-thirds lived in households with a monthly income ≤$1,000. Over two-thirds of the participants did not finish high school (69%) and only 16% were employed. About two-thirds (65%) of the participants spoke Spanish only. Almost all (97%) reported basic government sponsored health insurance (Table 1).
Table 1.
Associations between participants’ characteristics, and elevated depressive symptoms among Latinos with type 2 diabetes
| Variables | All | Non-elevated depressive symptoms | Elevated depressive symptoms | i | P | ||
|---|---|---|---|---|---|---|---|
| Age (y) | |||||||
| Mean (n) | 56.4 (211) | SD = 11.8 | 56.2 (106) | SD = 12.3 | 56.5 (105) | SD = 11.3 | 0.86 |
| Gender, % (n) | |||||||
| Male | 26.5 (56) | 29.2 (31) | 23.8 (25) | 0.37 | |||
| Female | 73.5 (155) | 70.8 (75) | 76.2 (80) | ||||
| Ethnicity, % (n) | |||||||
| PR/PR American | 93.8 (198) | 90.6 (96) | 97.1 (102) | 0.05 | |||
| Other Hispanics | 6.2 (13) | 9.4 (10) | 2.9 (3) | ||||
| Marital status, % (n) | |||||||
| Single | 28.0 (59) | 25.5 (27) | 30.5 (32) | 0.61 | |||
| Married/living together | 29.4 (62) | 32.1 (34) | 26.7 (28) | ||||
| Separated/widowed/divorced | 42.7 (90) | 42.5 (45) | 42.9 (45) | ||||
| Smoking, % (n) | |||||||
| Quit smoking | 43.1 (78) | 32.7 (34) | 41.9 (44) | 0.26 | |||
| No | 36.5 (89) | 48.1 (50) | 37.1 (39) | ||||
| Yes | 20.4 (42) | 19.2 (20) | 21.0 (22) | ||||
| Household size | |||||||
| Mean (n) | 2.6 (211) | SD = 1.6 | 2.9 (106) | SD = 1.7 | 2.2 (105) | SD = 1.4 | 0.004 |
| Monthly household income, % (n) | |||||||
| < $1,000 | 65.1 (127) | 58.3 (56) | 71.7 (71) | 0.03 | |||
| $1,001–1,500 | 27.2 (53) | 29.2 (28) | 25.3 (25) | ||||
| > $1,500 | 7.7 (15) | 12.5 (12) | 3.0 (3) | ||||
| Education, % (n) | |||||||
| No education | 4.3 (9) | 3.8 (4) | 4.8 (5) | 0.22 | |||
| Some schooling | 69.7 (147) | 71.7 (76) | 67.6 (71) | ||||
| High school graduate/technical training | 19.9 (42) | 21.7 (23) | 18.1 (19) | ||||
| College education | 6.2 (11) | 2.8 (3) | 9.5 (10) | ||||
| Employment, % (n) | |||||||
| Yes | 15.6 (33) | 21.7 (23) | 9.5 (10) | 0.02 | |||
| No | 84.4 (178) | 78.3 (77) | 90.5 (101) | ||||
| Food insecurity | |||||||
| Mean (n) | 1.9 (211) | SD = 2.0 | 1.6 (106) | SD = 1.9 | 2.3 (105) | SD = 2.0 | 0.01 |
| Social support | |||||||
| Mean (n) | 12.0 (211) | SD = 6.1 | 13.0 (106) | SD = 6.1 | 11.0 (105) | SD = 5.9 | 0.02 |
| Interference scale score | |||||||
| Mean (n) | 13.4 (211) | SD = 5.0 | 12.0 (106) | SD = 4.5 | 14.8 (105) | SD = 5.0 | <0.001 |
| Length of stay in the US | |||||||
| Mean (n) | 25.8 (204) | SD = 12.7 | 25.2 (104) | SD = 12.1 | 26.4 (100) | SD = 13.3 | 0.49 |
| Acculturation, % (n) | |||||||
| Level 1 | 3.8 (8) | 3.8 (4) | 3.8 (4) | 0.31 | |||
| Level 2 | 31.8 (67) | 33.0 (35) | 30.5 (32) | ||||
| Level 3 | 38.4 (81) | 42.5 (45) | 34.3 (36) | ||||
| Level 4 | 15.6 (33) | 10.4 (11) | 21.0 (22) | ||||
| Level 5 | 10.4 (22) | 10.4 (11) | 10.5 (11) | ||||
| Insurance, % (n) | |||||||
| Yes | 86.3 (182) | 82.1 (87) | 90.5 (95) | 0.08 | |||
| No | 13.7 (29) | 17.9 (19) | 9.5 (10) | ||||
| Fasting plasma glucose (mmol/L) | |||||||
| Mean (n) | 10.6 (211) | SD = 4.7 | 10.4 (106) | SD = 4.4 | 10.8 (105) | SD = 5.0 | 0.56 |
| HbA1c (%) | |||||||
| Mean (n) | 9.6 (211) | SD = 1.8 | 9.5 (106) | SD = 1.7 | 9.7 (105) | SD = 1.9 | 0.49 |
| Body mass index | |||||||
| Mean (n) | 33.7 (211) | SD = 7.8 | 34.0(106) | SD = 8.3 | 33.4 (105) | SD = 7.2 | 0.56 |
| Number of clinical symptoms | |||||||
| Mean (n) | 3.6 (211) | SD = 1.8 | 3.0 (106) | SD = 1.8 | 4.3 (105) | SD = 1.5 | <0.001 |
| Self reported health, % (n) | |||||||
| Fair to excellent | 84.8 (178) | 93.4 (99) | 76.0 (79) | <0.001 | |||
| Poor health | 15.2 (32) | 6.6 (7) | 24.0 (25) | ||||
| Insulin use, % (n) | |||||||
| No | 50.2 (101) | 54.5 (55) | 46.0 (46) | 0.23 | |||
| Yes | 49.8 (100) | 45.5 (46) | 54.0 (54) | ||||
| Number of medications | |||||||
| Mean (n) | 7.1 (211) | SD = 4.0 | 6.3 (106) | SD = 3.7 | 7.8 (105) | SD = 4.1 | 0.004 |
| CES-D scores, mean (n) | 21.7 (211) | SD = 13 | |||||
| Score ≥ 21, % (n) | 49.8 (105) | ||||||
| On antidepressant | 38.1 (40) | ||||||
| Not on antidepressant | 61.9 (65) | ||||||
PR Puerto-Rican
Most respondents were obese. Per study selection criteria, participants had poor glycemic control; mean FPG and HbA1c were 10.6 mmol/L (~191 mg/dL) and 9.6%, respectively. About half of the study participants used insulin (50%). The mean CES-D sample score was 21.7. About half (50%) endorsed clinically elevated depressive symptoms and only one-third of those reported taking antidepressant medications. Mean numbers of diabetes related clinical symptoms, and number of medications consumed daily were 3.6 and 7, respectively.
Bivariate Analyses
Participants with clinically elevated depressive symptoms were more likely to: identify themselves as Puerto-Ricans, live in households with fewer members, have lower income, be unemployed, have higher household food-insecurity, lower social support and higher diabetes interference scores, have higher number of diabetes related clinical symptoms, report poor health and have higher medication use (Table 1).
Multivariate Analyses
In the multivariate model, the following risk factors were significantly associated with elevated depressive symptoms: lower household income, higher perceived diabetes interference score, and higher diabetes related clinical symptoms (Table 2). At each level of food insecurity the risk of depression was lower the higher the level of social support (P < 0.05). Thus, findings suggest that social support buffers against the negative influence of household food insecurity on depression risk (Fig. 1).
Table 2.
Factors associated with risk of elevated depressive symptoms among Latinos with type 2 diabetes
| Variables (n) | Adjusted odds ratio | 95.0% CI |
|---|---|---|
| Gender | ||
| Male (48) | 0.56 | 0.24, 1.14 |
| Female (137) | 1 | – |
| Ethnicity | ||
| PR/PR American (175) | 2.75 | 0.42, 17.92 |
| Other Latinos (10) | 1 | – |
| Monthly household income | ||
| ≤$1,000 (121) | 5.26 | 1.16, 63.40 |
| $1,001–1,500 (49) | 9.76 | 1.61, 59.28 |
| > $1,500 (15) | 1 | – |
| Employment | ||
| Yes (28) | 0.35 | 0.10, 1.28 |
| No (157) | 1 | – |
| Household size (185) | 1.04 | 0.78, 1.39 |
| Household food insecurity (185) | 1.54 | 1.00, 2.37 |
| Social support (185) | 1.02 | 0.93, 1.11 |
| Interference score (185) | 1.11 | 1.02. 1.21 |
| HbA1c (185) | 1.12 | 0.90, 1.38 |
| Body mass index (185) | 0.96 | 0.91, 1.01 |
| Self rated health status | ||
| Fair to excellent (157) | 0.34 | 0.10, 1.14 |
| Poor health (28) | 1 | – |
| Number of clinical symptoms (185) | 1.66 | 1.29, 2.13 |
| Number of medications (185) | 1.05 | 0.96, 1.16 |
| Insulin use | ||
| No (91) | 1.55 | 0.68, 3.51S |
| Yes (94) | 1 | – |
| Social support × food insecurity | 0.96 | 0.93, 0.99 |
Multivariate logistic regression: Hosmer–Lemeshow goodness of fit test P value = 0.27
PR Puerto-Rican
Fig. 1.
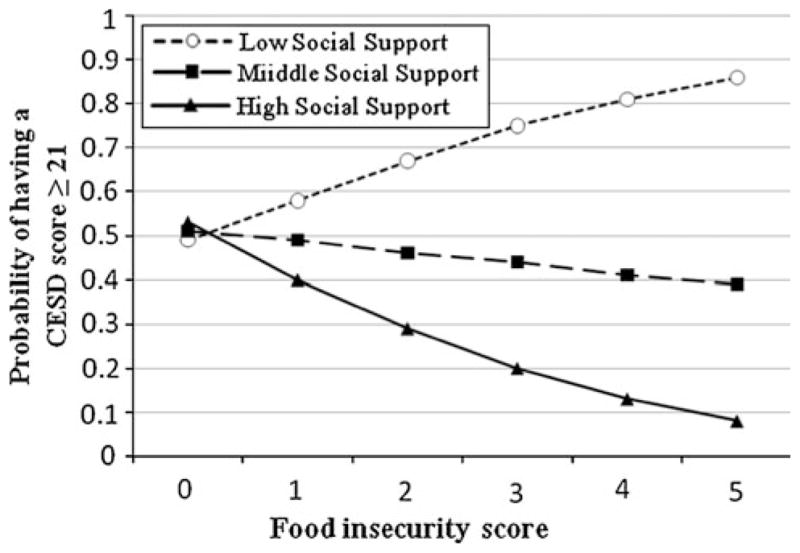
Social support × food insecurity interaction plot constructed using the logistic regression parameters to predict the probability of depression [CESD (Center for Epidemiological Studies Depression scale) score ≥21] for each level of food insecurity (range: 0–5) as a function of social support status [low (score = 0), middle (score = 12), high (score = 22)]
Discussion
Studies conducted among non-diabetic populations have consistently shown food insecurity to be associated with depression risk [3, 22–24]. To our knowledge, our study is one of the first to examine this association among individuals with T2D. Limited availability, access and/or intake of nutritionally adequate foods [2] may have direct biological effects on the central nervous system [25–28] in addition to psychological effects associated with the feelings of deprivation, restricted food choices, and constant anxiety or worry about availability of food supplies [29, 30]. Individuals from food insecure households also suffer from feelings of shame, powerlessness and guilt [29]. Household food insecurity is prevalent among vulnerable groups in the US and is emerging as an important psycho-social stressor that can lead to poor mental and physical health outcomes [3]. Household food insecurity in the US has been previously associated with type 2 diabetes [31], hypertension [32], and hyperlipidemia [32], obesity [33], and nutritional deficiencies [34]. It also has several social implications [3], as well. Our study documents that food insecurity is a risk factor for depression among Latinos with T2D.
An encouraging and innovative finding from our study is that higher social support protects low-income individuals with uncontrolled diabetes living in very food insecure households from developing elevated depression symptoms. Social networking could facilitate positive reinforcements such as a sense of belonging, and buffer the negative impacts of food insufficiency on poor mental health [35]. Indeed, relying on family or friends for protective resources such as food, money, or emotional support may help mitigate the negative consequences of major stressors [4, 30, 36, 37] such as household food insecurity. Pearlin’s process model of mental stress indeed supports our key finding that social support buffers the negative influence of food insecurity on depression risk [4].
Our study confirmed that lower household income (<$1,500/month) increases the risks for having elevated depressive symptoms in individuals with type 2 diabetes even after adjusting for other risk factors. Lower income in socio-demographically disadvantaged groups further strains the ability of individuals to cope with stress [1]. Limited resources to attend to other household (e.g. heating, electricity, and rent) [38], individual (e.g. transportation, clothing, and exercise facilities), and diabetes specific (e.g. diabetes self-management tools) needs could impose significant mental stress leading to depression [4].
Our study suggests that depression risk is associated with the perception of how much diabetes interferes with work, income generation, relationship with partner, daily routine activities, and/or social activities. This suggests that unmet psycho-emotional needs such as one’s personal relationships or social roles can affect depression risk independently from socio-demographic factors. Additionally, consistent with previous studies [39] higher numbers of clinical symptoms that are commonly associated with diabetes increased the risk for having elevated depression symptoms.
Limitations
Some limitations should be noted. Data were collected cross-sectionally, so the temporal sequence of depressive symptoms and their associated factors cannot be determined. Several underlying variables such as certain personality traits or genetic predispositions, which influence depression, diabetes, and the context in which individuals live, were not measured and thus could not be controlled for in the multivariate model. Participants were predominantly female Puerto Ricans, thus limiting generalization to other populations.
Implications and Conclusions
Our findings suggest that programs that are successful at increasing social capital in socio-economically deprived communities are also likely to protect the mental health of vulnerable individuals even in the presence of high levels of common and persistent stressors such as food insecurity among individuals with type 2 diabetes.
Acknowledgments
This study was funded and supported by Connecticut NIH Export Center for Eliminating Health Disparities among Latinos (NIH-NCMHD grant # P20MD001765). We would like to thank all study participants and community health care workers at the Hispanic Health Council. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center on Minority Health and Health Disparities or the National Institutes of Health.
Contributor Information
Grace Kollannoor-Samuel, Email: grace.kollannoor_samuel@uconn.edu, University of Connecticut, Unit 4017, 3624 Horse Barn Hill Rd Ext, Storrs, CT 06269, USA. Connecticut Center for Eliminating Health Disparities Among Latinos (CEHDL), Storrs, CT, USA.
Julie Wagner, Connecticut Center for Eliminating Health Disparities Among Latinos (CEHDL), Storrs, CT, USA. University of Connecticut Health Center, Farmington, CT, USA.
Grace Damio, Connecticut Center for Eliminating Health Disparities Among Latinos (CEHDL), Storrs, CT, USA. Hispanic Health Council, Hartford, CT, USA.
Sofia Segura-Pérez, Connecticut Center for Eliminating Health Disparities Among Latinos (CEHDL), Storrs, CT, USA. Hispanic Health Council, Hartford, CT, USA.
Jyoti Chhabra, Connecticut Center for Eliminating Health Disparities Among Latinos (CEHDL), Storrs, CT, USA. Hartford Hospital, Hartford, CT, USA.
Sonia Vega-López, Connecticut Center for Eliminating Health Disparities Among Latinos (CEHDL), Storrs, CT, USA. Arizona State University, Mesa, AZ, USA.
Rafael Pérez-Escamilla, Connecticut Center for Eliminating Health Disparities Among Latinos (CEHDL), Storrs, CT, USA. Yale School of Public Health, New Haven, CT, USA.
References
- 1.Gallo LC, Matthews KA. Understanding the association between socioeconomic status and physical health: do negative emotions play a role? Psychol Bull. 2003;129:10–51. doi: 10.1037/0033-2909.129.1.10. [DOI] [PubMed] [Google Scholar]
- 2.Nord M, Andrews M, Carlson S. Household food security in the United States, 2008: Economic Research Report. United States Department of Agriculture; 2009. pp. 1–66. [Google Scholar]
- 3.Hamelin AM, Habicht JP, Beaudry M. Food insecurity: consequences for the household and broader social implications. J Nutr. 1999;129:525S–8S. doi: 10.1093/jn/129.2.525S. [DOI] [PubMed] [Google Scholar]
- 4.Pearlin LI, Lieberman MA, Menaghan EG, Mullan JT. The stress process. J Health Soc Behav. 1981;22:337–56. [PubMed] [Google Scholar]
- 5.Pineda Olvera AE, Stewart SM, Galindo L, Stephens J. Diabetes, depression, and metabolic control in Latinas. Cultur Divers Ethnic Minor Psychol. 2007;13:225–31. doi: 10.1037/1099-9809.13.3.225. [DOI] [PubMed] [Google Scholar]
- 6.Ell K, Katon W, Cabassa LJ, Xie B, Lee PJ, Kapetanovic S, Guterman J. Depression and diabetes among low-income Hispanics: design elements of a socioculturally adapted collaborative care model randomized controlled trial. Int J Psychiatry Med. 2009;39:113–32. doi: 10.2190/PM.39.2.a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Perez-Escamilla R, Vega-López S, Damio G, Segura-Pérez S, Fernandez ML, Calle MC, Kollannoor Samuel G, Chhabra J, D’Agostino D. Short and long term impacts of diabetes peer counseling on HbA1c among Latinos: preliminary results. Fed Am Soc Exp Biol J. 2009;23:336–8. [Google Scholar]
- 8.Hromi-Fiedler A, Bermudez-Millan A, Melgar-Quinonez H, Perez-Escamilla R. Psychometric properties of an adapted version of the US household food security survey module for assessing food insecurity among low-income pregnant Latinas. J Hunger Environ Nutr. 2009;4:81–94. doi: 10.1080/19320240802706866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Teichman JR, Contreras-Grau JM. Acculturation and teaching styles among young mainland Puerto Rican mothers. Hisp J Behav Sci. 2006;28:84–101. [Google Scholar]
- 10.Hammons ME. The importance of addressing acculturative stress in marital therapy with Hispanic American women [Master of Science Thesis] Orlando, Florida: University of Central Florida; 2007. [Google Scholar]
- 11.Fitzgerald N. Identification of risk factors mediating the associations of socio-economic, cultural, and demographic factors with type 2 diabetes across ethnic groups [Doctoral Thesis] Storrs, Connecticut: University of Connecticut; 2004. [Google Scholar]
- 12.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. App Psych Meas. 1977;1:385–401. [Google Scholar]
- 13.Vera M, Alegria M, Freeman D, Robles RR, Rios R, Rios CF. Depressive symptoms among Puerto Ricans: island poor compared with residents of the New York City area. Am J Epidemiol. 1991;134:502–10. doi: 10.1093/oxfordjournals.aje.a116122. [DOI] [PubMed] [Google Scholar]
- 14.Turk DC, Okifuji A. Detecting depression in chronic pain patients: adequacy of self-reports. Behav Res Ther. 1994;32:9–16. doi: 10.1016/0005-7967(94)90078-7. [DOI] [PubMed] [Google Scholar]
- 15.Zich JM, Attkisson CC, Greenfield TK. Screening for depression in primary care clinics: the CES-D and the BDI. Int J Psychiatry Med. 1990;20:259–77. doi: 10.2190/LYKR-7VHP-YJEM-MKM2. [DOI] [PubMed] [Google Scholar]
- 16.Blumberg SJ, Bialostosky K, Hamilton WL, Briefel RR. The effectiveness of a short form of the Household Food Security Scale. Am J Public Health. 1999;89:1231–4. doi: 10.2105/ajph.89.8.1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zimet GD, Dahlem NW, Zimet SG, Farley GK. The multidimensional scale of perceived social support. J Pers Assess. 1988;52:30–41. doi: 10.1080/00223891.1990.9674095. [DOI] [PubMed] [Google Scholar]
- 18.Talbot F, Nouwen A, Gingras J, Gosselin M, Audet J. The assessment of diabetes-related cognitive and social factors: the Multidimensional Diabetes Questionnaire. J Behav Med. 1997;20:291–312. doi: 10.1023/a:1025508928696. [DOI] [PubMed] [Google Scholar]
- 19.Cuellar I, Arnold B, Maldonado R. Acculturation rating-scale for Mexican-Americans II—a revision of the original ARSMA scale. Hisp J Behav Sci. 1995;17:275–304. [Google Scholar]
- 20.Garcia L, Hurwitz EL, Kraus JF. Acculturation and reported intimate partner violence among Latinas in Los Angeles. J Interpers Violence. 2005;20:569–90. doi: 10.1177/0886260504271582. [DOI] [PubMed] [Google Scholar]
- 21.DeSalvo KB, Bloser N, Reynolds K, He J, Muntner P. Mortality prediction with a single general self-rated health question. A meta-analysis. J Gen Intern Med. 2006;21:267–75. doi: 10.1111/j.1525-1497.2005.00291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Maes KC, Hadley C, Tesfaye F, Shifferaw S. Food insecurity and mental health: surprising trends among community health volunteers in Addis Ababa, Ethiopia during the 2008 food crisis. Soc Sci Med. 2010;70:1450–7. doi: 10.1016/j.socscimed.2010.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pérez-Escamilla R. Food insecurity and hunger in children: impact on physical and psycho-emotional development. In: Ross CA, Caballero B, Cousins RJ, Tucker KL, Ziegler TR, editors. Modern nutrition in health and disease. 11. Baltimore, MD: Lippincott Williams & Wilkins; (In Press) [Google Scholar]
- 24.National Research Council, Committee on National Statistics, Division of Behavioral and Social Sciences and Education. Food insecurity and hunger in the United States: an assessment of the measure. Washington, DC: The National Academies Press; 2006. [Google Scholar]
- 25.Berk M, Sanders KM, Pasco JA, Jacka FN, Williams LJ, Hayles AL, Dodd S. Vitamin D deficiency may play a role in depression. Med Hypotheses. 2007;69:1316–9. doi: 10.1016/j.mehy.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 26.Penninx BW, Guralnik JM, Ferrucci L, Fried LP, Allen RH, Stabler SP. Vitamin B(12) deficiency and depression in physically disabled older women: epidemiologic evidence from the Women’s Health and Aging Study. Am J Psychiatry. 2000;157:715–21. doi: 10.1176/appi.ajp.157.5.715. [DOI] [PubMed] [Google Scholar]
- 27.Cabrera MA, Mesas AE, Garcia AR, de Andrade SM. Malnutrition and depression among community-dwelling elderly people. J Am Med Dir Assoc. 2007;8:582–4. doi: 10.1016/j.jamda.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 28.Guedes RC, Monteiro JS, Teodosio NR. Malnutrition and brain function: experimental studies using the phenomenon of cortical spreading depression. Rev Bras Biol. 1996;56(Su 1 Pt 2):293–301. [PubMed] [Google Scholar]
- 29.Wu Z, Schimmele CM. Food insufficiency and depression. Sociol Perspect. 2005;48:481–504. [Google Scholar]
- 30.Radimer K, Olson C, Greene J, Campbell C, Habicht J. Understanding hunger and developing indicators to assess it in women and children. J Nutr Educ. 1992;24:36S–44S. [Google Scholar]
- 31.Seligman HK, Bindman AB, Vittinghoff E, Kanaya AM, Kushel MB. Food insecurity is associated with diabetes mellitus: results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999–2002. J Gen Intern Med. 2007;22:1018–23. doi: 10.1007/s11606-007-0192-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr. 2011;140:304–10. doi: 10.3945/jn.109.112573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Adams EJ, Grummer-Strawn L, Chavez G. Food insecurity is associated with increased risk of obesity in California women. J Nutr. 2003;133:1070–4. doi: 10.1093/jn/133.4.1070. [DOI] [PubMed] [Google Scholar]
- 34.Eicher-Miller HA, Mason AC, Weaver CM, McCabe GP, Boushey CJ. Food insecurity is associated with iron deficiency anemia in US adolescents. Am J Clin Nutr. 2009;90:1358–71. doi: 10.3945/ajcn.2009.27886. [DOI] [PubMed] [Google Scholar]
- 35.Ahluwalia IB, Dodds JM, Baligh M. Social support and coping behaviors of low-income families experiencing food insufficiency in North Carolina. Health Educ Behav. 1998;25:599–612. doi: 10.1177/109019819802500507. [DOI] [PubMed] [Google Scholar]
- 36.Campbell C, Desjardins E. A model and research approach for studying the management of limited food resources by low-income families. J Nutr Educ. 1992;21:162–70. [Google Scholar]
- 37.Dodds J, Ahluwalia I, Baligh M. Experiences of families using food assistance and welfare programs in North Carolina: perceived barriers and recommendations for improvement. J Nutr Educ. 1996;28:101–8. [Google Scholar]
- 38.Seguin L, Potvin L, St-Denis M, Loiselle J. Chronic stressors, social support, and depression during pregnancy. Obstet Gynecol. 1995;85:583–9. doi: 10.1016/0029-7844(94)00449-N. [DOI] [PubMed] [Google Scholar]
- 39.Ludman EJ, Katon W, Russo J, Von Korff M, Simon G, Ciechanowski P, Lin E, Bush T, Walker E, Young B. Depression and diabetes symptom burden. Gen Hosp Psychiatry. 2004;26:430–6. doi: 10.1016/j.genhosppsych.2004.08.010. [DOI] [PubMed] [Google Scholar]


