Abstract
Objective
To examine the efficacy of exposure-based CBT plus a structured family intervention (FCBT) versus psychoeducation plus relaxation training (PRT) for reducing symptom severity, functional impairment, and family accommodation in youths with OCD.
Methods
Seventy-one 8–17 year old youngsters (mean 12.2 years, range 8–17, 37% male, 78% Caucasian) with primary OCD were randomized (70:30) to 12 sessions over 14 weeks of FCBT or PRT. Blind raters assessed outcomes with responders followed for six months to assess treatment durability.
Results
FCBT led to significantly higher response rates than PRT in ITT (57.1% vs 27.3%) and completer analyses (68.3% vs.35.3%). Using HLM, FCBT was associated with significantly greater change in OCD severity and child-reported functional impairment than PRT and marginally greater change in parent-reported accommodation of symptoms. These findings were confirmed in some, but not all, secondary analyses. Clinical remission rates were 42.5% for FCBT vs. 17.6% for PRT. Reduction in family accommodation temporally preceded improvement in OCD for both groups and child functional status for FCBT only. Treatment gains were maintained at 6-months.
Conclusions
FCBT is effective for reducing OCD severity and impairment. Importantly, treatment also reduced parent-reported involvement in symptoms with reduced accommodation preceding reduced symptom severity and functional impairment.
Clinical Trials Registry Information
Behavior Therapy for Children and Adolescents with Obsessive-Compulsive Disorder (OCD); http://www.clinicaltrials.gov; Unique Identifier: NCT00000386
Keywords: obsessive-compulsive disorder, child and adolescent, cognitive behavioral therapy, functional impairment, family accommodation
Pediatric obsessive compulsive disorder (OCD) is a common, functionally-impairing and distressing condition that can be debilitating in its severe forms.1,2,3 Untreated, the disorder is usually chronic, disrupts normal development and places youth at risk for multiple concurrent and long-term psychiatric comorbidities.3 Thus, the development and testing of effective interventions for childhood OCD remains a clear public health priority.
To date, evidence has emerged to support the efficacy of both exposure-based cognitive-behavior therapy (CBT) and pharmacological intervention with the serotonin reuptake inhibitors (SRIs) for this disorder.4,5,6,7,8,9 A recent meta-analysis of randomized-controlled trials for pediatric OCD yielded effect sizes of 1.45 (95%CI=.68–2.22) for CBT and 0.48 for pharmacotherapy (95%CI=.36–.61);8 however, weaknesses in comparison conditions and other features complicate interpretation of the extant data. Based on existing comparative efficacy and safety data, CBT has emerged as the most-often recommended first-line treatment for OCD in youth.4,8,9
Nonetheless, efforts to optimize CBT and establish its effectiveness for pediatric OCD lag behind similar efforts for other disorders,9 and surprisingly, no treatments for this disorder currently meet criteria as a well-established evidence-based psychosocial treatment.10 Although the CBT literature for pediatric OCD may seem crowded, a recent review4 identified only two methodologically rigorous published randomized controlled trials (e.g., Type 1 studies)11, comprising a total of 81 subjects treated with CBT alone.7,12 Although several less-rigorously designed CBT trials (e.g., Type 2 studies, defined as including a comparison group but with other methodological limitations)11 have been published,4 methodological concerns, including lack of random assignment, small sample size, or comparison of different intensity levels of the same treatment, partially limit their impact for determining the efficacy of exposure-based therapy for childhood OCD.
Importantly, no adequately powered randomized-controlled CBT trial for pediatric OCD has utilized a matched active comparison condition designed to control for the nonspecific effects of exposure-based CBT. Such a design is critical for determining whether or not the mechanisms underlying an observed treatment effect go beyond the nonspecific consequences of attention or the expectation of change.10 Moreover, because they are designed to isolate putative “active” treatment elements, psychotherapy trials that employ active comparison groups both increase confidence in the specific explanatory model on which the treatment is based and suggest that particular kinds of training and experience may be necessary to produce the desired treatment effect.10
Thus, the design of the current study, which contrasts individual exposure-based CBT for the child plus a concurrent family intervention (FCBT) with a matched active psychosocial comparison treatment consisting of psychoeducation about OCD plus systematic relaxation training (PRT) represents an important step for establishing the efficacy of FCBT for child OCD, especially in light of past non-OCD pediatric anxiety trials that failed to differentiate CBT from comparison therapies.13,14
The need for expanded research in this area is driven by several additional concerns. Perhaps most important is the realization of substantial room for improvement in treatment outcomes for pediatric OCD, particularly in light of findings that over half of study participants fail to achieve symptom remission in response to CBT,7 regardless of treatment condition. One potential target for optimizing the efficacy of existing approaches is the inclusion of intervention techniques to address family factors that may undermine response.15,16,17 In particular, accommodation (i.e., participation in rituals and/or modification of routines) is highly common among families of OCD youth15,17 and may mediate the link between symptom severity and functional impairment.17 Family accommodation is thought to be a barrier to treatment inasmuch as it reinforces avoidance behaviors and undermines exposure-based exercises.15
Unfortunately, research evaluating systematic efforts to address family accommodation and related factors is complicated by the heterogeneous nature of the literature with regard to the intensity and structure of family involvement, especially since some level of parental involvement in treatment is typically specified for OCD youth. Barrett et al.4 attempted to clarify confusion over what constitutes a “family treatment” by defining individual child+family interventions (FCBT) as those treatments which specify structured weekly intervention sessions focused on changing family dynamics as opposed to primarily individual child treatments which include family members in a less-structured or less-frequent manner, often as a brief check-in at the end of individual sessions. Using this definition, only two studies, one Type 1 (N=77)12 and one Type 2 (N=40)18 have critically evaluated FCBT, and only one18 found post-treatment changes in family dynamics, with families receiving intensive FCBT demonstrating greater reduction in family accommodation compared to those receiving weekly treatment. Moreover, in a partially-overlapping sample of children receiving FCBT through one of two separate open-label studies (N=49), decreases in family accommodation over the course of treatment predicted reduced symptom severity and OCD-related impairment post-treatment.19 Although requiring replication under controlled conditions, these findings suggest that efforts to target relevant family dynamics may lead to improved treatment outcomes.
Finally, only one prior published controlled FCBT trial for childhood OCD has employed a credible psychosocial comparison condition.20 Although including a relaxation training comparison condition similar to that used herein, this study was primarily a feasibility trial (N=42) not powered to address efficacy adequately and differed from the current study in several important ways, including a the use of a parent-focused play-therapy protocol designed for use with 5–8 year old children. As a result, generalization of findings to youngsters over age eight who comprise the largest share of treatment-seeking youth with OCD is limited. Unfortunately, the absence of rigorous comparative efficacy data for exposure-based CBT versus a credible psychosocial intervention limits conclusions about the efficacy of this treatment, its active ingredients, and impedes its potential classification as a “well-established” or even “probably efficacious” evidence-based intervention according to current guidelines.4,10
The goal of the current study was to examine, in randomized-controlled fashion, the efficacy of a manualized multi-component treatment which included individual child-focused exposure-based CBT plus a concurrent family intervention designed to facilitate family disengagement from the affected child’s OCD symptoms (FCBT) and a comparison individual treatment comprised of psychoeducation about OCD and systematic relaxation training (PRT). PRT included several active elements common to quality CBT in order to enhance its credibility and provide a more stringent test of FCBT. In spite of earlier negative trials,13,14 more recent studies have found exposure-based CBT superior to psychosocial comparison treatment for youth with nonOCD anxiety. 21,22 Based on these studies, as well as prior adult OCD research,23 we hypothesized that FCBT would prove superior to PRT in reducing OCD severity, associated impairment, and family accommodation of OCD symptoms. In addition, and in order to provide more information regarding the potential mechanisms underlying FCBT, we also examined the temporal relationship between changes in family accommodation and changes in OCD symptom severity and impairment.
Method
Design
Seventy one children and adolescents were randomly assigned to 12 sessions over 14 weeks of FCBT or PRT. An unbalanced randomization scheme (70:30) was employed to minimize the number of subjects receiving comparison treatment and to facilitate planned within-group secondary analyses examining therapeutic process in FCBT. The unbalanced randomization was taken into account in study power calculations. In total, 49 participants were randomized to FCBT and 22 to PRT. The trial was approved by the University Institutional Review Board and registered on clinical trials.gov (NCT00000386). Prior to study enrollment, informed consent was provided by a parent or guardian and children provided assent.
Participants
Participants aged 8–17 were recruited from a pediatric OCD specialty clinic at a major university medical center. Inclusion criteria included: 1) primary DSM-IV diagnosis of OCD,24 2) CYBOCS total score > 15, 3) IQ>70, and 4) free of any psychotropic medication for OCD at study entry. Participants were excluded if they met criteria for any psychiatric illness that contraindicated study participation including suicidality, psychosis, pervasive developmental disorder, mania, or substance dependence.
Procedure
Interested families completed a telephone screening to ascertain potential eligibility. Qualifying families were then invited to the Clinic to complete informed consent/assent and a baseline eligibility evaluation. Outreach efforts, including flyers, print ads, and mailings, were specifically targeted towards media outlets and providers serving predominantly minority populations in order to enhance the representativeness of the study sample. Diagnostic eligibility was determined by the Anxiety Disorders Interview Schedule, fourth edition (ADIS-IV),25 administered along with the Children’s Yale-Brown Obsessive Compulsive Scale26 and a battery of standardized self-report measures assessing functional impairment, family dynamics, and comorbid symptomatology.
After completion of the baseline assessment and final determination of eligibility, participants were randomly assigned to either active (FCBT) or comparison (PRT) treatment. To minimize a potential treatment by therapist confound, therapist assignment was balanced over time so that each therapist treated participants in both treatment conditions. Trained evaluators blind to treatment condition conducted assessments with families at baseline, treatment weeks 4 and 8, and post-treatment (week 14). Positive responders to either intervention completed follow-up assessments at one- and six-months post-treatment to examine the durability of observed treatment gains.
Treatment Conditions
Child CBT plus Family Intervention (FCBT)
The FCBT protocol consisted of 12 sessions, 90 minutes each, delivered over 14 weeks ad according to a detailed treatment manual since published.27,28 The first 10 sessions were delivered weekly with two-week intervals between the last two sessions in order to foster generalization and smooth termination from treatment. The initial two sessions involved both the patient and parents and focused on educating the family about OCD; presenting the treatment rationale; creating a symptom hierarchy; and implementing a behavioral reward system for treatment participation. Thereafter, the first hour of each session centered on individual ERP while the last 30 minutes were devoted to the family sessions focusing on psychoeducation designed to correct misattributions about childhood OCD, reducing feelings of blame and guilt, and promoting increased treatment compliance and awareness. Emphasis was placed on helping parents to disengage from their child’s OCD behaviors, promoting developmentally appropriate patterns of family interaction, and addressing relapse prevention and maintenance of therapeutic gains. Although both parents (or primary caregivers) were strongly encouraged to attend all sessions, in order to enhance sample generalizability this was not an explicit requirement of participation. However, at least one parent attended each FCBT session. To enhance the developmental sensitivity of FCBT, the treatment manual presented techniques in preferred order of administration but provided alternate wordings and examples for different ages. The developmentally appropriate use of language and examples was a key focus of ongoing therapist supervision.
Psychoeducation/Relaxation Training (PRT)
Participants in PRT received training in progressive muscle relaxation29 administered according to the same schedule as FCBT. PRT was selected as the comparison treatment because of its credibility as an anxiety treatment13 and acceptability to participants in a prior adult OCD trial.23
To further enhance the acceptability and credibility of PRT, the first two sessions were similar to those for FCBT and attended by both the child and parents. These sessions focused on information gathering, psychoeducation about OCD, presenting a treatment rationale, creating an OCD symptom hierarchy, and developing a behavior reward system targeting compliance with weekly assigned practice of the relaxation exercises learned in session. The remaining ten sessions consisted of both muscular and verbally-cued relaxation techniques plus fifteen minutes with parents at session end to review the child’s current status and the weekly homework assignments. Importantly, any instruction to parents about how to manage or deal with their child’s OCD symptoms, including exposure, or the impact of these symptoms on family functioning was prohibited. The final session also contained a “feedback” component with the child and parents to review treatment gains and strategies for maintenance of gains.
At the end of the first treatment session, parents and children separately rated their confidence that their assigned treatment would be helpful using a 7-point scale (1=not at all confident to 7=extremely confident). There were no significant differences in expectancy across the two treatment for either parents (FCBT (N=48): M=5.4, SD=1.1; PRT (N=22): M=5.0, SD=1.7; p=.24) or children (FCBT (N=48): M=5.0, SD=1.4; PRT (N=22): M=4.5, SD=1.6, p=.24).
Therapist Training, Supervision and Fidelity
Treatment was provided by doctoral-level psychologists and advanced clinical child psychology interns with specialty training in CBT for pediatric OCD. Training began with a systematic review of study treatment manuals to ensure understanding and competent delivery of all treatment procedures. Therapists were then required to treat at least one non-study patient under live or videotape observation before being allowed to treat study patients.
Throughout the study, therapists participated in weekly group supervision and case review. All therapy sessions were videotaped, and approximately 10% of FCBT session (n=53) videotapes, distributed evenly across the twelve treatment sessions, were randomly selected for adherence/quality review by experienced CBT therapists. Sessions were rated for adherence to the treatment manual (range = 0–100) and overall quality (range=0–10) using detailed forms developed for the study. These ratings indicated good therapist adherence (M=88.2, SD=7.9) and treatment quality (M=8.1, SD=1.1).
Measures
Anxiety Disorders Interview Schedule: Child and Parent Versions (ADIS:C/P)25
is a semi-structured psychiatric diagnostic interview administered separately to parent and child. A clinical severity rating (CSR) of 4 or higher on a 0–8 scale is indicative of clinically significant disorder and was required for an OCD diagnosis. The ADIS has demonstrated sound psychometric properties.30,31 Interviewers presented child and parent-reported symptom level data, but not DSM-IV diagnoses, for 37% of the sample (N=26) to a best-estimate panel led by licensed clinicians experienced in the evaluation of childhood OCD. 31 Although not a formal assessment of inter-rater reliability, interviewer diagnoses of OCD were confirmed by the panel in 25 of 26 cases (96%).
Children’s Yale-Brown Obsessive Compulsive Scale
(CYBOCS)26 is a 10-item clinician completed scale (range 0–40) assessing severity of illness over the previous week. Psychometric properties are well-documented and the CYBOCS is considered the gold standard measure for pediatric OCD research.32,33
Clinical Global Impression Improvement Scale34
The Clinical Global Impression-Improvement Scale (CGI-I) provides a global rating of clinical improvement from baseline with scores ranging from 1 (very much improved) to 7 (very much worse). IEs provided CGI-I ratings at each post-baseline evaluation. Participants receiving a CGI-I rating of 1 (very much improved) or 2 (much improved) by the IE at the end of treatment (Wk 14) were considered treatment responders.
Child Obsessive Compulsive Impact Scale-Revised
(COIS-R)35 assesses OCD-specific functional impairment across multiple domains of youth functioning. Both the parent and child forms require respondents to answer 33 items using a 0 (not at all) to 3 (very much) Likert-scale. Both child and parent forms demonstrate adequate psychometric properties including internal consistency, concurrent validity, and test-retest reliability.35
Family Accommodation Scale-Parent Report
(FAS-PR) The original FAS is a psychometrically-sound 13-item clinician-rated measure that assesses the degree to which relatives of persons with OCD have accommodated patient rituals over the preceding month.36 Following the strategy used by others,15,17,37 the present study employed a parent self-report format that was identical in scoring and content to the original FAS with items rated on a 5-point (0–4) Likert scale. The FAS-PR was reliable in the present sample (α=.88).
Interviewer Training, Supervision and Reliability
Interviewers were doctoral-level clinical psychologists or graduate students with prior training or experience in the assessment of childhood anxiety. Training involved attending a presentation on the administration of the ADIS, CYBOCS, and CGI-I, observing and coding a videotaped interview, co-rating multiple live interviews conducted by a trained diagnostician, and, following satisfactory completion of the earlier steps, conducting at least one evaluation while under the supervision of a trained diagnostician. Interviewers received ongoing group supervision over the course of the study. Independent rating of 37% of randomly-selected CYBOCS audiotapes indicated excellent inter-rater reliability for this measure at baseline (N=26; ICC=.96) and post-treatment (N=23; ICC=.99).
Statistical Analyses
Sample size determination was based on expected intent-to-treat response rates on the primary outcome measure (CGI-I), of 60% for FCBT and 25% for PRT, 70:30 randomization to active and comparison treatment respectively, and a p<.05 significance level. Based on these assumptions, a total sample size of 72 (FCBT, n=50; PRT, n=22) was determined to provide 82% power to detect at least a 35% between group difference in treatment response rate.38
Simple between-group tests were conducted with chi-square and t-tests. A last observation carried forward approach was used to address missing dichotomous data. For measures with four time-points of data (i.e., pre-, week-4, week-8, and post-treatment), data were primarily examined using hierarchical linear modeling (HLM), due to the ability of HLM to model change over time using more than two data points, to include incomplete longitudinal cases (e.g., cases with only three out of four repeated measures), and to include random effects in the model. When significant between-groups differences were found, secondary post-hoc ANCOVAs for post-treatment scores (controlling for baseline) were conducted and effect sizes (ES) were computed comparing post-treatment means (MRT-MERP/SDpooled).38
Results
Sample Characteristics
Seventy-six youngsters completed the initial assessment and 71 were deemed eligible and randomized to FCBT or PRT (Figure 1). The two groups did not differ on any demographic or clinical variables at baseline. Mean age of participants was 12.2 (SD=2.5), 36.6% were male, and 77.5% were Caucasian. Approximately 25% of the sample had a prior history of psychotropic medication use and six (8.5%) were receiving stable non-OCD medications at study entry (Table 1).
Fig 1.
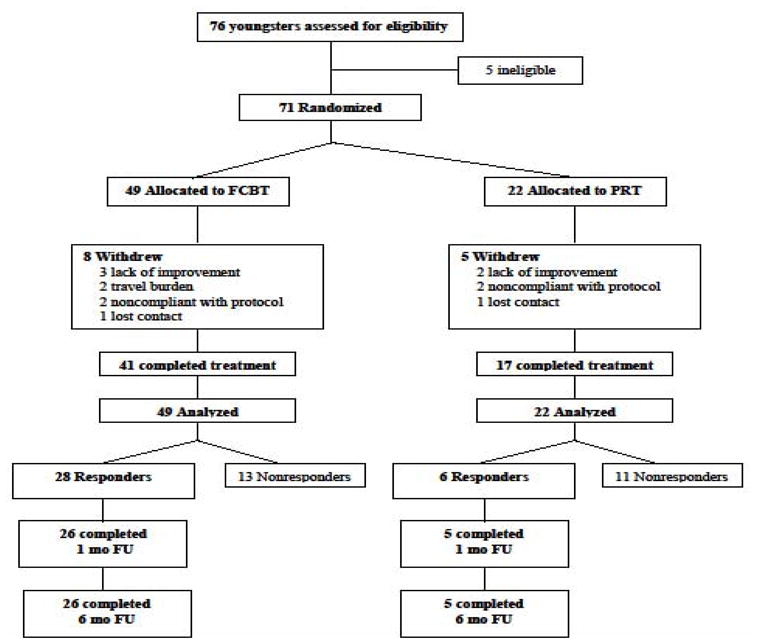
Study enrollment and retention. Note: FCBT= Individual Child plus Family Cognitive Behavior Therapy, FU=Follow-up; PRT= Psychoeducation plus Relaxation Training,
Table 1.
Baseline sample demographics and clinical characteristics.
| Total (N=71) | FCBT (N=49) | PRT (N=22) | |
|---|---|---|---|
| Mean Age (SD) | 12.2 (2.5) | 12.4 (2.6) | 11.6 (2.0) |
| Gender (%) | |||
| Male | 36.6 | 40.8 | 27.3 |
| Female | 63.4 | 59.2 | 72.7 |
| Ethnicity (%) | |||
| White | 77.5 | 77.6 | 77.3 |
| Latino | 9.9 | 10.2 | 9.1 |
| Asian | 4.2 | 4.1 | 4.5 |
| African American | 2.8 | 2.0 | 4.5 |
| Other/Mixed | 5.6 | 6.1 | 4.5 |
| Current Living Situation (%) | |||
| Both Biological Parents | 73.2 | 67.3 | 86.4 |
| Single Parent | 18.3 | 22.4 | 9.1 |
| Other | 8.5 | 10.2 | 4.5 |
| Prior Medication History (%) | |||
| Any Psychiatric | 25.4 | 22.4 | 31.8 |
| SSRI/SRI | 21.1 | 20.4 | 22.7 |
| Stimulant | 7.0 | 6.1 | 9.1 |
| Other | 3.7 | 4.1 | 9.1 |
| On Current Medication (%)a | 8.5 | 9.1 | 8.5 |
| Obsessions (%) | |||
| Contamination | 71.8 | 65.3 | 86.4 |
| Aggressive | 78.9 | 75.5 | 86.4 |
| Sexual | 18.3 | 16.3 | 22.7 |
| Hoarding | 33.8 | 34.7 | 31.8 |
| Superstitious | 28.2 | 30.6 | 22.7 |
| Somatic | 49.3 | 40.8 | 68.2 |
| Religious | 50.7 | 46.9 | 59.1 |
| Miscellaneous | 73.2 | 71.4 | 77.3 |
| Compulsions(%) | |||
| Cleaning | 67.6 | 63.3 | 77.3 |
| Checking | 63.4 | 61.2 | 68.2 |
| Repeating | 69.0 | 75.5 | 54.6 |
| Counting | 30.7 | 26.5 | 40.1 |
| Ordering | 70.4 | 69.4 | 72.7 |
| Hoarding | 38.0 | 34.7 | 45.5 |
| Superstitious | 28.1 | 26.5 | 31.8 |
| Involving Others | 69.0 | 67.4 | 72.7 |
| Miscellaneous | 94.4 | 93.9 | 95.5 |
Note: Contamination and Somatic Obsessions were significantly more common in Psychoeducation plus Relaxation Training (PRT) vs Individual Child plus Family Cognitive Behavior Therapy (FCBT) (p<.05). SSRI/SRI = Selective Serotonin Reuptake Inhibitor/Serotonin Reuptake Inhibitor
Current Medication: FCBT: methylphenidate = 3, trazodone (reportedly for sleep) = 1; PRT: Adderall = 1, clonodine (reportedly for tics) = 1.
Two-thirds (66.2%) of the sample met criteria for another DSM-IV diagnosis at entry with almost 30% meeting criteria for two or more additional disorders (Table 2). Collectively, non-OCD anxiety disorders were most common (46.5%) with generalized anxiety disorder the most common single co-occurring diagnosis (33.8%). Although a primary (e.g., most impairing) diagnosis of OCD was a requirement of study entry, subsequent inspection revealed the inadvertent inclusion of one child with a diagnosis of intermittent explosive disorder (IED) rated as marginally more impairing than OCD. Given this near equivalence in severity and the fact that the child was otherwise eligible for the study, these data were retained for subsequent analyses.
Table 2.
Diagnostic Status at Baseline
| Total(N=71) | FCBT (N=49) | PRT(N=22) | ||||
|---|---|---|---|---|---|---|
| N | (%) | N | (%) | N | (%) | |
| Tic Disorder | 8 | (11.3) | 6 | (12.2) | 2 | (9.1) |
| Tourette’s Disorder | 3 | (4.2) | 3 | (6.1) | 0 | (0.0) |
| Chronic Motor Tic Disorder | 3 | (4.2) | 2 | (4.1) | 1 | (4.5) |
| Transient Tic Disorder | 2 | (2.8) | 1 | (2.0) | 1 | (4.5) |
| Anxiety Disorder | 33 | (46.5) | 26 | (53.1) | 7 | (31.8) |
| Generalized Anxiety | 24 | (33.8) | 18 | (36.7) | 6 | (27.3) |
| Social Anxiety | 9 | (13.9) | 5 | (10.2) | 4 | 18.2) |
| Separation Anxiety | 7 | (9.9) | 5 | (10.2) | 2 | (9.1) |
| Specific Phobia | 5 | (7.0) | 2 | (4.1) | 3 | (13.6) |
| Panic | 1 | (1.4) | 1 | (2.0) | 0 | (0.0) |
| ADHD | 9 | (13.9) | 7 | (14.3) | 2 | (9.1) |
| Combined type | 6 | (8.5) | 5 | (10.2) | 1 | (4.5) |
| Inattentive type | 3 | (4.2) | 2 | (4.1) | 1 | (4.5) |
| Oppositional Defiant Disorder | 3 | (4.2) | 2 | (4.1) | 1 | (4.5) |
| Mood Disorder | 3 | (4.2) | 3 | (6.1) | 0 | (0.0) |
| Dysthymia | 2 | (2.8) | 2 | (4.1) | 0 | (0.0) |
| Major Depressive Episode | 1 | (1.4) | 1 | (2.0) | 0 | (0.0) |
| Other | 2 | (2.8) | 0 | (0.0) | 2 | (9.1) |
| Number of Co-occurring Diagnoses | ||||||
| None | 24 | (33.8) | 15 | (30.6) | 9 | (40.9) |
| One | 26 | (36.6) | 20 | (40.8) | 6 | (27.3) |
| Two | 15 | (21.1) | 11 | (22.4) | 4 | (18.2) |
| Three | 6 | (8.4) | 3 | (6.1) | 3 | (13.6) |
Note: ADHD = attention-deficit/hyperactivity disorder; FCBT = Individual Child plus Family Cognitive Behavior Therapy; PRT = Psychoeducation plus Relaxation Training.
Responder Status
Intent-to-treat analyses with the CGI-I revealed a significantly higher response rate at Week 14 for FCBT as compared to PRT (57.1% vs. 27.3%; η2=5.40, p<.05). Analysis of treatment completers yielded similar results (68.3% vs. 35.3%, η2=5.40, p<.05).
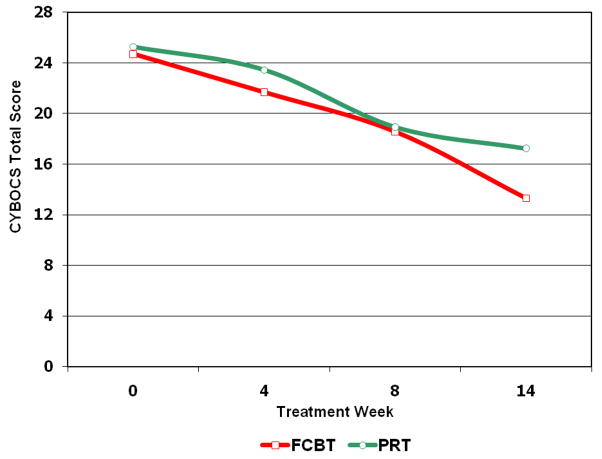
OCD Severity
The HLM analysis comparing the rate of change in CYBOCS total scores in FCBT and PRT yielded a statistically significant slope by treatment interaction, t = 2.25, p<.05. The means in Table 3 (and Figure 2) show that the nature of this interaction effect was a faster decline in CYBOCS scores over time in FCBT as compared to PRT. FCBT led to a 46.2% reduction in CYBOCS total score as compared to a 32.0% reduction for PRT. In contrast, the ANCOVA comparing post-treatment CYBOCS scores did not reach significance (F [1, 69] = 2.67, p<.14). The between-groups ITT ES at post-treatment was .40.
Table 3.
N, Means, 95% Confidence Intervals, and within-group effect sizes (d) for study outcome measures by treatment condition and week.
| FCBT | PRT | |||||
|---|---|---|---|---|---|---|
| Measure | N | M | (95%CI) | N | M | (95% CI) |
| CYBOCS | ||||||
| Week 0 | 49 | 24.7 | [23.4–26.1] | 22 | 25.3 | [23.4–27.2] |
| Week 4 | 48 | 21.7 | [20.2–23.2] | 20 | 23.5 | 21.2–25.8] |
| Week 8 | 43 | 18.6 | [16.5–20.7] | 17 | 18.9 | [15.2–22.6] |
| Week 14 | 40 | 13.3 | [10.7–15.9] | 17 | 17.2 | [13.0–21.4] |
| d = 2.37 | d = 1.80 | |||||
| COIS-RC | ||||||
| Week 0 | 48 | 15.4 | [12.8–18.8] | 22 | 14.9 | [9.2–20.6] |
| Week 4 | 48 | 10.9 | [8.4–13.4] | 20 | 11.6 | [6.5–16.7] |
| Week 8 | 42 | 9.2 | [6.3–12.1] | 16 | 15.5 | [9.1–21.9] |
| Week 14 | 39 | 5.6 | [3.3–8.0] | 16 | 14.3 | [8.0–20.6] |
| d = 0.81 | d = 0.05 | |||||
| COIS-RP | ||||||
| Week 0 | 47 | 22.4 | [19.0–25.8] | 22 | 21.4 | [13.8–29.0] |
| Week 4 | 48 | 21.2 | [17.2–25.2] | 21 | 20.5 | [13.8–27.2] |
| Week 8 | 43 | 17.4 | [13.0–21.8] | 17 | 16.2 | [10.4–22.0] |
| Week 14 | 39 | 10.6 | [7.1–14.1] | 17 | 11.2 | [7.3–15.1] |
| d = 1.01 | d = 0.57 | |||||
| FAS-PR | ||||||
| Week 0 | 48 | 17.5 | [14.5–20.5] | 22 | 18.0 | [13.7–22.3] |
| Week 14 | 39 | 9.3 | [6.4–12.2] | 17 | 15.2 | [10.5–19.9] |
| d = 0.78 | d = 0.27 | |||||
Note: COIS-R = Child Obsessive Compulsive Impact Scale-Revised Parent-Report; COIS-RC = Child Obsessive Compulsive Impact Scale-Revised Child-Report; CYBOCS = Children’s Yale-Brown Obsessive Compulsive Scale; FAS-PR = Family Accommodation Scale-Parent Report; FCBT = Individual Child plus Family Cognitive Behavior Therapy; PRT = Psychoeducation plus Relaxation Training.
Figure 2.
Change in Children’s Yale-Brown Obsessive Compulsive Scale (CYBOCS) Total Score by Treatment Condition over Time. Note: FCBT = Individual Child plus Family Cognitive Behavior Therapy; PRT = Psychoeducation plus Relaxation Training.
To examine clinically significant improvement, Wk 14 CYBOCS scores for treatment completers were categorized into an ordinal scale: 1 (remitted [<11]), 2 (subclinical [11–15]), 3 (moderate [16–24]), and 4 (severe [>24]) (Table 4). An ordinal regression analysis testing the difference between the treatment groups on these severity categories post-treatment indicated that a higher proportion of children in FCBT fell into the less severe CYBOCS categories than children in PRT (η2=3.81, p=.05). Rates of clinical remission, defined as CYBOCS total score<11,7 were 42.5% for FCBT versus 17.6% for PRT (η2=3.24, ns).
Table 4.
Response Status as determined by Week 14 Children’s Yale-Brown Obsessive Compulsive Scale (CYBOCS) Total Score.
| CYBOCS | FCBT | PRT | ||
|---|---|---|---|---|
| Total Score | N | (%) | N | (%) |
| 0 – 10 (Remitted) | 17 | (42.5) | 3 | (17.6) |
| 11 – 15 (Subclinical) | 10 | (25.0) | 5 | (29.4) |
| 16 – 24 (Moderately Ill) | 10 | (25.0) | 5 | (29.4) |
| 24 – 40 (Severely Ill) | 3 | (7.5) | 4 | (23.5) |
Note: FCBT = Individual Child plus Family Cognitive Behavior Therapy; PRT = Psychoeducation plus Relaxation Training;
Functional Status
Parallel HLM analyses for the COIS-RC also revealed a significant slope by treatment group interaction effect, t=2.14, p<.05 whereby the means for the FCBT group declined significantly from baseline to post-treatment on the COIS-RC in contrast to the PRT group where there was little lasting change. The post-treatment ITT ES was .48. The post-treatment ANCOVA for the COIS-RC did not reach significance, (F [1, 68] = 2.55, p < .12). Complementary HLM analyses revealed that while both groups improved over time on COIS-RP scores (t=−2.66, p<.01), there was no group by time interaction effect (t=.09, ns).
The COIS-RC does not have established clinical cut-points; therefore, to evaluate the clinical significance of observed changes, treatment completers were grouped according to whether they had no COIS items scored above 1 at post-treatment (i.e., no more than minimal OC-related impairment in any functional) or whether they had any COIS items scored above 1 (reflecting more than minimal impairment). In FCBT, 24 (66.7%) of children reported minimal impairment on the COIS-RC, while 12 (33.3%) reported more than minimal impairment. In contrast, only a minority of children who received PRT (n=5 [31.3%]) reported minimal impairment on the COIS-RC, while 11 (68.8%) reported more than minimal impairment (η2 = 5.63, p<.05).
Family Accommodation
HLM analysis of FAS-PR total scores yielded a marginally significant slope by treatment group interaction effect, t=1.95, p=.05. The means for the FCBT group declined from baseline to post-treatment on the FAS-PR, but there was less improvement for the PRT group (post-treatment ITT ES=.42) (Table 3).
Family Accommodation as Predictor of Response
Given preliminary prior evidence for the role of family accommodation as a potential predictor of outcome,19 lagged time-varying covariate analyses were undertaken in HLM to determine if reductions in FAS scores at a given time-point were associated with corresponding reductions in CYBOCS or COIS-R scores at the following time point. Group (within-person) centering was employed. FAS-PR scores (at time t, beginning with baseline) were the only predictors at level 1. Level 2 predictors were added after testing the basic level 1 model across groups, in which interactions with treatment group were specified at level 2. CYBOCS or COIS-RC or COIS-RP scores (at time t+1, beginning with week 4) were the DVs in three separate models. For the CYBOCS level 1 model, there was an association between the slope of the FAS and the CYBOCS total score, such that for each 1-point reduction in FAS scores compared to an individual’s overall mean score across time points at a particular assessment (e.g., week 4), their CYBOCS score also declined an average of .27 points compared to their overall mean score across time points at the following assessment (e.g., week 8) (t=2.68, p<.01). There was no treatment group by slope interaction effect for the CYBOCS model. However, for the COIS-RC model, a treatment group by slope interaction effect did emerge (t=−2.75, p<.01). For the FCBT group, a 1-point reduction in FAS-PR scores (relative to one’s own mean across time) at a particular assessment corresponded with a 1.2-point reduction in COIS-RC scores at the following assessment. This effect was reduced by more than 50%, to a 0.48-point corresponding reduction in COIS-RC scores in the PRT group. There was no significant effect found in the COIS-RP model.
Durability of Treatment Response
Twenty-six of 28 initial FCBT responders (93%) completed follow-up assessments with 81% (21/26) maintaining their positive response status (CGI-I<3) at one-month and 73% (19/26) at six-months post-treatment. Mean CYBOCS total scores for these 26 subjects were: post-treatment: M=9.7 (95%CI=6.0–12.0); one-month FU: M=4.1 (95%CI=2.8–5.3); six-month FU: M=3.2 (95%CI=1.8–4.5). Of the six PRT responders, 5 (83%) completed the one- and six-month follow-up assessments although CGI-I data was missing for one subject at six-months. Overall, 60% (3/5) maintained their positive response at one-month and 75% (3/4) at six-months. Mean CYBOCS total scores for these subjects were: post-treatment: M=9.8 (95%CI=5.3–14.3); one-month FU: M=4.2 (95%CI=1.1–7.3); six-month FU: M=3.4 (95%CI=−0.6–7.4).
Discussion
This study tested the efficacy of a family-focused CBT protocol (FCBT) for pediatric OCD in comparison to a credible psychosocial comparison treatment involving OCD psychoeducation and systematic relaxation training (PRT). As expected, primary analyses found that youth receiving FCBT demonstrated larger overall response rates and more rapid reduction of OCD symptom severity and child-reported functional impairment than those receiving PRT. Moreover, FCBT was associated with more rapid decreases in family accommodation than PRT. These findings were confirmed in some, but not all, secondary analyses. Changes in family accommodation temporally preceded reductions in CYBOCS symptom severity for both FCBT and PRT. However, reduced accommodation preceded improvement in child-reported OC-specific functional impairment only for FCBT. To our knowledge, this is the first controlled demonstration of the temporal ordering of changes in family accommodation and outcome in a pediatric sample. FCBT was associated with a two-fold greater rate of remission of OCD than PRT (43% versus 18%, respectively). In addition, acute responders in both conditions maintained their gains over the 6-month follow-up interval providing some evidence for the durability and clinical significance of initial treatment response. Controlled examination of response durability over longer follow-up periods is needed to better determine the long range and specific impact of successful CBT on course of disorder, impairment, and other outcomes.
At a broader level, findings from this study are consistent with the existing literature. In particular, the response and remission rates demonstrated for FCBT largely parallel those from other randomized controlled CBT trials4,7,20, and suggest that exposure-based CBT is an efficacious and potentially durable39 treatment for pediatric OCD in the majority of cases. Moreover, the use of an active comparator strategy designed to control for several critical elements of exposure-based treatment extends prior research and serves to increase confidence in study findings as well as the conceptual model model underlying this treatment approach.10
The magnitude of the between-group effect size (d=0.4) found for FCBT in this trial also needs to be evaluated in the context of the study comparison group. Although the within-group ES for FCBT (2.4) was comparable to those from other controlled pediatric OCD trials, e.g., 2.6,7 2.2,20 and 3.6,12 the within-group ES found for PRT in this study (1.8) was far superior to those reported for comparison conditions used in other controlled studies, e.g., −0.20 for waitlist,12 1.0 for relaxation training,20 and 1.1 for pill placebo.7 Notably, PRT outperformed the POTS sertraline-only condition which yielded a within-treatment ES of only 1.3.7 While the pediatric OCD research community has been moving towards the use of more active comparison conditions,7,20 the present findings suggest cautious interpretation of the existing literature and speak to the importance of more methodologically-rigorous treatment designs going forward. Importantly, and in line with prior negative trials using active comparison treatments,13,14 the relatively large effect sizes for PRT may have contributed to the lack of significant post-treatment ANCOVA findings.
It is also encouraging to note that FCBT was associated with significant reductions in both parent and child-reported OC-specific functional impairment. However, PRT was also associated with a significant reduction in parent- but not child-reported impairment such that the treatment by time interaction was only significant for child-reported impairment. The reasons for this discrepancy are not immediately clear. The most parsimonious explanation is that children are simply more accurate reporters of their psychosocial functioning than parents. However, it is also possible that PRT may have facilitated an increased level of psychosocial functioning in children which was noted by parents, but not reported by the children themselves perhaps because these activities were still distressing to accomplish. Alternatively, differential treatment effects on functioning may require longer periods of observation by parents to detect than our 12 week acute phase allowed. There has been growing emphasis on the importance of addressing functional outcomes1,2 and, regardless of the mechanism underlying the functional changes observed in the present study, these findings speak to the value of FCBT in reducing OCD-related interference and enhancing global functioning.
The present findings also shed light on family processes that may influence treatment outcome for youth with OCD. Accommodation is well-documented among families of youth with OCD15,16,17 and is hypothesized to undermine the success of exposure-based CBT. Nonetheless, prior controlled efforts to change family dynamics have produced largely negative results. The present findings are encouraging in that they provide the first controlled evidence that weekly treatment with brief, individual child CBT in combination with a structured family intervention can reduce parent-reported involvement in OC symptoms and that this reduction in accommodation may precede improvement in both symptom severity and OCD-related functional impairment. However, the fact that the treatment group by slope interaction was only marginally significant (p=.05), does not allow us to conclude that the reductions in accommodation which preceded OCD symptom reduction are specific to the FCBT group only. Whether or not this is actually the case or the result of insufficient statistical power remains to be established.
Although FCBT was designed to reduce family accommodation in order to support the child’s ability to engage in exposure plus response prevention, it is also not possible at present to rule out the alternative hypothesis that reductions in OCD severity resulting from individual child treatment instead led to decreased family involvement independent of the family intervention or that the observed effects are reciprocal or bidirectional in nature, particularly in light of the fact that a group by time interaction effect on the time-varying covariate analyses were only significant for functional impairment, not for symptom severity. Although failure to demonstrate a specific temporal relationship between reduced accommodation and symptom severity for FCBT may have been due to inadequate statistical power, clarification of this conundrum requires additional study.
Even though prior FCBT studies for childhood OCD have produced encouraging results, the present findings have important implications for furthering the classification of FCBT as an evidence-based intervention.10 Both expert consensus and professional-group guidelines have recommended some degree of family involvement in child OCD treatment;40,41 however, empirical support for these recommendations remains limited.4 Our use of an adequately-powered randomized design, systematic standardized assessment, and a credible comparison group qualify this study for Type 1 methodological classification11 and provide the necessary evidence to elevate FCBT from a “possibly efficacious” to a “probably efficacious” treatment for childhood OCD.4,10 While this may seem to be little more than an incremental advance, the determination of FCBT as a “probably efficacious” treatment is particularly important in a field where scientifically untested interventions are common and clinical outcomes often leave much to be desired. However, we also note that, similar to the POTS Study,7 over 40% of subjects receiving FCBT failed to achieve responder status, highlighting the variable response pediatric OCD treatment and the need for additional treatment development and refinement for non-responders to initial intervention.
In spite of the methodological strengths noted earlier along with careful quality adherence procedures, therapist assignment balanced across conditions, and a largely medication-free and relatively ethnically heterogeneous sample, a number of study limitations must also be noted. First, the study design did not allow for a controlled evaluation of treatment durability as ethical concerns led us to remove non-responders from the study in order to provide them with clinical treatment. Second, the lack of parent and child treatment credibility ratings does not exclude the possibility that between-group treatment differences were influenced by informant bias towards FCBT. However, this concern is at least partially mitigated by the fact that parent and child ratings of expected benefits were reasonably high and did not significantly differ across the two conditions. In addition, since the same therapists provided both treatments, it is also possible that, in spite of efforts to prevent this, active elements of FCBT may have inadvertently bled into the PRT protocol and led to some proportion of the positive effects associated with the comparison treatment. The lack of therapist adherence ratings for PRT does not allow us to examine this concern directly. However, the potential therapist-by-treatment confound resulting from restricting therapists to one condition only is arguably a far greater, and less controllable, threat to the internal validity of the study than potential bleed. Third, while enhancing the representativeness of the sample to more typical treatment settings, our decision to not explicitly require both parents to attend each FCBT session likely resulted in a less than ideal dose of the family intervention in some cases. Decisions such as these speak to the difficulty in balancing internal and external validity needs. Finally, while the study was powered to address primary aims, the study sample size, especially in light of the relative potency of PRT, limited the statistical power available for some secondary study analyses, did not allow us to examine predictors in a more comprehensive manner or allow definitive conclusions to be drawn from all of the predictor analyses that were conducted.
It is also important to note that the current study design does not allow us to estimate the incremental benefit of FCBT over more traditional individual child CBT; such trials have yet to be published for pediatric OCD. Head-to-head comparative trials for non-OCD pediatric anxiety disorders have yielded a range of outcomes,21,42,43 although FCBT has evidenced some superiority over individual treatment in certain subgroups, such as younger or female participants42 or when both parents had an anxiety disorder.21 In similar fashion, FCBT for pediatric OCD may ultimately prove most effective when tailored to address the specific needs of clinical subgroups characterized by family-related44 or other relevant factors. These issues will need to be addressed in order to develop the next generation of optimized and personalized interventions for youth with OCD and their families.45 Future work will also be needed to foster the translation of family CBT and similar treatments for pediatric OCD for use in community-based settings,46 to examine dosage and intensity effects of treatment, and to assess effectiveness in broader populations.
Acknowledgments
The authors wish to acknowledge Tami Roblek, PhD, University of Colorado at Denver and Health Sciences Center, and all of the therapists, interviewers, research coordinators, and consultants who were part of this study. Special gratitude is also extended to the children and families who participated in this research.
This study was funded by National Institute of Mental Health grant R01MH58549-01 (JP).
Footnotes
Disclosures: Dr. Piacentini has received grant support from the National Institute of Mental Health (NIMH), the Tourette Syndrome Association (TSA), and the Obsessive Compulsive Foundation. He has received royalties from Oxford University Press, including the manuals described in this paper, Guilford Press, and the American Psychological Association. He has served on the speakers’ bureau for the TSA. He has served as a consultant to Bayer Schering Pharma. Dr. Bergman has received research support from the National Alliance for Research on Schizophrenia and Depression (NARSAD). Dr. Chang has received grant support from NIMH and the TSA. He has served on the speakers’ bureau for the TSA. He has received royalties from Oxford University Press. Dr. Langley has received research support from NIMH and the Substance Abuse and Mental Health Services Administration. She has received royalties from Oxford University Press for the manuals described in this paper. Dr. Peris has received research support from NIMH and NARSAD. Dr. Wood has received grant support from NIMH, the Organization for Autism Research, and Autism Speaks. He has received royalties from WW Norton and Company. Dr. McCracken has received research support from NIMH, Bristol-Myers Squibb, Aspect, and Seaside Pharmaceuticals. He has served as a consultant to Novopharm and BioMarin. He has served on the speakers’ bureau for the TSA, Veritas, and CME Outfitters.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Piacentini J, Bergman RL, Keller M, McCracken J. Functional impairment in children and adolescents with Obsessive Compulsive Disorder. J Child Adol Psychopharmacology. 2003;13:61–70. doi: 10.1089/104454603322126359. [DOI] [PubMed] [Google Scholar]
- 2.Storch EA, Larson MJ, Muroff J, et al. Predictors of functional impairment in pediatric obsessive-compulsive disorder. J Anxiety Disord. 2010;24:275–283. doi: 10.1016/j.janxdis.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 3.Moore PS, Mariaski A, March J, et al. Obsessive-compulsive disorder in children and adolescents: Diagnosis, comorbidity, and developmental factors. Handbook of child and adolescent obsessive-compulsive disorder. 2007:17–45. [Google Scholar]
- 4.Barrett P, Farrell L, Pina A, Peris TS, Piacentini J. Evidence-based treatments for child and adolescent OCD. J Clin Child Adolesc Psychol. 2008;37:131–155. doi: 10.1080/15374410701817956. [DOI] [PubMed] [Google Scholar]
- 5.Geller D, Biederman J, Stewart S, et al. Which SSRI? A meta-analysis of pharmacotherapy trials for pediatric obsessive compulsive disorder. Am J Psychiatry. 2003;160:1919–1928. doi: 10.1176/appi.ajp.160.11.1919. [DOI] [PubMed] [Google Scholar]
- 6.O’Kearney RT, Anstey K, von Sanden C, Hunt A. Behavioural and cognitive behavioural therapy for obsessive compulsive disorder in children and adolescents. Cochrane Database of Systematic Reviews. 2006;(4):Art. No.:CD004856. doi: 10.1002/14651858.CD004856.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pediatric OCD Treatment Study Team. Cognitive-behavior therapy, sertraline, and their combination for children and adolescents with obsessive-compulsive disorder. JAMA. 2004;292:1969–1976. doi: 10.1001/jama.292.16.1969. [DOI] [PubMed] [Google Scholar]
- 8.Watson HJ, Rees CS. Meta-analysis of randomized, controlled treatment trials for pediatric obsessive-compulsive disorder. J Child Psychol Psychiatry. 2008;49:489–498. doi: 10.1111/j.1469-7610.2007.01875.x. [DOI] [PubMed] [Google Scholar]
- 9.Brown R, Antonuccio D, DuPaul G, et al. Childhood Mental Health Disorders: Evidence Base and Contextual Factors for Psychosocial, Psychopharmacological, and Combined Interventions. Washington DC: American Psychological Assoc Press; 2008. [Google Scholar]
- 10.Chambless DL, Hollon SD. Defining empirically supported therapies. J Consult Clin Psychology. 1998;66:7–18. doi: 10.1037//0022-006x.66.1.7. [DOI] [PubMed] [Google Scholar]
- 11.Nathan PE, Gorman JM. A guide to treatments that work. 2. New York: Oxford University Press; 2002. [Google Scholar]
- 12.Barrett PM, Healy-Farrell LJ, March JS. Cognitive-behavioral family treatment of childhood obsessive-compulsive disorder: A controlled trial. J Am Acad Child Adol Psych. 2004;43:46–62. doi: 10.1097/00004583-200401000-00014. [DOI] [PubMed] [Google Scholar]
- 13.Silverman W, Kurtines W, Ginsburg G, Weems C, Rabian B, Serafini L. Contingency management, self-control, and education support in the treatment of childhood phobic disorders: A randomized clinical trial. J Consult Clin Psychology. 1999;67:675–687. doi: 10.1037//0022-006x.67.5.675. [DOI] [PubMed] [Google Scholar]
- 14.Last C, Hansen C, Franco N. Cognitive-behavioral treatment of school phobia. J Am Acad Child Adol Psychiatry. 1998;37:404–411. doi: 10.1097/00004583-199804000-00018. [DOI] [PubMed] [Google Scholar]
- 15.Peris TS, Bergman RL, Langley A, Chang S, McCracken JT, Piacentini J. Correlates of family accommodation of childhood obsessive-compulsive disorder: Parent, child, and family characteristics. J Am Acad Child Adol Psychiatry. 2008;47:1173–1181. doi: 10.1097/CHI.0b013e3181825a91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Renshaw KD, Steketee G, Chambless DL. Involving family members in the treatment of OCD. Cogn Behav Ther. 2005;34:164–175. doi: 10.1080/16506070510043732. [DOI] [PubMed] [Google Scholar]
- 17.Storch EA, Geffken GR, Merlo LJ, et al. Family accommodation in pediatric obsessive-compulsive disorder. J Clin Child Adol Psychology. 2007;36:207–216. doi: 10.1080/15374410701277929. [DOI] [PubMed] [Google Scholar]
- 18.Merlo LJ, Lehmkuhl HD, Geffken GR, Storch EA. Decreased family accommodation associated with improved therapy outcome in pediatric obsessive-compulsive disorder. J Consult Clin Psychology. 2009;77:355–360. doi: 10.1037/a0012652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Freeman J, Garcia AM, Coyne L. Early childhood OCD: preliminary findings from a family-based cognitive behavioral approach. J Am Acad Child Adolesc Psychol. 2008;47:593–602. doi: 10.1097/CHI.0b013e31816765f9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Storch EA, Geffken GR, Merlo LJ, et al. Family-based cognitive-behavioral therapy for pediatric obsessive-compulsive disorder: Comparison of intensive and weekly approaches. J Am Acad Child Adolesc Psychiatry. 2007;46:469–478. doi: 10.1097/chi.0b013e31803062e7. [DOI] [PubMed] [Google Scholar]
- 21.Kendall P, Hudson J, Gosch E, Flannery-Schroeder E, Suveg C. Cognitive-behavioral therapy for anxiety disordered youth: A randomized clinical trial evaluating child and family modalities. J Consult Clin Psychology. 2008;76:282–297. doi: 10.1037/0022-006X.76.2.282. [DOI] [PubMed] [Google Scholar]
- 22.Ollendick T, Ost L-G, Reuterskiold L, et al. One-session treatment of specific phobias in youth: A randomized clinical trial in the United States and Sweden. J Consult Clin Psychology. 2009;77:504–516. doi: 10.1037/a0015158. [DOI] [PubMed] [Google Scholar]
- 23.Fals-Stewart W, Schafer J. The treatment of substance abusers with obsessive-compulsive disorder: An outcome study. J Subs Abuse Treatment. 1992;9:365–370. doi: 10.1016/0740-5472(92)90032-j. [DOI] [PubMed] [Google Scholar]
- 24.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington DC: American Psychiatric Association; 1994. [Google Scholar]
- 25.Silverman WK, Albano AM. Anxiety Disorders Interview Schedule for DSM-IV: Parent Version. San Antonio, TX: Graywing; 1996. [Google Scholar]
- 26.Scahill L, Riddle MA, McSwiggin-Hardin M, et al. Children’s Yale-Brown Obsessive Compulsive Scale: Reliability and validity. J Am Acad Child Adolesc Psychiatry. 1997;36:844–852. doi: 10.1097/00004583-199706000-00023. [DOI] [PubMed] [Google Scholar]
- 27.Piacentini J, Langley A, Roblek T. Cognitive-Behavioral Treatment of Childhood OCD: Therapist Guide. New York: Oxford University Press; 2007. [Google Scholar]
- 28.Piacentini J, Langley A, Roblek T. It’s Only a False Alarm: Child Workbook. New York: Oxford University Press; 2007. [Google Scholar]
- 29.Cautela J, Groden J. Relaxation: A Comprehensive Manual for Adults, Children, and Children with Special Needs. Champaign, IL: Research Press; 1978. [Google Scholar]
- 30.Silverman WK, Saavedra L, Pina A. Test-retest reliability of anxiety symptoms and diagnoses with anxiety disorders interview schedule for DSM-IV: Child and parent versions. J Am Acad Child Adolesc Psychiatry. 2001;40:937–944. doi: 10.1097/00004583-200108000-00016. [DOI] [PubMed] [Google Scholar]
- 31.Wood J, Piacentini J, Bergman RL, McCracken J, Barrios V. Concurrent validity of the anxiety disorders section of the Anxiety Disorders Interview Schedule for DSM-IV: Child and Parent Version. J Clin Child Psychol. 2002;31:335–342. doi: 10.1207/S15374424JCCP3103_05. [DOI] [PubMed] [Google Scholar]
- 32.Gallant J, Storch EA, Merlo LJ, et al. Convergent and discriminant validity of the Children’s Yale-Brown Obsessive Compulsive Scale-symptom checklist. J Anxiety Disord. 2008;22:1369–1376. doi: 10.1016/j.janxdis.2008.01.017. [DOI] [PubMed] [Google Scholar]
- 33.Lewin A, Piacentini J. Evidence-based assessment of child obsessive compulsive disorder: Recommendations for clinical practice and treatment research. Child and Youth Care Forum. 2010;39:73–89. doi: 10.1007/s10566-009-9092-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guy W, Bonato R, editors. CGI: Clinical Global Impressions. Chevy Chase, MD: National Institute of Mental Health; 1970. [Google Scholar]
- 35.Piacentini J, Peris TS, Bergman RL, Chang S, Jaffer M. The Child Obsessive-Compulsive Impact Scale-Revised (COIS-R): Development and psychometric properties. J Clin Child Adolesc Psychology. 2007;36:645–653. doi: 10.1080/15374410701662790. [DOI] [PubMed] [Google Scholar]
- 36.Calvocoressi L, Lewis B, Harris M, et al. Family accommodation in obsessive-compulsive disorder. Am J Psychiatry. 1995;152:441–443. doi: 10.1176/ajp.152.3.441. [DOI] [PubMed] [Google Scholar]
- 37.Stewart SE, Beresin C, Haddad S, Stack DE, Fama J, Jenike M. Predictors of family accommodation in obsessive-compulsive disorder. Ann Clin Psychiatry. 2008;20:65–70. doi: 10.1080/10401230802017043. [DOI] [PubMed] [Google Scholar]
- 38.Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- 39.O’Leary EMM, Barrett P, Fjermestad KW. Cognitive-behavioral family treatment for childhood obsessive-compulsive disorder: A 7-year follow-up study. J Anxiety Disord. 2009;23:973–978. doi: 10.1016/j.janxdis.2009.06.009. [DOI] [PubMed] [Google Scholar]
- 40.American Academy of Child and Adolescent Psychiatry: Practice parameters for the assessment and treatment of children and adolescents with obsessive-compulsive disorder. J Am Acad Child Adol Psych. 1998;37(suppl 10):27–45. doi: 10.1097/00004583-199810001-00003. [DOI] [PubMed] [Google Scholar]
- 41.March J, Frances A, Carpenter D, Kahn D. Expert consensus guidelines: Treatment of -obsessive–compulsive disorder. J Clin Psychiatry. 1997;58:1–72. [Google Scholar]
- 42.Barrett PM, Dadds MR, Rapee RM. Family treatment of childhood anxiety: A controlled trial. J Consult Clin Psychol. 1996;64:333–342. doi: 10.1037//0022-006x.64.2.333. [DOI] [PubMed] [Google Scholar]
- 43.Wood J, Piacentini J, Southam-Gerow M, Chu B, Sigman M. Family cognitive behavioral therapy for child anxiety disorders. J Am Acad Child Adol Psychiatry. 2006;45:314–321. doi: 10.1097/01.chi.0000196425.88341.b0. [DOI] [PubMed] [Google Scholar]
- 44.Peris T, Piacentini J. Preliminary results from a controlled feasibility trial of Positive Family Interaction Therapy (PFIT). Obsessive Compulsive Foundation Conference; Minneapolis, MN. 2009, August. [Google Scholar]
- 45.Piacentini J. Optimizing cognitive-behavioral therapy for childhood psychiatric disorders. J Am Acad Child Adol Psychiatry. 2008;47:481–482. doi: 10.1097/CHI.0b013e31816a0d8d. [DOI] [PubMed] [Google Scholar]
- 46.Valderhaug R, Larsson B, Gotestam G, Piacentini J. An open clinical trial with cognitive behavior therapy administered in outpatient psychiatric clinics to children and adolescents with OCD. Beh Res Therapy. 2007;45:577–589. doi: 10.1016/j.brat.2006.04.011. [DOI] [PubMed] [Google Scholar]