Abstract
Background:
Although the usage of combined motor and sensory intraoperative monitoring has been shown to improve the surgical outcome of patients with cervical myelopathy, the role of transcranial electric motor evoked potentials (tceMEP) used in conjunction with somatosensory evoked potentials (SSEP) in patients presenting with radiculopathy but without myelopathy has been less clear.
Methods:
We retrospectively reviewed all patients (n = 57) with radiculopathy but without myelopathy, undergoing anterior cervical decompression and fusion at a single institution over the past 3 years, who had intraoperative monitoring with both tceMEPs and SSEPs.
Results:
Fifty-seven (100%) patients presented with radiculopathy, 53 (93.0%) with mechanical neck pain, 35 (61.4%) with motor dysfunction, and 29 (50.9%) with sensory deficits. Intraoperatively, 3 (5.3%) patients experienced decreases in SSEP signal amplitudes and 4 (6.9%) had tceMEP signal changes. There were three instances where a change in neuromonitoring signal required intraoperative alteration of the surgical procedure: these were deemed clinically significant events/true positives. SSEP monitoring showed two false positives and two false negatives, whereas tceMEP monitoring only had one false positive and no false negatives. Thus, tceMEP monitoring exhibited higher sensitivity (33.3% vs. 100%), specificity (95.6% vs. 98.1%), positive predictive value (33.3% vs. 75.0%), negative predictive value (97.7% vs. 100%), and efficiency (91.7% vs. 98.2%) compared to SSEP monitoring alone.
Conclusions:
Here, we present a retrospective series of 57 patients where tceMEP/SSEP monitoring likely prevented irreversible neurologic damage. Though further prospective studies are needed, there may be a role for combined tceMEP/SSEP monitoring for patients undergoing anterior cervical decompression without myelopathy.
Keywords: Anterior cervical discectomy fusion, motor evoked potentials, radiculopathy, somatosensory evoked potentials
INTRODUCTION
Anterior cervical discectomy and fusion (ACDF) surgery is one of the most commonly performed procedures in neurosurgery and is often offered to patients with cervical radiculopathy.[1] Although an initial report by Flynn et al. in 1982 reported a complication rate of 0.45% in almost 70,000 patients,[15] more recent reports have suggested that the true complication rate is much higher, ranging from 4.4% to as high as approximately 20%.[15,16,25,27,28,31,42,43,48–50] These include a host of potential intra and postoperative complications including, but not limited to, vertebral artery laceration, carotid artery or jugular vein injury, spinal cord damage resulting in transient or permanent myelopathy, nerve root lesion, pharyngeal or esophageal laceration, postoperative epidural hematoma, wound infection, bone graft or instrumentation extrusion, and/or mechanical instability of the cervical spine.[3,6,20,24,38,44]
As timely correction of these complications is instrumental in establishing a positive outcome in patients, much focus has rested on the development of methods to ensure early identification of potentially devastating complications. Within the last decade, much debate has centered on the possibility of using somatosensory evoked potentials (SSEP) as a reliable way to detect intraoperative spinal cord injury.[22] However, the literature to date shows mixed results for SSEP monitoring during anterior cervical surgery.[28,31,34,49–51] In fact, while some conclude that SSEPs significantly lowered the incidence of postoperative neurological deficit, others report that SSEPs are not helpful at all. More recently, some have advocated the combined use of transcranial electric motor evoked potentials (tceMEP) in conjunction with SSEPs to increase the ability to detect intraoperatively possible spinal cord compromise.[9,23,27,36,42,51] However, many studies have failed to differentiate between patients with myelopathy and radiculopathy, and some even include other etiologies such as trauma or intraspinal tumors.[21,23,45] Because of the markedly different pathophysiologies of myelopathy, radiculopathy, trauma, or tumor, we believe that it is difficult to truly elucidate the utility of SSEP and/or tceMEP monitoring without studying each of these patient cohorts separately.
Thus, here we describe our retrospective experience with patients who had single or multilevel anterior cervical decompression and fusion for cervical radiculopathy without myelopathy. To our knowledge, this is one of the first case series to specifically report the outcomes of intraoperative SSEP monitoring in conjunction with tceMEPs in nonmyelopathic patients undergoing anterior cervical decompression.
MATERIALS AND METHODS
We retrospectively reviewed our patients who have undergone anterior cervical discectomy/corpectomy and fusion over the past 3 years. Inclusion criteria were defined to include patients with a preoperative diagnosis of radiculopathy who subsequently underwent one-, two-, or three-level anterior decompression and instrumented or non-instrumented fusion with either allograft or autograft bone. Exclusion criteria were defined to specifically exclude patients who had tumors or pre-existing myelopathy. Patient demographics such as age, sex, and co-morbidities including diabetes, coronary artery disease, osteoporosis, obesity, smoking, hypertension, and previous surgery were documented. Patients’ presenting symptoms, such as neck pain, weakness, motor and sensory deficits, as well as their duration were noted. The vertebral levels of each anterior cervical decompression were recorded.
Somatosensory evoked potentials monitoring
All monitoring was performed using the Viasys Endeavor CR (Carefusion). Initial (pre-baseline) SSEP signals were obtained after induction of anesthesia and after patient positioning in all cases unless there was a positioning concern (addressed by obtaining pre- and post-positioning data). Baseline signals were obtained after surgical exposure was completed. Continuous upper and lower extremity stimulation was performed simultaneously throughout the surgical procedure. Stimulation was accomplished with square-wave electrical pulses of 300 ms duration and an intensity of 25–50 mA at a frequency of 5.3 Hz. Somatosensory evoked responses were monitored after bilateral median and ulnar nerve stimulation at the wrist and posterior tibial nerve stimulation at the ankle using subdermal needle electrodes. Evoked potentials were recorded in a referential and a differential fashion from multiple scalp electrodes (international 10–20 system, Cz, C3, C4, and FpZ) as well as a linked ear electrode, Erb's points (arms) and the popliteal fossae (legs). Placement of Erb's point electrodes was outside the surgical field, and was typically easily recorded. The filter bandwidth was 30–500 Hz. For all patients, 300 trials were averaged. SSEP amplitude was defined as peak-to-peak amplitude.
Transcranial electric motor evoked potentials monitoring
For tceMEP, multipulse transcranial electrical stimulation was generated using the Viasys Endeavor CR (Carefusion) stimulator. Stimulation was applied using short trains of five square-waves, monophasic, anodal, constant-current electrical pulses of 500–1000 μs duration with an interstimulus interval of 2 ms at sites 2 cm anterior to C1/C2 position of the international 10–20 system. Stimulus intensity ranged from 250 to 400 V. tceMEPs were recorded simultaneously from abductor hallucis, anterior tibialis and abductor pollicis brevis muscles bilaterally using subdermal needles in these muscles with a distant reference electrode.
Electrophysiologic monitoring criteria
SSEP waveforms were analyzed for latency and peak-to-peak amplitude. Critical SSEP changes were defined as decreases in amplitude of more than 50% of baseline values or increases in latency of more than 10% of baseline values. A significant change was defined as a bilateral MEP loss or an asymmetric MEP loss or amplitude reduction. Systemic parameters or other potential factors such as anesthetic changes, level of neuromuscular blockade, blood pressure changes, body temperature changes, and technical problems were ruled out and discussed in real time with the surgeon as he was informed about changes. For patients with significant SSEP or tceMEP changes, operative records were reviewed to determine whether or not an intraoperative intervention took place, and whether or not such a change in surgical procedure led to an improvement of neurophysiologic monitoring signals. Any intraoperative intervention that was undertaken specifically due to significant SSEP or tceMEP changes was defined as a clinically significant event.
Medical chart review
Other intra and peri-operative data such as blood loss, length of hospitalization, incidental durotomies, CSF leakage, deep venous thrombosis, pulmonary embolism, infection, hematoma, wound dehiscence, dysphagia, discharge to rehabilitation facilities, reoperations, and instrumentation failure were obtained from operative, discharge, and clinic notes. Postoperative follow-up times, as well as functional outcomes (neck pain and arm radiculopathy), were ascertained from follow-up clinical notes.
RESULTS
Patient population
A total of 57 patients with cervical radiculopathy but without myelopathy underwent anterior cervical discectomy or corpectomy and fusion with both SSEP and tceMEP monitoring at our institution over the past 3 years. The average age was 47.6 11.1 years. All pathologies were degenerative in nature: 24 (42.1%), 30 (52.6%) and 3 (5.3%) patients had one-, two-, and three-level anterior cervical decompression and fusion, respectively. Eight (14.0%) had a history of diabetes, 1 (1.8%) osteoporosis, 4 (7.0%) obesity, 5 (8.8%) coronary artery disease, 12 (21.1%) smoking, 12 (21.1%) hypertension, and 9 (15.8%) had a history of previous spinal surgery. Fifty-three (93.0%) patients had a history of neck pain with an average length of 14.0 months; 57 (100%) patients had a history of radiculopathy with an average presenting symptom length of 13.9 months; 35 (61.4%) patients had motor deficits for an average of 7.6 months; and 29 (50.9%) had sensory deficits for an average of 9.5 months.
Intraoperative and postoperative outcomes
Intraoperative monitoring changes in cases with clinically significant events
Intraoperatively, three clinically significant events were encountered [Table 1]. The first involved a 64-year-old male patient who presented with C4–C5 and C5–C6 disc herniation, neck pain, and radiculopathy. He underwent a C5 corpectomy and C4–C5/C5–C6 discectomy and fusion. Intraoperatively, an incidental durotomy was encountered, and was repaired initially with a gel-foam matrix and dural sealant (DuraSeal). After the placement of the graft, left arm and leg tceMEP, but not SSEP, monitoring showed a significant decrease in signal which led to removal of the bone graft and the subsequent discovery of significant swelling of the dural sealant, causing noticeable spinal cord compression when the cage was applied. The dural sealant mass was removed and replaced with fibrin glue, and the tceMEP signals recovered to baseline immediately. Twenty milligrams of IV dexamethasone were administered intravenously. The operation was completed without further complications. The patient was discharged to home on postoperative day 3 without motor or sensory deficits. At his last follow-up at 8 months, the patient exhibited no neurological deficits, radicular pain resolution, and neck pain rated at 2/10.
Table 1.
Summary of intraoperative clinically significant events in patients undergoing anterior cervical discectomy and fusion for nonmyelopathic radiculopathy
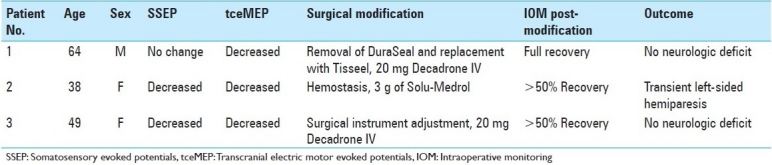
The second clinically significant event occurred with a 38-year-old female who presented with an acute C2–C3 disc herniation status post C3–C4 and C4–C5 ACDFs, 2 years prior. Intraoperatively, there was a transient SSEP and tceMEP decrease in signal for both the left arm and left leg. The change in signal was thought to be due to spinal cord manipulation, and led the surgeon to administer high dose IV steroids, as consistent with acute spinal cord injury protocols. Both SSEP and MEP signals on the left side recovered to greater than 50% of baseline by the end of the surgery, but did not fully return to baseline. Postoperatively, the patient had a transient course of left-sided hemiparesis and right-sided diminished sensation. She was discharged to rehabilitation on postoperative day 4. By 2 months follow-up, the patient had recovered full motor strength and experienced resolution of her neck pain and radiculopathy. However, by 6 months follow-up, the patient experienced dyphagia, plate back-out, and underwent reoperation for plate removal. At her most recent clinic visit at 27 months, the patient had excellent motor function with continued mild right-sided numbness.
The third clinically significant event occurred with a 49-year-old female who presented with left C7 radiculopathy and C5–C7 spondylosis. She underwent a two-level ACDF. Intraoperatively, there was an episode of excessive spinal cord manipulation which was suspected as a potential source for cord compromise by the surgeon and confirmed with a transient decrease in tceMEP, but not SSEP, signals in both upper and lower limbs on the left side. Immediately, 10 mg of epinephrine along with 20 mg of dexamethasone were administered. Greater than 50% of the affected tceMEP signals recovered, although not completely to baseline. Postoperatively, the patient complained of left-hand paresthesias and weakness. She was discharged home on postoperative day 3, requiring neuropathic pain medications. At her most recent follow-up of 24 months, the patient reported minimal neck and radicular pain. She experienced no weakness of her left hand.
Intraoperative monitoring changes in cases without clinically significant events
In total, three patients had significant SSEP changes intraoperatively [Table 2]. Nine patients did not have reliable SSEP readings. This may have been due to pre-existing neurological deficits affecting the sensory system in these patients, or could have been a function of the fact that our recording parameters were optimized for tceMEP recordings. These nine patients were excluded from our statistical analysis with regards to the utility of SSEP monitoring. None of the patients had irreversible SSEP changes. Among the patients who had SSEP changes, one had a clinically significant event, defined by intraoperative verification and treatment by the surgeon (as described above). Two additional patients had SSEP changes with were communicated to the surgeon. However, since no possible precipitating factors could be identified, no corrective measures were taken and the signals ultimately recovered without intervention.
Table 2.
Summary of somatosensory evoked potentials monitoring in patients (nine cases were excluded due to inability to record reliable somatosensory evoked potentials signals at baseline)

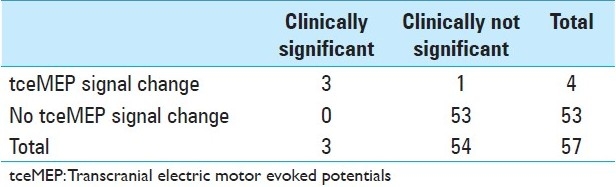
All the patients had reproducible baseline MEP responses. Intraoperatively, four patients had significant tceMEP changes, corresponding to the three patients who experienced clinically significant intraoperative events [Figure 1]. In addition, there was one patient whose tceMEP tracings returned to normal without surgical intervention before any exploration of the possible cause of the event could be undertaken [Table 3].
Figure 1.
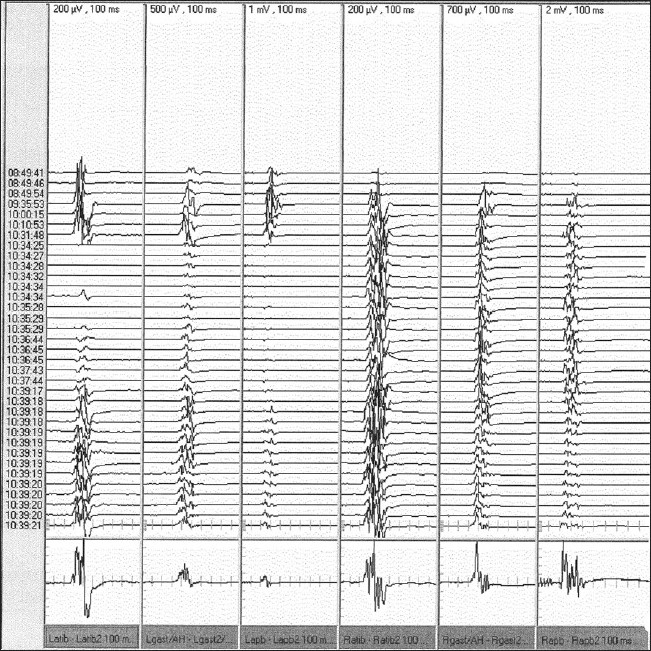
Representative motor evoked potentials signal from the left and right upper and lower extremities after transcranial electrical stimulation in a patient with a true clinically significant event. There was a sudden decrease/loss of the left-sided motor evoked potentials signals at 10:34:25, while the right-sided signals remained stable. The surgeons were informed immediately and the left-sided signals recovered at around 10:39:18 after surgical intervention. Latib: left anterior tibialis; Lgast/AH: left gastrocnemius/abductor hallucis; Lapb: left abductor pollicis brevis; Ratib: right anterior tibialis; Rgast/AH: right gastrocnemius/ abductor hallucis; Rapb: right abductor pollicis brevis
Table 3.
Summary of motor evoked potentials monitoring in patients
Clinically significant events without intraoperative monitoring changes
Lastly, two patients who had clinically significant events did not have SSEP signal changes (as described above) [Table 2], while none of the patients had clinically significant events without accompanying tceMEP changes [Table 3].
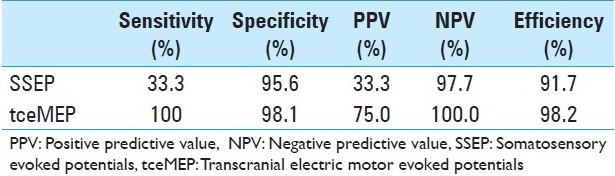
Statistical analysis
Thus, the positive predictive value for SSEP signal changes was 33.3% and the negative predictive value was 75.0% [Table 4]. The sensitivity and specificity were 33.3% and 95.6%, respectively. The overall efficiency of the test was 91.7%. In comparison, the positive predictive value for tceMEP monitoring in identifying clinically significant intraoperative events was 75.0% and the negative predictive value was 100.0%. The sensitivity was 100% and the specificity was 98.1%, significantly higher than that experienced by SSEP. The efficiency of tceMEP was calculated to be 98.2%.
Table 4.
Comparison of sensitivity, specificity, positive predictive value, and negative predictive value of somatosensory evoked potentials versus transcranial electric motor evoked potentials monitoring
Finally, it should be noted that no adverse events as a result of our monitoring occurred.
Postoperative outcomes
In the immediate postoperative period, there were no cases of mortality, wound infection, wound dehiscence, deep venous thrombosis, pulmonary embolism, hematoma, right laryngeal nerve palsy, Horner's syndrome, CSF leak, or pharyngeal/esophageal perforation. Other than the patients described above, there were no other cases of peri-operative neurologic deficit, dysphagia, or plate back-out. By an average of 8 months follow-up, 87.5% patients experienced neck pain resolution. 90.0% had no persistent or recurrent radiculopathy.
DISCUSSION
In this retrospective study, we describe our 3-year experience with patients who had single or multilevel anterior cervical decompression and fusion for cervical radiculopathy without myelopathy. Here, we have shown that tceMEP in conjunction with SSEP monitoring increases the sensitivity (from 33.3 to 100%), specificity (from 95.6 to 98.1%), positive predictive value (from 33.3 to 75.0%), negative predictive value (from 97.7 to 100%), and efficiency (from 91.7 to 98.2%) of detecting truly clinically significant events compared to SSEP monitoring alone [Table 4].
Although rare, neurologic deficit is one of the most devastating complications of spine surgery.[4,11,14] Thus, within the past two decades, increased emphasis has been placed on developing intraoperative neurophysiologic methods to accurately monitor the integrity of the spinal cord during spinal surgery.[5,8–9] Currently, one such widely used technique is SSEP.[19] Although SSEP monitoring has been utilized with great success in scoliosis and thoracolumbar spine surgery,[10,12,13,17,30,31,39–42,46,49,53–55] where it has been credited with reducing the incidence of neurological complications from 4–6.9% to 0–0.7%,[2,12,26,35,52,54] the usefulness of such a procedure in anterior cervical spine surgery (particularly in patients without myelopathy) is still unclear.[18,32,33,37] Indeed, although some studies have attributed SSEP monitoring to decrease the incidence of postoperative neurologic injury from 3.7 to 0%,[13] others have found SSEP monitoring in cervical spine surgery to be less useful, with Jones et al. highlighting two patients who experienced temporary quadriparesis after anterior cervical surgery despite having normal SSEP tracings.[25] In the largest series of nonmyelopathic patients recently published, Smith et al. analyzed 1039 consecutive patients undergoing cervical spine surgery.[49] Of these, 577 patients were monitored with SSEP only and six significant changes were reported (the remaining 462 cases were not monitored and served as controls). Increasing the blood pressure improved SSEP in five patients, and retractor repositioning led to SSEP improvement in the sixth patient. However, the only case of new postoperative neurological deficit (partial central cord syndrome) occurred in a patient who did not have any SSEP changes.
Due to this and other reports of SSEP's low sensitivity and positive predictive value, some have more recently suggested using tceMEP monitoring in conjunction with SSEP tracings during cervical spine surgery. To date, reports of combined monitoring are still sparse in the literature, and many intraoperative monitoring series combine patients monitored with SSEP only with those monitored with tceMEP in conjunction with SSEP. Moreover, although a number of studies within the past 5 years have reported beneficial results of tceMEP monitoring, all include patients with multiple etiologies, ranging from intradural tumors, degenerative disease, to myelopathy or trauma. In one of the largest intraoperative neuromonitoring studies to date, Kelleher et al. looked at 1055 patients, and found SSEP to have a sensitivity of 52%, specificity of 100%, positive predictive value of 100% and a negative predictive value of 97%. In contrast, tceMEPs had a sensitivity of 100%, specificity of 96%, positive predictive value of 96%, and a negative predictive value of 100%. While Kelleher et al. and others agree that tceMEPs decrease the rate of false negatives compared to SSEP monitoring alone, most base their conclusions on the use of tceMEPs in a small number of patients (e.g. only 26 out of 1055 patients in Kelleher et al.'s study were monitored using tceMEP in addition to SSEPs). Furthermore, these patients were usually those with pre-operative spinal cord damage such as myelopathy, trauma, or intramedullary tumors (approximately 80% in Kelleher et al.'s study).[29,31,32,47,49] Thus, to our knowledge, this study represents one of the first to examine the usage of combined SSEP and tceMEP monitoring in patients undergoing anterior cervical discectomy/corpectomy and fusion for radiculopathy only.
A challenge in all neurophysiologic monitoring studies is the appropriate definition of true positives, or clinically significant events. Objectively, a true positive is a patient with significant intraoperative SSEP or tceMEP changes who, without surgical intervention, experiences postoperative neurological deterioration. Thus, the gold standard experiment for determining the efficacy of SSEP/tceMEP monitoring would compare the neurological outcome of patients with surgical intervention with that of patients without intraoperative correction despite SSEP or tceMEP changes. However, ethical considerations make such a study unfeasible (especially in light of unexpected intraoperative complications), and thus a more utilitarian definition for a true positive must be constructed. Some studies have defined true positives as patients with postoperative neurological deficit.[49–51] However, this misses instances where a patient experiences SSEP or tceMEP changes and an intraoperative intervention restored the transient signal changes to baseline values. In these cases, it is very likely that such transient SSEP/tceMEP signal changes, if uncorrected, would have resulted in clinical morbidity. Therefore, these cases cannot be discounted from being clinically significant.
Because of this, we included in our true positives both patients with postoperative neurologic deficits as well as patients where the surgeon corrected his operative approach or administered steroids directly due to notification of SSEP or tceMEP changes. In our study, we were certain of our clinically significant events based on excellent documentation of the corrective surgical intervention that restored neuromonitoring signals. Furthermore, our team approach of troubleshooting our equipment, discussing systemic variables such as changes in body temperature, fluctuations in anesthesia concentration, or variations in arterial CO2 concentrations with the anesthesia team while updating the surgeons continuously helped to decrease the incidence of false positives by discounting the incidences of SSEP or tceMEP changes that could be attributed to nonsurgical variables.[7,8,20,32,54] Detailed documentation of this process allowed us to count a total of three patients with clinically significant events in our case series.
In our experience, the overall incidence of postoperative neurologic deficit was rare, as only 1 out of 57 patients (1.7%) experienced an episode of hemiparesis which ultimately proved to be transient. This is consistent with the fact that postoperative complications are uncommon overall in ACDF procedures.
A possible reason for the higher efficacy of tceMEP monitoring during anterior cervical surgery may be the anatomy of the spinal cord.[49] Whereas the ascending somatosensory pathways are located dorsally, the corticospinal motor tracts are located more anterolaterally. As ACDF involves approaching the spinal cord anteriorly, it is possible that the motor pathways are more at risk for injury that the ascending dorsal columns.
Taken together, we believe that tceMEP monitoring may be a safe and efficacious method of intraoperative neuromonitoring when combined with SSEP in ACDF surgeries for radiculopathy. It is important to note that SSEP monitoring is still necessary and of significant value in these cases since it aids with troubleshooting and may on occasion detect a complication affecting the posterior cord. Given that 3 out of 57 (5.3%) patients required steroid administration, increased perfusion pressure, or alteration in surgical strategy in response to significant changes in tceMEP, we believe that some patients, albeit few, might benefit from such combined neurophysiologic monitoring.
CONCLUSIONS
Although recent evidence supports the use of tceMEPs along with SSEP monitoring in myelopathic patients or patients with intraspinal tumors, none have examined the utility of tceMEP/SSEPs in the context of patients with radiculopathy without central spinal cord compromise. In this paper, we presented a series of 57 patients undergoing anterior cervical decompression and fusion for radiculopathy alone, who underwent concomitant SSEP/tceMEP neurophysiologic monitoring. In 3 (5.3%) cases, combined SSEP/tceMEP monitoring allowed for an immediate change in operative procedure, adequate elevation of blood pressure to maintain spinal cord perfusion, and administration of IV steroids – measures that are all known to protect the spinal cord from the secondary sequelae of injury. The use of tceMEPs in conjunction with SSEPs in radiculopathic patients without myelopathy may significantly enhance the efficaciousness of intraoperatively identifying possible spinal cord injury compared to SSEP monitoring alone, allowing for real-time correction and possible prevention of irreversible neurologic injury.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2011/2/1/133/85606
Contributor Information
Risheng Xu, Email: rxu4@jhmi.edu.
Eva K. Ritzl, Email: eritzl1@jhmi.edu.
Mohammed Sait, Email: mohsait@hotmail.com.
Daniel M. Sciubba, Email: dsciubb1@jhmi.edu.
Jean-Paul Wolinsky, Email: jwolins3@jhmi.edu.
Timothy F. Witham, Email: twitham2@jhmi.edu.
Ziya L. Gokaslan, Email: zgokasl1@jhmi.edu.
Ali Bydon, Email: abydon1@jhmi.edu.
REFERENCES
- 1.Angevine PD, Arons RR, McCormick PC. National and regional rates and variation of cervical discectomy with and without anterior fusion, 1990-1999. Spine (Phila Pa 1976) 2003;28:931–40. doi: 10.1097/01.BRS.0000058880.89444.A9. [DOI] [PubMed] [Google Scholar]
- 2.Balzer JR, Rose RD, Welch WC, Sclabassi RJ. Simultaneous somatosensory evoked potential and electromyographic recordings during lumbosacral decompression and instrumentation. Neurosurgery. 1998;42:1318–25. doi: 10.1097/00006123-199806000-00074. [DOI] [PubMed] [Google Scholar]
- 3.Bohlman HH, Emery SE, Goodfellow DB, Jones PK. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy.Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am. 1993;75:1298–307. doi: 10.2106/00004623-199309000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Bommireddy R, Kamat A, Smith ET, Nixon T, Pillay R, Pigott T, et al. Magnetic resonance image findings in the early post-operative period after anterior cervical discectomy. Eur Spine J. 2007;16:27–31. doi: 10.1007/s00586-005-0045-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bose B, Sestokas AK, Schwartz DM. Neurophysiological detection of iatrogenic C-5 nerve deficit during anterior cervical spinal surgery. J Neurosurg Spine. 2007;6:381–5. doi: 10.3171/spi.2007.6.5.381. [DOI] [PubMed] [Google Scholar]
- 6.Brigham CD, Tsahakis PJ. Anterior cervical foraminotomy and fusion.Surgical technique and results. Spine (Phila Pa 1976) 1995;20:766–70. [PubMed] [Google Scholar]
- 7.Browning JL, Heizer ML, Baskin DS. Variations in corticomotor and somatosensory evoked potentials: effects of temperature, halothane anesthesia, and arterial partial pressure of CO2. Anesth Analg. 1992;74:643–8. doi: 10.1213/00000539-199205000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Chappuis JL, Johnson G. Using intraoperative electrophysiologic monitoring as a diagnostic tool for determining levels to decompress in the cervical spine: A case report. J Spinal Disord Tech. 2007;20:403–7. doi: 10.1097/BSD.0b013e31803755d5. [DOI] [PubMed] [Google Scholar]
- 9.Costa P, Bruno A, Bonzanino M, Massaro F, Caruso L, Vincenzo I, et al. Somatosensory- and motor-evoked potential monitoring during spine and spinal cord surgery. Spinal Cord. 2007;45:86–91. doi: 10.1038/sj.sc.3101934. [DOI] [PubMed] [Google Scholar]
- 10.Deutsch H, Arginteanu M, Manhart K, Perin N, Camins M, Moore F, et al. Somatosensory evoked potential monitoring in anterior thoracic vertebrectomy. J Neurosurg. 2000;92(2 Suppl):155–61. doi: 10.3171/spi.2000.92.2.0155. [DOI] [PubMed] [Google Scholar]
- 11.Dimopoulos VG, Chung I, Lee GP, Johnston KW, Kapsalakis IZ, Smisson HF, 3rd, et al. Quantitative estimation of the recurrent laryngeal nerve irritation by employing spontaneous intraoperative electromyographic monitoring during anterior cervical discectomy and fusion. J Spinal Disord Tech. 2009;22:1–7. doi: 10.1097/BSD.0b013e31815ea8b6. [DOI] [PubMed] [Google Scholar]
- 12.Engler GL, Spielholz NJ, Bernhard WN, Danziger F, Merkin H, Wolff T. Somatosensory evoked potentials during Harrington instrumentation for scoliosis. J Bone Joint Surg Am. 1978;60:528–32. [PubMed] [Google Scholar]
- 13.Epstein NE, Danto J, Nardi D. Evaluation of intraoperative somatosensory-evoked potential monitoring during 100 cervical operations. Spine (Phila Pa 1976) 1993;18:737–47. doi: 10.1097/00007632-199305000-00011. [DOI] [PubMed] [Google Scholar]
- 14.Fehlings MG, Houldon D, Vajkoczy P. Introduction. Intraoperative neuromonitoring: An essential component of the neurosurgical and spinal armamentarium. Neurosurg Focus. 2009;27:E1. doi: 10.3171/2009.8.FOCUS.OCT09.INTRO. [DOI] [PubMed] [Google Scholar]
- 15.Flynn TB. Neurologic complications of anterior cervical interbody fusion. Spine (Phila Pa 1976) 1982;7:536–9. doi: 10.1097/00007632-198211000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Fountas KN, Kapsalaki EZ, Nikolakakos LG, Smisson HF, Johnston KW, Grigorian AA, et al. Anterior cervical discectomy and fusion associated complications. Spine (Phila Pa 1976) 2007;32:2310–7. doi: 10.1097/BRS.0b013e318154c57e. [DOI] [PubMed] [Google Scholar]
- 17.Gonzalez AA, Jeyanandarajan D, Hansen C, Zada G, Hsieh PC. Intraoperative neurophysiological monitoring during spine surgery: A review. Neurosurg Focus. 2009;27:E6. doi: 10.3171/2009.8.FOCUS09150. [DOI] [PubMed] [Google Scholar]
- 18.Gugino V, Chabot RJ. Somatosensory evoked potentials. Int Anesthesiol Clin. 1990;28:154–64. doi: 10.1097/00004311-199002830-00005. [DOI] [PubMed] [Google Scholar]
- 19.Gunnarsson T, Krassioukov AV, Sarjeant R, Fehlings MG. Real-time continuous intraoperative electromyographic and somatosensory evoked potential recordings in spinal surgery: correlation of clinical and electrophysiologic findings in a prospective, consecutive series of 213 cases. Spine (Phila Pa 1976) 2004;29:677–84. doi: 10.1097/01.brs.0000115144.30607.e9. [DOI] [PubMed] [Google Scholar]
- 20.Heidecke V, Rainov NG, Marx T, Burkert W. Outcome in Cloward anterior fusion for degenerative cervical spinal disease. Acta Neurochir (Wien) 2000;142:283–91. doi: 10.1007/s007010050037. [DOI] [PubMed] [Google Scholar]
- 21.Hilibrand AS, Schwartz DM, Sethuraman V, Vaccaro AR, Albert TJ. Comparison of transcranial electric motor and somatosensory evoked potential monitoring during cervical spine surgery. J Bone Joint Surg Am. 2004;86-A:1248–53. doi: 10.2106/00004623-200406000-00018. [DOI] [PubMed] [Google Scholar]
- 22.Hurlbert RJ, Fehlings MG, Moncada MS. Use of sensory-evoked potentials recorded from the human occiput for intraoperative physiologic monitoring of the spinal cord. Spine (Phila Pa 1976) 1995;20:2318–27. doi: 10.1097/00007632-199511000-00010. [DOI] [PubMed] [Google Scholar]
- 23.Hyun SJ, Rhim SC, Kang JK, Hong SH, Park BR. Combined motor- and somatosensory-evoked potential monitoring for spine and spinal cord surgery: Correlation of clinical and neurophysiological data in 85 consecutive procedures. Spinal Cord. 2009;47:616–22. doi: 10.1038/sc.2009.11. [DOI] [PubMed] [Google Scholar]
- 24.Jho HD, Kim WK, Kim MH. Anterior microforaminotomy for treatment of cervical radiculopathy: part 1-disc-preserving “functional cervical disc surgery”. Neurosurgery. 2002;51(5 Suppl):S46–53. [PubMed] [Google Scholar]
- 25.Jones SJ, Buonamassa S, Crockard HA. Two cases of quadriparesis following anterior cervical discectomy, with normal perioperative somatosensory evoked potentials. J Neurol Neurosurg Psychiatry. 2003;74:273–6. doi: 10.1136/jnnp.74.2.273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Keith RW, Stambough JL, Awender SH. Somatosensory cortical evoked potentials: A review of 100 cases of intraoperative spinal surgery monitoring. J Spinal Disord. 1990;3:220–6. [PubMed] [Google Scholar]
- 27.Kelleher MO, Tan G, Sarjeant R, Fehlings MG. Predictive value of intraoperative neurophysiological monitoring during cervical spine surgery: A prospective analysis of 1055 consecutive patients. J Neurosurg Spine. 2008;8:215–21. doi: 10.3171/SPI/2008/8/3/215. [DOI] [PubMed] [Google Scholar]
- 28.Khan MH, Smith PN, Balzer JR, Crammond D, Welch WC, Gerszten P, et al. Intraoperative somatosensory evoked potential monitoring during cervical spine corpectomy surgery: Experience with 508 cases. Spine (Phila Pa 1976) 2006;31:E105–13. doi: 10.1097/01.brs.0000200163.71909.1f. [DOI] [PubMed] [Google Scholar]
- 29.Kim DH, Zaremski J, Kwon B, Jenis L, Woodard E, Bode R, et al. Risk factors for false positive transcranial motor evoked potential monitoring alerts during surgical treatment of cervical myelopathy. Spine (Phila Pa 1976) 2007;32:3041–6. doi: 10.1097/BRS.0b013e31815d0072. [DOI] [PubMed] [Google Scholar]
- 30.Krassioukov AV, Sarjeant R, Arkia H, Fehlings MG. Multimodality intraoperative monitoring during complex lumbosacral procedures: Indications, techniques, and long-term follow-up review of 61 consecutive cases. J Neurosurg Spine. 2004;1:243–53. doi: 10.3171/spi.2004.1.3.0243. [DOI] [PubMed] [Google Scholar]
- 31.Lee JY, Hilibrand AS, Lim MR, Zavatsky J, Zeiller S, Schwartz DM, et al. Characterization of neurophysiologic alerts during anterior cervical spine surgery. Spine (Phila Pa 1976) 2006;31:1916–22. doi: 10.1097/01.brs.0000228724.01795.a2. [DOI] [PubMed] [Google Scholar]
- 32.Magit DP, Hilibrand AS, Kirk J, Rechtine G, Albert TJ, Vaccaro AR, et al. Questionnaire study of neuromonitoring availability and usage for spine surgery. J Spinal Disord Tech. 2007;20:282–9. doi: 10.1097/01.bsd.0000211286.98895.ea. [DOI] [PubMed] [Google Scholar]
- 33.Matz PG, Holly LT, Groff MW, Vresilovic EJ, Anderson PA, Heary RF, et al. Indications for anterior cervical decompression for the treatment of cervical degenerative radiculopathy. J Neurosurg Spine. 2009;11:174–82. doi: 10.3171/2009.3.SPINE08720. [DOI] [PubMed] [Google Scholar]
- 34.May DM, Jones SJ, Crockard HA. Somatosensory evoked potential monitoring in cervical surgery: identification of pre- and intraoperative risk factors associated with neurological deterioration. J Neurosurg. 1996;85:566–73. doi: 10.3171/jns.1996.85.4.0566. [DOI] [PubMed] [Google Scholar]
- 35.Meyer PR, Jr, Cotler HB, Gireesan GT. Operative neurological complications resulting from thoracic and lumbar spine internal fixation. Clin Orthop Relat Res. 1988;237:125–31. [PubMed] [Google Scholar]
- 36.Nagle KJ, Emerson RG, Adams DC, Heyer EJ, Roye DP, Schwab FJ, et al. Intraoperative monitoring of motor evoked potentials: A review of 116 cases. Neurology. 1996;47:999–1004. doi: 10.1212/wnl.47.4.999. [DOI] [PubMed] [Google Scholar]
- 37.Nair DR, Luders H. Does somatosensory evoked potential monitoring have a role during cervical corpectomy? Nat Clin Pract Neurol. 2006;2:594–5. doi: 10.1038/ncpneuro0344. [DOI] [PubMed] [Google Scholar]
- 38.Nandoe Tewarie RD, Bartels RH, Peul WC. Long-term outcome after anterior cervical discectomy without fusion. Eur Spine J. 2007;16:1411–6. doi: 10.1007/s00586-007-0309-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nuwer MR, Dawson EG, Carlson LG, Kanim LE, Sherman JE. Somatosensory evoked potential spinal cord monitoring reduces neurologic deficits after scoliosis surgery: results of a large multicenter survey. Electroencephalogr Clin Neurophysiol. 1995;96:6–11. doi: 10.1016/0013-4694(94)00235-d. [DOI] [PubMed] [Google Scholar]
- 40.Paradiso G, Lee GY, Sarjeant R, Fehlings MG. Multi-modality neurophysiological monitoring during surgery for adult tethered cord syndrome. J Clin Neurosci. 2005;12:934–6. doi: 10.1016/j.jocn.2005.03.012. [DOI] [PubMed] [Google Scholar]
- 41.Paradiso G, Lee GY, Sarjeant R, Hoang L, Massicotte EM, Fehlings MG. Multimodality intraoperative neurophysiologic monitoring findings during surgery for adult tethered cord syndrome: Analysis of a series of 44 patients with long-term follow-up. Spine (Phila Pa 1976) 2006;31:2095–102. doi: 10.1097/01.brs.0000231687.02271.b6. [DOI] [PubMed] [Google Scholar]
- 42.Pelosi L, Lamb J, Grevitt M, Mehdian SM, Webb JK, Blumhardt LD. Combined monitoring of motor and somatosensory evoked potentials in orthopaedic spinal surgery. Clin Neurophysiol. 2002;113:1082–91. doi: 10.1016/s1388-2457(02)00027-5. [DOI] [PubMed] [Google Scholar]
- 43.Peolsson A, Peolsson M. Predictive factors for long-term outcome of anterior cervical decompression and fusion: A multivariate data analysis. Eur Spine J. 2008;17:406–14. doi: 10.1007/s00586-007-0560-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pointillart V, Cernier A, Vital JM, Senegas J. Anterior discectomy without interbody fusion for cervical disc herniation. Eur Spine J. 1995;4:45–51. doi: 10.1007/BF00298418. [DOI] [PubMed] [Google Scholar]
- 45.Quinones-Hinojosa A, Gulati M, Lyon R, Gupta N, Yingling C. Spinal cord mapping as an adjunct for resection of intramedullary tumors: Surgical technique with case illustrations. Neurosurgery. 2002;51:1199–207. doi: 10.1097/00006123-200211000-00015. [DOI] [PubMed] [Google Scholar]
- 46.Quraishi NA, Lewis SJ, Kelleher MO, Sarjeant R, Rampersaud YR, Fehlings MG. Intraoperative multimodality monitoring in adult spinal deformity: Analysis of a prospective series of one hundred two cases with independent evaluation. Spine (Phila Pa 1976) 2009;34:1504–12. doi: 10.1097/BRS.0b013e3181a87b66. [DOI] [PubMed] [Google Scholar]
- 47.Resnick DK, Anderson PA, Kaiser MG, Groff MW, Heary RF, Holly LT, et al. Electrophysiological monitoring during surgery for cervical degenerative myelopathy and radiculopathy. J Neurosurg Spine. 2009;11:245–52. doi: 10.3171/2009.2.SPINE08730. [DOI] [PubMed] [Google Scholar]
- 48.Sebastian C, Raya JP, Ortega M, Olalla E, Lemos V, Romero R. Intraoperative control by somatosensory evoked potentials in the treatment of cervical myeloradiculopathy. Results in 210 cases. Eur Spine J. 1997;6:316–23. doi: 10.1007/BF01142677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Smith PN, Balzer JR, Khan MH, Davis RA, Crammond D, Welch WC, et al. Intraoperative somatosensory evoked potential monitoring during anterior cervical discectomy and fusion in nonmyelopathic patients-a review of 1,039 cases. Spine J. 2007;7:83–7. doi: 10.1016/j.spinee.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 50.Taunt CJ, Jr, Sidhu KS, Andrew SA. Somatosensory evoked potential monitoring during anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 2005;30:1970–2. doi: 10.1097/01.brs.0000176321.02963.72. [DOI] [PubMed] [Google Scholar]
- 51.Weinzierl MR, Reinacher P, Gilsbach JM, Rohde V. Combined motor and somatosensory evoked potentials for intraoperative monitoring: Intra-and postoperative data in a series of 69 operations. Neurosurg Rev. 2007;30:109–16. doi: 10.1007/s10143-006-0061-5. [DOI] [PubMed] [Google Scholar]
- 52.Whittle IR, Johnston IH, Besser M. Recording of spinal somatosensory evoked potentials for intraoperative spinal cord monitoring. J Neurosurg. 1986;64:601–12. doi: 10.3171/jns.1986.64.4.0601. [DOI] [PubMed] [Google Scholar]
- 53.Wiggns GC, Rauzzino MJ, Bartkowski HM, Nockels RP, Shaffrey CI. Management of complex pediatric and adolescent spinal deformity. J Neurosurg. 2001;95(1 Suppl):17–24. doi: 10.3171/spi.2001.95.1.0017. [DOI] [PubMed] [Google Scholar]
- 54.Wilber RG, Thompson GH, Shaffer JW, Brown RH, Nash CL., Jr Postoperative neurological deficits in segmental spinal instrumentation.A study using spinal cord monitoring. J Bone Joint Surg Am. 1984;66:1178–87. [PubMed] [Google Scholar]
- 55.Zeiller SC, Lee J, Lim M, Vaccaro AR. Posterior thoracic segmental pedicle screw instrumentation: evolving methods of safe and effective placement. Neurol India. 2005;53:458–65. doi: 10.4103/0028-3886.22613. [DOI] [PubMed] [Google Scholar]


