Abstract
Background:
Psammomatous melanotic schwannomas (PMS) of the spine may be a component of the Carney complex in 50% of cases and is inherited in an autosomal dominant manner. Most PMS are benign and frequently associated with lentiginous pigmentation; cardiac, cutaneous, or breast myxomas; endocrine overactivity; and cutaneous blue nevi. These tumors are characterized by melanin containing cells having ultrastructural characteristics of Schwann cells.
Case Description:
Two patients had spinal PMS that were surgically resected with adjacent local radiotherapy, followed by local recurrence and metastasis. The aggressive nature of this tumor is reported.
Conclusion:
Spinal PMS are rarely malignant with local recurrence and distal metastases. Inquiry into the patient's and family members’ hereditary background for the Carney complex is important to avoid overlooking potential lethal associated abnormalities.
Keywords: Carney complex, malignant, melanin, psammoma body, schwannoma, spine
INTRODUCTION
Melanotic schwannomas consist of melanin containing nerve sheath tumors[5,11,21] arising from somatic and autonomic nerves. Most tumors are benign; however, 10% are malignant with metastasis.[1,3,15,19]
Psammomatous melanotic schwannomas (PMS) (predominantly spinal), myxomas (cardiac, mammary, and cutaneous), spotty pigmentation, endocrine overactivity, and cutaneous blue nevi constitute the Carney complex with autosomal dominant inheritance.[3,24] The mean age is 37 years (10–84 years) with a female preponderance (1.4:1).[21]
Two cases of malignant spinal PMS are reported with a uniquely aggressive course. The differential diagnosis, surgical treatment, and pathological appearance of this tumor are presented. The hereditary nature mandates an extensive investigation to identify the presence of this tumor in patients and their families.
CASE REPORTS
Case 1
A 65-year-old woman presented with a history of mid-thoracic spinal pain. Neurological and physical examination as well as family history were noncontributory. Erosion of the right T7 and T8 pedicles was observed on computed tomography (CT) scan [Figure 1a], and a magnetic resonance imaging (MRI) scan revealed a 3.0 × 2.0 × 1.5 cm, right enhancing, T6-8 extradural mass [Figure 1b] with transforamenal extension into the mediastinum.
Figure 1.
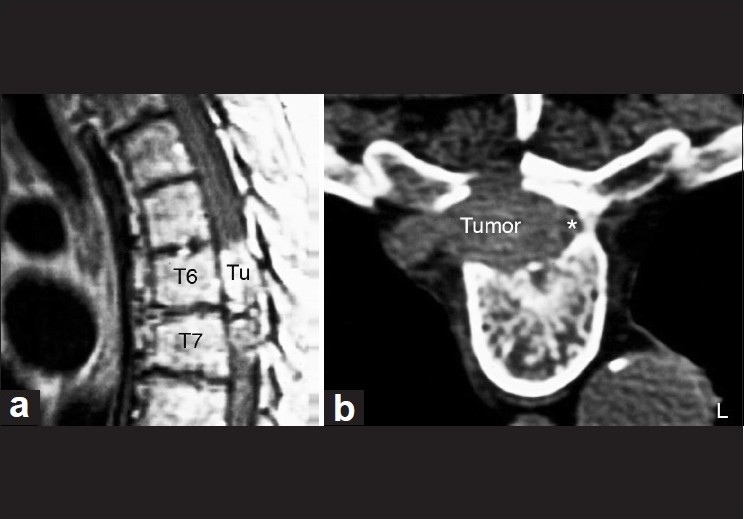
(a) MRI scan demonstrating intraspinal PMS. Tu = tumor. (b) The spinal cord is displaced to the right (asterisk), along with erosion and enlargement of the right T6–T7 intervertebral foramen and extension into the posterior mediastinum
A laminectomy was performed and a circumscribed soft black extradural mass was resected, initially thought to be a melanotic melanoma. Complete tumor resection was not possible; however, margins were resected where possible. Postoperative external beam radiotherapy (XRT) with a boost to the tumor bed was performed. Eight months later, local tumor developed in the T8 vertebral body, necessitating local resection of a tumor with identical histology as the initial diagnosis. The patient died within a short time postoperatively.
Histological examination revealed epithelioid and spindle-shaped cells [Figure 2a] with intracytoplasmic melanotic granules, psammoma bodies [Figure 2b], and positive S-100 protein and vimentin immunostaining which confirmed it to be a malignant PMS.
Figure 2.
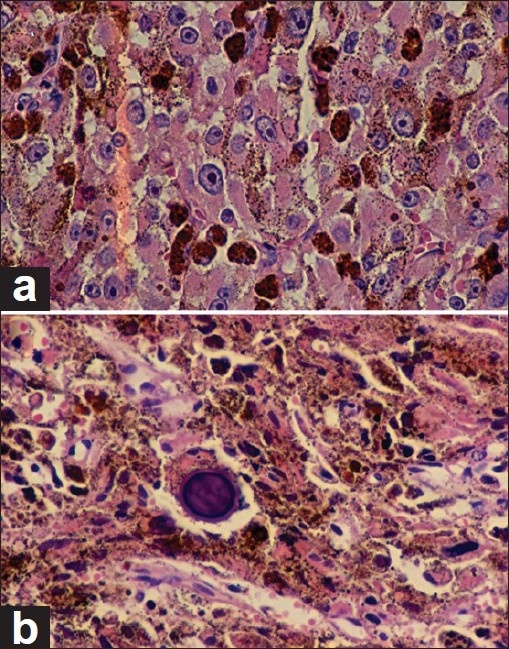
(a) Epithelioid pattern of tumor cells with dense intracytoplasmic melanin granules by H and E stain (magnification ×400). (b) Large psammoma body in the center. Large amount of melanin throughout the area of the tumor (H and E, ×400)
Case 2
A 33-year-old male developed low back pain and right L5 radiculopathy. There was a family history of "cardiac tumors", but no symptoms of the Carney complex were elicited. Lumbar MRI revealed a right L5-S1 epidural mass with transforamenal extraspinal extension.
At surgery, a black tumor in the right L5-S1 neural foramen encased adjacent nerve roots. Frozen section suggested a malignant melanoma and therefore, a wide resection was performed including resection of the L5 nerve root providing grossly clear margins. Eighteen months later, an MRI scan revealed a recurrent tumor in the right sacrum [Figure 3] with retroperitoneal extension infiltrating the right iliacus and psoas muscles. An anterior L5 vertebrectomy and interbody fusion were performed concurrently with resection of the extradural and sacral components. XRT was administered to the lumbosacral area and retroperitoneum. Two years later, an MRI disclosed an 8.0 × 7.0 × 5.5 cm recurrent tumor involving both sacra. A 2.0-cm right lung nodule presumed to be a metastatic lesion was also detected. The patient died from systemic disease following aggressive chemotherapy. Histopathologic examination revealed atypical epithelioid cells, melanin-like pigment interspersed between fibrovascular tissue, focal calcification, and foreign body type giant cells that were consistent with PMS.
Figure 3.
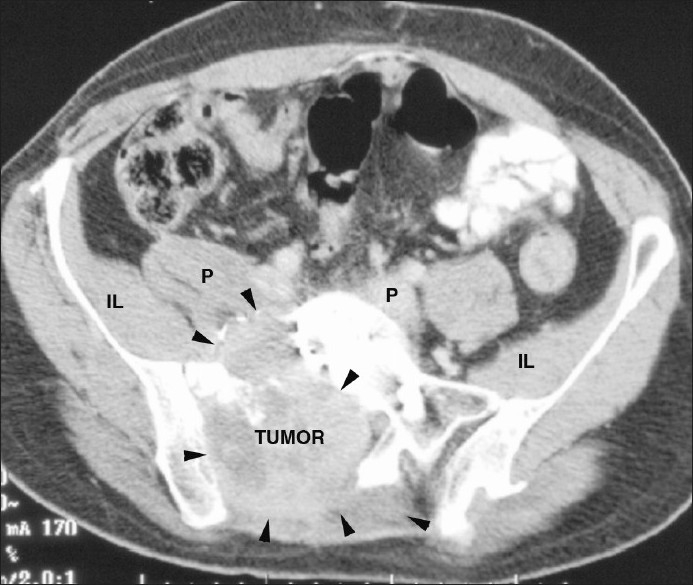
Pelvic CT scan reveals a large tumor mass (black arrowheads) with erosion and destruction of the right sacrum. Retroperitoneal extension of tumor has infiltrated into the right iliacus (IL) and psoas (P) muscles
DISCUSSION
Carney described a syndrome consisting of myxomas (cardiac, cutaneous, and mammary), spotty pigmentation, endocrine overactivity (Cushing's syndrome and acromegaly),[4] often in conjunction with PMS.[3,24] PMS occur at 22.5 years, a decade younger than the classic melanotic schwannoma.[3,21] Of 338 individuals who have been diagnosed with the Carney complex, 57% were females.[24] These tumors most frequently occur in the cervical and thoracic spine (46%).[5,21] Spinal melanotic schwannomas are usually benign,[1,6,7,10,12,13,17,18,20,26,27] but two cases of psammomatous spinal melanotic schwannomas have been reported.[11,17]
PMS may be cured by wide en bloc resection.[12,13] Without complete resection, local tumor recurrence or malignant transformation and remote metastasis may occur.[2,15,17,26] Aggressive local tumor recurrence following incomplete resection of the PMS occurred in both of our patients. In Case 1, death occurred 20 months following its diagnosis. In Case 2, recurrent tumor presented 1 year following the initial operation, with the patient dying from the effects of systemic disease. En bloc resection was not considered to be an option for either patient because of the intraoperative diagnosis of a malignant melanoma on frozen section.
The differential diagnosis of a melanotic schwannoma includes malignant melanoma, pigmented meningioma and neurofibroma, rhabdomyosarcoma, clear cell soft tissue sarcoma,[3,8] melanotic medulloblastoma, ganglioneuroblastoma, ectomesenchymoma (triton tumor), neurotrophic melanoma, and melanotic neuroendocrine carcinomas and carcinoids.[19]
-
1.
Surgery: The optimal surgical approach is complete tumor resection without aggravating the neurological deficit. Successful outcome depends on 1) grade of malignancy, 2) bone metastasis, and 3) visceral metastasis.[25] With a Tomita prognostic score of 2–3 points, wide or marginal excision for long-term local control is justified if it can be performed with minimal complications;[23] a Tomita score of 4–5 points suggests that marginal or intralesional excision is appropriate; with 6–7 points, only palliative surgery is possible; and nonoperative supportive care is indicated for patients with a prognostic score of 8–10.[25] Both our patients had a Tomita score of 4. Using this classification, intratumoral resection with marginal resection was justified. Dural/intradural involvement makes an en bloc resection problematic.
Would a more aggressive initial resection have improved the clinical outcome? Tumor-free margins in highly aggressive tumors are uncommon in spinal surgery as most oncological spine operations are palliative.[14] Frozen section in our patients initially diagnosed these tumors as malignant melanomas. Efforts were made to obtain a complete intratumor resection, but a complete en bloc resection was not indicated with this presumed diagnosis. Because of the malignant histological appearance of this tumor on frozen section (Tomica grade 4–5), an intralesional decompression and fusion was performed for pain control and to decrease tumor bulk prior to adjuvant therapy.
Preoperative percutaneous CT-guided biopsy was not performed prior to surgical intervention as recommended for tumor staging to determine the surgical strategy.[14,16,22] It is unlikely that preoperative biopsy and en bloc resection would have altered the poor outcome in either patient.
-
2.
Pathology: Melanotic schwannomas (also termed pigmented schwannoma, melanogenic schwannoma, or melanotic nerve sheath tumor) are circumscribed black, brown, blue, or gray tumors on gross examination. Microscopic characteristics of this tumor are (1) spindle and epithelioid shaped cells, (2) spindle cells arranged in whorl formation with occasional nuclear palisading,[3,9] 3) rare mitotic figures, 4) immunoreactivity for S-100 protein and vimentin but not for glial fibrillary acidic protein (GFAP), and 5) occasional periodic acid Schiff (PAS)-positive psammoma bodies and adipose tissue.[3] The PMS in our cases demonstrated an aggressive malignant predisposition. The melanotic schwannoma does not possess Antoni A and B characteristics, but may contain adipose tissue.[21]
-
3.
Pathogenesis and genetics: Associated cardiac, thyroid, and other systemic manifestations may occur in the same patient as PMS, leading to a poor prognosis. Close evaluation of family members should be undertaken to prevent unanticipated potentially catastrophic events. Our two patients and their families were interviewed for other features of the Carney complex, with a suggestion of cardiac disease being obtained only in Case 2.
CONCLUSION
Malignant PMS are rarely encountered by spine surgeons. Total excision with tumor-free margins is recommended for both conventional and psammomatous types.[21] Melanotic schwannomas are usually benign; however, the malignant type tends to metastasize. Our two cases underscore the predisposition for multiple recurrences, necessitating an extensive systemic examination to discern possible metastasis. A search for features associated with PMS is necessary when encountering a patient with this unique tumor.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2011/2/1/136/85609
Contributor Information
Lisa B. E. Shields, Email: LBES@earthlink.net.
Steven D. Glassman, Email: SDG12345@aol.com.
George H. Raque, Email: George.Raque@nortonhealthcare.org.
Christopher B. Shields, Email: cbshields1@gmail.com.
REFERENCES
- 1.Buhl R, Barth H, Hugo HH, Mautner VF, Mehdorn HM. Intracranial and spinal melanotic schwannoma in the same patient. J Neurooncol. 2004;68:249–54. doi: 10.1023/b:neon.0000033491.23654.6c. [DOI] [PubMed] [Google Scholar]
- 2.Burns DK, Silva FG, Forde KA, Mount PM, Clark HB. Primary melanocytic schwannoma of the stomach.Evidence of dual melanocytic and schwannian differentiation in an extra-axial site in a patient without neurofibromatosis. Cancer. 1983;52:1432–41. doi: 10.1002/1097-0142(19831015)52:8<1432::aid-cncr2820520816>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 3.Carney JA. Psammomatous melanotic schwannoma.A distinctive, heritable tumor with special associations, including cardiac myxoma and the Cushing syndrome. Am J Surg Pathol. 1990;14:206–22. [PubMed] [Google Scholar]
- 4.Carney JA, Gordon H, Carpenter PC, Shenoy BV, Go VL. The complex of myxomas, spotty pigmentation, and endocrine overactivity. Medicine (Baltimore) 1985;64:270–83. doi: 10.1097/00005792-198507000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Carrasco CA, Rojas-Salazar D, Chiorino R, Venega JC, Wohllk N. Melanotic nonpsammomatous trigeminal schwannoma as the first manifestation of Carney complex: Case report. Neurosurgery. 2006;59:E1334–5. doi: 10.1227/01.NEU.0000245608.07570.D2. [DOI] [PubMed] [Google Scholar]
- 6.Christensen C. Malignant melanocytic schwannoma.A case report. Acta Chir Scand. 1986;152:385–6. [PubMed] [Google Scholar]
- 7.Erlandson RA. Melanotic schwannoma of spinal nerve origin. Ultrastruct Pathol. 1985;9:123–9. doi: 10.3109/01913128509055494. [DOI] [PubMed] [Google Scholar]
- 8.Erlandson RA, Woodruff JM. Peripheral nerve sheath tumors: An electron microscopic study of 43 cases. Cancer. 1982;49:273–87. doi: 10.1002/1097-0142(19820115)49:2<273::aid-cncr2820490213>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 9.Font RL, Truong LD. Melanotic schwannoma of soft tissues.Electron-microscopic observations and review of literature. Am J Surg Pathol. 1984;8:129–38. doi: 10.1097/00000478-198402000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Gregorios JB, Chou SM, Bay J. Melanotic schwannoma of the spinal cord. Neurosurgery. 1982;11:57–60. doi: 10.1227/00006123-198207010-00012. [DOI] [PubMed] [Google Scholar]
- 11.Janzer RC, Makek M. Intraoral malignant melanotic schwannoma. Ultrastructural evidence for melanogenesis by Schwann's cells. Arch Pathol Lab Med. 1983;107:298–301. [PubMed] [Google Scholar]
- 12.Leger F, Vital C, Rivel J, Benjelloun B, San GF, Guerin J. Psammomatous melanotic schwannoma of a spinal nerve root.Relationship with the Carney complex. Pathol Res Pract. 1996;192:1142–6. doi: 10.1016/S0344-0338(96)80034-3. [DOI] [PubMed] [Google Scholar]
- 13.Lowman RM, Livolsi VA. Pigmented (melanotic) schwannomas of the spinal canal. Cancer. 1980;46:391–7. doi: 10.1002/1097-0142(19800715)46:2<391::aid-cncr2820460230>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 14.Mazel C, Balabaud L, Bennis S, Hansen S. Cervical and thoracic spine tumor management: Surgical indications, techniques, and outcomes. (6, 7).Orthop Clin North Am. 2009;40:75–92. doi: 10.1016/j.ocl.2008.09.008. [DOI] [PubMed] [Google Scholar]
- 15.McGavran WL, 3rd, Sypert GW, Ballinger WE. Melanotic schwannoma. Neurosurgery. 1978;2:47–51. doi: 10.1227/00006123-197801000-00010. [DOI] [PubMed] [Google Scholar]
- 16.McLoughlin GS, Sciubba DM, Wolinsky JP. Chondroma/Chondrosarcoma of the spine. Neurosurg Clin N Am. 2008;19:57–63. doi: 10.1016/j.nec.2007.09.007. [DOI] [PubMed] [Google Scholar]
- 17.Mennemeyer RP, Hallman KO, Hammar SP, Raisis JE, Tytus JS, Bockus D. Melanotic schwannoma. Clinical and ultrastructural studies of three cases with evidence of intracellular melanin synthesis. Am J Surg Pathol. 1979;3:3–10. doi: 10.1097/00000478-197902000-00001. [DOI] [PubMed] [Google Scholar]
- 18.Noubari BA, Chiaramonte I, Magro G, Tropea R, Mancuso P. Spinal malignant melanotic schwannoma. Case report. J Neurosurg Sci. 1998;42:245–9. [PubMed] [Google Scholar]
- 19.Rowlands D, Edwards C, Collins F. Malignant melanotic schwannoma of the bronchus. J Clin Pathol. 1987;40:1449–55. doi: 10.1136/jcp.40.12.1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Santaguida C, Sabbagh AJ, Guiot MC, Del Maestro RF. Aggressive intramedullary melanotic schwannoma: Case report. Neurosurgery. 2004;55:1430. doi: 10.1227/01.neu.0000143617.25417.68. [DOI] [PubMed] [Google Scholar]
- 21.Scheithauer BW, Woodruff JM, Erlandson RA. Schwannoma. In: Rosai J, editor. Schwannoma. Washington, D.C.: Armed Forces Institute of Pathology; 1999. pp. 105–76. [Google Scholar]
- 22.Sciubba DM, Chi JH, Rhines LD, Gokaslan ZL. Chordoma of the spinal column. Neurosurg Clin N Am. 2008;19:5–15. doi: 10.1016/j.nec.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 23.Shimada Y, Hongo M, Miyakoshi N, Kasukawa Y, Ando S, Itoi E, et al. Giant cell tumor of fifth lumbar vertebrae: Two case reports and review of the literature. Spine J. 2007;7:499–505. doi: 10.1016/j.spinee.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 24.Stratakis CA, Kirschner LS, Carney JA. Clinical and molecular features of the Carney complex: Diagnostic criteria and recommendations for patient evaluation. J Clin Endocrinol Metab. 2001;86:4041–6. doi: 10.1210/jcem.86.9.7903. [DOI] [PubMed] [Google Scholar]
- 25.Tomita K, Kawahara N, Baba H, Tsuchiya H, Fujita T, Toribatake Y. Total en bloc spondylectomy. A new surgical technique for primary malignant vertebral tumors. Spine (Phila Pa 1976) 1997;22:324–33. doi: 10.1097/00007632-199702010-00018. [DOI] [PubMed] [Google Scholar]
- 26.Watson JC, Stratakis CA, Bryant-Greenwood PK, Koch CA, Kirschner LS, Nguyen T, et al. Neurosurgical implications of Carney complex. J Neurosurg. 2000;92:413–8. doi: 10.3171/jns.2000.92.3.0413. [DOI] [PubMed] [Google Scholar]
- 27.Zonenshayn M, Edgar MA, Lavyne MH. Removal of a lumbar melanotic schwannoma via the far-lateral approach in a patient with Carney complex.Case report. J Neurosurg. 2000;92:241–5. doi: 10.3171/spi.2000.92.2.0241. [DOI] [PubMed] [Google Scholar]


