Abstract
Background:
Spinal fusion is the most rapidly increasing type of lumbar spine surgery for various lumbar degenerative pathologies. The surgical treatment of lumbar spine degenerative disc disease may involve decompression, stabilization, or arthroplasty procedures. Lumbar disc athroplasty is a recent technological advance in the field of lumbar surgery. This study seeks to determine the clinical impact of anterior lumbar disc replacement on the surgical treatment of lumbar spine degenerative pathology. This is a retrospective assessment of the Nationwide Inpatient Sample (NIS).
Methods:
The NIS was searched for ICD-9 codes for lumbar and lumbosacral fusion (81.06), anterior lumbar interbody fusion (81.07), and posterolateral lumbar fusion (81.08), as well as for procedure codes for revision fusion surgery in the lumbar and lumbosacral spine (81.36, 81.37, and 81.38). To assess lumbar arthroplasty, procedure codes for the insertion or replacement of lumbar artificial discs (84.60, 84.65, and 84.68) were queried. Results were assayed from 2000 through 2008, the last year with available data. Analysis was done using the lme4 package in the R programming language for statistical computing.
Results:
A total of nearly 300,000 lumbar spine fusion procedures were reported in the NIS database from 2000 to 2008; assuming a representative cross-section of the US health care market, this models approximately 1.5 million procedures performed over this time period. In 2005, the first year of its widespread use, there were 911 lumbar arthroplasty procedures performed, representing 3% of posterolateral fusions performed in this year. Since introduction, the number of lumbar spine arthroplasty procedures has consistently declined, to 653 total procedures recorded in the NIS in 2008. From 2005 to 2008, lumbar arthroplasties comprised approximately 2% of lumbar posterolateral fusions. Arthroplasty patients were younger than posterior lumbar fusion patients (42.8 ± 11.5 vs. 55.9 ± 15.1 years, P < 0.0000001). The distribution of arthroplasty procedures was even between academic and private urban facilities (48.5% and 48.9%, respectively). While rates of posterolateral lumbar spine fusion steadily grew during the period (OR 1.06, 95% CI: 1.05-1.06, P < 0.0000001), rates of revision surgery and anterior spinal fusion remained static.
Conclusions:
The impact of lumbar arthroplasty procedures has been minimal. Measured as a percentage of more common lumbar posterior arthrodesis procedures, lumbar arthroplasty comprises only approximately 2% of lumbar spine surgeries performed in the United States. Over the first 4 years following the Food and Drug Administration (FDA) approval, the frequency of lumbar disc arthroplasty has decreased while the number of all lumbar spinal fusions has increased.
Keywords: Artificial disc, lumbar spinal fusion, total disc replacement
INTRODUCTION
The management of lumbar degenerative pathology with surgical treatment continues to increase, accounting for a significant expenditure of health care resources.[14] Spinal fusion surgery is the most rapidly increasing type of lumbar spine surgery. The number of lumbar fusions performed in the United States increased over 113% from 1996 to 2001.[8] While surgical treatments of lumbar pathologies are becoming more common, the clinical impact of the various treatments has been questioned.[10] Significant increases in health care expenditures and technological advances may not correlate with improved patient outcomes.[9] The United States Food and Drug Administration (FDA) approved the Depuy Charité LDR device in 2004 and the Synthes ProDisc device in 2006.
The clinical and economic impact of lumbar disc arthroplasty device introduction in the United States has yet to be determined. It was predicted that arthroplasty procedures in the cervical and lumbar spine could account for nearly 50% of spine stabilization procedures.[20]
The Nationwide Inpatient Sample (NIS) maintained by the Agency for Healthcare Research and Quality (AHRQ) is the largest collection of hospital inpatient care and cost data in the United States, including data from a variety of payers.[1–5] The NIS was developed as part of the Healthcare Cost and Utilization Project (HCUP), a federal, state, and industry partnership sponsored by the AHRQ. As of 2008, the NIS contains all discharge data from 1056 hospitals located in 42 states, a stratified sample representing approximately 20% of US hospitals.
This study seeks to determine the impact of lumbar arthroplasty on the rate of lumbar spine fusion and to determine the population-based clinical implications of the introduction of lumbar arthroplasty on US patients. Since its introduction, lumbar arthroplasty devices have had a minimal impact on overall rates of lumbar spine surgery in the United States.
MATERIALS AND METHODS
NIS databases were obtained from the AHRQ's Healthcare Cost and Utilization Project. Results were assayed from 2000 through 2008, the last year with available data. Hospitalization patient records were cross-matched by ICD-9 codes for posterior lumbar and lumbosacral fusion (81.08), anterior approach to the lumbar spine and anterior lumbar interbody fusion (ALIF, 81.06), and posterolateral intertransverse process lumbar fusion (81.07). ICD-9 procedure codes for revision fusion surgery in the lumbar and lumbosacral spine were separately assessed (81.36, 81.37, and 81.38).
To assess lumbar arthroplasty, procedure codes 84.60 (insertion and replacement of artificial discs, NOS), 84.65 (insertion and replacement of lumbar and lumbosacral total artificial disc prosthesis), and 84.68 (removal of partial or total lumbosacral spinal disc prosthesis with synchronous insertion of new spinal disc prosthesis and repair of previously inserted lumbosacral spinal disc prosthesis) were queried. Results were imported into a MySQL database for querying. Analysis was done using the lme4 package in the R programming language for statistical computing, R version 2.11.0 and lme4 version 0.999375-33, both available under the GNU public license (http://www.cran.r-project.org.)
RESULTS
From 2000 to 2008, there were 292,780 index lumbar spinal fusions reported in the AHRQ NIS database, with 18,825 revision surgeries. Assuming a representative sampling provided by the NIS, this sample represents over 1.5 million spine fusion procedures performed over the 9 years assessed. Over the same time period, there were 56,049 anterior lumbar fusions noted in the database.
Lumbar arthroplasties were first reported in the NIS in 2004. From 2005 to 2008, there were a total of 2890 standalone arthroplasty procedures performed, and 60 additional procedures with a combination of arthroplasty and arthrodesis were noted. The average age of arthroplasty patients was 42.8 (SD ±11.5) years, younger than the average reported for posterior lumbar fusion (55.9 ± 15.1 years, P < 0.0000001) or ALIF procedures (48.6 ± 13.4 years, P < 0.0000001) over the same time period. A majority of patients undergoing arthroplasty procedures were male (52.7%) as opposed to those undergoing ALIF (45.1% male) or posterior lumbar fusion procedures (43.4% male; Figure 1).
Figure 1.
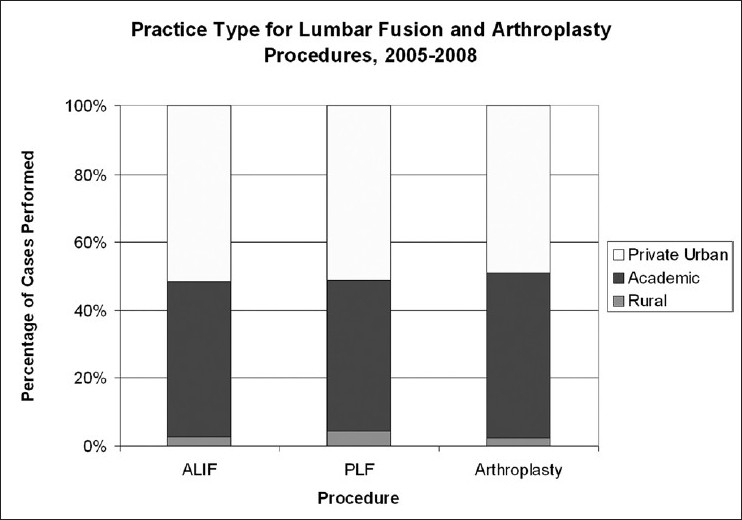
Practice type and choice of operative procedures from 2005 to 2008. The majority of lumbar stabilization and arthroplasty procedures were performed at private urban or academic medical centers
There was a steady growth in lumbar spinal fusion procedures reported in the NIS database from 2000 to 2008 (OR 1.06, 95% CI: 1.05–1.06, P < 0.0000001). Lumbar fusion procedures nearly doubled during this period, from 22,709 procedures in 2000 to 44,366 procedures in 2008. In 2005, the first year of the widespread availability of Charité, 911 lumbar discs arthroplasty procedures were reported in the NIS, in comparison to 34,086 index lumbar spine posterior fusion procedures and 6186 anterior lumbar interbody fusions.
While the number of fusion cases continued to increase until 2008, the number of lumbar arthroplasty operations decreased by 28% over the same period. Figure 2 depicts lumbar arthroplasty as a percent of lumbar posterior fusions performed over the study time period. Lumbar arthroplasty consistently comprised less than 2% of index posterior lumbar spine procedures performed over the period.
Figure 2.
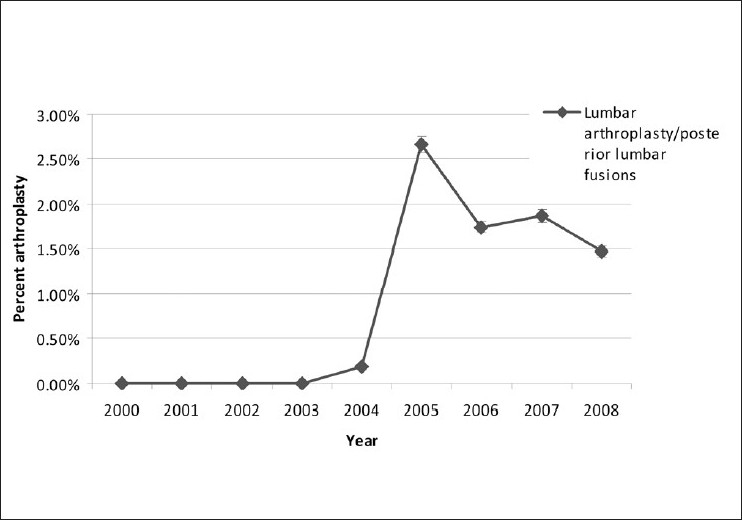
Lumbar arthroplasty as a percentage of posterior lumbar fusion procedures. Lumbar arthroplasty accounts for less than 2% of posteror lumbar fusions performed in the United States
Over the period assessed, the number of revision surgeries remained static, while the number of index surgeries grew significantly [Figure 3]. The number of anterior spinal fusion cases remained stable relative to the total number of spinal fusion procedures, accounting for a consistent average of 19% of spinal fusion procedures over the 9-year study period.
Figure 3.
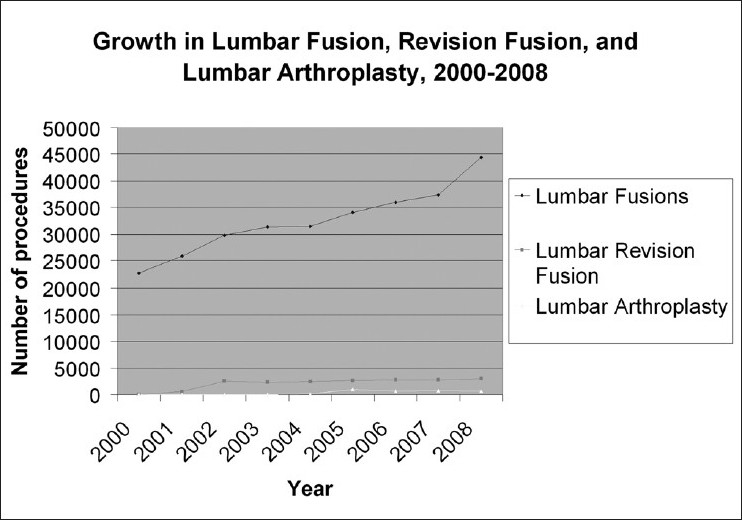
The steady growth in lumbar fusion procedures, with steady rates of lumbar revision and arthroplasty procedures
DISCUSSION
The advantage of lumbar arthroplasty over conventional fusion is its potential to preserve joint motility.[27] Proponents of arthroplasty argue that eliminating the need for an arthrodesis procedure may decrease the risk of adjacent segment disease and may limit some of the late complications of fusion surgery. It was anticipated that the introduction of lumbar arthroplasty techniques would herald a transformation of lumbar spinal surgery from posterior, arthrodesis procedures to anterior, motion preservation approaches.[23]
Surgery for degenerative disc disease
Degenerative disease is the most common surgical indication for low back pain surgery in the United States.[1] The most common surgical approach for this condition has been spinal fusion, which involves removing diseased discs and using bone graft, autograft, allograft, or synthetic graft to stabilize the spine. Over 150,000 lumbar fusion surgeries are performed in the United States alone every year.[7,8] The rate of lumbar fusion increased, especially in the 1990s, following the availability of new surgical implants for spinal fusion.[8,12]
Lumbar disc arthroplasty
The Charité artificial disc achieved an FDA approval for spinal arthroplasty in patients aged 18–60 with degenerative disc disease at one level from L4–S1. Prodisc-L was approved in the same age group from L3–S1. The FDA IDE trial of the Charité artificial disc was the first prospective, randomized, controlled, multicenter study of two different surgical treatments for degenerative disc disease of the spine.
Since the FDA approval of these agents, early experience with lumbar arthroplasty has been mixed.[6,11,18,21,26] Limited long-term follow-up studies demonstrate high rates of revision surgery, explantation surgery, and secondary fusions, although these complications may be linked to incorrect preoperative indications or suboptimal operative technique.[13,25]
RESULTS
The impact of lumbar arthroplasty upon the overall spine market has been limited, with lumbar disc arthroplasty comprising less than 2% of lumbar spine stabilization procedures performed in the United States from 2005 to 2008. The same time period has seen a steady increase in the number of spine fusion procedures performed.[8]
Challenges to the adoption of lumbar arthroplasty
Growth of lumbar disc arthroplasty in the United States has been slow since the FDA approval of lumbar arthroplasty agents. Clinical trials and follow-up studies of the use of lumbar arthroplasty have shown that these devices are not inferior when compared with the standard spinal fusion practices. The limited eligibility of patients, the lack of long-term clinical outcomes after TDA, the unfamiliarity of neurosurgeons and orthopedic surgeons with the devices, the absence of health insurance support, and the popularity of spinal fusion techniques may be some reasons that contribute to the poor adoption of lumbar arthroplasty.
It is unclear if the addition of more arthroplasty agents will favor lumbar disc replacement surgeries. A recent report described 18 lumbar disc arthroplasty designs pending an FDA approval.[16] New implant devices are expected to offer an improved design with an improved stability and less invasive implantation. The clinical impact of the introduction of new approaches to lumbar arthroplasty is similarly unknown.[17]
The rigid eligibility criteria of the FDA IDE trial might contribute to the slow adoption of lumbar arthroplasty devices. Simmons et al. noted that of 252 patients who underwent lumbar surgeries, only about 16 patients, 6.3%, were potential candidates for disc replacement surgery.[19] The lack of a clear revision strategy is another challenge facing anterior arthroplasty procedures. Fear over the risks involved in the case of a revision retroperitonal approach may limit enthusiasm for anterior approaches to lumbar disc replacement.[22]
A recent survey study involving orthopedic and neurosurgical spine surgeons revealed a decreasing interest in lumbar arthroplasty when compared with cervical arthroplasty. The lack of enthusiasm was attributed to questions concerning long-term outcomes and perceived difficulties in obtaining financial compensation from insurance companies.[24]
The adoption of lumbar disc arthroplasty might have been limited by the lack of payer coverage for the procedure. Age limitations in the initial clinical trials led to a noncoverage decision by the Center for Medicare Services (CMS) for this technology.[15] Although the majority of patients in the Medicare age group would not be appropriate candidates for the TDA technology, this decision was followed by similar noncoverage decisions by many private insurance organizations, making it difficult to obtain coverage even for appropriate candidates for disc arthroplasty.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2011/2/1/139/85980
Contributor Information
Olatilewa O. Awe, Email: Olatilewa.Awe@jefferson.edu.
Mitchel G. Maltenfort, Email: mxm974@jefferson.edu.
Srinivas Prasad, Email: srinivas.prasad@jefferson.edu.
James S. Harrop, Email: james.harrop@jefferson.edu.
John K Ratliff, Email: john.ratliff@jefferson.edu.
REFERENCES
- 1.Auerbach JD, Wills BP, McIntosh TC, Balderston RA. Evaluation of spinal kinematics following lumbar total disc replacement and circumferential fusion using in vivo fluoroscopy. Spine (Phila Pa 1976) 2007;32:527–36. doi: 10.1097/01.brs.0000256915.90236.17. [DOI] [PubMed] [Google Scholar]
- 2.Beaule PE, Matta JM, Mast JW. Hip arthrodesis: Current indications and techniques. J Am Acad Orthop Surg. 2002;10:249–58. doi: 10.5435/00124635-200207000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Blumenthal S, McAfee PC, Guyer RD, Hochschuler SH, Geisler FH, Holt RT, et al. A prospective, randomized, multicenter food and drug administration investigational device exemptions study of lumbar total disc replacement with the CHARITE artificial disc versus lumbar fusion: Part I: Evaluation of clinical outcomes. Spine (Phila Pa 1976) 2005;30:1565–75. doi: 10.1097/01.brs.0000170587.32676.0e. discussion E387-91. [DOI] [PubMed] [Google Scholar]
- 4.Buttermann GR, Garvey TA, Hunt AF, Transfeldt EE, Bradford DS, Boachie-Adjei O, et al. Lumbar fusion results related to diagnosis. Spine (Phila Pa 1976) 1998;23:116–27. doi: 10.1097/00007632-199801010-00024. [DOI] [PubMed] [Google Scholar]
- 5.Cahill KS, Chi JH, Day A, Claus EB. Prevalence, complications, and hospital charges associated with use of bone-morphogenetic proteins in spinal fusion procedures. JAMA. 2009;302:58–66. doi: 10.1001/jama.2009.956. [DOI] [PubMed] [Google Scholar]
- 6.Cinotti G, David T, Postacchini F. Results of disc prosthesis after a minimum follow-up period of 2 years. Spine (Phila Pa 1976) 1996;21:995–1000. doi: 10.1097/00007632-199604150-00015. [DOI] [PubMed] [Google Scholar]
- 7.Davis H. Increasing rates of cervical and lumbar spine surgery in the United States, 1979-1990. Spine (Phila Pa 1976) 1994;19:1117–23. doi: 10.1097/00007632-199405001-00003. discussion 1123-4. [DOI] [PubMed] [Google Scholar]
- 8.Deyo RA, Gray DT, Kreuter W, Mirza S, Martin BI. United states trends in lumbar fusion surgery for degenerative conditions. Spine (Phila Pa 1976) 2005;30:1441–5. doi: 10.1097/01.brs.0000166503.37969.8a. discussion 1446-7. [DOI] [PubMed] [Google Scholar]
- 9.Deyo RA, Mirza SK. The case for restraint in spinal surgery: Does quality management have a role to play? Eur Spine J. 2009;18(Suppl 3):331–7. doi: 10.1007/s00586-009-0908-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Deyo RA, Mirza SK, Martin BI, Kreuter W, Goodman DC, Jarvik JG. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA. 2010;303:1259–65. doi: 10.1001/jama.2010.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guyer RD, Siddiqui S, Zigler JE, Ohnmeiss DD, Blumenthal SL, Sachs BL, et al. Lumbar spinal arthroplasty: Analysis of one center's twenty best and twenty worst clinical outcomes. Spine (Phila Pa 1976) 2008;33:2566–9. doi: 10.1097/BRS.0b013e318185941a. [DOI] [PubMed] [Google Scholar]
- 12.Harris IA, Dao AT. Trends of spinal fusion surgery in Australia: 1997 to 2006. ANZ J Surg. 2009;79:783–8. doi: 10.1111/j.1445-2197.2009.05095.x. [DOI] [PubMed] [Google Scholar]
- 13.Ma YZ, Xue HB, Chen X, Guo LX, Li HW, Liu HR. The mid- or long-term clinical results of prosthetic disc nucleus replacement in the treatment of lumbar disc disease. Zhonghua Wai Ke Za Zhi. 2008;46:350–3. [PubMed] [Google Scholar]
- 14.Martin BI, Deyo RA, Mirza SK, Turner JA, Comstock BA, Hollingworth W, et al. Expenditures and health status among adults with back and neck problems. JAMA. 2008;299:656–64. doi: 10.1001/jama.299.6.656. [DOI] [PubMed] [Google Scholar]
- 15.National Coverage Determination (NCD) for Lumbar Artificial Disc Replacement (LADR) (150.10): Centers for Medicare and Medicaid Services. National coverage determination for lumbar artificial disc replacement. 2009 [PubMed] [Google Scholar]
- 16.Orr RD, Postak PD, Rosca M, Greenwald AS. The current state of cervical and lumbar spinal disc arthroplasty. J Bone Joint Surg Am. 2007;89(Suppl 3):70–5. doi: 10.2106/JBJS.G.00396. [DOI] [PubMed] [Google Scholar]
- 17.Pimenta L, Oliveira L, Schaffa T, Coutinho E, Marchi L. Lumbar total disc replacement from an extreme lateral approach: Clinical experience with a minimum of 2 years’ follow-up. J Neurosurg Spine. 2011;14:38–45. doi: 10.3171/2010.9.SPINE09865. [DOI] [PubMed] [Google Scholar]
- 18.Siepe CJ, Mayer HM, Heinz-Leisenheimer M, Korge A. Total lumbar disc replacement: Different results for different levels. Spine (Phila Pa 1976) 2007;32:782–90. doi: 10.1097/01.brs.0000259071.64027.04. [DOI] [PubMed] [Google Scholar]
- 19.Simmons J. Philadelphia: North American Spine Society; 2005. Inclusion criteria for disc arthroplasty. [Google Scholar]
- 20.Singh K, Vaccaro AR, Albert TJ. Assessing the potential impact of total disc arthroplasty on surgeon practice patterns in North America. Spine J. 2004;4:195S–201. doi: 10.1016/j.spinee.2004.07.009. [DOI] [PubMed] [Google Scholar]
- 21.Tumialan LM, Ponton RP, Garvin A, Gluf WM. Arthroplasty in the military: A preliminary experience with ProDisc-C and ProDisc-L. Neurosurg Focus. 2010;28:E18. doi: 10.3171/2010.1.FOCUS102. [DOI] [PubMed] [Google Scholar]
- 22.Van Ooij A, Oner FC, Verbout AJ. Complications of artificial disc replacement: A report of 27 patients with the SB CHARITE disc. J Spinal Disord Tech. 2003;16:369–83. doi: 10.1097/00024720-200308000-00009. [DOI] [PubMed] [Google Scholar]
- 23.Weinstein M, Denhoy R, Krishnan A. JP Morgan: North American Equity Research; 2003. Disruptive medical technologies. The next big thing in spine. [Google Scholar]
- 24.Whang PG, Simpson AK, Rechtine G, Grauer JN. Current trends in spinal arthroplasty: An assessment of surgeon practices and attitudes regarding cervical and lumbar disk replacement. J Spinal Disord Tech. 2009;22:26–33. doi: 10.1097/BSD.0b013e3181659804. [DOI] [PubMed] [Google Scholar]
- 25.Wiedenhofer B, Ewerbeck V, Suda AJ, Carstens C. [Current short- and long-term results of lumbar disc replacement: Update 2008] Chirurg. 2008;79:937–43. doi: 10.1007/s00104-008-1519-5. [DOI] [PubMed] [Google Scholar]
- 26.Zeegers WS, Bohnen LM, Laaper M, Verhaegen MJ. Artificial disc replacement with the modular type SB CHARITE III: 2-year results in 50 prospectively studied patients. Eur Spine J. 1999;8:210–7. doi: 10.1007/s005860050160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zigler JE. Lumbar spine arthroplasty using the ProDisc II. Spine J. 2004;4:260S–7. doi: 10.1016/j.spinee.2004.07.018. [DOI] [PubMed] [Google Scholar]


