Abstract
BACKGROUND:
Clomiphene citrate is commonly used for ovulation induction in women with anovulatory infertility. However, pregnancy rates with this drug are not as good as ovulation rates. Tamoxifen may be a better choice in some patients who fail to either ovulate or conceive with clomiphene due to its favorable effect on the cervical mucus and endometrium. This study was conducted to evaluate the role of tamoxifen in women with anovulatory infertility and find out the optimum dose needed for achieving the best outcome.
MATERIALS AND METHODS:
160 women attending the infertility clinic and suffering from anovulatory infertility were recruited for the study. Tamoxifen was administered in the dose of 40 mg daily and ovulation monitored. In case of anovulation, the dose was increased to 80 mg daily. Ovulation and pregnancy rates were calculated.
RESULTS:
Twenty-three out of 160 women who received 40 mg of tamoxifen conceived, giving a pregnancy rate of 14.38% and pregnancy rate per ovulatory cycle as 14.94%. 32 out of 80 women who received 80 mg of tamoxifen conceived, giving a pregnancy rate of 40% and pregnancy rate per cycle as 33.68%. This difference in the pregnancy rate between the two groups was statistically significant. 35 women out of 90 with polycystic ovary syndrome (PCOS) became pregnant with a pregnancy rate of 38.8% and 20 out of 70 women with clomiphene citrate failure conceived, giving a pregnancy rate of 28.5%.
CONCLUSIONS:
Tamoxifen is a good alternative to clomiphene in women with PCOS and clomiphene-resistant cases.
Keywords: Anovulation, clomiphene, induction of ovulation, polycystic ovary syndrome, tamoxifen
INTRODUCTION
Ovulation is the central event in the reproduction cycle. Ovulatory disorders account for 20-25% of all cases of infertility.[1] Successful therapy of anovulation is one of the most dramatic advances in infertility management. Clomiphene citrate (CC) is the most widely used pharmacological preparation among the ovulation-inducing drugs. Pregnancy rate with CC is 30-40% which is not as good as the ovulation rate (70-80%).[2] The disparity between ovulation and pregnancy rates is most probably due to antiestrogenic action of CC on the endometrium or its interference with the functioning of the corpus luteum. Gonadotrophins have been used in cases of clomiphene failure but these are very expensive and can lead to hyperstimulation, thus needing close supervision and monitoring.
Tamoxifen (Tx), another antiestrogenic compound very similar to CC in structure has been evaluated as a fertility agent in the recent past. With limited literature on the use of Tx for ovulation induction, ovulation rates have been reported as 50-90% and pregnancy rates as 30-50%.[3–5] Tamoxifen has shown reasonably good results in CC failure cases too.[3] The better ovulation and pregnancy rates may be because of higher score of cervical mucus and better functioning of the corpus luteum.[3,6] It does not cause hyperstimulation and multiple pregnancies and is cheap. The present study has been carried out to find out the efficacy of the drug for inducing ovulation and achieving pregnancy in women with polycystic ovary syndrome (PCOS) and clomiphene failure.
MATERIALS AND METHODS
One hundred and sixty women suffering from infertility due to anovulation or oligoovulation were recruited for study from the infertility clinic of Nehru Hospital attached to the Post Graduate Institute of Medical Education and Research. A detailed evaluation of the patients was done. It included history-taking, clinical examination of both the partners, baseline investigations, endometrial biopsy, hysterosalpingography, semen analysis and laparoscopy if required. Diagnosis of anovulation was made on the basis of two or more of the following parameters: Oligomenorrhoea/amenorrhoea with positive progesterone withdrawal, endometrial biopsy in premenstrual phase showing proliferative endometrium, and ultrasonographic evidence of polycystic ovaries or absence of dominant follicle on Day 11 of cycle. Clomiphene failure was defined as failure to ovulate with 150 mg of CC. Women with infertility due to causes other than anovulation were excluded.
Tamoxifen 40 mg (20 mg twice a day) was given from Day 5-9 of the menstrual cycle in the first cycle. Monitoring was done by transvaginal ultrasound starting from Day 11 and continued every alternate day till the day of ovulation or Day 20. If ovulation did not occur, the dose of tamoxifen was increased to 80 mg (40 mg twice a day).
Monitoring
Ultrasound was done from Day 11 onwards. The occurrence of ovulation was documented by one or more of the following criteria:
Development of dominant follicle ≥17 mm, followed by disappearance,
Reduction in size of dominant follicle by more than 5 mm
A change in the shape and appearance of internal echoes within the follicle
Appearance of free fluid in the pouch of Douglas.
At the same time endometrial thickness was also measured. The participants were allowed to pursue natural sexual life and no intervention like intra uterine insemination was done.
Statistical analysis
The primary outcome was ovulation rate per cycle and secondary outcome was pregnancy rate per cycle. For the evaluation of statistical significance, Chi-square test was employed. Probability values less than 0.05 were considered significant.
RESULTS
A total of 160 women with anovulatory infertility were recruited for the study. Table 1 shows the demographic features of these women. The age of the women ranged from 21-40 years with the majority between 21–35 years. Duration of infertility varied from 12 to >72 months and majority of the women had primary infertility.
Table 1.
Demographic features of 160 anovulatory women
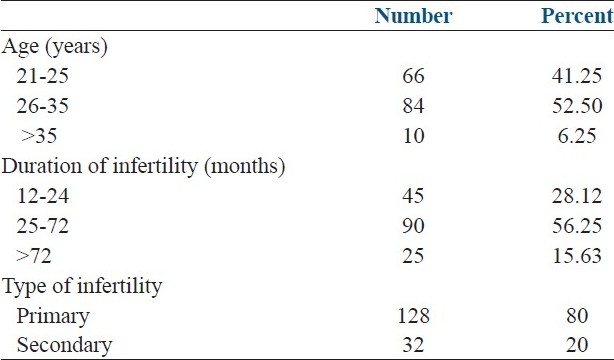
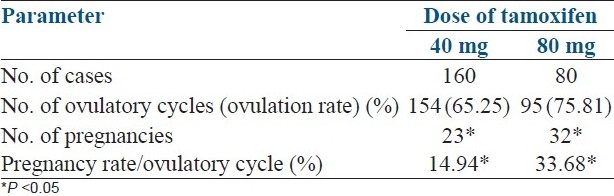
Table 2 shows results of treatment with tamoxifen. One hundred and sixty women received 40 mg of tamoxifen daily and only 80 of them ovulated with this dose. The rest of them received 80 mg of tamoxifen daily. Twenty-three out of 160 women who received 40 mg of tamoxifen conceived, giving a pregnancy rate of 14.38% and the pregnancy rate per ovulatory cycle as 14.94%. Thirty-two out of 80 women who received 80 mg of tamoxifen conceived, giving a pregnancy rate of 40% and pregnancy rate per cycle as 33.68%. This difference in the pregnancy rate between the two groups was statistically significant.
Table 2.
Dose of tamoxifen vs. ovulation and pregnancy rates
Endometrial thickness was more than 8 mm in 60% and 6 mm-8 mm in 30% and more than 10 mm in 10% of women. Endometrial thickness was more than 8 mm in 84% of women who conceived.
35 women out of 90 with PCOS became pregnant with a pregnancy rate of 38.8% and 20 out of 70 women with clomiphene citrate failure conceived, giving a pregnancy rate of 28.5%. There was no statistically significant difference between the two groups.
Tables 3 and 4 show pregnancy rates at different doses of tamoxifen in women with PCOS and who failed to ovulate with clomiphene citrate respectively. In the group with PCOS the ovulation rate with 80 mg was higher than with 40 mg but was not statistically different. Pregnancy rate per ovulatory cycle was significantly higher in the 80-mg group (32.3%) than the 40-mg group (16.5%).
Table 3.
Treatment outcome in women with polycystic ovary syndrome
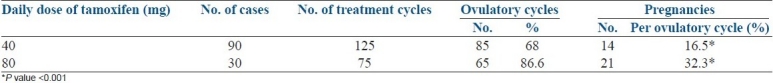
Table 4.
Treatment outcome in women with clomiphene failure
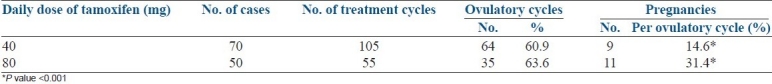
Out of 160 women 70 had already received treatment with clomiphene citrate and were considered as clomiphene failures. Out of the 70 women, 50 required 80 mg of tamoxifen. Nine conceived with 40 mg dosage and 11 became pregnant with 80 mg of tamoxifen. Pregnancy rate per ovulatory cycle was significantly higher in the 80-mg group (31.4%) than the 40-mg group (14.6%).
Out of 55 pregnancies 1 was ectopic and 5 had miscarriage. There was no case of multiple pregnancies.
Women were asked for side-effects. There was no side-effect in the study patients.
DISCUSSION
In the present study, out of 160 women 125 ovulated and 55 of them became pregnant, thus giving a pregnancy rate of 44%. The ovulation rate achieved in this study was 78.1% and out of a total of 360 treatment cycles, 69.2% were ovulatory.
Clomiphene citrate (CC) introduced by Greenblatt et al.[7] is one of the most commonly used agents in this regard. However, pregnancy rates (30-40%) with CC are not as good as ovulation rates (70-80%).[2] The possible explanations given for this discrepancy are that it interferes with functioning of the corpus luteum and has an antiestrogenic action on the cervical glands and the endometrium. Another downside of CC is the controversial suggestion that clomiphene use could be associated with epithelial ovarian cancer.[8] Gonadotrophins have been used as the next choice but these are very expensive, the complication rate is high and they need close supervision and monitoring.
Tamoxifen (Tx), another antiestrogenic compound very similar structure to CC, in use as an anticancer agent has also been evaluated as a fertility agent. The mechanism of tamoxifen in improving folliculogenesis may involve a direct action on the ovary without intervention of hypothalamo-pituitary system as suggested in the studies by Fukushima et al.[9] and Groom Griffith.[10] Tamoxifen also has a beneficial effect on the cervical mucus and the endometrium.[3,11]
Steiner et al., in a meta-analysis concluded that CC and tamoxifen are equally effective in inducing ovulation.[12]
Tamoxifen used for a short duration does not appear to be associated with an increased risk of ovarian or endometrial cancer.[13] The present prospective study was conducted to find out the ovulation and pregnancy rates with different doses of tamoxifen in women with anovulatory infertility.
Williamson et al., reported an ovulation rate of 81% and percentage ovulatory cycles of 63.1 which are comparable to the results of our study.[5] In another study by Messinis et al., the ovulation rate was 76.08% and the percentage ovulatory cycles was 56.2.[14] Comparable pregnancy rates were reported in the study by Williamson et al. Fukushima et al., used tamoxifen in cases of luteal phase defects and reported a pregnancy rate of 35.5%.[9]
The pregnancy rate per ovulatory cycle was 20.1% which was much higher than reported by Suginami et al., which was only 4.8%.[15] The ovulation rate at the dose of 40 mg was 65.25% which was similar to the rate reported by Willamson et al.[5] Gulekli et al., reported an ovulation rate of 70% in cases of polycystic ovarian disease.[16] The pregnancy rate in the present study at the dose of 40 mg was 14.38% which was lower than reported by Williamson et al., and Gulekli et al.[5,16] The ovulation rate at the 80 mg dose was 75.81% and pregnancy rate 40% which are again lower than those reported by Williamson et al., which are 80% and 75% respectively. The pregnancy rates with a higher dose of 80 mg are better than with a 40 mg dose of tamoxifen.
The overall pregnancy rate achieved in cases of polycystic ovarian disease was 38.8% and two-thirds of these pregnancies were achieved with 80 mg dose thus stressing that a higher dose is needed in women with polycystic ovarian disease.
Tamoxifen proved to be quite effective in anovulatory women who failed to ovulate or conceive with CC. The ovulation and pregnancy rate in cases of clomiphene failure was 61.8% and 28.5% respectively. Similar results were reported by Borenstein et al., (pregnancy rate 32.5%).[3]
All the pregnancies were single and none of them had hyperstimulation or any other side-effect.
Williamson et al.[5] and Klopper et al.[17] did report mild side-effects in the form of headache and mild ovarian enlargement.
The present study has shown that tamoxifen is a good ovulation-inducing agent and is devoid of side-effects and complications in women with anovulation. Ghafourzadeh et al.[18] compared clomiphene with clomiphene plus tamoxifen in women with PCOS and showed significantly better ovulation and pregnancy rate with the combination of two drugs.[18] This may be due to the favorable effect of tamoxifen on the endometrium.
Most of the studies, including the meta-analysis by Steiner et al.[12] have shown similar pregnancy rates with clomiphene and tamoxifen. Our study has shown good pregnancy rates in women with clomiphene failure too, thus proving that tamoxifen is a good first-line as well as second-line ovulation-inducing agent.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Rowland M. Infertility therapy. Effect of innovations and increasing experience. J Reprod Med. 1980;25:42–5. [PubMed] [Google Scholar]
- 2.Wu CH. A practical approach to clomiphene therapy. Clin Obstet Gynecol. 1984;27:953–65. doi: 10.1097/00003081-198412000-00016. [DOI] [PubMed] [Google Scholar]
- 3.Borenstein R, Shoham Z, Yemini M, Barash A, Fienstein M, Rozenman D. Tamoxifen treatment in women with failure of clomiphene citrate therapy. Austr NZ J Obstet Gynaecol. 1989;29:173–5. doi: 10.1111/j.1479-828x.1989.tb01711.x. [DOI] [PubMed] [Google Scholar]
- 4.Gulekli B, Ozaksit G, Turhan NO, Senoz S, Oral H, Gokman O. Tamoxifen: An alternative approach in clomiphene resistant polycystic ovarian syndrome patients. J Pak Med Assoc. 1993;43:89–91. [PubMed] [Google Scholar]
- 5.Williamson JG, Ellis JD. The induction of ovulation by tamoxifen. J Obstet Gynecol Brit Commonw. 1973;80:844–7. doi: 10.1111/j.1471-0528.1973.tb11230.x. [DOI] [PubMed] [Google Scholar]
- 6.Roumen ME, Doesburg HW, Rolland R. Treatment of infertile women with a deficient post-coital test with two antiestrogens: Clomiphene and tamoxifen. Fertil Steril. 1984;41:237–43. doi: 10.1016/s0015-0282(16)47597-7. [DOI] [PubMed] [Google Scholar]
- 7.Greenblatt RB, Barfield WE, Jungck CC, Ray AW. Induction of ovulation with MRL/41: Preliminary report. JAMA. 1961;178:101–06. doi: 10.1001/jama.1961.03040410001001. [DOI] [PubMed] [Google Scholar]
- 8.Rossing MA, Daling JR, Weis NS, Moore DE, Self SG, et al. Ovarian tumors in a cohort of infertile women. N Engl J Med. 1994;331:771–6. doi: 10.1056/NEJM199409223311204. [DOI] [PubMed] [Google Scholar]
- 9.Fukushima T, Choshin T, Keizo F, Masao M. Tamoxifen in the treatment of infertility associated with luteal phase deficiency. Fertil Steril. 1982;37:755–61. doi: 10.1016/s0015-0282(16)46334-x. [DOI] [PubMed] [Google Scholar]
- 10.Groom GV, Griffiths K. Effect of the antiestrogen tamoxifen on plasma levels of luteinizing hormone, follicle stimulating hormone, prolactin, estradiol and progesterone in normal premenopausal women. J Endocrinol. 1976;70:421–4. doi: 10.1677/joe.0.0700421. [DOI] [PubMed] [Google Scholar]
- 11.Fukushima T, Maeyama M. Action of tamoxifen on folliculogenesis in the menstrual cycle of infertile patients. Fertil Steril. 1983;40:210–4. doi: 10.1016/s0015-0282(16)47239-0. [DOI] [PubMed] [Google Scholar]
- 12.Steiner AZ, Terplan M, Paulson RJ. Comparison of tamoxifen and clomiphene citrate for ovulation induction: A meta-analysis. Hum Reprod. 2005;20:1511–5. doi: 10.1093/humrep/deh840. [DOI] [PubMed] [Google Scholar]
- 13.Cook LS, Weiss NS, schwartz SM. Population-based study of tamoxifen therapy and subsequent ovarian, endometrial and breast cancers. J Natl Cancer Inst. 1995;87:1359–64. doi: 10.1093/jnci/87.18.1359. [DOI] [PubMed] [Google Scholar]
- 14.Messinis IE, Nillius SJ. Comparison between tamoxifen and clomiphene therapy for induction of ovulation. Acta Obstet Gynaecol Scand. 1982;61:377–9. [PubMed] [Google Scholar]
- 15.Suginami H, Kitagawa H, Nekahashi N, Yano K, Matsubara K. A clomiphene citrate and tamoxifen citrate combination therapy: A novel therapy for ovulation induction. Fertil Steril. 1993;59:976–9. doi: 10.1016/s0015-0282(16)55913-5. [DOI] [PubMed] [Google Scholar]
- 16.Gulekli B, Ozaksit G, Turhan NO, Senoz S, Oral H, Goakman O. Tamoxifen: An alternative approach in clomiphene resistant polycystic ovarian syndrome patients. J Pak Med Assoc. 1993;43:89–91. [PubMed] [Google Scholar]
- 17.Klopper A, Hall M. New synthetic agent for the induction of ovulation: Preliminary trials in women. Br Med J. 1971;1:152–4. doi: 10.1136/bmj.1.5741.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ghafourzadeh M, Karimi M, Karimazadeh MA, Bokai M. Comparison between two methods of ovulation induction: Clomiphene alone and clomiphene + tamoxifen in PCOS patients. Irani J Reprod Med. 2004;2:74–7. [Google Scholar]


