Abstract
BACKGROUND:
The effect of infertility on marital and sexual functioning, health-related quality of life (QoL) and the acceptability of the treatment modalities is a poorly researched area in India.
AIMS AND OBJECTIVES:
To measure and compare the impact of infertility on marital adjustment, sexual functioning, QoL and the acceptability of various treatment modalities in infertility.
DESIGN AND SETTING:
Hospital-based cross-sectional controlled study.
MATERIALS AND METHODS:
Data regarding infertility, socio-demographic characteristics and treatment acceptability was obtained via a semi-structured questionnaire. validated, standardized scales were used to measure marital adjustment (abbreviated dyadic adjustment scale), sexual functioning (abbreviated sexual functioning questionnaire) in cases and controls, and quality of life (FertiQol) in cases. Data from 106 women attending tertiary infertility centers who met the definition of primary infertility and 212 controls attending the medical outpatient department in the same centers was obtained.
RESULTS:
Body mass index and socioeconomic status were significant (P < 0.006 and < 0.0001 respectively) for infertility. Fertility-enhancing regimens and adoption had the highest acceptability with a wide dispersion of range for adoption and least acceptance for sperm, egg, embryo donation and surrogate motherhood. Logistic regression analysis revealed a significant effect size of infertility on marital adjustment (Nagelkerke R2 0.725, Cohen's D 0.86) and sexual functioning (Nagelkerke R2 0.73, Cohen's D 0.815). QoL showed a decrease in mean scores on the FertiQol scale similar to normative data.
CONCLUSIONS:
Effective counseling, reassurance and measures to reduce the impact of the condition on marital and sexual life, overall QoL are needed to impart a holistic treatment in infertility.
Keywords: Infertility, marital adjustment, quality of life, sexual functioning
INTRODUCTION
Infertility, defined by the failure to achieve a clinical pregnancy after twelve months or more of regular unprotected sexual intercourse,[1] not only brings out societal pressures and a psychological burden to achieve procreation, the pinnacle for married couples, it also has a myriad of treatment options for each of its myriad causes, bewildering for most, physically uncomfortable, costly and without a guarantee of success which adds to the impact of the condition making it particularly stressful.
Infertility is known to cause an impact on the mental health of the infertile couple, causing anxiety, depression, social isolation and sexual dysfunction.[2] The triad of the condition, its investigation and treatment, the stigma associated with male and female infertility in traditional societal interactions cause a high level of psychosocial distress with a direct impact on the couple's marital and sexual relations. While several studies have proven this association between the impact of infertility and marriage and sex in couples,[2–5] the unique societal circumstances and cultural settings in India require further investigation into this effect and quantification of the measure of impact.
While the clinical effect and the direct impact of the condition are accurately measured, the subtler effects and multidimensional impact of the condition on holistic health, daily functioning, societal interaction and quality of life (QoL) are often not evaluated while managing the condition. It has been postulated that the brunt of the condition is heavier in women and has more severe emotional and social repercussions than in men.[2,6]
With an estimated overall median global prevalence of 9%,[7] 15% in Indian couples[8,9] and an estimated 56% of these seeking medical care,[7] infertility represents a significant share of the burden on health manpower and healthcare costs. Post intervention, half of these women will eventually conceive while the rest will remain childless.[10] In one-fourth of these women, the etiology for infertility remains unknown in spite of investigation.[11] The cost of treatment remains prohibitive and is a barrier for treatment-seeking in most developing countries in spite of advances in treatment techniques.[10] In a study by Wilkes et al., 50% of infertile couples opted for in vitro fertilization (IVF) and 9% of them achieved pregnancy in one year after multiple attempts.[12]
The current study aimed to establish the distribution of infertility, socio-demographic characteristics in the sample and quantify the impact of the condition on marital, sexual functioning and health-related QoL in women.
MATERIALS AND METHODS
A cross-sectional controlled study was conducted to obtain the socio-demographic characteristics of the sample, duration and baseline data regarding infertility, and to evaluate the impact of infertility on marital adjustment, sexual functioning and QoL using a semi-structured questionnaire with standardized, validated scales. Cases who met the definition of infertility were selected from the outpatient department (OPD) of a teaching hospital (Prathima Institute of Medical Sciences, Karimnagar) and two specialist infertility centers in the same district and age-matched controls were selected among women who had previously conceived and had one living child, attending the medical OPD of the teaching hospital. The study was conducted between January 2010 and April 2010. Pre-testing of the questionnaire was done via a pilot study. The purpose of the study was explained and informed consent was obtained from the respondents. Responses were obtained from the sample via a face-to-face interview after the questionnaire was explained in lay language and recorded by lady house-surgeons who were trained previously in questionnaire administration and interview techniques. Complete privacy and confidentiality was ensured during the process. A total of 106 infertile women who met the definition of primary infertility and 212 controls consented and participated in the study.
Among the socio-demographic characteristics, information was obtained regarding the age of the respondents, duration of married life, duration of attempts for conception, socioeconomic status, literacy, body mass index, habits and occupation of the respondent and spouse. Specific information regarding the type of infertility, obstetrical history, contraceptive history, menstrual history, significant medical history and factors in spouse leading to infertility if any was obtained from the cases.
History regarding treatment sought, the level of specialization of the interventionist, whether faith healing or home remedies were utilized and the duration of treatment were obtained. Cases were asked to rate their attitude towards and acceptability of various treatment modalities, viz. adoption, fertility enhancing regimens, intrauterine insemination, surrogate motherhood, sperm, egg and embryo donation on a five-point Likert scale ranging from strongly disagree to strongly agree. In addition, responses to supportive questions relating to acceptability and dissemination of information to child and society in case of adoption, surrogate motherhood or donation were obtained.
Marital adjustment, sexual functioning was evaluated in both the cases and controls and the QoL was evaluated in cases using standardized, validated scales. Marital adjustment was evaluated using the abbreviated version of the dyadic adjustment scale (ADAS) which is a seven-item questionnaire validated by Sharpley et al.,[13] and Hunsley et al.,[14] and based on the 32-item dyadic adjustment scale by Spanier et al.,[15] It consists of three domains to measure the adjustment and marital accord among couples, namely cohesion with a score range of 1 to 7, consensus with a score range of 3 to 18 and satisfaction with a score range of 3 to 18. The responses are graded on a seven-point Likert scale for the cohesion domain and a six-point scale for the consensus and satisfaction domain. Normal coding was applied to the cohesion and satisfaction domain and reverse coding for the consensus domain during statistical analysis. The total obtainable score ranges from 7 to 43 where a higher score indicates better functioning of relationships.
Sexual functioning was evaluated using the abbreviated sexual functioning questionnaire (ASFQ), a 15-item questionnaire developed and validated by Quirk et al.,[16,17] to measure multiple dimensions of normal sexual functioning with socially appropriate answers. The four domains, desire with a score range of 5 to 30, arousal-sensation with a score range of 0 to 20, lubrication-arousal with a range of 0 to 10 and orgasm 0 to 15, assess desire, lubrication, pain and discomfort with intercourse, emotional stress, pleasure, satisfaction and the ability to achieve orgasm. The responses are graded on an ordinal scale ranging from seven points to five points with lower scores representing poor sexual functioning and higher scores representing good sexual functioning.
QoL was measured in infertile women using FertiQol, an internationally validated and standardized instrument for women experiencing fertility problems. FertiQol is a more sensitive, reliable and valid measure of QoL in infertile women than general measures of QoL such as WHO-BREF and SF-36. It assesses the influence of fertility problems in diverse areas such as self-esteem, emotions, general health, partnership, family and social relationships, work life and future life plans.[18] It consists of 24 items with two additional items to measure overall satisfaction with physical health and QoL. The personal QoL dimension includes two domains, a six-item emotional domain and a six-item mind-body domain. The interpersonal QoL dimension includes a six-item relational domain and a six-item social domain. Responses were obtained on a five-point scale, and the raw score for each domain after appropriate coding for statistical analysis was transformed into scaled scores. The maximum possible scaled score obtainable is 100 representing optimal QoL in comparison to lower scaled scores indicating a lower QoL. A cross-cultural comparison of FertiQol scores is possible with scores from other samples available.
Statistical analysis was done by using Predictive analytics software 18 (PASW), presentation methods included use of box plots and statistical measures obtained were means, confidence intervals, proportions significance test, effect size and logistic regression.
RESULTS
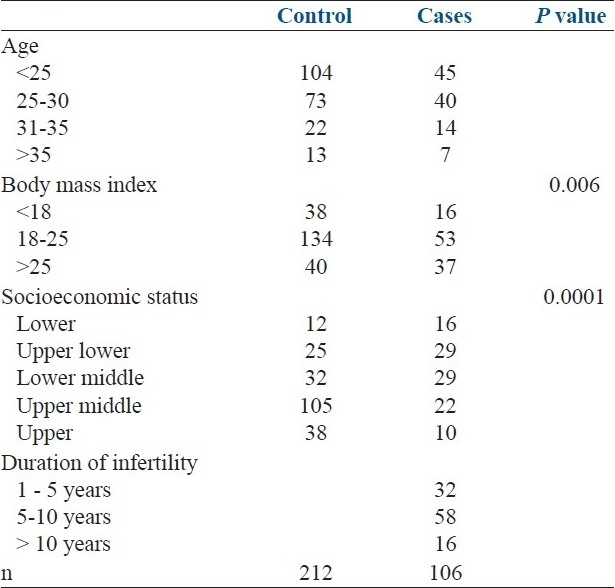
Of the 318 women sampled, 106 met the definition of infertility and 212 controls were obtained from women visiting the same centers. Most infertile women were aged below 25 years (42%), between 25 to 30 years (37%), 30 to 35 (13%) and few were aged above 35 years (6%). The mean age of cases was 26.79 ± 0.76 while the mean age of controls was 25.61 ± 0.70. Among the socio-demographic characteristics evaluated, a higher body mass index and a higher socioeconomic status (based on occupation, literacy and monthly family income – Kuppuswamy scale) were significant for an outcome of infertility with P values of less than 0.006 and 0.0001 respectively on a proportions significance test. The duration of infertility in the sample ranged from 1 to 15 years with a median duration of seven years. This is depicted in Table 1.
Table 1.
Socio-demographic characteristics of the sample
The median number of episodes of intercourse in the control group was 12, and 18 in the cases per month. Infertile women in the sample approached more than one type of practitioner with most women approaching a medical practitioner first followed by referral to a specialist center (88%) and some directly approaching a specialist center (12%). All infertile women in the sample had at one time practiced faith healing and home remedies. Among the various treatment modalities, adoption and fertility-enhancing regimens had the highest acceptance among the sample with a wider distribution of disagreement for adoption than fertility-enhancing drugs. Surrogate motherhood had the least acceptance followed by sperm, egg and embryo donation. This is depicted in Figure 1.
Figure 1.
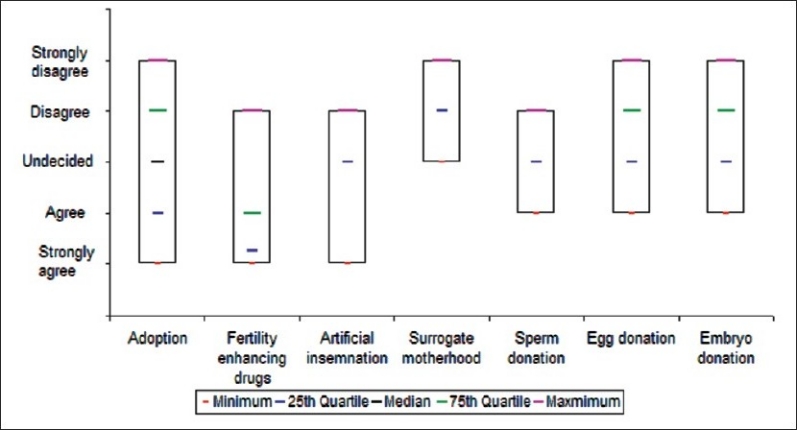
Acceptibility of treatment modalities in infertile women
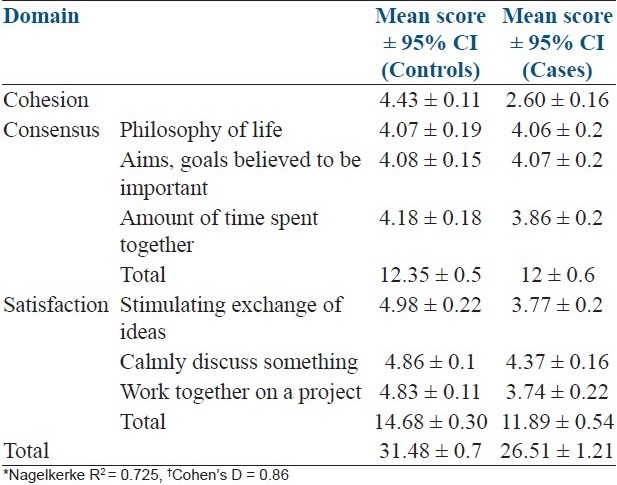
The individual and cumulative mean scores obtained by adding up the individual response scores on the three domains of cohesion, consensus and satisfaction for marital adjustment are presented in Table 2. Marital adjustment scores were impacted more in the infertile group with means scores on the domains of cohesion, consensus and satisfaction being 2.6, 12 and 11.89 and in the controls being 4.43, 12.35 and 14.68 respectively. The most affected domains were cohesion and satisfaction and almost equivocal scores were obtained on the consensus domain. A binomial logistic regression analysis performed on the scores revealed a Nagelkerke R2 score of 0.725 and a Cohen's D of 0.86, close to one, suggesting a strong effect size of infertility on marital adjustment.
Table 2.
Dyadic marital adjustment scores*†
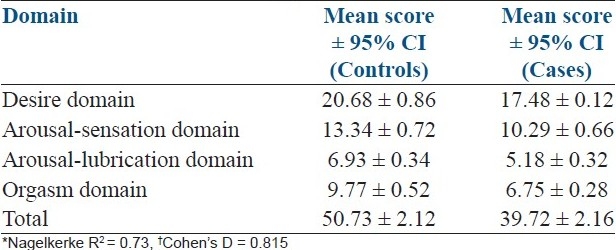
The cumulative mean scores obtained by adding up the individual response scores on the four domains of desire, arousal sensation, arousal lubrication and orgasm for sexual satisfaction are presented in Table 3. The score from the ASFQ showed the largest difference in means in the desire, arousal sensation and orgasm domain with a narrow confidence interval with mean scores of 17.48, 10.29 and 6.75 in the cases and mean scores of 20.68, 13.34 and 9.77 in the controls. There was a smaller difference among the mean scores obtained on the arousal lubrication domain with mean scores of 5.18 and 6.93 among cases and controls respectively. A binomial logistic regression analysis performed on the scores showed a significant value for Nagelkerke R2 of 0.73 and a Cohen's D of 0.815, close to one, implying a strong effect size of infertility on sexual functioning.
Table 3.
Sexual functioning scores*†
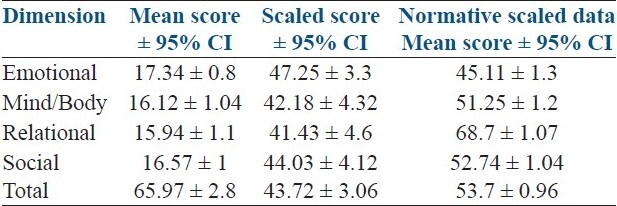
The raw FertiQol scores showed a mean of 17.34, 16.12, 15.94 and 16.57 on the domains of emotional, mind body, relational and social dimensions with a narrow confidence interval of 0.8, 1.04, 1.1 and 1 respectively implying a congruence of impairment of QoL uniformly among the sample in infertile women. The raw scores were transformed to scaled scores for cross-cultural comparisons with international data. These scores are depicted in Table 4.
Table 4.
Infertility quality of life scores
DISCUSSION
The investigation into the varied causes of infertility, the multitude of attempts required and the cost and length of the treatment takes a tremendous toll on the physical and mental health of the woman, which needs to be holistically approached to minimize the burden of the impact of the condition. With several studies examining the causes and treatment modalities for infertility, the effect on health-related QoL and marital and sexual functioning and the acceptability of the treatment modalities is a poorly researched area in India.
The sample in our study contained an equitable distribution of infertile women over the peak childbearing age in India, with ages ranging from 19 to 40, with the number of infertile women decreasing over the age of 35. This may be explained as the sample was obtained from women seeking treatment in specialist infertility centers and attrition of treatment-seeking and acceptance of childlessness may have occurred after multiple attempts with age. A significant association was obtained between rising body mass index and infertility in the cases which is similar to the finding in the study by Mola[19] who found a similar association between being overweight and seeking care for infertility. He postulated a multi-factorial interaction and effect of obesity through endogenous hormones on the hypothalamic-pituitary-ovarian axis leading to anovulatory cycles and the association of obesity with polycystic ovarian disease to explain the relation between body mass index and infertility. A significant association was also obtained between high socioeconomic status and infertility which is similar to the results in the study by Wilcox et al.,[20] which has been explained as a reflection of the socio-demographic profile seeking treatment in specialist infertility clinics and due to the delayed trends of motherhood in high socioeconomic status individuals and associated problems with pregnancy.
The decision for selecting a treatment modality and acceptability among infertile women was evaluated, with fertility-enhancing regimens having the highest acceptability followed by adoption and least acceptance for methods such as sperm, egg, embryo donation and surrogate motherhood. The reasons for lesser acceptance of these methods may not be attributed to societal causes as most infertile women were willing to disclose the genetic non-linkage of the child to society and to a greater extent in their close relatives while to a lesser extent not revealing it to the child. Adoption, however, had varied acceptability implying heterogeneity in the choice. The length of the attempts, physical and emotional travails with lesser amounts of success and the cost of the treatment may play a role in the selection of these modalities. A similar pattern of acceptability was obtained in a study by Sohrabvand et al.,[21] who examined knowledge, attitude, practices and treatment-seeking in infertile couples. Further study is required into the factors playing a role in this decision-making so that the best possible match can be obtained between the patient's needs and available options with a minimal impact on the physical, mental wellbeing and socioeconomic status. A cafeteria-based approach for infertility treatment could be evaluated.
The pressure to conceive, programmed approach to conception, loss of privacy to interventionists and the treatment itself negatively impacts the marital adjustment and sexual functioning among infertile couples as evidenced in the current study where a strong effect size was obtained between infertility and marital adjustment and sexual functioning on validated scales. On the dyadic scale for marital adjustment, the domains affected more severely were the cohesion between couples and satisfaction with marital life, reflecting a strained relationship when compared to the controls. The consensus domain which included an agreement on the philosophy of life, goals and aims and the time spent together had little difference between the groups. On the sexual functioning questionnaire, there was an impact on the mean scores of the desire, arousal-sensation and orgasm domain implying a decreasing want and satisfaction with sexual functioning due to the higher artificial frequency as a result of the need to conceive impacting the health of the sexual relationship. Arousal-lubrication domains remained comparable with a slight difference between the groups indicating a normal physiological response, yet a diminishment in the desire and satisfaction impacting both sexual functioning and thence marital adjustment. Studies by Monga et al., Benazon et al., Lee et al., and Drosdzol et al.,[3,4,22,23] obtained similar results on the dimensions of marital adjustment and sexual functioning in cross-cultural settings with other validated scales implying a congruence of the impact of infertility on both marital adjustment and sexual functioning.
Health-related QoL was measured with the FertiQol instrument which is designed to specifically evaluate QoL in infertile couples. Women in the sample reported dissatisfaction with overall QoL and the scores obtained on the relational domain being maximally impacted followed by mind-body, social and emotional domains when compared to normative data from previous large-scale samples. This impact is congruent with the effect obtained on marital adjustment and sexual functioning which are components of fertility-impacted QoL.[18,24]
Further studies should aim to evaluate the role of the male partner and also the impact of infertility treatment, before and after, on marital, sexual satisfaction and QoL to help the specialist better manage this condition with minimal impact on the related domains of marital life and quality of life.
CONCLUSION
Infertility in women has a varied impact on multiple dimensions of health and functioning such as martial adjustment, sexual functioning and QoL as evidenced by the study. The study also sought the preferred modalities of infertility treatment among women in India. While a large amount of healthcare resources, manpower and research is spent on the investigation and treatment of infertility, lagging behind is essential and complete care of the person as a whole. Effective counseling, reassurance and measures to reduce the impact of the condition on marital and sexual life, overall QoL are needed to impart a holistic treatment in infertility. This can be achieved in conjunction with treatment regimens by clinicians to provide a rounded approach in alleviation of the condition reducing the stress in infertile couples and helping them cope better.
LIMITATIONS
Data was obtained solely on verbal response and the response of the subjects were taken on a ‘as is’ basis. Being a hospital-based study, sample subjects were women who were attending infertility centers for treatment causing a potential bias. The correlation and divergence with regard to the response from male partners was not obtained due to the focus of the study on women and the limited scope of the study which would require further analysis in future studies. Due to the sensitive nature of the questionnaire, in spite of measures to ensure privacy and comfort through utilization of female interviewers, some questions regarding marital life and sexual life may not have obtained accurate responses.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Zegers-Hochschild F, Adamson GD, de Mouzon J, Ishihara O, Mansour R, Nygren K, et al. International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) revised glossary of ART terminology, 2009. Fertil Steril. 2009;92:1520–4. doi: 10.1016/j.fertnstert.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 2.Rashidi B, Montazeri A, Ramezanzadeh F, Shariat M, Abedinia N, Ashrafi M. Health-related quality of life in infertile couples receiving IVF or ICSI treatment. BMC Health Serv Res. 2008;8:186. doi: 10.1186/1472-6963-8-186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Monga M, Alexandrescu B, Katz SE, Stein M, Ganiats T. Impact of infertility on quality of life, marital adjustment, and sexual function. Urology. 2004;63:126–30. doi: 10.1016/j.urology.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 4.Benazon N, Wright J, Sabourin S. Stress, sexual satisfaction, and marital adjustment in infertile couples. J Sex Marital Ther. 1992;18:273–84. doi: 10.1080/00926239208412852. [DOI] [PubMed] [Google Scholar]
- 5.Repokari L, Unkila-Kallio L, Vilska S, Poikkeus P, Sinkkonen J, Almqvist F, et al. Infertility treatment and marital relationships: A 1-year prospective study among successfully treated ART couples and their controls. Hum Reprod. 2007;22:1481–91. doi: 10.1093/humrep/dem013. [DOI] [PubMed] [Google Scholar]
- 6.Chachamovich JR, Chachamovich E, Zachia S, Knauth D, Passos EP. What variables predict generic and health-related quality of life in a sample of Brazilian women experiencing infertility? Hum Reprod. 2007;22:1946–52. doi: 10.1093/humrep/dem080. [DOI] [PubMed] [Google Scholar]
- 7.Boivin J, Bunting L, Collins JA, Nygren KG. International estimates of infertility prevalence and treatment-seeking: Potential need and demand for infertility medical care. Hum Reprod. 2007;22:1506–12. doi: 10.1093/humrep/dem046. [DOI] [PubMed] [Google Scholar]
- 8.Zargar AH, Wani AI, Masoodi SR, Laway BA, Salahuddin M. Epidemiologic and etiologic aspects of primary infertility in the Kashmir region of India. Fertil Steril. 1997;68:637–43. doi: 10.1016/s0015-0282(97)00269-0. [DOI] [PubMed] [Google Scholar]
- 9.Kumar D. Prevalence of female infertility and its socio-economic factors in tribal communities of Central India. Rural Remote Health. 2007;7:456. [PubMed] [Google Scholar]
- 10.Lunenfeld B, Van Steirteghem A. Bertarelli Foundation. Infertility in the third millennium: Implications for the individual, family and society: Condensed meeting report from the Bertarelli Foundation's second global conference. Hum Reprod Update. 2004;10:317–26. doi: 10.1093/humupd/dmh028. [DOI] [PubMed] [Google Scholar]
- 11.Jose-Miller AB, Boyden JW, Frey KA. Infertility. Am Fam Physician. 2007;75:849–56. [PubMed] [Google Scholar]
- 12.Wilkes S, Chinn DJ, Murdoch A, Rubin G. Epidemiology and management of infertility: A population-based study in UK primary care. Fam Pract. 2009;26:269–74. doi: 10.1093/fampra/cmp029. [DOI] [PubMed] [Google Scholar]
- 13.Sharpley CF, Rogers JH. Preliminary validation of the abbreviated Spanier dyadic adjustment scale: Some psychometric data regarding a screening test of marital adjustment. Educ Psychol Meas. 1984;44:1045–9. [Google Scholar]
- 14.Hunsley J, Best M, Lefebvre M, Vito D. The seven-item short form of the dyadic adjustment scale: Further evidence for construct validity. Am J Fam Ther. 2001;29:325–35. [Google Scholar]
- 15.Spanier GB. Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. J Marriage Fam. 1976;38:15–27. [Google Scholar]
- 16.Quirk FH, Heiman JR, Rosen RC, Laan E, Smith MD, Boolell M. Development of a sexual function questionnaire for clinical trials of female sexual dysfunction. J Womens Health Gend Based Med. 2002;11:277–89. doi: 10.1089/152460902753668475. [DOI] [PubMed] [Google Scholar]
- 17.Guay A, Munarriz R, Jacobson J, Talakoub L, Traish A, Quirk F, et al. Serum androgen levels in healthy premenopausal women with and without sexual dysfunction: Part A.Serum androgen levels in women aged 20-49 years with no complaints of sexual dysfunction. Int J Impot Res. 2004;16:112–20. doi: 10.1038/sj.ijir.3901178. [DOI] [PubMed] [Google Scholar]
- 18.European Society of Human Reproduction and Embryology: American Society of Reproductive Medicine (ASRM), and Merck-Serono International. Fertiqol Website. [Last cited on 2010, July 20]. Available at: http://www.fertiqol.org .
- 19.Loret de Mola JR. Obesity and its relationship to infertility in men and women. Obstet Gynecol Clin North Am. 2009;36:333–46. doi: 10.1016/j.ogc.2009.03.002. [DOI] [PubMed] [Google Scholar]
- 20.Wilcox LS, Mosher WD. Use of infertility services in the United States. Obstet Gynecol. 1993;82:122–7. [PubMed] [Google Scholar]
- 21.Sohrabvand F, Jafarabadi M. Knowledge and attitudes of infertile couples about assistedreproductive technology. Iran J Reprod Med. 2005;3:90–4. [Google Scholar]
- 22.Lee TY, Sun GH, Chao SC. The effect of an infertility diagnosis on the distress, marital and sexual satisfaction between husbands and wives in Taiwan. Hum Reprod. 2001;16:1762–7. doi: 10.1093/humrep/16.8.1762. [DOI] [PubMed] [Google Scholar]
- 23.Drosdzol A, Skrzypulec V, Mazur B, Pawlinńska-Chmara R. Quality of life and marital sexual satisfaction in women with polycystic ovary syndrome. Folia Histochem Cytobiol. 2007;45:S93–7. [PubMed] [Google Scholar]
- 24.Wilkins KM, Warnock JK, Serrano E. Depressive symptoms related to infertility and infertility treatments. Psychiatr Clin North Am. 2010;33:309–21. doi: 10.1016/j.psc.2010.01.009. [DOI] [PubMed] [Google Scholar]


