Abstract
Intrathecal baclofen (ITB) has been found to be helpful not only for spasticity but also for unconsciousness in a vegetative patient. This is the first case of ITB in Nepal, and here we discuss the effectiveness of ITB for spasticity in a patient in vegetative state. We also discuss about a simple technique for ITB used in Nepal where baclofen pump is not available. Here, we present a case of a 40-year-old male patient who had severe head injury with diffuse axonal injury treated conservatively. He went on to a vegetative state and subsequently developed severe spasticity of all the limbs. ITB was started under the guidance of one of the authors , Prof. Taira. Baclofen was injected to the spinal intrathecal space through a catheter which is used for spinal anesthesia. Spasticity improved significantly and his higher mental function also showed signs of improvement. He finally became fully conscious and well oriented. ITB is very useful in cases of severe spasticity and vegetative condition, a state of unconsciousness lasting longer than a few weeks. Even with a simple technique in the absence of baclofen pump, ITB can be used with its optimum effect.
Keywords: Intrathecal baclofen, Nepal, spasticity, vegetative state
Introduction
Spasticity is a state when there is an abnormal increase in the muscle tone resulting in muscle spasm and ultimately leading to pain and malfunctioning of the limbs and whole body. It results due to injury to upper motor neurons, mainly pyramidal tract, either in brain or in spinal cord. Stroke, trauma, degenerative lesions, etc. are the examples that can lead to spasticity.
Baclofen, a gamma-aminobutyric acid (GABA) agonist, is an effective muscle relaxant used for spasticity. But it has limitation of inability to cross the blood-brain barrier. Thus, oral administration of baclofen, though helpful in mild spasticity, cannot help in cases of severe intractable spasticity. Moreover, baclofen injected directly to cerebrospinal fluid has fewer side effects than high dose of oral baclofen.
Intrathecal baclofen (ITB) has been found to be very effective in treating spasticity of various causes of spinal as well as cerebral origin.[1,2] It has also been found to be effective in treating spasticity of any cause though the result seems to be poorer with smaller dose in cases of degenerative and demyelinating conditions like multiple sclerosis.[3] Though baclofen is a muscle relaxant, ITB has also been found to be helpful in regaining of consciousness in a vegetative state.[4–6]
The main aim of this article is not only to emphasize the use and effectiveness of ITB, but also to emphasize that ITB can be used effectively with a simple device like intrathecal catheter without any pumping system in underdeveloped countries like Nepal where baclofen pump is not available and is out of reach of poor people.
Case Report
A 40-year-old male patient presented to us with a history of severe head injury in a bus accident while traveling in it. Initial Glasgow Coma Scale (GCS) was about 6/15 with bilateral normal. There was no focal neurological deficit, deep tendon jerks (DTR) were absent in all the limbs and computerized tomography (CT) scan of head was grossly normal without any surgical lesion. Conservative management was started considering the case as diffuse axonal injury (DAI).
Though there was some improvement in neurological status after few weeks, he went on to a vegetative state, i.e. remained unconscious with GCS about 9/15 and without any specific motor and verbal function. He could occasionally open eyes and move limbs spontaneously, but there was no verbal function, no purposeful limb movement, no bowel and bladder control and he did not respond to any verbal command. Finally, he developed generalized spasticity. Considering an appropriate candidate, ITB was planned. Baclofen injection was not available in Nepal and ITB therapy was never used before in this country. Fortunately, Prof. Taira had brought a few ampoules of injection baclofen from Japan and gave them to us as a gift.
But, we did not have baclofen pump and other accessories for ITB. Therefore, an epidural catheter, which is used by an anesthetist for spinal anesthesia or for continuous lumbar drainage [Figure 1], was inserted into the thecal sac at second and third lumbar space and was fixed. The catheter was placed in situ throughout the ITB period and baclofen was injected everyday through it with aseptic precaution. Patency of catheter was confirmed every time before ITB by free flow of cerebrospinal fluid (CSF). We injected 50 μg of baclofen intrathecally everyday for the first 2 weeks and then increased the dose to 100 μg everyday. Oral baclofen was stopped. Patient was placed in lying position during ITB and bedside physiotherapy was continued. In due course of time with ITB, his limbs became less stiff and clonus improved significantly. His higher mental function also showed signs of improvement, and he started producing few words and sounds, followed verbal commands and moved limbs purposefully. Occasionally, he also started showing his emotion in terms of agitation and irritation especially with his family members.
Figure 1.
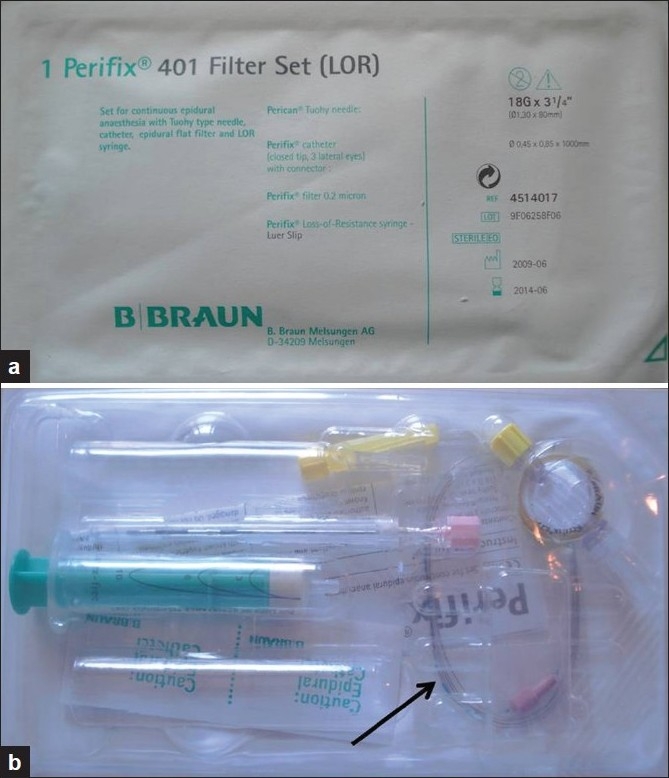
Sample of epidural catheter used for epidural spinal anesthesia: (a) outer cover showing manufacturing company and details of the product; (b) epidural catheter, indicated by arrow, and other accessories
Slowly, we increased physiotherapy, made him sit on wheel chair few times a day, started catheter clamping for his bladder training. His higher mental function improved day by day, could speak a few sentences, followed verbal commands well, and understood and recognized his surroundings and family members. However, we had to stop ITB after about 5 weeks due to CSF leakage through skin puncture site.
By the time he was discharged from the hospital after about 2.5 months of hospital stay, he was fully conscious, i.e. he was well oriented, could speak appropriately and walk with support. He did not have any neurological deficit except for squint due to internuclear ophthalmoplegia that he had developed immediately after trauma and mild spasticity of limbs. Bladder catheter was removed and he could pass urine by himself. He had some behavioral problem, occasionally used to get agitated and violent and also had some psychotic features. Therefore, he was referred to a psychiatrist. Electroencephalogram (EEG) done in 2 months of follow-up was normal.
Discussion
ITB is an established treatment modality for spasticity.[7] However, for that, baclofen pump system is required which is not easily available in developing countries. Since baclofen pump is not available in Nepal, we planned to use a simple technique using an epidural catheter set, by daily injection of baclofen. We found it very simple to inject the required amount of baclofen. We could not find this simple technique mentioned in literature.
ITB has been found to be helpful not only in improving muscle tone and spasticity, but also in improving consciousness in a vegetative patient.[4] Our patient had both spasticity as well as very low consciousness and was in a vegetative state due to severe head injury. Both of these problems seemed to be markedly helped by ITB.
In cerebral palsy, ITB has been found to be very effective in improving higher mental and social function as well.[8] It has also been found to be helpful in improving neurogenic pain, sleep disturbance, sphincter function and dystonia in cerebral palsy.[9–11] Our case also seemed to be benefited significantly in terms of the above neurological symptoms. Literature suggests lack of appropriate explanation for improvement in consciousness level due to ITB.
Though ITB sounds simple, it has a few important complications also. Most common complication has been found to be due to catheter malfunction, followed by procedure-related complications and pump problems.[12] The complication that we encountered in our technique was percutaneous CSF leak which increased the risk of infections like meningitis. Therefore, we had to stop ITB and withdraw the catheter after 5 weeks.
Conclusion
Our case showed significant improvement in spasticity as well as in consciousness level with ITB. Even though we did not have pump system, we could use ITB by a simple technique with effective result. Though it cannot be concluded with mere one case, we strongly suggest that ITB may be helpful for severely head injured patients in a vegetative state with simple intrathecal injection, whenever the pump system is not available.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
References
- 1.Nakajima T, Akagawa H, Ochiai T, Hayashi M, Goto S, Taira T, et al. Intrathecal baclofen therapy for spastic paraparesis due to aortic dissecting aneurysm; recent progress in treatment strategy. Kyobu Geka. 2009;62:1039–42. [PubMed] [Google Scholar]
- 2.Borowski A, Littleton AG, Borkhuu B, Presedo A, Shah S, Dabney KW, et al. Complications of intrathecal baclofen pump therapy in pediatric patients. J Pediatr Orthop. 2010;30:76–81. doi: 10.1097/BPO.0b013e3181c6b257. [DOI] [PubMed] [Google Scholar]
- 3.Saval A, Chiodo AE. Intrathecal baclofen for spasticity management: A comparative analysis of spasticity of spinal vs cortical origin. J Spinal Cord Med. 2010;33:16–21. doi: 10.1080/10790268.2010.11689670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Oyama H, Kito A, Maki H, Hattori K, Tanahashi K. Consciousness recovery induced by intrathecal baclofen administration after subarachnoid hemorrhage -two case reports. Neurol Med Chir. 2010;50:386–90. doi: 10.2176/nmc.50.386. [DOI] [PubMed] [Google Scholar]
- 5.Taira T. Intrathecal administration of GABA agonists in the vegetative state. Prog Brain Res. 2009;177:317–28. doi: 10.1016/S0079-6123(09)17721-X. [DOI] [PubMed] [Google Scholar]
- 6.Sarà M, Pistoia F, Mura E, Onorati P, Govoni S. Intrathecal baclofen in patients with persistent vegetative state: 2 hypotheses. Arch Phys Med Rehabil. 2009;90:1245–9. doi: 10.1016/j.apmr.2009.01.012. [DOI] [PubMed] [Google Scholar]
- 7.Taira T, Ochiai T, Goto S, Hori T. Fifteen year experience of intrathecal baclofen treatment in Japan. Acta Neurochir Suppl. 2006;99:61–3. doi: 10.1007/978-3-211-35205-2_12. [DOI] [PubMed] [Google Scholar]
- 8.Ramstad K, Jahnsen R, Lofterod B, Skjeldal OH. Continuous intrathecal baclofen therapy in children with cerebral palsy - when does improvement emerge? Acta Paediatr. 2010;99:1661–5. doi: 10.1111/j.1651-2227.2009.01596.x. [DOI] [PubMed] [Google Scholar]
- 9.Jagatsinh Y. Intrathecal baclofen: Its effect on symptoms and activities of daily living in severe spasticity due to spinal cord injuries: A pilot study. Indian J Orthop. 2009;43:46–9. doi: 10.4103/0019-5413.45323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Krach LE. Intrathecal baclofen use in adults with cerebral palsy. Dev Med Child Neurol. 2009;51(Suppl 4):106–12. doi: 10.1111/j.1469-8749.2009.03422.x. [DOI] [PubMed] [Google Scholar]
- 11.Taira T, Hori T. Intrathecal baclofen in the treatment of post-stroke central pain, dystonia, and persistent vegetative state. Acta Neurochir Suppl. 2007;97:227–9. doi: 10.1007/978-3-211-33079-1_31. [DOI] [PubMed] [Google Scholar]
- 12.Stetkarova I, Yablon SA, Kofler M, Stokic DS. Procedure- and device-related complications of intrathecal baclofen administration for management of adult muscle hypertonia: A review. Neurorehabil Neural Repair. 2010;24:609–19. doi: 10.1177/1545968310363585. [DOI] [PubMed] [Google Scholar]


