Abstract
There has been explosive growth in the utilization of cross-sectional imaging studies in the evaluation of patients with known or suspected abdominal and pelvic pathology. These imaging studies have led to a veritable epidemic of incidentally detected adnexal masses in both oncology and non-oncology patient populations that in the past remained undiscovered. In this commentary we provide some guidance and practical advice for further investigation and management of the adnexal incidentaloma.
Keywords: Adnexal incidentaloma, multidetector computed tomography, MDCT
Introduction
In the past decade, there has been explosive growth in the utilization of cross-sectional imaging studies in the evaluation of patients with known or suspected abdominal and pelvic pathology. Most conventional genitourinary and gastrointestinal tract studies have been replaced by multidetector computed tomography (MDCT). These imaging studies have led to a veritable epidemic of incidentally detected adnexal masses in both oncology and non-oncology patient populations that in the past remained undiscovered. These incidentalomas (incidental, by coincidence; oma, tumor in Greek) are unexpected, asymptomatic abnormalities that are discovered serendipitously while searching for other pathology or during screening examinations[1].
The detection of these adnexal incidentalomas has created a management dilemma for both clinicians and radiologists, particularly in the oncology patient in whom any mass, clinical or subclinical, warrants further evaluation[2–4]. Subjecting the patient to unnecessary testing and treatment carries its own set of risks that can result in an injurious and expensive cascade of imaging and intervention. The exhaustive evaluation performed in some patients reflects the unwillingness of many physicians to accept diagnostic uncertainty. This unwillingness is in part driven by a paucity of data on the topic, the lack of clear-cut algorithms with regard to diagnostic and treatment strategies, fear of potential malpractice liability, and/or the anxiety of the patient. In this commentary we provide some guidance and practical advice for further investigation and management of the adnexal incidentaloma.
There are four major management pathways for the patient with an adnexal incidentaloma or the indeterminate adnexal mass[5]:
discussion
further investigation (either immediately or after a defined time interval with another imaging test)
intervention (biopsy or surgery)
procrastination (watchful waiting)
The likelihood that the incidentaloma represents a relevant finding rather than a nuisance lesion is determined to a large degree by the patient’s past medical history. There may be a prior gynecologic or non-gynecologic malignancy or complex benign condition such as endometriosis, which can manifest with an adnexal mass. In this scenario, discussion has an important role and for the oncology patient this is optimized in the context of a multidisciplinary team meeting (MDTM). An important additional factor to consider is whether the woman is pre- or postmenopausal, with the risk of a significant abnormality being greater in the latter group.
If the adnexal incidentaloma is of sufficient concern on MDCT, ultrasound (US) should be the next investigation. It is inexpensive, widely available, well tolerated, and in many cases can clarify the nature of the mass. In a pre-menopausal woman there are arguments for performing an interval US assessment after 6 weeks at a different stage of another menstrual cycle. The mass may spontaneously resolve. Some older women are reluctant to undergo transvaginal scanning and in the infirm and overweight patient even transabdominal scanning may be of limited value. In these problematic cases and when US is unable to characterize the incidentaloma, magnetic resonance imaging (MRI) is often diagnostic (Figs. 1 and 2).
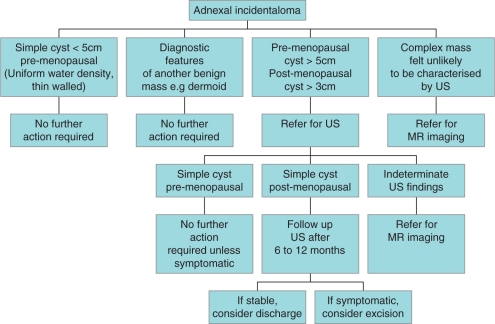
Figure 1.
Management of an adnexal incidentaloma discovered on an MDCT examination.
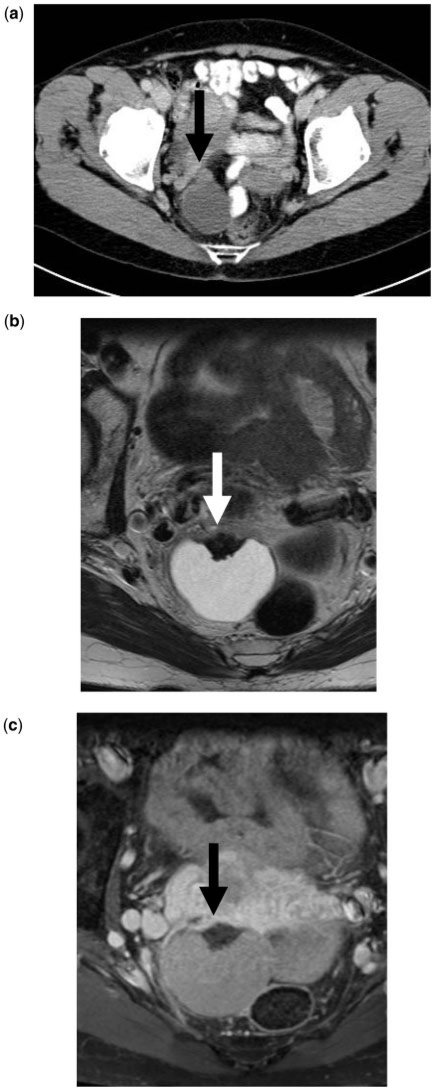
Figure 2.
A right adnexal incidentaloma discovered during investigation of gastrointestinal symptoms using MDCT. (a) CT shows a 2.8-cm cystic right adnexal mass with a nodule in its anterior wall (arrow). (b) T2-weighted axial image shows a well-marginated, cystic, hyperintense, otherwise thin-walled right adnexal mass with a region of markedly reduced signal intensity anteriorly (arrow). (c) T1-weighted, fat suppressed, contrast-enhanced MR scan shows that this lesion has moderately high signal intensity except for the non-enhancing very low signal intensity region seen anteriorly (arrow) probably related to hemosiderin deposition. This is consistent with a benign lesion, such as an old endometrioma.
Intervention should be regarded as the last alternative. Biopsy from a transabdominal route risks rupture of the mass with peritoneal spread of tumor from a malignancy. Laparoscopy is more invasive and subject to similar risks unless direct visualization of the mass or its environs results in a confident diagnosis.
For many years, watchful waiting has been a mainstay in the management of adnexal masses. Indeterminate or difficult to diagnose masses that disappear, become smaller or remain unchanged over time are deemed to be benign or at least to require no active management. Cohort studies have shown that adnexal cysts in postmenopausal women, the group most at risk of ovarian cancer, are far less worrying than was believed in the past[6]. Some 17% of 184 volunteer postmenopausal women had adnexal cysts and in 4 years of prospective follow-up, no woman developed cancer. Most cysts disappeared or remained stable but in that group even enlargement of the cyst was not an indicator of an adverse outcome[6].
Recent guidelines from the Society of Radiologists in Ultrasound (SRU) indicate when and how US follow-up is required and these guidelines stratify risk based on the size of masses and the menopausal status of the woman[7]. Many women with adnexal masses can be reassured that they need no further follow-up and many more can be reassured after one further US examination showing stability or regression of the mass.
The Society of Radiologists in Ultrasound (SRU) guidelines state that[7]:
in women of menstrual age only cysts >3 cm should be mentioned in US reports, that only cysts >5 cm need imaging follow-up and that cysts >7 cm may be better evaluated with MRI;
in postmenopausal women only cysts of >1 cm are mentioned in reports, that cysts of 3–7 cm have follow-up US to confirm stability and again that cysts >7 cm have MRI.
These recommendations also address the imaging management for hemorrhagic cysts, endometriomas and dermoid cysts[7]. The need for follow-up of hemorrhagic cysts can be minimized by using the guidelines: hemorrhagic cysts <5 cm do not need follow-up; follow-up is advised after 6–12 weeks and ideally in the follicular phase on days 3–10 of the menstrual cycle; such a cyst in the postmenopausal women must be regarded with greater suspicion and, although the SRU recommends surgical evaluation, MRI may be able to confidently exclude any neoplastic change within such a cyst.
The major rationale for the follow-up of a hemorrhagic cyst is to assess resolution of the blood products. If the blood products fail to resorb, an ovarian infarct or endometrioma should be considered. Follow-up of an endometrioma and dermoid cyst depends on patient related factors such as pain. Most dermoid tumors can be confidently diagnosed with computed tomography (CT) and an end point is reached (Fig. 3). In some patients, annual US examination is advised[7] but in our view the interval between scans can be lengthened or further examinations become unnecessary when stable features are established. The need for follow-up of these lesions is the rare instance of malignant transformation quoted as 1% and up to 2% for endometrioma and dermoid tumors, respectively.
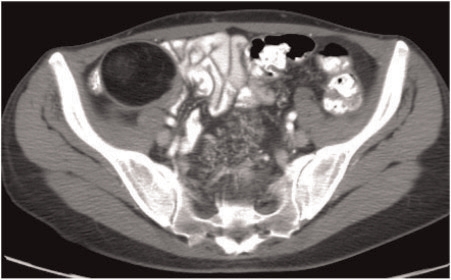
Figure 3.
Right ovarian teratoma. The fat density of this lesion is sufficiently characteristic to establish the diagnosis and no further action is required (Fig. 1).
The SRU consensus statement reconfirms that characteristics worrisome for malignancy are[7]:
thick septations >3 mm
solid elements with flow at Doppler US
focal wall thickening >3 mm
A cyst with a nodule that has internal blood flow has the highest likelihood of being malignant[7].
The SRU guidelines are of enormous benefit but expressly deal with asymptomatic women with a relatively low risk of malignancy. Accordingly, there are some limitations for other patient populations. Their advice relies heavily on procrastination (watchful waiting) as a discriminator. Follow-up in 6–12 weeks does not appropriately address the more complex adnexal incidentaloma, which could represent a metastatic lesion from a malignancy otherwise amenable to radical therapy. When staging investigations reveal such an adnexal mass, MRI can help guide further management (Fig. 1).
Although the utility of MRI has been extensively validated in the evaluation of indeterminate adnexal masses[8–10], no reports concerning its efficacy in the assessment of the adnexal incidentaloma have been published. There are, however, no reasons to believe that MRI would work any less well in that context. There are now widely accepted problem-solving approaches that form the basis of practical guidelines[11,12].
A number of studies over the past two decades have investigated the significance of adnexal incidentalomas in different patient populations[13,14]. In a study of 3448 women examined over 1 year, with wide-ranging indications for abdominopelvic CT, adnexal incidentalomas were commented on in 5% of the reports. The CT evaluations were: 69% benign disease, 30% indeterminate lesion and; 1% malignant lesion. None of these represented primary ovarian cancer. Some of the women were known to have malignant disease. Of the 67 women with known non-gynecological cancer, 46% were considered to have benign disease, 48% undetermined lesions and 3% to have metastases to the ovaries[13]. This study emphasizes the fact the majority of adnexal incidentalomas found on CT, even in patients with known malignancy, are benign. In a similar 3-year retrospective study of 749 women aged over 50 years undergoing the specialized examination of CT colonography (CTC), some 71 (9.5%) had gynecologic abnormalities discovered in a key word retrospective trawl through the imaging reports[14]. Almost half of these were due to fibroid disease (leiomyomata). Because of clinical or radiological concerns 14 women underwent additional radiological or surgical evaluation. No malignancies were found[14].
There have been few longer term outcome studies describing the fate of patients with adnexal incidentalomas found on specialized CT studies. Pickhardt and Hanson[15] describe 118 women aged 50 years and over who had such abnormalities discovered during low-dose unenhanced CTC studies. This represented 4.1% of the study group of 2869 women. For a variety of reasons, 26 of the 118 women underwent surgical excision. All except one woman had a normal CA125 level and none was found to have a malignant adnexal mass. Conversely 4 women among the remaining 2751 who had had normal adnexal appearances on their CT examinations subsequently developed malignant adnexal disease in the 15–44 months follow-up period.
The conclusions from a large and increasing number of studies are encouraging. The vast majority of adnexal incidentalomas found on MDCT investigations of women with or without a known malignancy are benign, even in postmenopausal women. We should not be surprised by this as before the use of cross-sectional imaging these lesions went undetected without demonstrable harm. A small minority of these incidentalomas require excision but in the reported literature no primary ovarian cancers were discovered.
In masses discovered on MDCT studies, US has a major role in defining which need follow-up. There are well-defined and easy to follow guidelines for such follow-up[7] and using these guidelines, many fewer adnexal masses need even a mention in the imaging report, let alone any further follow-up (Fig. 1). MRI offers a robust means of evaluation of adnexal incidentalomas that cannot be characterized by US (Figs. 1 and 2).
Footnotes
This paper is available online at http://www.cancerimaging.org. In the event of a change in the URL address, please use the DOI provided to locate the paper.
References
- 1.Berland LL, Silverman SG, Gore RM, et al. Managing incidental findings on abdominal CT: white paper of the ACR Incidental Findings Committee. J Am Coll Rad. 2010;7:754–73. doi: 10.1016/j.jacr.2010.06.013. [DOI] [PubMed] [Google Scholar]
- 2.Xiong T, Richardson M, Woodroffe R, Halligan S, Morton D, Lilford RJ. Incidental lesions found on CT colonography: their nature and frequency. Br J Radiol. 2005;78:22–9. doi: 10.1259/bjr/67998962. . PMid:15673525. [DOI] [PubMed] [Google Scholar]
- 3.Pickhardt PJ, Hanson ME, Vanness DJ, et al. Unsuspected extracolonic findings at screening CT colonography: clinical and economic impact. Radiology. 2008;249:151–9. doi: 10.1148/radiol.2491072148. . PMid:18796673. [DOI] [PubMed] [Google Scholar]
- 4.Katz DS, Scheer M, Lumerman JH, Mellinger BC, Stillman CA, Lane MJ. Alternative or additional diagnoses on unenhanced helical computed tomography for suspected renal colic: experience with 1000 consecutive examinations. Urology. 2000;56:53–7. doi: 10.1016/S0090-4295(00)00584-7. . PMid:10869622. [DOI] [PubMed] [Google Scholar]
- 5.Spencer JA. Indeterminate lesions in cancer imaging. Clin Radiol. 2008;63:843–52. doi: 10.1016/j.crad.2007.11.025. . PMid:18625347. [DOI] [PubMed] [Google Scholar]
- 6.Levine D, Gosink BB, Wolf IS, et al. Simple adnexal cysts: the natural history in postmenopausal women. Radiology. 1992;184:653–9. doi: 10.1148/radiology.184.3.1509047. PMid:1509047. [DOI] [PubMed] [Google Scholar]
- 7.Levine D, Brown DL, Andreotti RF, et al. Management of asymptomatic ovarian and other adnexal cysts imaged at US: Society of Radiologists in Ultrasound Consensus Conference Statement. Radiology. 2010;256:943–54. doi: 10.1148/radiol.10100213. . PMid:20505067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sohaib SA, Mills TD, Sahdev A, et al. The role of magnetic resonance imaging and ultrasound in patients with adnexal masses. Clin Radiol. 2005;60:340–8. doi: 10.1016/j.crad.2004.09.007. . PMid:15710137. [DOI] [PubMed] [Google Scholar]
- 9.Adusumilli S, Hussain HK, Caoili EM, et al. MRI of sonographically indeterminate adnexal masses. Am J Roentgenol. 2006;187:732–40. doi: 10.2214/AJR.05.0905. [DOI] [PubMed] [Google Scholar]
- 10.Kinkel K, Lu Y, Mehdizade A, Pelte MF, Hricak H. Indeterminate ovarian mass at US: incremental value of second imaging test for characterization–meta-analysis and Bayesian analysis. Radiology. 2005;236:85–94. doi: 10.1148/radiol.2361041618. . PMid:15955864. [DOI] [PubMed] [Google Scholar]
- 11.Spencer JA, Forstner R, Cunha TM, Kinkel K on behalf of the ESUR Female Imaging Sub-Committee. ESUR guidelines for MR imaging of the sonographically indeterminate adnexal mass: an algorithmic approach. Eur Radiol. 2010;20:25–35. doi: 10.1007/s00330-009-1584-2. . PMid:20069737. [DOI] [PubMed] [Google Scholar]
- 12.Spencer JA, Ghattamaneni S. MR imaging of the sonographically indeterminate adnexal mass. Radiology. 2010;256:677–94. doi: 10.1148/radiol.10090397. . PMid:20720065. [DOI] [PubMed] [Google Scholar]
- 13.Slanetz PJ, Hahn PF, Hall DA, et al. The frequency and significance of adnexal lesions incidentally revealed by CT. Am J Roentgenol. 1997;168:647–50. doi: 10.2214/ajr.168.3.9057508. [DOI] [PubMed] [Google Scholar]
- 14.Stitt IA, Stany MP, Moser RP, 3rd, et al. Incidental gynecological findings on computed tomographic colonography: prevalence and outcomes. Gynecol Oncol. 2009;115:138–41. doi: 10.1016/j.ygyno.2009.05.016. . PMid:19500823. [DOI] [PubMed] [Google Scholar]
- 15.Pickhardt PJ, Hanson ME. Incidental adnexal masses on low-dose CT colonography in asymptomatic women ≥50. Radiology. 2010;257:144–50. doi: 10.1148/radiol.10100511. . PMid:20663974. [DOI] [PubMed] [Google Scholar]