Abstract
Objective
To compare the type and degree of impulsivity among adolescents with bipolar disorder (BD), adolescents with attention-deficit/hyperactivity disorder (ADHD), and healthy comparison subjects using the Barratt Impulsiveness Scale, Version 11 (BIS-11).
Methods
Manic adolescents with BD (n=31), adolescents with ADHD (n=30), and healthy subjects (n=25) completed the BIS-11, a 30-item, self-report scale with three subscales (cognitive, motor, and nonplanning). The BIS-11 total and subscale scores were compared among groups. We also examined associations among the BIS-11, Young Mania Rating Scale and co-occurring disruptive behavioral disorders (DBDs) within the BD group.
Results
Total and each subscale scores were significantly higher for the BD group than for the healthy controls (p<0.05). The total scores and the cognitive and motor subscale scores were significantly higher for the ADHD group than for the healthy control group (p<0.05). However, there was no statistically significant difference between the nonplanning subscale scores of the ADHD group and the healthy control group (p>0.05). There were no significant differences between the BD and ADHD groups or between the BD groups with and without ADHD. The BD patients with DBDs (i.e., oppositional defiant disorder or conduct disorder) scored significantly higher on the motor subscale than did BD patients without DBDs. There were no statistically significant associations between the Young Mania Rating Scale and BIS-11 scores within the BD group.
Conclusion
Our findings suggest that impulsivity is elevated in adolescents with BD as well as adolescents with ADHD, except for nonplanning impulsivity, which was not significantly different between adolescents with ADHD and the healthy comparison group. This may suggest that nonplanning impulsivity is relatively specific to adolescents with BD. Additionally, our data indicate that elevations in impulsivity, as measured by the BIS-11, may be independent of symptoms severity and, therefore, may be a stable, trait-related component of BD.
Introduction
Impulsivity is a complex, multifaceted construct with behavioral and cognitive manifestations. It is a key feature of a number of psychiatric disorders, such as bipolar disorder (BD), attention-deficit/hyperactivity disorder (ADHD), disruptive behavior disorders (DBDs), substance use disorders, and personality disorders; it is also a part of the normal behavior spectrum (Moeller et al. 2001). Clinically, there appear to be differences in the core aspects of impulsivity between these psychiatric disorders. Patients with either ADHD or BD exhibit impulsive behaviors by engaging in dangerous activities, but the types of impulsivity they exhibit may not be similar. For example, patients with BD often crave pleasurable activities, whereas patients with ADHD seek stimulation in any form and do not restrict to pleasurable activities (McBurnett et al. 1993; Evenden 1999; Holmes et al. 2009). However, it is unclear whether the impulsive behaviors seen in youth with BD and ADHD encompass all aspects of impulsivity or are measurably distinct.
One of the commonly used self-rated measures of impulsivity is the Barratt Impulsiveness Scale, Version 11 (BIS-11), which incorporates three behavioral components of impulsivity: motor, which refers to acting on the spur of the moment without thinking; nonplanning, which refers to a lack of future orientation; and cognitive, which refers to issues with concentration and tendency to shift attention rapidly (Patton et al. 1995). Although several studies have examined impulsivity using the BIS-11 in adults with psychiatric disorders, there are few such studies in adolescents (Ray et al. 2005).
With these considerations in mind, the aims of our study were (1) to compare the level and type of impulsivity among adolescents with BD, adolescents with ADHD, and healthy comparison subjects using the BIS-11, and (2) to examine associations among levels of impulsivity with symptoms severity and co-morbid psychiatric disorders in adolescents with BD.
We predicted that both the BD and ADHD groups would score higher than the healthy controls on a self-report measure of impulsivity, the BIS-11. We also predicted that the BD group would score higher on the nonplanning impulsiveness ratings as compared to the ADHD group, whereas the ADHD group would score higher on the motor impulsiveness ratings compared with the BD group, based upon the differences in impulsive behaviors that are observed clinically in these patients (McBurnett et al. 1993; Evenden 1999; Holmes et al. 2009). Additionally, we expected the presence of ADHD and DBDs to increase the level of impulsivity in BD adolescents, as these disorders themselves are associated with increased impulsivity (Moeller et al. 2001).
Methods
Subjects
Adolescents (aged 11–18 years) who met Diagnostic and Statistical Manual of Mental Disorders, 4th edition, Text Revision (DSM-IV-TR) (American Psychiatric Association 2000) criteria for a manic or mixed episode associated with bipolar I disorder (N=31) and adolescents with ADHD without a co-morbid mood or psychotic disorder in themselves or any first-degree relatives (N=30) were recruited from Cincinnati Children's Hospital Medical Center. Demographically matched healthy adolescents (N=25) were recruited from the community in which the patients resided. Within the BD group, 13 (42%) subjects had co-occurring ADHD and 14 (45%) subjects had co-occurring DBDs (i.e., oppositional defiant disorder or conduct disorder; no patient was found to have DBD Not Otherwise Specified). Only two (6.6%) of the patients with ADHD had co-occurring DBDs and only three (9.7%) of the patients with BD had co-occurring anxiety disorders.
Procedures
The subjects provided written assent, and their legal guardians provided written informed consent after study procedures were fully explained. The Washington University in St. Louis Kiddie Schedule for Affective Disorders and Schizophrenia (WASH-U KSADS), a semi-structured diagnostic interview, administered by trained raters with established diagnostic reliability (kappa=0.82–1.00) was used to confirm diagnoses (Geller et al. 1996, 2001, 2002). All study participants were asked to complete the BIS-11. The Young Mania Rating Scale (YMRS) was used to assess severity of mania in the BD group. The YMRS was administered by trained raters with established inter-rater reliability of 0.93 (Young et al. 1978).
Statistical analysis
The total and three subscale scores of the BIS-11 were contrasted among groups. We also contrasted the total and subscale scores between the BD patients with and without ADHD and with and without DBDs. We did not compare the BIS-11 scores between the ADHD patients with and without DBDs due to the small sample size of the group of ADHD patients with co-morbid DBDs. Analysis of variance was used to compare group differences in demographics and clinical variables and the total and subscale scores on the BIS-11. Levine's test for homogeneity was performed to compare the variance of BIS-11 total and subscale scores. Fisher's exact test and chi square analyses were used to measure statistical significance for count/frequency data. Pearson coefficients were calculated to examine associations between the BIS-11 and YMRS scores within the bipolar group. Inferential statistics were assessed at a significance level of α<0.05. Eta-squared and Cohen's d were used to calculate effect sizes for three- and two-group comparisons, respectively (Cohen 1988).
Results
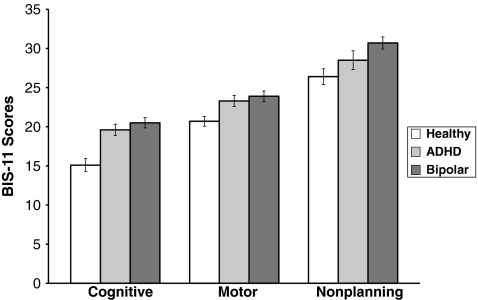
There were no statistically significant differences in demographic characteristics among BD, ADHD, and healthy comparison adolescents (Table 1). The total and subscale scores on the BIS-11 were significantly higher for the BD group than for the healthy control group. The total scores and the cognitive and motor subscale scores on the BIS-11 were significantly higher for the ADHD group than for the healthy control group. However, there was no statistically significant difference between the nonplanning subscale scores of the ADHD group and the healthy control group. There were no statistically significant differences in the total or subscale scores between the BD group and the ADHD group, or between the BD with ADHD group and the ADHD group, or between the BD without ADHD group and the ADHD group. No significant differences were noted between the BD patients with and without ADHD (Tables 2 and 3, Fig. 1). Levine statistics were not statistically significant in any of the three group comparisons, indicating appropriate homogeneity of variance.
Table 1.
Demographic Characteristics of Study Subjects
| Variable | BD (N=31) | ADHD (N=30) | Healthy (N=25) | p Value |
|---|---|---|---|---|
| Age mean (SD), years | 15.3 (1.5) | 14.9 (1.9) | 15.3 (1.7) | 0.53 |
| Sex, n (%) female | 14 (45) | 10 (33) | 11 (44) | 0.73 |
| Race, n (%) white | 22 (71) | 25 (83) | 19 (76) | 0.22 |
BD=bipolar disorder; ADHD=attention-deficit/hyperactivity disorder.
Table 2.
Total and Subscale Scores on Barratt Impulsiveness Scale, Version 11
| BIS-11 scores | BD (N=31)a | ADHD (N=30)a | Healthy (N=25)a | Fb | p< | Partial η2 | Contrasts |
|---|---|---|---|---|---|---|---|
| Cognitive | 20.5 (3.6) | 19.6 (4.0) | 15.1 (4.2) | 14.90 | 0.001 | 0.26 | BD, ADHD>Healthy |
| Motor | 23.9 (3.7) | 23.3 (3.9) | 20.7 (3.2) | 6.08 | 0.01 | 0.13 | BD, ADHD>Healthy |
| Nonplanning | 30.7 (4.3) | 28.5 (6.3) | 26.4 (5.0) | 4.69 | 0.05 | 0.10 | BD>Healthy |
| Total | 75.1 (8.1) | 71.5 (12.1) | 62.1 (10.7) | 11.29 | 0.001 | 0.21 | BD, ADHD>Healthy |
Values are mean (SD).
Degrees of freedom=2, 85.
BIS-11=Barrett Impulsiveness Scale-Version 11; SD=standard deviation.
Table 3.
Barratt Impulsiveness Scale, Version 11, Scores of Bipolar Disorder Subjects With and Without Attention-Deficit/Hyperactivity Disorder
| BIS-11 scores | BD with ADHD (N=13)a | BD without ADHD (N=18)a | Fb | p< | d |
|---|---|---|---|---|---|
| Cognitive | 20.6 (2.8) | 20.4 (4.1) | 0.02 | 0.90 | 0.03 |
| Motor | 24.5 (3.4) | 23.4 (3.9) | 0.65 | 0.43 | 0.30 |
| Nonplanning | 30.7 (5.0) | 30.7 (3.9) | 0.01 | 0.99 | 0.08 |
| Total | 75.8 (6.6) | 74.6 (9.2) | 0.17 | 0.68 | 0.16 |
Values are mean (SD).
Degrees of freedom=1, 30.
FIG. 1.
BIS-11 Subscale Scores in Healthy, ADHD, and Bipolar Adolescents. BIS-11=Barrett Impulsiveness Scale-Version 11; ADHD=attention-deficit/hyperactivity disorder.
The BD patients with DBDs scored significantly higher on the motor subscale than did those without DBDs (p=0.005, d=1.09). There were no statistically significant differences in the cognitive (p=0.5, d=0.22) or nonplanning (p=0.8, d=0.08) subscale scores nor the total scores (p=0.3, d=0.38).
There were no statistically significant correlations between the YMRS (mean: 29.3, SD: 8.8) and BIS-11 total or subscale scores within the BD group (cognitive: p=0.5, motor: p=0.6, nonplanning: p=0.7, total: p=0.8).
Discussion
Our results confirm that adolescents with BD or ADHD are more impulsive than healthy adolescents. The adolescents with ADHD were not more impulsive than the healthy comparison group on the nonplanning subscale. This may indicate that nonplanning impulsivity is relatively more specific to BD than to ADHD. The nonplanning subscale is represented mostly by behaviors such as not planning ahead (e.g., I plan trips well ahead of time), present focused thoughts (e.g., I am more interested in the present than the future), and problem-solving deficits (e.g., I like to think about complex problems), which are behaviors that are often clinically observed in adolescents with BD rather than the psychomotor impulsivity that is typically observed in adolescents with ADHD.
We did not observe significant associations between the severity of mania and the degree of impulsivity in the adolescents with BD. Consistent with these observations, studies of adults with BD have shown almost identical elevations in levels of impulsivity during both manic and euthymic mood states (Swann et al. 2001, 2003). This implies that impulsivity associated with BD may have a stable, trait-related component, which is independent of symptom severity and perhaps mood state (Peluso et al. 2007). Consequently, bipolar patients may have a potential for acting impulsively even when their mood appears to be stable.
Adolescents with BD frequently present with co-occurring syndromes such as ADHD, DBDs, and substance use disorders. All of these conditions, most notably ADHD and DBDs, produce symptoms that can mimic and overlap with symptoms of BD, so that distinguishing among these conditions can be diagnostically challenging (Biederman et al. 1996; Kowatch et al. 2005). In this study, the severity or type of impulsivity exhibited by bipolar patients with or without co-morbid ADHD was similar, as measured by the BIS-11. However, bipolar adolescents with co-morbid DBDs scored higher on the motor subscale, which may potentially act as a differentiating factor for this subgroup of patients. Additional studies with larger and more varied samples are needed to confirm these findings. Comparing youth with co-occurring BD and DBDs to adolescents with DBDs or BD would help provide a better understanding of this subgroup of patients. Further investigations examining the role of other comorbidities, such as substance use and anxiety disorders, on impulsivity in adolescents with BD are also needed.
Limitations
The small sample size in this study may have lowered the power to differentiate impulsivity between bipolar and ADHD patients as well as to find an association between the mood state and impulsivity in the bipolar youth. However, effect size calculations suggested that there were small effect sizes for differences in BIS-11 scores between the BD and ADHD groups. Although the BIS-11, with its well-established subscales, is one of the oldest instruments available for assessing impulsivity, it has an inherent disadvantage of being a self-report questionnaire that relies on the veracity of the person answering the questions. This may be particularly problematic in adolescents. Research on the validity of youth self-reports, teacher reports, and parent reports on various scales used in assessing pediatric BD, such as the Child Behavior Checklist, the parent YMRS, the General Behavior Inventory, the parent General Behavior Inventory, the Achenbach Youth Self Report, and Teacher Report Form, have consistently shown that parent reports have greater validity than youth or teacher reports, even when the parent has a diagnosed mood disorder (Youngstrom et al. 2004). Studies examining the validity of parent and adolescent reports on the BIS-11 may be useful.
Conclusion
Our findings suggest that impulsivity is elevated in adolescents with BD, as well as in adolescents with ADHD, relative to healthy adolescents. On notable exception is that nonplanning impulsivity was not significantly different between adolescents with ADHD and healthy adolescents. This may suggest that nonplanning impulsivity is relatively specific to adolescents with BD. Additionally, our data indicate that elevations in impulsivity, as measured by the BIS-11, may be independent of symptoms severity and, therefore, may be a stable, trait-related component of BD.
Clinical Significance
To our knowledge, this is the first study to utilize the BIS-11 to measure impulsivity in adolescents with BD or ADHD. The nonplanning subscale of the BIS-11 may potentially differentiate between adolescents with BD and ADHD. Understanding the characteristics of impulsivity in youth with BD or ADHD could potentially lead to unique behavioral intervention strategies. Future studies using the BIS-11 to examine the role of psychotropic medication exposure and lifetime history of behavioral intervention on impulsivity in these disorders could be useful in the future.
Disclosures
Dr. Nandagopal has received research support from AstraZeneca, BMS/Otsuka, Lilly, GSK, Pfizer, J & J, Shire, Abbott, Janssen, Martek, Somerset, Repligen, Sumitomo, NIDA, NIMH, NIAAA, and NARSAD.
Dr. DelBello has received research support from AstraZeneca, Otsuka, Eli Lilly, GSK, Pfizer, J & J, Shire, Abbott Laboratories, Janssen, Martek, Somerset, Repligen, Sumitomo, NIDA, NIMH, NIAAA, and NARSAD, and has served as a speaker and/or consultant for American Academy of Child and Adolescent Psychiatry, AstraZeneca, BMS, GSK, Schering Plough, Merck, and Pfizer.
Dr. Adler has received research support from Abbott Laboratories, AstraZeneca, Eli Lilly, Shire, Janssen (Johnson & Johnson), Pfizer, Bristol Myers Squibb, Repligen, Martek, and Somerset, and has served as a speaker and/or consultant for Schering-Plough/Merck and Janssen (Johnson and Johnson).
Dr. Strakowski has received research support from Eli Lilly, Janssen, AstraZenecha, Martek Biosciences, Nutrition 21, Repligen, NIDA, NIAAA, NIMH, and NARSAD, Speaking: American Academy of Child and Adolescent Psychiatry. Other: Consensus Medical Communications.
Dr. David Fleck and Mr. Neil Mills have no disclosures.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed., Text Revision (DSM-IV-TR) Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Biederman J. Faraone S. Mick E. Wozniak J. Chen L. Ouellette C. Marrs A. Moore P. Garcia J. Mennin D. Lelon E. Attention-deficit/hyperactivity disorder and juvenile mania: An overlooked comorbidity? J Am Acad Child Adolesc Psychiatry. 1996;35:997–1008. doi: 10.1097/00004583-199608000-00010. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Evenden J. Impulsivity: A discussion of clinical and experimental findings. J Psychopharmacol. 1999;13:180–192. doi: 10.1177/026988119901300211. [DOI] [PubMed] [Google Scholar]
- Geller B. Williams M. Zimerman B. Frazier J. Washington University in St. Louis Kiddie Schedule for Affective Disorders and Schizophrenia (WASH-U KSADS) St Louis, MO: Washington University; 1996. [DOI] [PubMed] [Google Scholar]
- Geller B. Zimerman B. Williams M. Bolhofner K. Craney JL. DelBello M. Soutullo C. Reliability of the Washington University in St. Louis Kiddie Schedule for Affective Disorders and Schizophrenia (WASH-U KSADS) mania and rapid cycling sections. J Am Acad Child and Adolesc Psychiatry. 2001;40:450–455. doi: 10.1097/00004583-200104000-00014. [DOI] [PubMed] [Google Scholar]
- Geller B. Zimerman B. Williams M. DelBello MP. Frazier J. Beringer L. Phenomenology of prepubertal and early adolescent bipolar disorder: Examples of elated mood, grandiose behaviors, decreased need for sleep, racing thoughts and hypersexuality. J Child Adolesc Psychopharmacol. 2002;12:3–10. doi: 10.1089/10445460252943524. [DOI] [PubMed] [Google Scholar]
- Holmes MK. Bearden CE. Barguil M. Fonseca M. Monkul ES. Nery FG. Soares JC. Mintz J. Glahn DC. Conceptualizing impulsivity and risk taking in bipolar disorder: Importance of history of alcohol abuse. Bipolar Disord. 2009;11:33–40. doi: 10.1111/j.1399-5618.2008.00657.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kowatch RA. Youngstrom EA. Danielyan A. Findling RL. Review and meta-analysis of the phenomenology and clinical characteristics of mania in children and adolescents. Bipolar Disord. 2005;7:483–496. doi: 10.1111/j.1399-5618.2005.00261.x. [DOI] [PubMed] [Google Scholar]
- McBurnett K. Lahey BB. Pfiffner LJ. Diagnosis of attention deficit disorders in DSM-IV: Scientific basis and implications for education. Except Child. 1993;60:108–117. [Google Scholar]
- Moeller FG. Barratt ES. Dougherty DM. Schmitz JM. Swann AC. Psychiatric aspects of impulsivity. Am J Psychiatry. 2001;158:1783–1793. doi: 10.1176/appi.ajp.158.11.1783. [DOI] [PubMed] [Google Scholar]
- Patton JH. Stanford MS. Barratt ES. Factor structure of the Barratt impulsiveness scale. J Clin Psychol. 1995;51:768–774. doi: 10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Peluso MAM. Hatch JP. Glahn DC. Monkul ES. Sanches M. Najt P. Bowden CL. Barratt ES. Soares JC. Trait impulsivity in patients with mood disorders. J Affect Disord. 2007;100:227–231. doi: 10.1016/j.jad.2006.09.037. [DOI] [PubMed] [Google Scholar]
- Ray Li CS. Chen SH. Lin WH. Yang YY. Attentional blink in adolescents with varying levels of impulsivity. J Psychiatry Res. 2005;39:197–205. doi: 10.1016/j.jpsychires.2004.06.003. [DOI] [PubMed] [Google Scholar]
- Swann AC. Anderson JC. Dougherty DM. Moeller FG. Measurement of inter-episode impulsivity in bipolar disorder. Psychiatry Res. 2001;101:195–197. doi: 10.1016/s0165-1781(00)00249-3. [DOI] [PubMed] [Google Scholar]
- Swann AC. Pazzaglia P. Nicholls A. Dougherty DM. Moeller FG. Impulsivity and phase of illness in bipolar disorder. J Affect Disord. 2003;73:105–111. doi: 10.1016/s0165-0327(02)00328-2. [DOI] [PubMed] [Google Scholar]
- Young R. Biggs JT. Ziegler VE. Meyer DA. A rating scale for mania: Reliability, validity and sensitivity. Br J Psychiatry. 1978;133:429–435. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]
- Youngstrom EA. Findling RL. Calabrese JR. Gracious BL. Demeter C. Bedoya DD. Price M. Comparing the diagnostic accuracy of six potential screening instruments for bipolar disorder in youths aged 5 to 17 years. J Am Acad Child Adolesc Psychiatry. 2004;43:847–858. doi: 10.1097/01.chi.0000125091.35109.1e. [DOI] [PubMed] [Google Scholar]