Abstract
Context:
Clusterin has been associated with several pathologies, including cardiovascular disease and neoplasias. However, little is known about its physiology and its association with metabolic and anthropometric parameters in humans.
Objective:
The aim of the study was to examine whether circulating clusterin levels exhibit a day/night variation pattern and whether clusterin is associated with anthropometric and metabolic parameters.
Design:
Study A was a frequent sampling study to evaluate potential periodicity in clusterin secretion. Study B was an observational study to evaluate the cross-sectional and prospective associations of clusterin with anthropometric and metabolic parameters.
Participants:
Study A participants were healthy males (n = 6) and females (n = 6), aged 22.3 ± 3.1 and 22.8 ± 3.4 yr, respectively. Study B participants were 186 healthy males aged 18.4 ± 0.14 yr. Ninety-one of the study B subjects were studied again 2 yr later and clusterin's associations with change of anthropometric and metabolic parameters were thus investigated prospectively.
Intervention:
Samples in study A were collected every 15 min during an overnight admission, and subsequently pooled every hour. Samples in study B were collected during a screening visit.
Main Outcome Measure:
Circulating clusterin levels were measured.
Results:
In study A, spectral domain and cosinor regression analysis failed to reveal any day/night variation pattern. In study B, clusterin was positively correlated with total and low-density lipoprotein cholesterol (r = 0.23, P = 0.002; and r = 0.20, P = 0.005). Baseline clusterin did not predict change of any anthropometric, biochemical, or metabolic parameters prospectively.
Conclusions:
We report for the first time that circulating clusterin does not have a day/night variation pattern in healthy young individuals. Clusterin levels are associated with total and low-density lipoprotein cholesterol cross-sectionally but do not predict short-term changes in metabolic parameters in healthy young males.
Clusterin [apolipoprotein J (ApoJ)] (1, 2) constitutes a separate subclass of high-density lipoproteins (HDL), the ApoJ–HDL, with a vertical gradient centrifugation density ranging from the values of HDL-2 up to the values of very HDL (3). Clusterin has been shown to be associated with a variety of biological processes, including promotion of erythrocyte aggregation, attenuation of complement activity, reverse lipid transportation, sperm maturation, and regulation of apoptosis (4). Accumulating evidence has emerged in the areas of inflammation, lipid metabolism, diabetes mellitus (DM)/metabolic syndrome, and associated conditions, namely cancer and atherosclerosis.
The physiology of clusterin and any associations with metabolic factors in healthy individuals remain largely unknown (5). The purpose of this study is to evaluate for the first time whether circulating clusterin displays a day/night variation pattern and to examine associations of clusterin with anthropometric parameters, including body mass index (BMI), waist to hip ratio, fat mass, fat free mass, and adipocytokines; biochemical metabolic parameters, including blood glucose, HDL, low-density lipoprotein (LDL), and triglycerides; as well as cardiovascular parameters, namely, heart rate and systolic and diastolic arterial pressure (SAP and DAP) in a population sample of young healthy individuals.
Subjects and Methods
Study A: Frequent sampling study of healthy individuals
To examine whether circulating clusterin displays a day/night variability pattern, we analyzed serum samples collected from six lean males aged 22.3 ± 3.1 yr and six lean females aged 22.8 ± 3.4 yr that were studied in an isocaloric fed state in the General Clinical Research Center at Beth Israel Deaconess Medical Center in Boston, Massachusetts (6, 7). Serum samples were processed immediately and stored at −80 C until analysis. The average BMI of the male and female subjects was 23.4 ± 1.7 and 21.7 ± 2.2 kg/m2, respectively. All subjects were healthy and were not on any medication. All female subjects had a regular menstrual cycle (length, 26–32 d), and blood sampling was scheduled within menstrual cycle d 6–11. Samples were drawn through an indwelling peripheral iv line every 15 min while the subjects were in the isocaloric fed state and then pooled every hour to reach adequate sample volume for the purposes of our experiments. Meals, sleep, and other potential confounders were standardized as previously described (6, 7). The study received approval of the local Institutional Review Board (IRB). All subjects had given written informed consent to participate.
Study B: Cross-sectional and prospective epidemiologic study (Cyprus Metabolism Study)
To evaluate the association of clusterin with anthropometric, metabolic, and cardiovascular parameters, we used a random sample of 186 participants of the Cyprus Metabolism study who were recruited during 2006. The number of subjects was selected so that the study would have 80% power at the α = 0.05 level to detect associations with r > 0.2. Details of this study have been previously described (8). Briefly, this is a study of 18-yr-old males that were enrolled during health screening before their 2-yr mandatory military service in the Cypriot Armed Forces. Serum samples were collected and stored at −80 C until analyzed. The fact that military service is mandatory in Cyprus at the age of 18 prevents any potential selection bias. From the 186 subjects that we used in this study, 91 were also followed up 2 yr later. This study has received approval from the Harvard School of Public Health IRB and the Cyprus National Bioethics Committee.
Biochemical analysis
Measurements of clusterin and other biochemical and hormonal measurements were performed using standard assays as described in the Supplemental Data (published on The Endocrine Society's Journals Online web site at http://jcem.endojournals.org).
Statistical analysis
Statistical analysis was performed with STATA v11.1 (STATA Corp., College Station, TX) and Pulse XP (University of Virginia, Charlottesville, VA) software. Results are presented as means ± sd. All tests were two-sided, and the α criterion was set at 0.05. Details of the statistical analyses are reported in the Supplemental Data.
Results
Day/night variability analysis
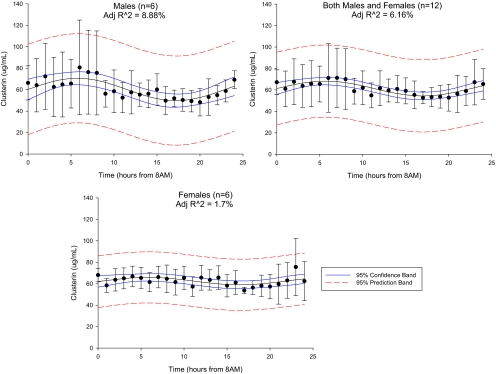
Repeated measurements ANOVA on normalized clusterin levels revealed no statistically significant different clusterin levels between hourly time points (P = 0.28 for males and P = 0.26 for females). We managed to fit a nonlinear, ordinal least squares, four-parameter sine model to males (amplitude = 10.39 ± 2.46 μg/ml, P < 0.001; period = 22.9 ± 2.46 h, P < 0.001), females (amplitude = 3.45 ± 1.46 μg/ml, P < 0.02; period = 21.43 ± 3.48 h, P < 0.001), and the combined dataset (amplitude = 6.88 ± 1.47 μg/ml, P < 0.001; period = 22.60 ± 2.04 h, P < 0.001). Although the aforementioned models were statistically significant, the nonlinear adjusted coefficients of determination (R2) were 8.88, 1.7, and 6.16%, respectively (Fig. 1), enabling us to report with confidence the absence of any significant day/night variation pattern.
Fig. 1.
Twenty-four-hour circulating clusterin level variation in males (n = 6), females (n = 6), and both (n = 12). Error bars represent sd, continuous line represents 95% confidence band, and dashed line represents 95% prediction bands. Adj-R∧2, Adjusted coefficient of determination.
Cross-sectional results from the Cyprus Metabolism Study
The mean age of the 186 male subjects was 18.47 ± 0.15 yr, and their mean BMI was 23.07 ± 3.87 kg/m2. Baseline characteristics of these subjects are described in detail in Supplemental Table 1. Spearman's correlations demonstrated a statistically significant positive correlation between circulating clusterin levels and total and LDL cholesterol (r = 0.21 and 0.19; P = 0.003 and 0.008, accordingly). We failed to demonstrate any association of clusterin with BMI, fat mass, fat free mass, bioelectrical impedence, total body water (TBW), basic metabolic rate (BMR), SAP, DAP, triglycerides, glucose, and HDL cholesterol (data not shown). Clusterin does not exhibit any significant correlation with other metabolism regulators such as leptin (r = 0.055; P = 0.46), resistin (r = −0.089; P = 0.23), or total adiponectin (r = 0.072; P = 0.34). Subjects with LDL cholesterol above 130 mg/dl had statistically significant higher clusterin levels compared with the subjects with LDL cholesterol below 130 mg/dl (86.41 ± 12.53 vs. 78.19 ± 12.53 ng/ml; P = 0.002).
Prospective results from the Cyprus Metabolism Study
Characteristics of the cohort that was used to examine the prospective effects of clusterin on the previously described anthropometric, biochemical, and cardiometabolic parameters were not different from the total sample (Supplemental Table 1). Weight, BMI, BMR, fat free mass, TBW, glucose, total cholesterol, triglycerides, SAP, DAP, and heart rate increased statistically significantly over the 2-yr follow-up period (Table 1). Specifically, the percentage of fat mass increased from 12.79 ± 5.70 to 15.5 ± 6.04% (P < 0.001), fat mass increased from 9.47 ± 6.5 to 11.98 ± 7.51 kg (P < 0.001), and fasting glucose increased from 78.07 ± 6.67 to 86.65 ± 9.20 mg/dl (P < 0.001). However, despite this increase, on average these variables still remained within the normal range. To evaluate whether baseline clusterin levels could be a predictor of these changes, we used a mixed-effect linear regression model, adjusting for BMI. Although for some variables clusterin seemed to have a regression coefficient statistically different from zero (Table 1), the coefficient was too small to have any significant predictive clinical significance.
Table 1.
Mixed-effects linear regression model to evaluate the effect of baseline clusterin levels on the 2-yr change (adjusted for BMI) in study B
| Parameter | Age (yr) |
Baseline clusterin (μg/ml) |
||
|---|---|---|---|---|
| b (95% CI) | P | b (95% CI) | P | |
| Weight (kg) | 1.07 (0.53, 1.60) | <0.001 | −0.15 (−0.31, −0.005) | 0.06 |
| Height (m) | 0.00 (0.002, 0.003) | <0.001 | 0.00 (−0.001, 0.001) | 0.04 |
| BMR (kJ) | 47.94 (18.35, 77.55) | 0.002 | −11.65 (−23.03, −0.26) | 0.045 |
| BMR (kcal) | 11.48 (4.40, 18.55) | 0.001 | −2.78 (−5.51, −0.064) | 0.045 |
| BIA | 4.54 (1.12, 7.98) | 0.009 | 0.4 (−0.24, 1.12) | 0.21 |
| % Fat | 0.65 (0.33, 0.98) | <0.001 | −0.002 (−0.05, 0.04) | 0.92 |
| Fat mass (kg) | 0.51 (0.18, 0.83) | 0.002 | −0.03 (−0.10, 0.02) | 0.24 |
| Free fat mass (kg) | 0.46 (0.20, 0.74) | 0.001 | −0.11 (−0.22, −0.007) | 0.035 |
| TBW | 0.34 (0.14, 0.54) | 0.001 | −0.08 (−0.15, −0.005) | 0.035 |
| Glucose (mg/dl) | 3.85 (2.86, 4.85) | <0.001 | −0.03 (−0.15, 0.09) | 0.63 |
| Total cholesterol (mg/dl) | 7.38 (5.24, 9.53) | <0.001 | 0.49 (0.05 − 0.93) | 0.03 |
| HDL (mg/dl) | −0.41 (−1.08, 0.26) | 0.25 | 0.03 (−0.11, 0.18) | 0.66 |
| LDL (mg/dl) | −1.77 (−3.54, 0.11) | 0.06 | 0.38 (0.002, 0.79) | 0.05 |
| Triglycerides (mg/dl) | 6.81 (2.84, 10.77) | 0.001 | 0.53 (0.06, 0.99) | 0.026 |
| Waist (cm) | 1.21 (0.65, 1.78) | <0.001 | −0.065 (−0.16, 0.03) | 0.17 |
| Hip (cm) | −0.15 (−0.6, 0.29) | 0.49 | −0.09 (−0.17, −0.12) | 0.025 |
| Waist/hip ratio | −0.004 (−0.01, 0.02) | 0.16 | 0.00 (−0.005, 0.0006) | 0.8 |
| Heart rate (bpm) | 2.41 (1.39, 3.43) | <0.001 | 0.03 (−0.11, 0.17) | 0.67 |
| SAP (mm Hg) | 1.71 (0.68, 2.73) | 0.001 | 0.009 (−0.12, 0.14) | 0.89 |
| DAP (mm Hg) | 4.33 (3.61, 5.06) | <0.001 | −0.006 (−0.11, 0.10) | 0.91 |
b, Unstandardized regression coefficient; 95% CI, 95% confidence interval of the unstandardized regression coefficient; BIA, bioelectrical impedence. Bold signifies a significance defined from a P value ≤ 0.05.
Discussion
The role of clusterin in attenuation of inflammation and reverse cholesterol transfer makes this molecule a potential candidate as a marker for cancer, cardiovascular disease, DM, and metabolic syndrome. Although an increasing number of studies have been published in the cancer area (9, 10), relatively fewer publications describe potential associations of clusterin with DM and the metabolic syndrome, and the latter have reported controversial results (11–13). Importantly, no study to date has examined whether clusterin has any day/night variation pattern, a question of direct relevance to timing of sampling in all clinical research studies on clusterin. The physiology of clusterin also remains unknown, including whether it is associated with anthropometric and metabolic parameters in healthy individuals.
We first studied whether levels of clusterin vary during the day. We demonstrate that only 8.88% (males), 1.7% (females), and 6.16% (combined) of the variability could be explained by a potential underlying day/night rhythm, as modeled by a cosine function. These results, in conjunction with the high temporal resolution of our study (every 1 h), enable us to report with great confidence that clusterin does not have any clinically significant day/night variability. Moreover, meals and sleep do not seem to affect circulating levels throughout the day. These data not only contribute toward our knowledge of clusterin physiology but also are of direct relevance to the timing of sampling for future studies on clusterin.
The results from our cross-sectional analysis demonstrated that clusterin is positively correlated with total and LDL cholesterol in healthy young males but were not associated with any other metabolic variables and/or hormones important in energy homeostasis and metabolism, including leptin (14–16), adiponectin (17, 18), and/or resistin (19). This is consistent with a previous study demonstrating a positive correlation of clusterin with ApoA; ApoB; total, LDL, and HDL cholesterol; and years of documented DM and a negative correlation with ApoE in individuals with established cardiac and/or metabolic disease (11). In the same study, subjects with DM, myocardial infraction, chronic coronary artery disease, or chronic coronary artery disease plus DM had statistically significantly higher serum clusterin levels compared with the healthy individuals (11). A later study of similar size confirmed increased clusterin levels in diabetics when compared with controls but failed to demonstrate any significant changes in patients with coronary artery disease (12).
Contrary to these reports, Hoofnagle et al. (13) demonstrated that HDL clusterin was significantly decreased in a lean insulin-resistant group and even lower in an obese insulin-resistant group when compared with lean, insulin-sensitive, middle-aged individuals. In addition, they also described a positive correlation between HDL clusterin and BMI, homeostasis model of assessment for insulin resistance, and HDL, as well as a negative association between clusterin and triglyceride levels. Furthermore, Hoofnagle et al. (13) report that HDL clusterin is not different in diabetic vs. healthy individuals, whereas it is significantly lower in patients with metabolic syndrome compared with healthy individuals. In a recent genomic study, clusterin gene polymorphisms were associated with increased insulin resistance and decreased insulin secretion (20).
Our study is the first study to examine potential day/night variability in circulating clusterin levels. We used samples collected every 15 min and pooled hourly, i.e. samples with a temporal resolution of 1 h, thus increasing the accuracy of our results. The sample size that we used has been shown in the past to be adequate to detect hormonal day/night patterns (6, 7). Furthermore, our subjects were standardized for the caloric intake, light/dark environment, gender, and phase of menstrual cycle (females only). This is also the first cross-sectional study to examine associations of clusterin in healthy individuals and the first prospective study overall. This study was adequately powered to demonstrate any association at the r above 0.2 level with an α criterion of 0.05. Future studies with longer follow-up time are needed to confirm associations reported herein. Although the day/night variation results apply to both males and females, results from the observational study cannot necessarily be generalized to females and/or other races because the sample was composed of Caucasian males.
To summarize, this study is the first to demonstrate that clusterin levels do not have a day/night variability pattern. Furthermore, this is the first study that demonstrates a positive correlation between clusterin and total and LDL cholesterol in young healthy individuals cross-sectionally.
Acknowledgments
This work was supported by National Center for Research Resources Grant M01-RR-01032-328840 (to the Harvard Clinical and Translational Science Center). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health. Funding was also received from the National Institute of Diabetes and Digestive and Kidney Diseases (Grants DK058785, DK079929, and DK081913), the National Institute on Aging (Grant AG032030), and a VA Merit award.
Disclosure Summary: The authors have nothing to disclose.
Footnotes
- Apo
- Apolipoprotein
- BMI
- body mass index
- BMR
- basal metabolic rate
- DAP
- diastolic arterial pressure
- DM
- diabetes mellitus
- HDL
- high-density lipoprotein
- LDL
- low-density lipoprotein
- SAP
- systolic arterial pressure
- TBW
- total body water.
References
- 1. Blaschuk O, Burdzy K, Fritz IB. 1983. Purification and characterization of a cell-aggregating factor (clusterin), the major glycoprotein in ram rete testis fluid. J Biol Chem 258:7714–7720 [PubMed] [Google Scholar]
- 2. de Silva HV, Stuart WD, Park YB, Mao SJ, Gil CM, Wetterau JR, Busch SJ, Harmony JA. 1990. Purification and characterization of apolipoprotein J. J Biol Chem 265:14292–14297 [PubMed] [Google Scholar]
- 3. de Silva HV, Stuart WD, Duvic CR, Wetterau JR, Ray MJ, Ferguson DG, Albers HW, Smith WR, Harmony JA. 1990. A 70-kDa apolipoprotein designated ApoJ is a marker for subclasses of human plasma high density lipoproteins. J Biol Chem 265:13240–13247 [PubMed] [Google Scholar]
- 4. Bettuzzi S. 2009. Conclusions and perspectives. Adv Cancer Res 105:133–150 [DOI] [PubMed] [Google Scholar]
- 5. Aronis KN, Kim YB, Mantzoros CS. 2011. Clusterin (apolipoprotein J): wither link with diabetes and cardiometabolic risk? Metabolism 60:747–748 [DOI] [PubMed] [Google Scholar]
- 6. Chan JL, Heist K, DePaoli AM, Veldhuis JD, Mantzoros CS. 2003. The role of falling leptin levels in the neuroendocrine and metabolic adaptation to short-term starvation in healthy men. J Clin Invest 111:1409–1421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chan JL, Matarese G, Shetty GK, Raciti P, Kelesidis I, Aufiero D, De Rosa V, Perna F, Fontana S, Mantzoros CS. 2006. Differential regulation of metabolic, neuroendocrine, and immune function by leptin in humans. Proc Natl Acad Sci USA 103:8481–8486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hamnvik OP, Liu X, Petrou M, Gong H, Chamberland JP, Kim EH, Christophi CA, Kales SN, Christiani DC, Mantzoros CS. 2011. Soluble leptin receptor and leptin are associated with baseline adiposity and metabolic risk factors, and predict adiposity, metabolic syndrome, and glucose levels at 2-year follow-up: the Cyprus Metabolism Prospective Cohort Study. Metabolism 60:987–993 [DOI] [PubMed] [Google Scholar]
- 9. Panico F, Rizzi F, Fabbri LM, Bettuzzi S, Luppi F. 2009. Clusterin (CLU) and lung cancer. Adv Cancer Res 105:63–76 [DOI] [PubMed] [Google Scholar]
- 10. Rizzi F, Bettuzzi S. 2009. Clusterin (CLU) and prostate cancer. Adv Cancer Res 105:1–19 [DOI] [PubMed] [Google Scholar]
- 11. Trougakos IP, Poulakou M, Stathatos M, Chalikia A, Melidonis A, Gonos ES. 2002. Serum levels of the senescence biomarker clusterin/apolipoprotein J increase significantly in diabetes type II and during development of coronary heart disease or at myocardial infarction. Exp Gerontol 37:1175–1187 [DOI] [PubMed] [Google Scholar]
- 12. Kujiraoka T, Hattori H, Miwa Y, Ishihara M, Ueno T, Ishii J, Tsuji M, Iwasaki T, Sasaguri Y, Fujioka T, Saito S, Tsushima M, Maruyama T, Miller IP, Miller NE, Egashira T. 2006. Serum apolipoprotein j in health, coronary heart disease and type 2 diabetes mellitus. J Atheroscler Thromb 13:314–322 [DOI] [PubMed] [Google Scholar]
- 13. Hoofnagle AN, Wu M, Gosmanova AK, Becker JO, Wijsman EM, Brunzell JD, Kahn SE, Knopp RH, Lyons TJ, Heinecke JW. 2010. Low clusterin levels in high-density lipoprotein associate with insulin resistance, obesity, and dyslipoproteinemia. Arterioscler Thromb Vasc Biol 30:2528–2534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mantzoros CS. 2000. Role of leptin in reproduction. Ann NY Acad Sci 900:174–183 [DOI] [PubMed] [Google Scholar]
- 15. Mantzoros CS, Liolios AD, Tritos NA, Kaklamani VG, Doulgerakis DE, Griveas I, Moses AC, Flier JS. 1998. Circulating insulin concentrations, smoking, and alcohol intake are important independent predictors of leptin in young healthy men. Obes Res 6:179–186 [DOI] [PubMed] [Google Scholar]
- 16. Kelesidis T, Kelesidis I, Chou S, Mantzoros CS. 2010. Narrative review: the role of leptin in human physiology: emerging clinical applications. Ann Intern Med 152:93–100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Blüher M, Brennan AM, Kelesidis T, Kratzsch J, Fasshauer M, Kralisch S, Williams CJ, Mantzoros CS. 2007. Total and high-molecular weight adiponectin in relation to metabolic variables at baseline and in response to an exercise treatment program: comparative evaluation of three assays. Diabetes Care 30:280–285 [DOI] [PubMed] [Google Scholar]
- 18. Mantzoros CS, Trakatelli M, Gogas H, Dessypris N, Stratigos A, Chrousos GP, Petridou ET. 2007. Circulating adiponectin levels in relation to melanoma: a case-control study. Eur J Cancer 43:1430–1436 [DOI] [PubMed] [Google Scholar]
- 19. Wolfe BE, Jimerson DC, Orlova C, Mantzoros CS. 2004. Effect of dieting on plasma leptin, soluble leptin receptor, adiponectin and resistin levels in healthy volunteers. Clin Endocrinol (Oxf) 61:332–338 [DOI] [PubMed] [Google Scholar]
- 20. Daimon M, Oizumi T, Karasawa S, Kaino W, Takase K, Tada K, Jimbu Y, Wada K, Kameda W, Susa S, Muramatsu M, Kubota I, Kawata S, Kato T. 2011. Association of the clusterin gene polymorphisms with type 2 diabetes mellitus. Metabolism 60:815–822 [DOI] [PubMed] [Google Scholar]