Abstract
Objective
We determine whether (1) an audiocomputer-delivered tailored feedback intervention increases emergency department (ED) patient uptake of opt-in, nontargeted rapid HIV screening; and (2) uptake is greater among patients who report more HIV risk and among those whose self-perceived HIV risk increases from baseline after completion of an HIV risk assessment.
Methods
ED patients aged 18 to 64 years were randomly assigned to receive either an assessment about reported and self-perceived HIV risk or an identical assessment plus feedback about their risk for having or acquiring an HIV infection, tailored according to their reported risk. All participants were offered a fingerstick rapid HIV test. Two-sample tests of binomial proportions were used to compare screening uptake by study arm. Multivariable logistic regression was used to assess the relationship of reported HIV risk and an increase in self-perceived HIV risk with uptake of HIV screening.
Results
Of the 566 participants, the median age was 29 years, 62.2% were women, and 66.9% previously had been tested for HIV. Uptake of HIV screening was similar in the intervention and no intervention arms (54.1% versus 55.5% [Δ =–0.01%; 95% confidence interval {CI} –0.09% to 0.07%]). An increase in self-perceived HIV risk predicted greater uptake of HIV screening for women (odds ratio 2.15; 95% CI 1.08 to 4.28) but not men (odds ratio 1.61; 95% CI 0.60 to 4.30). Uptake of HIV screening was not related to reported HIV risk.
Conclusion
Uptake of rapid HIV screening in the ED was not improved by this feedback intervention. Other methods need to be investigated to improve uptake of HIV screening by ED patients.
Introduction
Background
In a previous study, we observed that uptake of opt-in rapid HIV screening by a random sample of adult emergency department (ED) patients was approximately 40%, and that uptake varied by patient demographic characteristics and perception of risk for an HIV infection.1 Research on ED-based HIV screening indicates that a belief of not being at risk for an HIV infection is a major reason for declining opt-in HIV screening.1–7 In a randomized controlled trial, we found that self-perceived risk for an HIV infection was modestly increased when ED patients underwent a tailored feedback intervention about their HIV risk behaviors with an audiocomputer-assisted interview system.8 If self-perceived HIV risk can be increased, perhaps uptake of HIV screening can also be increased through this type of intervention.
Importance
The Centers for Disease Control and Prevention recently recommended that EDs in the United States use an opt-out approach to help improve uptake of HIV screening, according to the promise of this approach in other health care settings.9 However, opt-out HIV screening is not yet available in all states,10,11 which has been the subject of controversy,12–14 and it is unclear whether and to what extent this approach will increase HIV screening uptake in EDs. The utility of using an opt-out approach for HIV screening in EDs is under investigation.15 The importance of this study is its exploration of an alternative method to increase uptake of HIV screening in the ED and its potential to serve as a means of comparison to the findings from studies that evaluate uptake of HIV screening when an opt-out approach is used. If shown to be effective, an intervention based on an audiocomputer-assisted interview system, which is a self-administered, private, low-labor-intensive technique, would be a potentially labor and time-saving method to conduct HIV screening in US EDs.
Goals of This Investigation
The primary objective of this randomized controlled trial was to determine the effectiveness of an audiocomputer-assisted, interview system–delivered, tailored feedback intervention about reported HIV risk behaviors on increasing uptake of opt-in, nontargeted (universal), rapid HIV screening among adult ED patients. Trial participants were randomly assigned to receive tailored, immediate, audiocomputer-assisted, interview system–based feedback about these risk behaviors or no feedback. The secondary objectives were to determine whether participant uptake of HIV screening increased as reported HIV risk increased and whether uptake was higher for patients who had an increase in self-perceived HIV risk through their involvement in the trial.
Methods
Study Design
This randomized controlled trial included a random sample of 18- to 64-year-old subcritically ill or injured ED patients who were assessed for their study eligibility and enrolled those who met study eligibility criteria and agreed to participate. Participants were randomly assigned to receive audiocomputer-assisted interview system–based feedback (intervention) or no feedback (no intervention) about their risk for having or acquiring an HIV infection according to their reported HIV risk behaviors. Participant uptake of rapid HIV screening was compared between patients in the feedback versus no feedback conditions. The Rhode Island Hospital institutional review board approved the study.
Setting
The trial was conducted at an urban, academic, not-for-profit, adult ED in New England from October 1, 2007, to September 30, 2008. The ED had approximately 54,000 visits by English-speaking 18- to 64-year-olds for a subcritical illness or injury during this 1-year period. This ED does not have a standing HIV screening program.
Selection of Participants
In an effort to obtain a representative sample of ED patients, we randomly selected the dates we conducted the study, the shifts we collected data, and the patients we approached to assess their study eligibility.1,8 The methods of selecting patients for assessment and enrollment, a description of the training of the research assistant who conducted the study, and the randomization methods have been described previously.1,8 Patients were study eligible if they were 18 to 64 years old; English speaking; not critically ill or injured; not prison inmates, under arrest, or undergoing home confinement; not presenting for a psychiatric illness; not known to be HIV infected; not participating in an HIV vaccine trial; not intoxicated; and not with a physical disability or mental impairment that prevented them from providing consent for participating in the study. No incentives were offered to participate. ED staff was not permitted to encourage or refer patients to be in the study.
Patients were queried about their demographic characteristics and HIV testing history with instruments developed and used in previous studies.1,16 Study-eligible patients were invited to participate in a study that entailed answering an anonymous, private, audiocomputer-assisted, interview system–based questionnaire about their risk for an HIV infection from injection drug use and sex. They were also informed that they would be randomly assigned to receive audiocomputer-assisted interview system–based feedback or no feedback to their answers. They were not informed about the intent of the intervention, the purpose of the study, or that they would be offered an HIV test at the end of the study.
Study Questionnaire, Intervention, and Primary Outcome Measurement
We used the HIV risk questionnaire as the assessment tool for this study, which we have described previously.8 The questionnaire asked participants to report their HIV injection drug use and sexual risk behaviors and to indicate their self-perceived risk for having an HIV infection. The reported HIV sexual risk behavior questions are sex-specific. The self-perceived HIV risk questions refer to participants’ perception that they currently could be HIV infected (before knowing their HIV test results), as opposed to their future risk for an HIV infection. The questionnaire asked participants about their self-perceived HIV risk twice: once before questions about their reported HIV risk behaviors (“pre”), and again after these questions (“post”). Participants completed the audiocomputer-assisted interview system–based HIV risk questionnaire with a tablet personal computer with headphones for the audio components.
The no-intervention arm received the questionnaire only, whereas the intervention arm received the questionnaire plus tailored feedback messages to responses about the reported HIV risk behaviors. The feedback messages advised participants about their risk for an HIV infection from engaging in each HIV risk behavior queried about in the questionnaire. The feedback messages were tailored to participant responses to the questionnaire as follows. Those who responded “yes” to the reported HIV risk behavior questions received qualitative feedback about the risk for an HIV infection from that behavior. Those who responded with “no” or “don’t know” or who refused to respond received qualitative feedback about their risk for an HIV infection if they engaged in (but did not report) or in the future engaged in that HIV risk behavior. The feedback messages were given immediately after the participant responded to each question and were directed to the participant in the second person (“you”). The feedback messages were displayed on the computer screen simultaneously with the accompanying audiotape of the messages. The feedback messages did not mention HIV testing.
The primary outcome measured in the trial was uptake of rapid HIV screening. After completion of the HIV risk questionnaire (with or without feedback), the research assistant offered each participant a free, rapid, fingerstick HIV test, using an opt-in and nontargeted approach. The research assistant also asked each participant to provide the main reason for accepting or declining HIV screening. The research assistant performed the rapid HIV test for those who elected to be tested and provided them their test results during the ED visit.
Data Analysis
Using an analytic approach developed previously, we calculated the reported HIV risk scores and change in self-perceived HIV risk for trial participants.8 In brief, the reported HIV risk scores were the sum of the participant responses to the reported HIV risk behavior questions divided by the total possible points assigned to each response to the risk questions. More points were assigned for responses indicating previous or current engagement in a given risk behavior (eg, injection drug use) or a higher level of involvement in a risk behavior (eg, more sexual partners). Because risk behaviors vary by sex (eg, male-male sexual intercourse), reported HIV risk behaviors were calculated by sex. Change in self-perceived HIV risk was calculated by subtracting the post from the pre self-perceived HIV risk and was reported as no change, a decrease, or an increase in self-perceived HIV risk.
Participants in the intervention and no intervention arms were compared according to their demographic characteristics, history of HIV testing, distribution of reported HIV risk scores, and change in self-perceived HIV risk using Wilcoxon rank-sum tests for continuous variables and Pearson’s χ2 tests for categorical variables. These and all other analyses were conducted with Stata 9.2 (StataCorp, College Station, TX). In all analyses, a significance level of α=.05 was used.
For the primary objective of assessing the effectiveness of the intervention on uptake of HIV screening, study arms were compared using 2-sample tests of proportions. Differences in proportions (Δ) with corresponding 95% confidence intervals (CIs) were calculated. For the secondary objective, proportions of participants accepting HIV screening according to reported HIV risk scores (in quartiles) and change in self-perceived HIV risk were calculated as stratified by sex and study arm. Separate multivariable logistic regression models were created to evaluate the relationship between reported HIV risk score and change in self-perceived HIV risk with uptake of HIV screening. Models were adjusted for participant demographic characteristics, HIV testing history, and study arm. Models were formed for women and men separately. Odds ratios with corresponding 95% CIs were estimated. Hosmer-Lemeshow goodness-of-fit testing demonstrated adequate model fitness of reported models.
Results
Characteristics
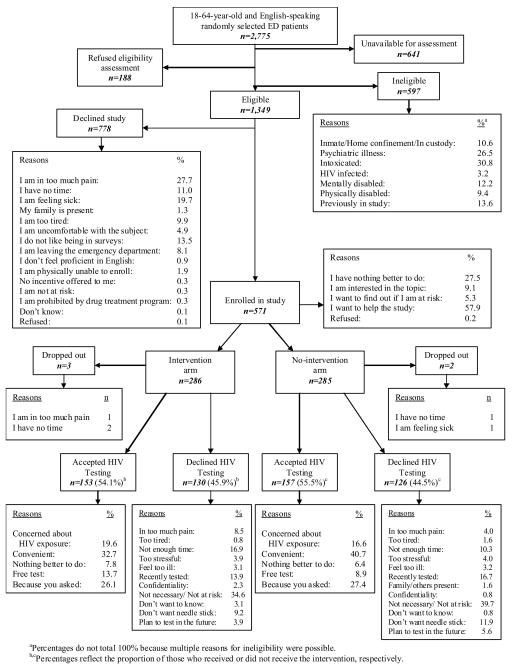
During the 12-month study period, 2,775 English-speaking 18- to 64-year-old ED patients were randomly selected and assessed for study eligibility. Five hundred sixty-six patients completed the randomized, controlled trial. The Figure depicts the results of eligibility assessments through study arm assignment and the major reasons for study ineligibility and for accepting or declining study enrollment. Participants in the 2 study arms were similar in terms of demographic characteristics, history of HIV testing, distribution of reported HIV risk behavior scores, and changes in self-perceived HIV risk (Tables E1 and E2, available online at http://www.annemergmed.com).
Figure.
Eligibility assessment and enrollment flow diagram.
Effect of Intervention on Uptake of HIV Screening
The Figure shows the proportion of trial participants by study arm who accepted or declined HIV screening and the main reasons participants provided for accepting or declining HIV screening. Uptake of HIV screening was similar in the intervention versus no intervention arms for all participants (54.1% versus 55.5% [Δ =−0.01%; 95% CI −0.09% to 0.07%]), female participants only (56.6% versus 53.4% [Δ =0.03%; 95% CI −0.07% to 0.14%]), and male participants only (50.0% versus 59.0% [Δ =−0.09%; 95% CI −0.22% to 0.04%]). The most common reason for declining HIV screening was a belief of not being at risk for HIV (37.1%), and the most common reason for accepting HIV screening was the convenience of being tested then in the ED (36.8%). The distribution of reasons for accepting or declining screening was also similar between the intervention and no intervention arms, regardless of sex (data not shown).
Relationship of Reported HIV Risk and Self-perceived HIV Risk With Uptake of HIV Screening
Table 1 displays the proportion of participants willing to be screened for HIV, as stratified by reported HIV risk scores and change in self-reported HIV risk for male and female participants by study arm. There was no apparent relationship between uptake of HIV screening and reported HIV risk scores, although female and male participants in the highest quartile of HIV risk scores appeared to have the highest uptake of screening (Table 1). Female and male participants exhibiting an increase in self-perceived HIV risk also appeared to have higher uptake of HIV screening (Table 1). However, as shown by the results of the multivariable logistic regression models (Table 2), there was no relationship between reported HIV risk scores and uptake of screening for women or men. Women with an increase in self-perceived HIV risk, compared with those with no change, had greater odds of accepting HIV screening. There was no relationship between change in self-perceived HIV risk and uptake of HIV screening for men.
Table 1.
Uptake in HIV screening according to reported HIV risk and self-perceived HIV risk by study arm and sex.
| Women, No. (%) | Men, No. (%) | |||||
|---|---|---|---|---|---|---|
| All Women | Intervention | No Intervention | All Men | Intervention | No Intervention | |
| Reporte d HIV risk score, quartiles | ||||||
| 1 | 51 (52.9) | 22 (63.6) | 29 (44.8) | 68 (52.9) | 31 (48.4) | 37 (56.8) |
| 2 | 123 (45.5) | 67 (46.3) | 56 (44.6) | 57 (41.1) | 33 (33.3) | 24 (54.2) |
| 3 | 104 (58.7) | 56 (64.3) | 48 (52.1) | 27 (48.2) | 16 (62.5) | 11 (27.3) |
| 4 | 75 (66.7) | 30 (60.0) | 45 (71.1) | 61 (70.5) | 28 (64.3) | 33 (75.8) |
| Change in self-perceive d HIV risk | ||||||
| Decrease | 22 (54.6) | 10 (80.0) | 12 (52.8) | 20 (60.0) | 11 (36.4) | 9 (88.9) |
| No change | 279 (52.0) | 135 (51.1) | 144 (33.3) | 166 (51.8) | 80 (50.0) | 86 (53.5) |
| Increase | 52 (71.2) | 30 (73.3) | 22 (68.2) | 27 (66.7) | 17 (58.8) | 10 (80.0) |
Table 2.
Correlates of HIV screening uptake.
| Women, OR (95% CI) | Men, OR (95% CI) | |
|---|---|---|
| Reported risk score, quartiles* | ||
| 1 | Reference | Reference |
| 2 | 0.89 (0.42–1.88) | 0.65 (0.30–1.42) |
| 3 | 1.41 (0.66–2.98) | 0.58 (0.21–1.55) |
| 4 | 1.73 (0.75–3.97) | 1.46 (0.63–3.39) |
| Change in self-perceived HIV risk* | ||
| No change | Reference | Reference |
| Decrease | 1.36 (0.53–3.49) | 1.00 (0.35–2.85) |
| Increase | 2.15 (1.08–4.28) | 1.61 (0.60–4.30) |
OR, Odds ratio.
Models were adjusted for intervention arm, history of HIV testing, age, ethnicity/race, partner status, insurance status, and years of formal education.
Limitations
There are a number of potential study limitations. First, despite efforts taken to obtain a representative sample, the study findings might not be applicable to other EDs with different distributions of patient demographic characteristics, HIV testing histories, and HIV risk or to patients who do not speak English. Second, willingness to participate might have been related to self-perceived HIV risk and the value of HIV screening, which in turn might have affected HIV screening uptake. However, as shown in the reasons for declining study participation (Figure), the subject of the study did not appear to deter participation. Third, although the study instrument was rigorously developed, it has not yet been demonstrated to predict HIV infection, and therefore the HIV risk behavior score cannot be interpreted to represent actual risk. Fourth, lack of blinding of the research assistant and patient to the study arm assignment could have affected the results. However, if this bias were present, we would expect a difference, rather than lack of difference, in screening uptake between study arms. Fifth, although patients were not informed that they would be offered an HIV test at the conclusion of the study, some patients might have suspected or anticipated this offer and declined the study. As such, the participants included in the study and the uptake of testing might not reflect true testing uptake in the absence of a research study.
Discussion
In this randomized controlled trial, an audiocomputer-assisted interview system–based feedback intervention about HIV infection risk from injection drug use and risky sexual behaviors did not improve uptake of opt-in, nontargeted (universal) HIV screening among this random sample of English-speaking, 18- to 64-year-old ED patients. The study findings indicate that the intervention used in this study is not a useful means of improving HIV screening among these patients. The failure of the intervention might be because the feedback messages concerned only the risk for HIV infection from the behaviors themselves and did not advocate for HIV screening more generally. Participants had to infer the need for HIV screening according to the feedback. Self-perception of risk for HIV infection, beliefs about the need for and value of testing, self-awareness about HIV risk, fears of testing, and other factors might have influenced that inference. It is possible that directly advising for HIV screening in the feedback overrode self-reflection and inference about need for HIV screening. Other reasons why the intervention failed include that the focus of the questions and responses on higher HIV risk behaviors might have led some patients to discount the need for HIV screening; the audiocomputer-assisted interview system feedback might have been too impersonal, and instead an in-person intervention is necessary; or the feedback messages might have been too limited in scope and depth, and further exploration to include thoughts, perceptions, feelings, and the nature of the behaviors and events in relation to a need for HIV screening is needed for this type of intervention. Future studies should investigate these possibilities.
Although greater reported HIV risk has been linked to ever having been tested for HIV (which includes being tested as part of a medical examination, being required to be tested, and having requested to be tested),17,18 the association between reported HIV risk and uptake of screening when it is offered has not been fully explored. Previous research in the ED has found that declining HIV screening partially depends on the perception of being at risk for HIV.1–7 We presumed, by extension of this logic, that patients who report more HIV risk behaviors would be more aware of their risk, would see the value of HIV screening for them, and therefore would be more likely to accept HIV screening. Much to our surprise, there was no relationship between reported HIV risk and uptake of screening. We also anticipated that because, as shown in our previous investigation, undergoing a risk assessment through our questionnaire is modestly associated with an increase in self-perceived HIV risk, higher self-perceived HIV risk would mediate greater uptake in HIV screening.8 However, uptake of screening was related to an increase in self-perceived HIV risk only for female participants, regardless of whether feedback was provided. Our previous study did show that self-perceived HIV risk was associated with reported HIV risk among women but not men.8 We do not know the reason for this difference response by sex, given that the proportion of female (14.7%) and male (12.6%) participants with an increase in self-perceived HIV risk was similar (Δ =2.1%; 95% CI −7.9% to 3.7%). As shown in previous studies, the relationship between self-perceived current or future risk for an HIV infection and reported HIV risk might not be strong or may even be discrepant.19–26 The interrelationship of having engaged in HIV risk behaviors, self-perception of the risk for having an HIV infection, and willingness to be screened for HIV also appears to be quite complex and should be the subject of future research.
Uptake of HIV screening was approximately 55% among study participants compared with 40% in our previous study, in which participants did not complete a risk assessment before being asked to undergo HIV screening.1 This finding suggests that asking patients about their HIV risk behaviors through an audiocomputer-assisted, interview system–based, HIV risk assessment questionnaire may improve uptake of screening by 15%, regardless of a feedback intervention about HIV risk. However, because participants were not randomized to a risk assessment or no risk assessment, we cannot definitely conclude that this type of HIV risk assessment alone will increase uptake of HIV screening. Future studies might investigate using a risk assessment alone as an intervention itself to increase uptake of HIV screening in EDs, whether an opt-out or an opt-in approach is used.
Supplementary Material
Acknowledgments
The authors acknowledge the assistance of Eric Feuchtbaum, who helped with the development and cognitive-based assessments of the questionnaire used in this study, as well as the staff and patients of the Rhode Island Hospital Emergency Department who made this study possible.
Funding and support: By Annals policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article that might create any potential conflict of interest. See the Manuscript Submission Agreement in this issue for examples of specific conflicts covered by this statement. Dr. Merchant and this study were supported by a career development grant from the National Institute for Allergy and Infectious Diseases (K23 A1060363). Dr. Mayer was supported by the Center for AIDS Research at Lifespan/Tufts/Brown (P30 AI42853).
Footnotes
Reprints not available from the authors.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Merchant RC, Seage GR, III, Mayer KH, et al. Emergency department patient acceptance of opt-in, universal, rapid HIV screening. Public Health Rep. 2008;123(suppl 3):27–40. doi: 10.1177/00333549081230S305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lyss SB, Branson BM, Kroc KA, et al. Detecting unsuspected HIV infection with a rapid whole-blood HIV test in an urban emergency department. J Acquir Immune Defic Syndr. 2007;44:435–442. doi: 10.1097/QAI.0b013e31802f83d0. [DOI] [PubMed] [Google Scholar]
- 3.Kelen GD, Shahan JB, Quinn TC. Emergency department–based HIV screening and counseling: experience with rapid and standard serologic testing. Ann Emerg Med. 1999;33:147–155. doi: 10.1016/s0196-0644(99)70387-2. [DOI] [PubMed] [Google Scholar]
- 4.Glick NR, Silva A, Zun L, et al. HIV testing in a resource-poor urban emergency department. AIDS Educ Prev. 2004;16:126–136. doi: 10.1521/aeap.16.2.126.29391. [DOI] [PubMed] [Google Scholar]
- 5.Lyons MS, Lindsell CJ, Ledyard HK, et al. Emergency department HIV testing and counseling: an ongoing experience in a low-prevalence area. Ann Emerg Med. 2005;46:22–28. doi: 10.1016/j.annemergmed.2004.12.022. [DOI] [PubMed] [Google Scholar]
- 6.Brown J, Kuo I, Bellows J, et al. Patient perceptions and acceptance of routine emergency department HIV testing. Public Health Rep. 2008;123(suppl 3):21–26. doi: 10.1177/00333549081230S304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.White DA, Scribner AN, Huang JV. A comparison of patient acceptance of fingerstick whole blood and oral fluid rapid HIV screening in an emergency department. J Acquir Immune Defic Syndr. 2009;52:75–78. doi: 10.1097/QAI.0b013e3181afd33d. [DOI] [PubMed] [Google Scholar]
- 8.Merchant RC, Clark MA, Langan TJ, IV, et al. Effectiveness of increasing emergency department patients’ self-perceived risk for being HIV infected through audio-computer self-interview (ACASI)–based feedback about reported HIV risk behaviors. Acad Emerg Med. 2009;16:1143–1155. doi: 10.1111/j.1553-2712.2009.00537.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Branson B, Handsfield HH, Lampe MA, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep. 2006;55:1–17. [PubMed] [Google Scholar]
- 10.Mahajan AP, Stemple L, Shapiro MF, et al. Consistency of state statutes with the Centers for Disease Control and Prevention HIV testing recommendations for health care settings. Ann Intern Med. 2009;150:263–269. doi: 10.7326/0003-4819-150-4-200902170-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Neff S, Goldschmidt RH. Impact of the 2006 CDC routine HIV testing recommendations on state HIV testing laws [abstract E07-2]. Paper presented at: 2009 National HIV Prevention Conference; 2009; Atlanta, GA. [Google Scholar]
- 12. [Accessed April 14, 2007.];Coalition comments on CDC’s draft revised HIV testing guidelines. Available at: http://www.champnetwork.org/media/Testing-Letter.pdf. Published March 31, 2006.
- 13. [Accessed April 14, 2007.];Federal HIV testing initiatives can only succeed with expanded healthcare, patient and provider education. Available at: http://www.champnetwork.org/media/Testing-Statement-092106.pdf. Published September 21, 2006.
- 14.American Civil Liberties Union. [Accessed April 14, 2007.];ACLU says new CDC HIV testing recommendations raise health and civil liberties concerns. Available at: http://www.aclu.org/hiv/testing/26819prs20060921.html. Published September 21, 2006.
- 15.Haukoos JS, Hopkins E, Byyny RL, et al. Design and implementation of a controlled clinical trial to evaluate the effectiveness and efficiency of routine opt-out rapid human immunodeficiency virus screening in the emergency department. Acad Emerg Med. 2009;16:800–808. doi: 10.1111/j.1553-2712.2009.00477.x. [DOI] [PubMed] [Google Scholar]
- 16.Merchant R, Gee E, Clark M, et al. Comparison of patient comprehension of rapid HIV pre-test fundamentals by information delivery format in an emergency department setting. BMC Public Health. 2007;7 doi: 10.1186/1471-2458-7-238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Anderson JE, Mosher WD, Chandra A. Measuring HIV risk in the US population aged 15–44: results from Cycle 6 of the National Survey of Family Growth. Adv Data. 2006;(377):1–27. [PubMed] [Google Scholar]
- 18.Anderson JE, Chandra A, Mosher WD. HIV testing in the United States, 2002. Adv Data. 2005;(363):1–32. [PubMed] [Google Scholar]
- 19.Lapidus JA, Bertolli J, McGowan K, et al. HIV-related risk behaviors, perceptions of risk, HIV testing, and exposure to prevention messages and methods among urban American Indians and Alaska Natives. AIDS Educ Prev. 2006;18:546–559. doi: 10.1521/aeap.2006.18.6.546. [DOI] [PubMed] [Google Scholar]
- 20.Brown EJ, Outlaw FH, Simpson EM. Theoretical antecedents to HIV risk perception. J Am Psychiatr Nurses Assoc. 2000;6:177–182. [Google Scholar]
- 21.Takahashi TA, Johnson KM, Bradley KA. A population-based study of HIV testing practices and perceptions in 4 US states. J Gen Intern Med. 2005;20:618–622. doi: 10.1111/j.1525-1497.2005.0112.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Klein H, Elifson KW, Sterk CE. “At risk” women who think that they have no chance of getting HIV: self-assessed perceived risks. Women Health. 2003;38:47–63. doi: 10.1300/J013v38n02_04. [DOI] [PubMed] [Google Scholar]
- 23.Adams AL, Becker TM, Lapidus JA, et al. HIV infection risk, behaviors, and attitudes about testing: are perceptions changing? Sex Transm Dis. 2003;30:764–768. doi: 10.1097/01.OLQ.0000078824.33076.45. [DOI] [PubMed] [Google Scholar]
- 24.Fichtner RR, Wolitski RJ, Johnson WD, et al. Influence of perceived and assessed risk on STD clinic clients’ acceptance of HIV testing, return for test results, and HIV serostatus. Psychol Health Med. 1996;1:83–98. [Google Scholar]
- 25.Gerrard M, Gibbons FX, Bushman BJ. Relation between perceived vulnerability to HIV and precautionary sexual behavior. Psychol Bull. 1996;119:390–409. doi: 10.1037/0033-2909.119.3.390. [DOI] [PubMed] [Google Scholar]
- 26.Amadora-Nolasco F, Alburo RE, Aguilar EJT, et al. Knowledge, perception of risk for HIV, and condom use: a comparison of registered and freelance female sex workers in Cebu City, Philippines. AIDS Behav. 2001;5:319–330. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.