Abstract
Objective
Uncertainty is one key factor influencing physician and patient behavior. We examined the propensity to express uncertainty on mental health versus biomedical issues by elderly patients (> 65 years) and physicians during primary care visits.
Methods
385 videotaped visits were coded according to “topics,” which are issues raised by any participant during the visit. This approach allowed us to examine if uncertainty was expressed in biomedical, mental health or other topics, and the factors associated with expressions of uncertainty.
Results
We found that physicians expressed uncertainty in 20.21% of topics compared to patients expressing uncertainty in 11.73% of topics discussed in all visits. Patients expressed uncertainty in 22% of biomedical and 46.5% (p<0.01) of mental health topics. Similar statistics were found in physician’s expression of uncertainty with more uncertainty being expressed with mental health topics (23.9%) than biomedical topics (12.56%, p<0.05).
Conclusion
Physicians expressed more uncertainties than patients during visits. Patients and physicians both expressed more uncertainties on mental health topics suggesting that patients and primary care physicians felt less knowledgeable or less confident about dealing with mental health issues.
Practice Implications
Understanding the inherent uncertainties in medicine can help physicians and patients engage in more productive discussion about both biomedical and mental health topics.
Keywords: Uncertainty, Mental Health, Physical Health, Mixed Methods, Topic Coding, Interaction Analysis
1. Introduction
Uncertainty is one of the key factors influencing physician [1–2] and patient behavior [3–4]. Defined technically, uncertainty is a cognitive state that occurs when the decision maker is unable to assign definite probabilistic values to events [5–6]. Intrinsic to the technical parameters and cognitive experiences of uncertainty are its expressions in interpersonal communication and behavioral responses. Uncertainty about disease incidence is associated with excessive ordering of tests and repeated visits [7] in part due to the “physician’s responsibility … to ‘do everything possible’ to forward the complete, early and painless recovery of his patients” [8]. Overuse of diagnostic tests and office visits related to uncertainty contributes to significant variations in health care service use and costs [2, 9–11]. Uncertainty in outcome of treatments produces anxiety for both physicians [12] and patients [13–14]. These challenges are more severe for primary care physicians treating elderly patients with multiple and complex chronic conditions [15]. Uncertainty around the diagnosis of mental illnesses—e.g. depression—can be more complicated to manage than biomedical issues as there are “no physiological or laboratory test, radiological examination, or tissue diagnosis to definitively establish the diagnosis” [16]. Thus, practitioners face major obstacles to identifying depression due to inadequate knowledge of the diagnostic criteria, the best questions to ask to evaluate whether those criteria are met, and time constraints in a busy office practice setting [17].
Communication is thought to be essential to the construction, management, and resolution of uncertainty [18]. The literature contains a wealth of theoretical and empirical research on the sources of uncertainty [18–21]. Although some authors have addressed uncertainty as a negative event, others see uncertainty as reflective of a neutral cognitive state [22]. While initially uncertainty prevents a physician from reaching a judgment, a primary diagnostic tool -- differential diagnosis -- can be used to organize the resolution of uncertainty. Empirical research on medical uncertainty is often informed by physician [23–24] and patient surveys [25]. While physicians’ expressions of uncertainty in actual clinical encounters have been identified as deserving more empirical research [23], direct observation of uncertainty expressions in clinical encounters is relatively uncommon. A limited number of studies analyzed transcripts of audio recordings of medical consultations and showed that physicians expressed more uncertainty to more educated patients who showed a greater desire for information [26–27]. One study in particular by Gordon, et al.[26] reported that physicians verbally expressed uncertainty in 71% of visits of male patients with at least one chronic illness, suggesting that physician uncertainty is overwhelmingly present in clinical encounters. Previous research has produced conflicting results as to how patients react to physician uncertainty. Some studies indicate that patient satisfaction decreases as physicians demonstrate uncertainty [24] while others suggest the opposite [26].
Many studies have surveyed patients regarding the amount of uncertainty they experienced, generally according to an interval or Likert scale [3–4, 28–29]. Nevertheless, research on how patients actually express uncertainty in clinical encounters is uncommon. One exception was found in a study that documented patients’ joking about their uncertainties as a strategy to seek information and influence the physician [30].
No studies to date, however, have examined uncertainty expressed by patients or physicians in relation to specific clinical topics discussed during visits, eg. biomedical topics vs. mental health or psychosocial topics. Analysis at the topic level allows us to account for possible variations in uncertainty depending upon the subject being discussed. This specificity could inform development of interventions targeting areas of the greatest uncertainty for patients and physicians. It is in the special context of communication between patients and physicians that we study clinical expression of uncertainty. Our research questions are: (1) What kinds of discussions between patients and physicians contain expressions of uncertainty? (2) Are there differences in the propensity for patients or physicians to express uncertainty across biomedical, mental health, or other topics? (3) Are patients who are more activated in clinical discussions more likely to express uncertainties? Likewise, do physicians express more uncertainties to patients who are more engaged in the visit? The study focuses on elderly patient-physician communication based on availability of communication data from an existing study of older patient-physician communication.
2. Methods
We chose a mixed methods research approach because it enabled us to combine qualitative and quantitative methods to address our hypotheses while providing breadth and depth of understanding beyond what would be obtained by either method alone [32–34].
2.1 Data sources
Our data came from videotapes collected in 1998–2000 as part of a separate study of a convenience sample of office-based physicians and their older patients in three types of practices [35]. The practices included a salaried medical group as part of an academic medical center (AMC) in the Southwest, a managed care group (MCG) in a Midwest suburb, and a number of fee-for-service solo practitioners in a Midwestern inner city (ICS). These sites included diverse practice forms and representation of patients and physicians from racial minority groups.
2.2 Participants
The recruitment effort resulted in a sample of 35 physicians and 385 patients (Table 1). Patients were at least 65 years of age and had identified the participating physician as their usual source of care. When patients came to the clinic for a visit, regardless of the reason for visit, they were invited to participate. If they expressed willingness to participate, informed consents were obtained and their visits were recorded. Patient participation rates ranged from 61%–65% at the three sites. Details of participant recruitment have been reported in greater detail elsewhere [36].
Table 1.
Key demographic characteristics of study participants
| Patient N=385 |
Physician N=35 |
||
|---|---|---|---|
| Age | Mean | 74.4 | 49.4 |
| S.D., min – max | 6.6, 65 – 91 | 11.6, 32 – 82 | |
| <65 | 0 | 31 | |
| 65 – 74 | 176 | 2 | |
| 74 – 84 | 142 | 1 | |
| > 84 | 40 | 1 | |
| Gender | Male | 124 | 27 |
| Female | 242 | 8 | |
| Race | White | 299 | 29 |
| African American | 40 | 6 | |
| Other | 27 | 0 | |
| Setting | Academic Medical Center | 125 | 10 |
| Managed Care Group | 209 | 21 | |
| Inner City Solo | 32 | 4 | |
| Specialty | Internal Medicine | 229 | 22 |
| Family Medicine | 100 | 10 | |
| Other | 37 | 3 |
Compared with national data [37], our physician sample is similar in gender composition but has fewer physicians in the extremes of the age distribution. African-American physicians were over-represented in our data (14%, compared with 6% nationally). Our patient sample is similar to national data on elderly patients in age distribution and living arrangement [38], but different in having more educated and fewer married patients [39] (see Table 1).
2.3 Measurement of uncertainty
We developed a tool for identifying expressions of uncertainty directly from the videotapes, after reviewing pertinent literature [1, 18, 23–24, 40–41] and consulting with physicians, medical sociologists, and communications researchers. Our measure of uncertainty was based on verbal expressions, behavioral actions related to searching for additional information [24, 26], and the context of the interaction.
Verbal expressions that conveyed uncertainty were coded as the presence of uncertainty. For example, an elderly patient wanted her physician to identify the cause of her fatigue. Her physician stated that “I don’t know why you are feeling so tired.” The physicians examined her and ordered a stress cardiogram. This is a topic in which both patient and physician expressed uncertainty over the nature of the illness.
In addition to identifying verbal exchanges suggesting uncertainty, we also identified behavioral actions taken by either participant that suggested searching for information. Many physicians stepped out to call a specialist for consultation while others went to look up side effect profiles of medications from the Physician’s Desk Reference. For instance, a physician stated to his patient that he needed to call a cardiologist in order to verify whether her dry cough was caused by a blood pressure medication (Lisinopril) he had prescribed. Upon his return a few minutes later, he said that the cardiologist confirmed his concern and suggested an alternative (Cozaar). His leaving the room to make a call to a specialist conveyed his inability to determine the cause of her symptom. (The context in which the behavior took place was important. If a physician went out of the room to answer a page that was unrelated to the patient at hand, his leaving the room was not considered a behavioral expression of uncertainty.) Both verbal and behavioral expressions were combined into our primary uncertainty score.
2.4 Qualitative data analysis
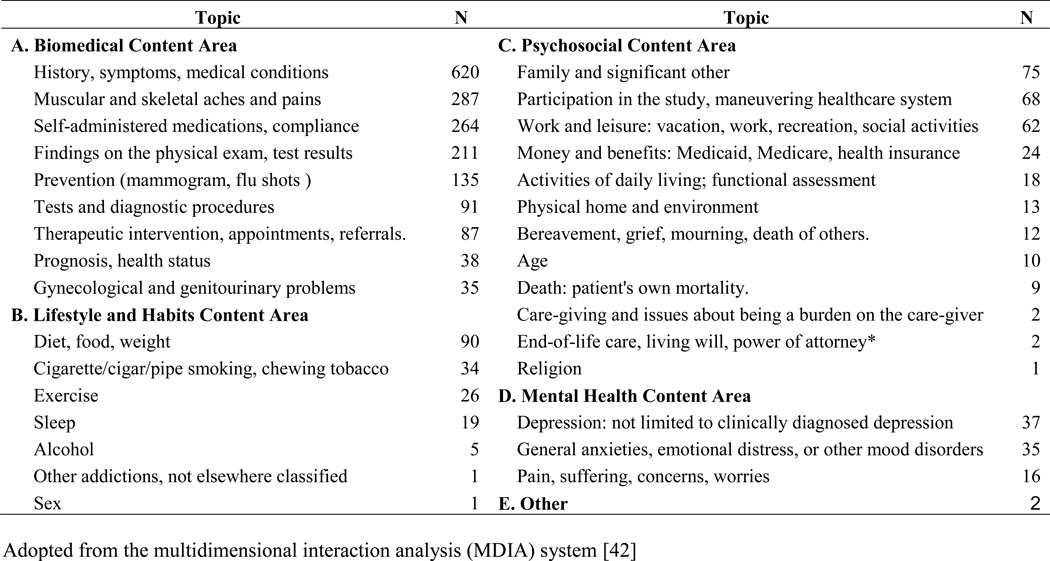
The content of visits is composed of decision making units we refer to as “topics,” operationalized as clinical issues raised by either participant. Our approach follows the multidimensional interaction analysis (MDIA) system, which codes an interaction directly from an audiotape of the visit. Figure 1 presents detailed information on the topics and the frequencies of the topics covered during the visits. Because only those topics under content areas A–D generally required clinical decisions that could potentially involve dealing with uncertainties, we excluded topics in content area E (others). Each topic was assigned a number using a pre-determined list [42]. The analyses were based on 2,350 topics, totaling about 111 hours of video-recording.
Figure 1.
Major content areas and topics
Our approach allows us to examine if uncertainty was expressed in each topic and the factors associated with these expressions. Coding of the videotaped visits consisted of three major components: identifying topics discussed in a visit, recording uncertainty expression in patient-physician interaction on each topic, and coding the dynamics of the talk-- e.g., who initiated the discussion of a particular topic and how many times (i.e., instances) a particular topic was discussed. We view patient initiation of a topic as a sign of patient engagement or activation in clinical decision making [43]. Additional details of other coding measures are reported elsewhere [31].
Training coders involved over 8 hours of initial didactic training, and independent coding of a series of visits by each five coders. The coders included four physicians and one registered nurse. Following accepted coding consistency practice [44], 10% of visits coded by each coder were coded by another coder to ensure inter-rater consistency whereas 5% of visits coded by a coder were coded by the same coder again to ensure intra-rater consistency. Further, weekly meetings with the lead author clarified concepts and resolved difficulties. Percent agreement among coders was 93% on physicians’ expression of uncertainty and 87% on patients’ expression of uncertainty. These scores are consistent with other studies using direct observation for physicians’ expressions of uncertainty (87%) [26].
Besides videotaping, patients were given a brief survey–before seeing the physician—on demographics, whether the physician was their regular source of care, and the purpose of the visit. Participating physicians also responded to a survey on specialization, practice setting, amount of time in practice, and socio-demographic characteristics.
Given our distinct way of coding by topic, we have provided an example below to illustrate how we conducted our analyses.
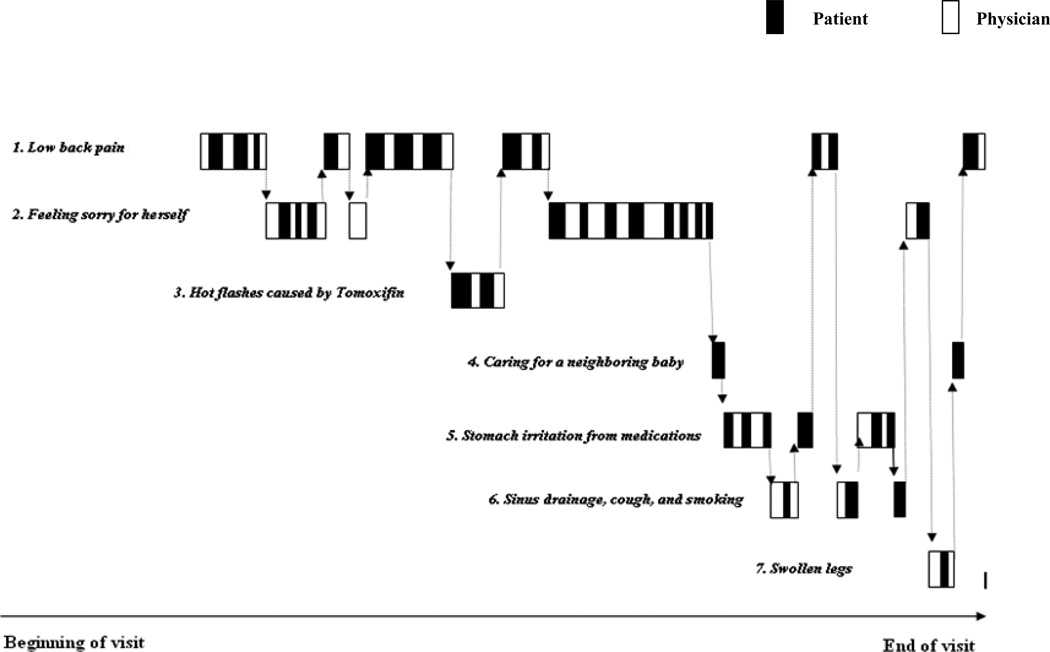
2.4.1 Example of identifying topics
Coders first carefully reviewed the entire video to determine the nature and number of topics raised during the visit. Figure 2 depicts the flow of conversation during one office visit and illustrates how this is grouped into topics for coding. After watching the visit video, seven topics were identified: 1) difficulties managing lower back pain, awaiting orthopedic diagnosis and treatment, 2) burden of caring for husband with dementia and daughter with substance abuse issues, 3) angst over hot flashes caused by Tamoxifen, 4) joy in caring for a neighboring baby with cerebral palsy, 5) stomach irritation from medications, 6) sinus drainage, cough and smoking, and 7) swollen legs. The initiator of each topic and instances within the topic were recorded.
Figure 2.
Illustration of interactional dynamics in one visit
2.4.2 Example of recording expressions of uncertainty
Coders documented whether patient or physician expressed uncertainty during each topic and whether verbal or behavioral expressions match any of the criteria described earlier. The following excerpt suggests physician uncertainty about the effects of psychoactive medications. The patient is concerned about taking an “addictive” medication and the physician offers his definition of an addictive medicine and expresses uncertainty about how effective the medication he plans to prescribe will be in making the patient feel less anxious: (Dr = physician, Pt = patient):
Pt: Sounds good to me, I'll try anything. I just don't want to get hooked on drugs forever.
Dr: Right.
Pt: Would I take them forever?
Dr: No. We would try
Pt: Are they addictive?
Dr: Addiction's a name I use for drugs that make you feel happy or high.
Pt: Like my scotch?
Dr: No comment. I think that benzodiazepines like Valium is addictive. But I think if I give you a medicine called Celexa, and I'll give you samples, and we'll try you out on it and give you a couple weeks of it and then give you a prescription and see if it makes you feel less anxious. I'm not saying that you're going to feel happy, but you'll notice that you're not feeling as anxious.
2.5 Quantitative analysis
The dependent variables were binary variables for whether the physician or patient expressed uncertainty. Main explanatory variables included the nature of topic (biomedical versus mental health, psychosocial, personal habits) [42], patient’s age, and the initiator of the topic (patient versus physician). Covariates included physician’s gender, years in medical practice, and specialty (family practice versus others) [45], patient race, gender, education [23–24], the length of association between the patient and physician (continuity of care) [45], and the reason for visit (acute versus chronic conditions).
Besides univariate and bivariate analyses, we examined the association between physician’s or patient’s expressions of uncertainty and the explanatory variables using a logistic regression model. The structure of the data contains multiple observations (topics) within the visit between the same patient-physician dyad. We chose panel data analysis approach (PROC GENMOD) to address the hierarchical nature of our data structure given the clustering of topics within a visit and the clustering of patients within an individual physician. Physician’s practice setting was accounted for by two binary variables. All analyses were done in SAS 9.2. Categorical variables have been “centered” to prevent potential errors in statistical inference [46].
3. Results
The 385 visits contained 2,350 topics in aggregate. The sample characteristics are presented in Table 1. T-tests and chi-squared tests were used to determine statistical significance of patient and physician characteristics associated with expressions of uncertainty (see Table 2).
Table 2.
Topic characteristics by patient or physician expressions of uncertainty
| Patient Uncertainty | Physician Uncertainty | |
|---|---|---|
| All topics, % (N=2,350) | 20.21 | 11.73 |
| Topic Characteristics | ||
| Biomedical topics, % (control) | 22.16 | 12.56 |
| Lifestyle and health habit topics, % | 13.58 ** | 9.88 |
| Mental health topics, % | 46.48 ** | 23.94 * |
| Psychosocial topics, % | 8.59 ** | 6.11 ** |
| MD Initiate Topics, % | 13.79 | 10.8 |
| Patient Initiate Topics, % | 28.27 ** | 12.9 |
| Number of instances in topic, mean | 2.30 ** | 2.24 ** |
| Visit Characteristics, % | ||
| Reason for visit: chronic, % (control) | 22.18 | 12.52 |
| acute, % | 13.86 ** | 9.36 |
| Patient Characteristics | ||
| Age 65 – 74 (control) | 20.65 | 12.4 |
| Age 75 – 84 | 18.67 | 12.49 |
| Age > 85 | 23.79 | 7.05 |
| Male, % (control) | 18.5 | 9.52 |
| Female, % | 21.06 | 12.88 |
| White, % (Control) | 19.7 | 11.25 |
| African American, % | 18.59 | 9.05 |
| Education, ≤ high school, % (Control) | 20.3 | 11.16 |
| ≥college, % | 20.19 | 12.52 |
| Mental Health Score, mean | 42.14 | 41.83 |
| Physician Characteristics | ||
| Male, % (control) | 19.36 | 12.35 |
| Female, % | 23.12 | 9.63 |
| White, % (control) | 19.62 | 11.89 |
| African American, % | 25.1 | 10.89 |
| Years in medical practice, mean | 21.31 | 22.16 |
| Internal medicine, % (control) | 16.84 | 7.91 |
| Family medicine, % | 24 | 13.91 |
| Other specialties, % | 20.97 | 14.02 |
| Practice Setting Characteristics | ||
| Academic Medical Center, % (control) | 25.26 | 16.02 |
| Managed care organization, % | 17.13 | 9.17 * |
| Inner city solo, % | 18.75 | 10.42 |
| Dyad Characteristics | ||
| Year of patient-MD relationship, mean | 5.68 | 5.17 |
p<0.05,
p<0.01
3.1 Descriptive analysis
3.1.1 Patients
At the topic level, patients expressed uncertainty in 20% of topics whereas physicians expressed uncertainty in 12% of all topics discussed in all visits. In comparison to patients expressing uncertainty in 22% of biomedical topics, mental health topics had a higher percentage of expressions of uncertainty (46.48%, p<0.01), lifestyle and health habits (13.58%) and psychosocial topics had lower percentages (8.59%, p<0.01). Supporting our hypothesis, topics initiated by the patient had more expressions of patient uncertainty (28.27%, p<0.01) compared to physician-initiated topics (13.79%).
At the visit level, the patient was significantly less likely to express uncertainty during visits for acute issues (13.86%, p<0.01) as compared to visits for chronic issues (22.18%). No racial, gender, age, nor education differences in either patient characteristics or physician characteristics in the expression of patient uncertainty were detected. No statistically significant differences were detected for patient uncertainty in relationship to their mental health score (mean), year of patient-MD relationship (mean), or three types of practice settings.
3.1.2 Physicians
Physicians were similar to patients in expressing more uncertainty with mental health topics (23.94%, p<0.05) compared to biomedical (12.56%) and psychosocial (6.11%, p<0.05) topics. Although not statistically significant, physicians gave a few more expressions of uncertainty in topics initiated by the patient (12.9% versus 10.8% of topics initiated by physicians). Physicians in the MCG were less likely to express uncertainty compared with AMC physicians (9% versus 16%, p<0.05). No statistically significant difference was detected between MCG and ICS physicians in their propensity to express uncertainty. No statistically significant differences appeared for physician uncertainty for patient characteristics of age, gender, race/ethnicity, education, nor mean mental health score. Additionally, there were no statistically significant differences observed for physician uncertainty according to physician characteristics of gender, race/ethnicity, years in practice, or years of the patient-physician relationship.
3.2 Regression analysis results
Table 3 displays results from the logistic regression analysis with odds ratios and shows statistically significant effects for the nature of topic discussed. Compared with biomedical topics, patients were 2.8 times (p<0.01) and physicians 2.1 times more likely (p<0.01) to express uncertainty in discussing mental health topics. Patients and physicians were much less likely to express uncertainty in discussions of psychosocial or lifestyle issues. Supporting our initial hypothesis, patients were more likely to express uncertainty (OR=2.6, p<0.01) in relation to topics that they had initiated versus physician initiated topics. Further, patients were less likely to express uncertainty in visits for acute issues than chronic issues (OR=0.52, p<0.01). High number of instances in a topic is associated with more expressions of patient (OR=1.18) and physician uncertainty (OR=1.14, p<0.01). Physicians were less likely to express uncertainty in the MCO than the AMC (OR=0.55, p<0.05). Patient’s age was not a significant factor.
Table 3.
Factors associated with the probability of expressing uncertainties: panel data analysis method
| Hypothesized Factors | Patient Uncertainty Odds Ratio |
Physician Uncertainty Odds Ratio |
|---|---|---|
| Compared with biomedical topics | ||
| Mental health topics | 2.796 ** | 2.072 ** |
| Psychosocial topics | 0.302 ** | 0.469 ** |
| Lifestyle and personal habits topics | 0.56 * | 0.845 |
| Compared with physician-initiated topics | ||
| Patient initiation | 2.599 ** | 1.16 |
| Compared with visits for chronic conditions | ||
| Reason for visit was acute condition | 0.522 ** | 0.764 |
| Number of instances | 1.181 ** | 1.143 ** |
| Compared with patients age 65 – 74 | ||
| Patient age 75 – 84 | 0.861 | 0.998 |
| Patient age ≥ 85 | 1.191 | 0.46 |
| Compared with Academic Medical Center | ||
| Managed care organization | 0.731 | 0.552 * |
| Inner city solo | 0.832 | 0.655 |
| Log likelihood | 2099.888 | 1607.02 |
| Number of topics | 2285 | 2284 |
p<0.05,
p<0.01
Note: Controlled for number of instances in topic, patient gender, education, years of patient-physician relationship, physician’s years in medical practice, physician’s specialty, and practice settings. Because none of these were statistically significant, they are not reported in the table.
4. Discussion and conclusion
Uncertainty is an integral part of medicine and a central feature of illness experience. Although expressions of clinical uncertainty do not in themselves indicate appropriateness of care [21], they are an important factor of medical practice and patient experience.
4.1 Discussion
The low disclosure of uncertainty suggests that uncertainty expressions were uncommon among the physicians and patients who participated in this study. The discrepancy between our findings and those of Gordon et al., [26] who reported that physicians expressed uncertainty in more than 70% of their visits, is worthy of further exploration. While having similar expressions of uncertainty, other methodological differences may have contributed to the different frequencies. For example, they used the physician as the unit of analysis and averaged the data collected at the patient level and related visits within each physician. Further, a majority (65%) of the physicians in that study were still in training as opposed to our sample, in which all physicians had finished their medical training, been in practice for an average of 20 years, and were their patients’ usual source of care. The majority of patients had fewer than four visits with the physician in that study. Therefore, the continuity of care is more limited in that study. In addition, all of their patients were male and younger than our patients. Lastly, practice patterns in one Northwestern VA clinic may be different from patterns in private practices in the Midwest or Southwest regions where data for our study were gathered. Furthermore, our use of panel data analysis method to account for the clustering of patients within each physician might have produced more accurate estimates.
The finding that patients and physicians both expressed more uncertainties on mental health topics could suggest that patients and primary care physicians felt less knowledgeable or less comfortable dealing with mental health issues. It has been well documented that many clinicians are unprepared to recognize and treat anxiety and depression in primary care [47–50]. The lack of lab or imaging tests to confirm a mental health diagnosis could also contribute to uncertainty in dealing with mental health concerns [51]. The validity of screening tools such as the PHQ9, PHQ2 [52], or SIGE CAPS [53] could begin to remove some uncertainties in diagnosis, however, if they are applied in primary care. As shown in the bivariate and regression analyses of our data, physicians at the MCO expressed uncertainty less than those at the AMC. This finding answers one of the calls for future research from Gerrity, et al. [54] about how practice settings affect physicians’ expressions of uncertainty. To our knowledge, this is the first study comparing physicians’ uncertainty expressions across multiple types of care settings. The higher propensity to express uncertainty among physicians at the AMC could be associated with their tendency to attract “a sicker mix of patients” due to their focus on tertiary care. [55] Thus, the cases the physicians receive are more complex, which is associated with greater uncertainty regarding diagnosis, treatment, and outcomes. Also, AMCs have been touted for being “more competent in managing-- and educating students to manage-- the uncertainty involved in creating clinical paradigms” [56]. Physicians at these institutions may be more apt to discuss uncertainty with patients since they already engage in these discussions while teaching medical students. Replication and further study is needed to better understand the impact of medical practicing setting on expressions of uncertainty.
This study has several limitations. First, the gradients of uncertainty are not captured by the binary definition used. Future study can benefit from differentiating levels of uncertainty. Second, the cross-sectional nature of the data precludes ruling out the possibility that the physician revealed uncertainty in other visits with the same patient. It is possible that the physician may choose to not express any uncertainty about an issue, even if he may still be uncertain, if he has already discussed the uncertainties with the patient in a previous visit. Non-disclosure in this context is different from non-disclosure completely. Third, external validity may be limited due to the convenience sample. The latter two limitations are shared with other communications studies using audio or video recording of patient encounters. Fourth, this article discussed the direct expressions of uncertainty - regardless of whether they were explicit or implicit expressions - during patient-physician encounters. Future studies may want to differentiate implicit and explicit expressions of uncertainty. Further, this study does not address how the expression of uncertainty might have been suppressed when physicians not only do not know the probability of events but also do not reveal their uncertainty about it. Lastly, the study was based on communication between older patients and their primary care physicians. Comparison of the results of this study with other studies covering patients of different ages should be done with care.
4.2 Conclusion
We used a mixed methods research approach to gain insight into how often uncertainties were shared between physicians and their elderly patients during clinical encounters. We will continue to examine the extent to which the disclosure of uncertainty is related to referrals to specialists or further tests, both of which can be costly, when the incremental benefit can be limited. While it is beyond the scope of this study to also examine the extent of subsequent use of costly services in order to reduce uncertainty, we have recognized examples of this in our qualitative analysis. For example, a colonoscopy was ordered for a patient who suffered from anxiety disorder and sought treatment for irritable bowel syndrome even though she had had a colonoscopy three years ago. Another colonoscopy would be unlikely to yield useful new information. The unrealistic pursuit of certainty and control contributes to the overuse of medical technology, and a subsequent escalation of health care costs [57]. Future studies can attempt to separate these actions associated with uncertainty with more appropriate management of uncertainty that could lead to a healthy recognition of the irreducible unpredictability of natural phenomena as illness and healing. Sending patients for more tests that are of questionable additional value would only delay the more skill-intensive and empathetic problem solving that results in shared decision making and a subsequent reduction in use of invasive services [57]. This example further demonstrates that it is important for physicians to be familiar with mental health issues and treat them appropriately rather than resorting to ordering more costly diagnostic test in order to alleviate patients’ uncertainty about the nature of their illnesses.
4.3 Practice Implications
Taking uncertainty into account can enhance physicians’ therapeutic effectiveness because it demonstrates their honesty, willingness to be more engaged with patients, and commitment to the reality of the situation rather than resorting to evasion, half-truth, and even lies [58]. Physicians have much to gain from tactfully expressing medical uncertainties. Graduate medical training and continuing medical education should equip learners with necessary skills. Patients can also benefit from expressing their uncertainties. Some patients are concerned about being perceived as “stupid” if they ask too many questions [59]. However, it is only after lifting the veil of supposed certainty and infallibility of medicine-- and exposing its inherent uncertainties-- that physicians and patients can engage in more productive discussions about both biomedical and mental health topics [60].
Acknowledgments
Role of funding source: This research was funded by the National Institute of Mental Health (MH01935) and the National Institute on Aging (AG15737), which played no role in the collection, analysis, or interpretation of data.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Statement: “I confirm all patient/personal identifiers have been removed or disguised so the patient/person(s) described are not identifiable and cannot be identified through the details of the story.”
Contributor Information
Ming Tai-Seale, Health Policy Research, Palo Alto Medical Foundation Research Institute, 795 El Camino Real, Ames Building, Palo Alto, CA 94301-2302, USA, Tel: +1 650 853 4779, Fax: +1 650 329 9114, Tai-SealeM@pamfri.org.
Cheryl Stults, Health Policy Research, Palo Alto Medical Foundation Research Institute, Palo Alto, Ca, USA.
Weimin Zhang, Samueli Institute, Alexandria, VA, USA.
Martha Shumway, Department of Psychiatry, University of California, San Francisco, CA, USA.
References
- 1.Fox R. The evolution of medical uncertainty. Milbank Memorial Fund Q. 1980;58:1–49. [PubMed] [Google Scholar]
- 2.Wennberg JE, Barnes BA, Zubakoff M. Professional uncertainty and the problem of supplier-induced demand. Soc Sci & Med. 1982;16:811–824. doi: 10.1016/0277-9536(82)90234-9. [DOI] [PubMed] [Google Scholar]
- 3.Fraenkel L. Uncertainty and patients' preferred role in decision making. Patient Educ Couns. 2010 Mar 20; doi: 10.1016/j.pec.2010.02.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lien CY, Lin HR, Kuo IT, Chen ML. Perceived uncertainty, social support and psychological adjustment in older patients with cancer being treated with surgery. J. Clin. Nurs. 2009;18:2311–2319. doi: 10.1111/j.1365-2702.2008.02549.x. [DOI] [PubMed] [Google Scholar]
- 5.Budner S. Intolerance of ambiguity as a personality variable. J Pers Soc Psychol. 1962;30:29–50. doi: 10.1111/j.1467-6494.1962.tb02303.x. [DOI] [PubMed] [Google Scholar]
- 6.Mishel M. Perceived uncertainty and stress in medical patients. Res Nurs Health. 1984;7:163–171. doi: 10.1002/nur.4770070304. [DOI] [PubMed] [Google Scholar]
- 7.Kassirer JP. Our stubborn quest for diagnostic certainty: a cause of excessive testing. New Engl J Med. 1989;320:1489–1491. doi: 10.1056/NEJM198906013202211. [DOI] [PubMed] [Google Scholar]
- 8.Pascoe SW, Neal RD, Allgar VL. Open-access versus bookable appointment systems: survey of patients attending appointments with general practitioners. Br J Gen Pract. 2004;54:367–369. [PMC free article] [PubMed] [Google Scholar]
- 9.Detsky AS, Stricker SC, Mulley AG, Thibault GE. Prognosis, survival, and the expenditure of hospital resources for patients in an intensive-care unit. N Engl J Med. 1981;305:667–672. doi: 10.1056/NEJM198109173051204. [DOI] [PubMed] [Google Scholar]
- 10.Eddy DM. Variations in physician practice: the role of uncertainty. Health Affairs (Millwood) 1984;3:74–89. doi: 10.1377/hlthaff.3.2.74. [DOI] [PubMed] [Google Scholar]
- 11.Applegate WB. Physician management of patients with adverse outcomes. Arch Intern Med. 1986;146:2249–2252. [PubMed] [Google Scholar]
- 12.Parsons T. The Social System. New York: Free Press; 1951. [Google Scholar]
- 13.Johnson CG, Levenkron JC, Suchman AL, Manchester R. Does physician uncertainty affect patient satisfaction? J Gen Intern Med. 1988;3:144–149. doi: 10.1007/BF02596120. [DOI] [PubMed] [Google Scholar]
- 14.Curley SP, Eraker SA, Yates JF. An investigation of patients' reactions to therapeutic uncertainty. Med Decis Making. 1984;4:501–511. [Google Scholar]
- 15.Engel G. The need for a new medical model: a challenge for biomedicine. Science. 1977;196:129–136. doi: 10.1126/science.847460. [DOI] [PubMed] [Google Scholar]
- 16.Williams JW, Jr, Noel PH, Cordes JA, Ramirez G, Pignone M. Is this patient clinically depressed? JAMA. 2002;287:1160–1170. doi: 10.1001/jama.287.9.1160. [DOI] [PubMed] [Google Scholar]
- 17.Spitzer RL, Williams JB, Kroenke K, et al. Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME-MD 1000 study. JAMA. 1994;272:1749–1756. [PubMed] [Google Scholar]
- 18.Babrow A, Kasch C, Ford L. The many meanings of uncertainty in illness: toward a systematic accounting. Health Commun. 1998;10:1–23. doi: 10.1207/s15327027hc1001_1. [DOI] [PubMed] [Google Scholar]
- 19.Babrow AS. Uncertainty, evaluation, communication, and problematic integration. J Comm. 2001;51:453–455. [Google Scholar]
- 20.Babrow AS, Kline KN. From 'reducing' to 'coping with' uncertainty: reconceptualizing the central challenge in breast self-exams. Soc Sci & Med. 2000;51:1805–1816. doi: 10.1016/s0277-9536(00)00112-x. [DOI] [PubMed] [Google Scholar]
- 21.Babrow AS, Hines SC, Kasch CR. Illness and uncertainty: problematic integration and strategies for communicating about medical uncertainty and ambiguity. Paper presented at: Annual Conference of the National Communication Association; Chicago, IL. 2000. [Google Scholar]
- 22.Babrow AS, Hines S, Kasch C. Illness and uncertainty: Problematic integration and strategies for communicating about medical uncertainty and ambiguity. Explaining Illness. 2000 [Google Scholar]
- 23.Gerrity MS, Earp JL, DeVellis RF, Light DW. Uncertainty and professional work: perceptions of physicians in clinical practice. Am J Sociol. 1992;97:1022–1051. [Google Scholar]
- 24.Ogden J, Fuks K, Gardner M, et al. Doctors expressions of uncertainty and patient confidence. Patient Educ Couns. 2002;48:171–176. doi: 10.1016/s0738-3991(02)00020-4. [DOI] [PubMed] [Google Scholar]
- 25.Fagermoen MS, Hamilton G. Patient information at discharge--a study of a combined approach. Patient Educ Couns. 2006;63:169–176. doi: 10.1016/j.pec.2005.09.016. [DOI] [PubMed] [Google Scholar]
- 26.Gordon GH, Joos SK, Byrne J. Physician expressions of uncertainty during patient encounters. Patient Educ Couns. 2000;40:59–65. doi: 10.1016/s0738-3991(99)00069-5. [DOI] [PubMed] [Google Scholar]
- 27.Waitzkin H. Doctor-patient communication. Clinical implications of social scientific research. JAMA. 1984;252:2441–2446. doi: 10.1001/jama.252.17.2441. [DOI] [PubMed] [Google Scholar]
- 28.Mishel MH. The measurement of uncertainty in illness. Nurs Res. 1981;3:258–263. [PubMed] [Google Scholar]
- 29.Madar H, Bar-Tal Y. The experience of uncertainty among patients having peritoneal dialysis. J Adv Nurs. 2009;65:1664–1669. doi: 10.1111/j.1365-2648.2009.05013.x. [DOI] [PubMed] [Google Scholar]
- 30.Greenfield S, Kaplan S, Ware JE., Jr Expanding patient involvement in care: effects on patient outcomes. Ann Intern Med. 1985;102:520–528. doi: 10.7326/0003-4819-102-4-520. [DOI] [PubMed] [Google Scholar]
- 31.Tai-Seale M, McGuire T, Zhang W. Time allocation in primary care office visits. Health Serv Res. 2007;42:1871–1894. doi: 10.1111/j.1475-6773.2006.00689.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Johnson RB, Onwuegbuzie AJ, Turner LA. Toward a definition of mixed methods research. J Mixed Methods Res. 2007;1:112–133. [Google Scholar]
- 33.Creswell J, Fetters M, Ivankova N. Designing a mixed methods study in primary care. Ann Fam Med. 2004;2:7–12. doi: 10.1370/afm.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Creswell JW, Plano Clark VL. Designing and conducting mixed methods research. Thousand Oaks, Ca: Sage; 2006. [Google Scholar]
- 35.Cook M. Final Report: Assessment of Doctor-Elderly Patient Encounters, Grant No. R44 AG5737-S2. Washington, DC: National Institute of Aging; 2002. [Google Scholar]
- 36.Tai-Seale M, Bramson R, Drukker D, et al. Understanding primary care physicians' propensity to assess elderly patients for depression using interaction and survey data. Med Care. 2005;43:1217–1224. doi: 10.1097/01.mlr.0000185734.00564.c1. [DOI] [PubMed] [Google Scholar]
- 37.American Medical Association. Physician characteristics and distribution in the US, 2001/2002 Ed. Chicago: American Medical Association Press; 2001. [Google Scholar]
- 38.US Census Bureau. 2001. [Google Scholar]
- 39.Federal Interagency Forum on Aging Related Statistics. Older Americans 2000: Key Indicators of Well-Being. Hyattsville, MD: National Center for Health Statistics; 2000. [Google Scholar]
- 40.Gordon GHJS, Byrne J. Physician expressions of uncertainty during patient encounters. Patient Educ Couns. 2000;40:59–65. doi: 10.1016/s0738-3991(99)00069-5. [DOI] [PubMed] [Google Scholar]
- 41.Mishel M. Reconceptualization of the uncertainty in illness theory. J Nurs Scholar. 1990;22:256–262. doi: 10.1111/j.1547-5069.1990.tb00225.x. [DOI] [PubMed] [Google Scholar]
- 42.Charon R, Greene MG, Adelman RD. Multi-dimensional interaction analysis: a collaborative approach to the study of medical discourse. Soc Sci & Med. 1994;39:955–965. doi: 10.1016/0277-9536(94)90207-0. [DOI] [PubMed] [Google Scholar]
- 43.Kaplan SH, Gandek B, Greenfield S, Rogers W, Ware JE. Patient and visit characteristics related to physicians' participatory decision-making style: results from the Medical Outcomes Study. Med Care. 1995;33:1176–1187. doi: 10.1097/00005650-199512000-00002. [DOI] [PubMed] [Google Scholar]
- 44.Braddock CH, 3rd, Edwards KA, Hasenberg NM, Laidley TL. Levinson W. Informed decision making in outpatient practice: time to get back to basics. JAMA. 1999;282:2313–2320. doi: 10.1001/jama.282.24.2313. [DOI] [PubMed] [Google Scholar]
- 45.Waitzkin H. Information giving in medical care. J Health Soc Behav. 1985;26:81–101. [PubMed] [Google Scholar]
- 46.Kraemer HC, Blasey CM. Centering in regression analyses: a strategy to prevent errors in statistical inference. Internat J Methods in Psychiat Res. 2004;13:141–151. doi: 10.1002/mpr.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Callahan CM, Nienaber NA, Hendrie HC, Tierney WM. Depression of elderly outpatients: primary care physicians' attitudes and practice patterns. J Gen Intern Med. 1992;7:26–31. doi: 10.1007/BF02599097. [DOI] [PubMed] [Google Scholar]
- 48.Volkers AC, Nuyen J, Verhaak PF, Schellevis FG. The problem of diagnosing major depression in elderly primary care patients. J Affect Disord. 2004;82:259–263. doi: 10.1016/j.jad.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 49.Young HN, Bell RA, Epstein RM, Feldman MD, Kravitz RL. Physicians' shared decision-making behaviors in depression care. Arch Intern Med. 2008;168:1404–1408. doi: 10.1001/archinte.168.13.1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lipkin MJ, Quill T, Napodano R. The medical interview: a core curriculum for residencies in internal medicine. Ann Intern Med. 1984;100:277–284. doi: 10.7326/0003-4819-100-2-277. [DOI] [PubMed] [Google Scholar]
- 51.Light D. Uncertainty and control in professional training. J Health Soc Behav. 1979;20:310–322. [PubMed] [Google Scholar]
- 52.Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41:1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 53.Remick RA. Diagnosis and management of depression in primary care: a clinical update and review. CMAJ. 2002;167:1253–1260. [PMC free article] [PubMed] [Google Scholar]
- 54.Gerrity M, DeVellis R, Earp J. Physicians' reactions to uncertainty in patient care: a new measure and new insights. Med Care. 1990;28:724–736. doi: 10.1097/00005650-199008000-00005. [DOI] [PubMed] [Google Scholar]
- 55.Fox PD, Wasserman J. Academic medical centers and managed care: uneasy partners. Health Aff (Millwood) 1993;12:85–93. doi: 10.1377/hlthaff.12.1.85. [DOI] [PubMed] [Google Scholar]
- 56.Fargason C, Jr, Evans H, Ashworth C, Capper S. The importance of preparing medical students to manage different types of uncertainty. Acad Med. 1997;72:688. doi: 10.1097/00001888-199708000-00013. [DOI] [PubMed] [Google Scholar]
- 57.Frosch DL, Kaplan RM. Shared decision making in clinical medicine: past research and future directions. Am J Prev Med. 1999;17:285–294. doi: 10.1016/s0749-3797(99)00097-5. [DOI] [PubMed] [Google Scholar]
- 58.Groopman J. How Doctors Think. New York: Houghton Mifflin Company; 2007. [Google Scholar]
- 59.Tran AN, Haidet P, Street RL, O'Malley KJ, Martin F, Ashton CM. Empowering communication: a community-based intervention for patients. Patient Educ Couns. 2004;52:113–121. doi: 10.1016/s0738-3991(03)00002-8. [DOI] [PubMed] [Google Scholar]
- 60.Brody D. The patient’s role in clinical decision-making. Ann Intern Med. 1980;93:718–722. doi: 10.7326/0003-4819-93-5-718. [DOI] [PubMed] [Google Scholar]