Abstract
Background
Balance impairment is a significant problem for older adults, as it can influence daily functioning. Treating balance impairment in this population is a major focus of physical therapist practice.
Objective
The purpose of this study was to document current practices in clinical balance assessment and compare components of balance assessed and measures used across practice areas among physical therapists.
Design
This was a cross-sectional study.
Methods
A survey questionnaire was mailed to 1,000 practicing physical therapists in Ontario, Canada.
Results
Three hundred sixty-nine individuals completed the survey questionnaire. More than 80% of respondents reported that they regularly (more than 60% of the time) assessed postural alignment, static and dynamic stability, functional balance, and underlying motor systems. Underlying sensory systems, cognitive contributions to balance, and reactive control were regularly assessed by 59.6%, 55.0%, and 41.2% of the respondents, respectively. The standardized measures regularly used by the most respondents were the single-leg stance test (79.1%), the Berg Balance Scale (45.0%), and the Timed “Up & Go” Test (27.6%). There was considerable variation in the components of balance assessed and measures used by respondents treating individuals in the orthopedic, neurologic, geriatric, and general rehabilitation populations.
Limitations
The survey provides quantitative data about what is done to assess balance, but does not explain the factors influencing current practice.
Conclusions
Many important components of balance and standardized measures are regularly used by physical therapists to assess balance. Further research, however, is needed to understand the factors contributing to the relatively lower rates of assessing reactive control, the component of balance most directly responsible for avoiding a fall.
Balance, defined as the ability to keep the body's center of mass (COM) within the limits of the base of support (BOS),1 is required for many functional activities of daily life such as mobility and fall avoidance.2 Balance impairment occurs in up to 75% of people aged 70 years and older3 and is common in people with neurological and musculoskeletal disorders such as stroke and arthritis.4,5 Given the high prevalence of balance impairments and their potential impact on function, interventions to improve balance are major foci of physical therapist practice.6 Assessment of balance abilities7 is important for accurate diagnosis of potential impairments, identifying fall risk, treatment planning, and evaluating change over time, but is complicated by the complex, multifactorial nature of balance8 and the plethora of psychometrically valid, standardized measures available.9 To date, there is limited information about how physical therapists assess balance in clinical practice, and this information is important for understanding how to optimize quality of care.
The multifactorial nature of balance has implications for assessment because maintaining balance requires complex interactions from several underlying physiological systems in response to varying task demands and situational contexts.10,11 For example, components of the musculoskeletal and central nervous systems must be constantly integrated with one another to control the COM when the BOS is stable, as in stance (static stability), in advance of and during voluntary movements (dynamic stability or anticipatory control), and in response to externally induced instability that threatens to move the COM outside the BOS (reactive control). This systems model of balance highlights that each underlying component and type of control could individually lead to a balance impairment and need to be included in the balance assessment to understand which components are affected in order to develop individualized treatment approaches.12
Evidence-based health care requires the use of valid and reliable tests during clinical assessment.13 Many measures of balance are available; a systematic review identified 68 balance tests used to evaluate the effect of resistance training.9 Most clinical balance measures are functional in nature14–23 and evaluate performance of behaviors using observed judgments or measurement of a quantifiable parameter.24 However, these measures all consider different components of balance, tasks, scoring formulas, and measurement techniques and are validated for different populations, such that different tests may provide different information and make it difficult to compare across measures.
Although a number of review articles have summarized the available standardized balance measures to assist clinicians with selecting appropriate tests,24–28 there is little evidence documenting which measures are used in clinical practice. Two conference proceedings have published limited quantitative data on the use of standardized measures to assess balance.29,30 These abstracts suggest that physical therapists working in different practice areas use different measures to assess balance, although it has not been possible to make direct comparisons among groups. Moreover, no studies to date have examined the components of balance assessed using the systems model of balance. Therefore, the overall purpose of this study was to examine current practices in balance assessment across a broad range of settings and practice areas. The specific objectives were: (1) to identify which components of balance were most commonly evaluated, (2) to identify which standardized balance measures were most commonly used, and (3) to compare balance components assessed and measures used across practice areas.
Method
Study Design
This study was a cross-sectional survey of physical therapists practicing in the province of Ontario, Canada, which has more than 13 million inhabitants.31 A modified Dillman 3-step mailing approach was used.32 The survey package was mailed in March 2010, followed by a reminder postcard at 4 weeks and a complete survey package to nonresponders at 8 weeks.
Participants and Sampling
Practicing physical therapists who were providing services to adults with balance impairment were eligible for this study. Potential participants were sampled from the registry of the College of Physiotherapists of Ontario, the provincial regulatory body. The college provided a mailing list of individuals who specified orthopedics, neurology, rehabilitation, health promotion and prevention, or general as their primary area of practice in adult or geriatric populations. Of the 3,841 physical therapists identified, 1,000 randomly sampled individuals were surveyed. Survey questionnaires were mailed to potential participants, and they were given the option of completing and returning the questionnaire by mail or online. Only those physical therapists who treated people with balance impairments were asked to complete the questionnaire. Physical therapists who did not treat people with balance impairments were ineligible and were asked to return the questionnaire, as were individuals who declined to participate. Consent was considered implied when a questionnaire was returned.
Survey Instrument
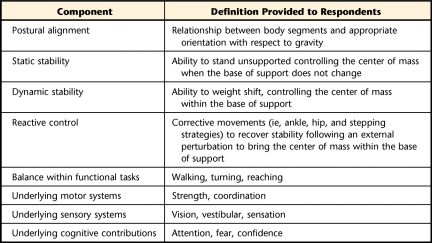
Questionnaire items were developed to determine the components of balance assessed and standardized balance measures used and to collect demographic and practice setting information. Respondents reported the frequency with which they assessed each of 8 components of balance (Tab. 1) and each of 8 standardized measures of balance identified from a review of the literature (Balance Evaluation Systems Test [BESTest],16 Berg Balance Scale [BBS],14 Clinical Test of Sensory Integration in Balance [CTSIB],19 Community Balance and Mobility Scale [CB&M],21 Performance-Oriented Mobility Assessment [POMA],20 push and release test,33 single-leg stance test,18 and Timed “Up & Go” Test [TUG]15). Respondents reported their use on a 6-point Likert scale that included both numeric and descriptive anchors (most of the time [≥80%], frequently [60%–79%], sometimes [41%–59%], occasionally [21%–40%], rarely [1%–20%], and never [0%]). The survey underwent pilot testing for sensibility and face and content validity with a convenience sample of 12 physical therapists who represented varied patient populations and practice settings. Pilot data were collected until no new information on survey format and content were gained. Pilot data were not included in the final analysis.
Table 1.
Components of Balance Surveyed
Data Analysis
For each of the balance components and measures surveyed, a binary variable was created that represented whether the component was included or the measure was used regularly in the assessment of balance (yes/no). Regular use was defined as 60% or more of the time. The primary outcomes were estimations of the percentage of respondents who regularly used of each of the surveyed balance components and measures and were summarized with descriptive statistics. Demographic and practice setting information also were summarized with descriptive statistics. For each of the balance components and measures surveyed, differences in the frequency of regular use among practice areas were compared using chi-square tests with predicted proportions for the expected values. Statistical significance was set at P<.05. Data analysis was conducted using Statistical Analysis Software, version 9.1 (SAS Institute Inc, Cary, North Carolina).
Role of the Funding Source
Dr Sibley is supported by a postdoctoral fellowship from the Canadian Institutes of Health Research and the Toronto Rehabilitation Institute. Dr Straus holds a Canada Research Chair in Knowledge Translation and Quality of Care. Dr Jaglal holds the Toronto Rehabilitation Institute Chair in Rehabilitation Research at the University of Toronto. The authors thank the College of Physiotherapists of Ontario for providing the mailing list. They acknowledge the support of the Toronto Rehabilitation Institute, which receives funding under the Provincial Rehabilitation Research Program from the Ministry of Health and Long Term Care in Ontario.
Results
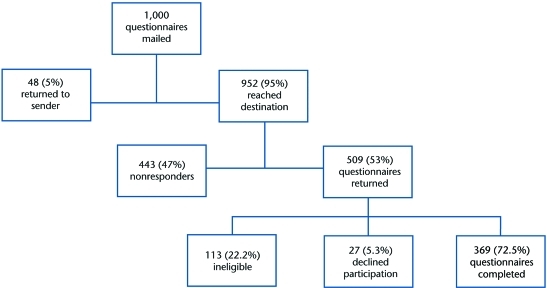
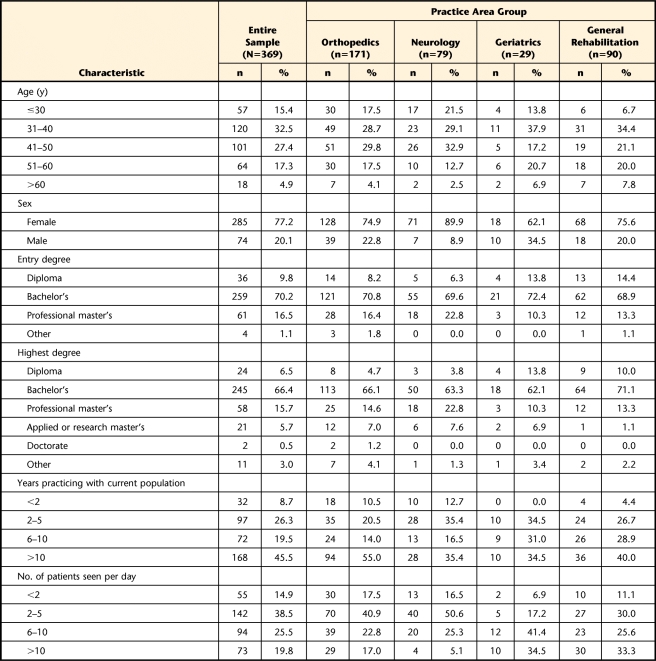
Of the 1,000 questionnaires mailed, 509 were returned (Figure). Of the respondents, 27 (5.3%) declined to participate, 113 (22.2%) did not treat balance impairments or were no longer practicing and were ineligible to participate, and 369 (72.5%) completed the survey. Respondent demographic and practice characteristics are summarized in Table 2. Four practice area groups were identified: orthopedics (n=171, 46.3%); neurology (n=79, 21.4%); geriatrics (n=29, 7.9%); and general rehabilitation, which represented respondents who treated multiple conditions from a combination of the other practice areas (n=90, 24.4%).
Figure.
Sampling results.
Table 2.
Respondent Demographic and Practice Characteristicsa
Percentages may not add up to 100% due to missing values.
b Other facility types: alternate level of care, mental health, retirement home, public/outreach home visits, industry, government, and occupational health.
Components of Balance Included in Assessment
Postural alignment, static stability, dynamic stability, balance in functional tasks, and underlying motor systems were all regularly assessed by more than 80% of the respondents (Tab. 3). Underlying sensory and cognitive contributions to balance were regularly assessed by 59.6% and 55.0% of respondents respectively, and reactive control was regularly assessed by the fewest respondents (41.2%). There were no significant differences across practice areas in the percentage of respondents regularly assessing static and dynamic stability, but there were significant variations in the proportion of respondents regularly assessing postural alignment, reactive control, functional balance, and underlying motor, sensory, and cognitive contributions across practice areas.
Table 3.
Frequency of Respondents Who Reported Regularly Assessing a Balance Component
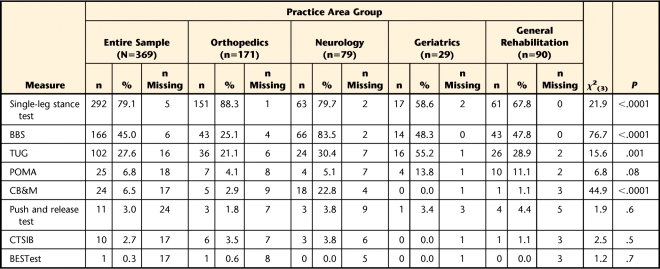
Use of Standardized Balance Measures
Overall, 90% of the respondents regularly used at least one standardized balance measure in their assessment of balance, and 53% of the respondents regularly used more than one measure (Tab. 4). The single-leg stance test was the measure most commonly used (79.1% of the respondents). Forty-five percent and 27.6% of the respondents regularly used the BBS and TUG, respectively. All other measures surveyed were regularly used by fewer than 10% of the respondents. In addition, 89.4% of the respondents reported regularly using informal observations to assess balance. There were significant differences in the proportion of respondents regularly using the single-leg stance test, BBS, TUG, and CB&M across practice areas, but no differences in the proportion of respondents using the POMA, push and release test, CTSIB, and BESTest across practice areas.
Table 4.
Frequency of Respondents Who Reported Regularly Using a Standardized Balance Measurea
BBS=Berg Balance Scale, TUG=Timed “Up & Go” Test, POMA=Performance-Oriented Mobility Assessment, CB&M=Community Balance and Mobility Scale, CTSIB=Clinical Test of Sensory Integration in Balance, BESTest=Balance Evaluation Systems Test.
Discussion
The study findings illustrate some important aspects of balance assessment in a broad sample of physical therapists practicing in Ontario, Canada. To our knowledge, this is the first study documenting balance assessment practices using a systems model of balance and comparing assessment practices across clinical domains. Of particular note was the observation that reactive balance control (reactions to external perturbations that threaten to move the COM outside the BOS) was regularly assessed the least, whereas the single-leg stance test was the measure regularly used by the most respondents—a finding obtained previously in older adults.9,30 Although some findings were common across all practice areas (eg, the low rates of reactive control assessment), there also were unique practice patterns in each group. For example, the neurology group tended toward the highest rates of assessing all components of balance, with more than 75% of the group regularly assessing all balance components, with the exception of reactive control. The BBS was the most commonly used measure in this group, but many therapists in this group also used the single-leg stance test, the TUG, and the CB&M. In contrast, almost all of the physical therapists in the orthopedics group used the single-leg stance test, which was more than double the use of any other measure in that group. The general rehabilitation group also used the single-leg stance test the most, followed by the BBS and then the TUG. The geriatrics group had similar rates of use of the single-leg stance test, the BBS, and the TUG.
Survey respondents regularly assessed many components of balance that are important for functional activities, including postural alignment, static and dynamic stability, functional balance, and underlying motor contributions to balance. The high proportion of individuals assessing these components suggests that respondents were comfortable performing these assessments and that doing so was feasible in their practice. In contrast, 20% to 25% fewer respondents regularly assessed underlying sensory and cognitive contributions to balance, and fewer than half of the respondents regularly evaluated reactive balance control. Assessment of these components is important because they are all distinct constructs that are individually related to falls34–36 and are amenable to treatment.37–39 The particularly low frequency of reactive control assessment is concerning because the ability to successfully react following a loss of balance determines whether an individual will fall.40
Additional study is needed to examine the factors influencing the inclusion of specific components of balance in an assessment and, in particular, why some physical therapists do not routinely evaluate reactive control. The nature of the assessment tools or measures used could influence what components of balance are assessed. For example, examination of the individual items on the measures included in the survey reveals that only the POMA, BESTest, and push and release test include a task that evaluates balance reactions to an external perturbation. Given that fewer than 10% of the respondents used any of these tests, the fact that many of the tools used by most respondents did not provide them with information about reactive control could have contributed to lower rates of assessment of this component. It also is possible that therapists' knowledge or perceptions influence practice patterns. Previous work suggests that a therapist's perception about the patient population is a primary factor influencing balance assessment methods. McGinnis et al41 conducted a qualitative examination of decision making in balance assessment in physical therapists and reported that participants shaped their initial balance assessment based on expected patient presentations and prior experience with patient-specific factors such as medical diagnosis, age, and history. However, they did not examine the influence of theoretical models of balance, such as the systems framework, on choice of assessment methods, and this is a focus of our ongoing work.
The high proportion (90%) of respondents who reported regularly using at least one standardized measure for balance is consistent with previous work on the use of outcome measures by physical therapists.42 Despite this positive finding, there is evidence to suggest that the findings of standardized measures are not necessarily incorporated into clinical decision making, but are primarily used for documentation and communication purposes.41 Other qualitative studies have suggested that physical therapists may doubt the information provided by outcome measures.43 Given the significant time and resources invested in administering standardized measures, additional study is needed to understand how their use may be optimized in clinical practice.
The majority of respondents (89%) used at least one of the top 3 measures for assessing balance (single-leg stance test, BBS, or TUG), and few respondents used any of the other balance measures surveyed. Only 17% of the respondents used the POMA, CB&M, push and release test, CTSIB, or BESTest. There is little information to explain the observed pattern of standardized measure use, and additional work is needed to understand the factors influencing the use or nonuse of particular measures. Known barriers such as time to administer the test may not have played a role, as the second most common measure used, the BBS, takes significantly more time to administer than either the single-leg stance test or the TUG. Similarly, the less popular tests are both long (BESTest, CB&M) and short (push and release test) in duration. McGinnis et al41 reported that physical therapists value the information gained in a test more than the time required to administer it, but the present results do not indicate how therapists use the measurements they collect.
A related ongoing challenge that warrants more attention is determining the “best” measure for assessing balance. The popularity of a measure is not necessarily related to its overall quality or value. Given the multiple purposes of measures and variations among patient populations and practice settings, identification of a single all-purpose balance measure is unlikely. Rather, recommendations for measure selection by function is likely more appropriate. This approach was attempted by McGinnis et al,44 who used expert consensus ranking to identify the suitability of 10 balance tests for the purposes of screening, impairment identification, identifying functional limitation, prognosis, or evaluating change. However, they did not rank measures against one another and did not include many balance measures that are available. Algorithms that might be tested for accuracy and effectiveness include initial screening tests followed by more in-depth tests to identify specific impairments,24 or begin with “easier” tests to identify individuals with obvious balance problems and progress to more challenging assessments in individuals who are higher functioning to rule out or identify more subtle impairments.
This study provides new information about how Canadian physical therapists assess balance in their clinical practice. Although the survey provides a large amount of quantitative data, there are a number of limitations. First, the survey relied on self-report measurements, which may overestimate perceived performance of a behavior.45 Second, although we asked respondents what components of balance they assess and what measures they use, we did not survey how respondents evaluate each component of balance. This is important information that would reflect the respondents' approach to balance assessment and clinical reasoning and will form a major component of subsequent work. Furthermore, we asked respondents how they assess balance in the context of the systems framework, and although we defined the terms of reference, this approach assumed that respondents used this framework as well. Aside from McGinnis and colleagues' work showing that physical therapists use a highly individualized approach to assess balance,41 there are few data demonstrating how physical therapists conceptualize balance. Additionally, due to the nature of the survey design, it was not possible to conduct hypothesis testing on rates of assessment and use across components and measures, so we are limited to descriptive reporting of the data. Finally, although pilot testing confirmed that we included the most common standardized balance measures in the survey, and none of the “other” measures listed by respondents had more than 3 users, it was not feasible to survey all of the possible balance measures available. There may be regional differences in the practice patterns across Canada and internationally that were not investigated in this study, so caution should be exercised when considering the generalizability of the findings.
Conclusions
Respondents regularly assessed many components of balance that are important for daily functioning; however, reactive components of balance specifically related to fall avoidance were not regularly assessed by many physical therapists. The reasons for this difference are not evident from the present study but could be related to the properties of existing measures. Most respondents used at least one standardized balance measure in addition to informal observation in their assessment of balance. Further work is needed to understand the factors influencing therapists' approach to balance assessment and explore factors contributing to the reduced frequency of reactive control assessment in order to assist with the development of interventions to ensure this important component of balance is included in the course of assessment and treatment.
Footnotes
All authors provided concept/idea/research design, writing, and consultation (including review of manuscript before submission). Dr Sibley, Ms Inness, and Dr Jaglal provided data collection. Dr Sibley provided data analysis. Dr Jaglal provided fund procurement.
This study was approved by the University of Toronto Research Ethics Board.
Dr Sibley is supported by a postdoctoral fellowship from the Canadian Institutes of Health Research and the Toronto Rehabilitation Institute. Dr Straus holds a Canada Research Chair in Knowledge Translation and Quality of Care. Dr Jaglal holds the Toronto Rehabilitation Institute Chair in Rehabilitation Research at the University of Toronto. The authors thank the College of Physiotherapists of Ontario for providing the mailing list. They acknowledge the support of the Toronto Rehabilitation Institute, which receives funding under the Provincial Rehabilitation Research Program from the Ministry of Health and Long Term Care in Ontario.
Preliminary results were presented at the Balance, Mobility, and Fitness Conference; January 28, 2011; Toronto, Ontario, Canada.
References
- 1. Shumway-Cook A, Woollacott MH. Motor Control Translating Research Into Clinical Practice. 3rd ed Philadelphia, PA: Lippincott Williams & Wilkins; 2007 [Google Scholar]
- 2. Howe TE, Rochester L, Jackson A, et al. Exercise for improving balance in older people. Cochrane Database Syst Rev. 2007;(4):CD004963 [DOI] [PubMed] [Google Scholar]
- 3. Dillon CF, Gu Q, Hoffman HJ, Ko CW. Vision, hearing, balance, and sensory impairments in Americans aged 70 years and older: United States, 1999–2006. NCHS Data Brief. April 2010(31):1–8 [PubMed] [Google Scholar]
- 4. Tyson SF, Hanley M, Chillala J, et al. Balance disability after stroke. Phys Ther. 2006;86:30–38 [DOI] [PubMed] [Google Scholar]
- 5. Sturnieks DL, Tiedemann A, Chapman K, et al. Physiological risk factors for falls in older people with lower limb arthritis. J Rheumatol. 2004;31:2272–2279 [PubMed] [Google Scholar]
- 6. Berg WP, Alessio HM, Mills EM, Tong C. Circumstances and consequences of falls in independent community-dwelling older adults. Age Ageing. 1997;26:261–268 [DOI] [PubMed] [Google Scholar]
- 7. Guide to Physical Therapist Practice. Phys Ther. 2nd ed 2001;81:9–746 [PubMed] [Google Scholar]
- 8. Woollacott MH, Tan PF. Balance control during walking in the older adult: research and its implications. Phys Ther. 1997;77:646–660 [DOI] [PubMed] [Google Scholar]
- 9. Orr R, Raymond J, Fiatarone Singh M. Efficacy of progressive resistance training on balance performance in older adults: a systematic review of randomized controlled trials. Sports Med. 2008;38:317–343 [DOI] [PubMed] [Google Scholar]
- 10. Woollacott MH, Shumway-Cook A. Changes in postural control across the life span: a systems approach. Phys Ther. 1990;70:799–807 [DOI] [PubMed] [Google Scholar]
- 11. Horak FB, Macpherson JM. Postural orientation and equilibrium. In: Rowell LB, Shepherd JT, eds. Handbook of Physiology: Exercise—Regulation and Integration of Multiple Systems. New York, NY: American Physiological Society; 1996:255–292 [Google Scholar]
- 12. Horak FB. Postural orientation and equilibrium: What do we need to know about neural control of balance to prevent falls? Age Ageing. 2006;35(suppl 2):ii7–ii11 [DOI] [PubMed] [Google Scholar]
- 13. Straus SE, Richardson WS, Glasziou P, et al. Evidence-based Medicine: How to Practice and Teach EBM. 3rd ed Edinburgh, Scotland: Churchill Livingstone; 2005 [Google Scholar]
- 14. Berg K, Wood-Dauphinée S, Williams JL, Maki BE. Measuring balance in the elderly: preliminary development of an instrument. Physiother Can. 1989;41:304–311 [Google Scholar]
- 15. Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–148 [DOI] [PubMed] [Google Scholar]
- 16. Horak FB, Wrisley DM, Frank J. The Balance Evaluation Systems Test (BESTest) to Differentiate balance deficits. Phys Ther. 2009;89:484–498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rose DJ, Lucchese N, Wiersma LD. Development of a multidimensional balance scale for use with functionally independent older adults. Arch Phys Med Rehabil. 2006;87:1478–1485 [DOI] [PubMed] [Google Scholar]
- 18. Fregly AR, Graybiel A. An ataxia test not requiring rails. Aerosp Med. 1968;3:277–282 [PubMed] [Google Scholar]
- 19. Shumway-Cook A, Horak FB. Assessing the influence of sensory interaction on balance: suggestion from the field. Phys Ther. 1986;66:1548–1550 [DOI] [PubMed] [Google Scholar]
- 20. Tinetti ME. Performance-oriented assessment of mobility problems. J Am Geriatr Soc. 1986;34:119–125 [DOI] [PubMed] [Google Scholar]
- 21. Howe JA, Inness EL, Venturini A, et al. The Community Balance and Mobility Scale: a balance measure for individuals with traumatic brain injury. Clin Rehabil. 2006;20:885–895 [DOI] [PubMed] [Google Scholar]
- 22. Tyson SF, DeSouza LH. Development of the Brunel Balance Assessment: a new measure of balance disability post stroke. Clin Rehabil. 2004;18:801–810 [DOI] [PubMed] [Google Scholar]
- 23. Haines T, Kuys SS, Morrison G, et al. Development and validation of the Balance Outcome Measure for Elder Rehabilitation. Arch Phys Med Rehabil. 2007;88:1614–1621 [DOI] [PubMed] [Google Scholar]
- 24. Browne JE, O'Hare NJ. Review of different methods for assessing standing balance. Physiotherapy. 2001;87:489–495 [Google Scholar]
- 25. Huxham FE, Goldie PA, Patla AE. Theoretical considerations in balance assessment. Aust J Physiother. 2001;47:89–100 [DOI] [PubMed] [Google Scholar]
- 26. Mancini M, Horak FB. The relevance of clinical balance assessment tools to differentiate balance deficits. Eur J Rehabil Med. 2010;46:239–248 [PMC free article] [PubMed] [Google Scholar]
- 27. Tyson SF, Desouza LH. A systematic review of methods to measure balance and walking post-stroke, part 1: ordinal scales. Phys Ther Rev. 2002;7:173–186 [Google Scholar]
- 28. Tyson SF, Desouza LH. The measurement of balance and walking post-stroke, part 2: functional performance tests. Phys Ther Rev. 2002;7:187–191 [Google Scholar]
- 29. McGinnis PQ, Bonstead K, Gorden J. Balance assessment methods utilized by members of the section on geriatrics. J Geriatr Phys Ther. 2002;25:27–28 [Google Scholar]
- 30. Saliga S, Bongiovanni C. Standing balance tests used by employed physical therapists in Michigan: a pilot study. J Geriatr Phys Ther. 2005;28:123–124 [Google Scholar]
- 31. Office of Economic Policy Ontario Fact Sheet February 2011. Toronto, Ontario, Canada: Ontario Ministry of Finance; 2011 [Google Scholar]
- 32. Dillman DA. Mail and Internet Surveys: The Tailored Design Method. 2nd ed New York, NY: John Wiley & Sons Inc; 2000 [Google Scholar]
- 33. Jacobs J, Horak FB, Van Tran K, Nutt JG. An alternative clinical postural stability test for patients with Parkinson's disease. J Neurol. 2006;253:1404–1413 [DOI] [PubMed] [Google Scholar]
- 34. Maki BE, Norrie RG, Zecevic A, et al. Control of rapid limb movements for balance recovery: do age-related changes predict falling risk? In: Duysens J, Smits-Engelsman BCM, Kingma H, eds. Control of Posture and Gait. Maastricht, the Netherlands: International Society for Postural and Gait Research; 2001:126–129 [Google Scholar]
- 35. Horak FB, Shupert CL, Mirka A. Components of postural dyscontrol in the elderly: a review. Neurobiol Aging. 1989;10:727–738 [DOI] [PubMed] [Google Scholar]
- 36. Shumway-Cook A, Woollacott M, Kerns KA, Baldwin M. The effects of two types of cognitive tasks on postural stability in older adults with and without a history of falls. J Gerontol A Biol Sci Med Sci. 1997;52:M232–M240 [DOI] [PubMed] [Google Scholar]
- 37. Mansfield A, Peters AL, Liu BA, Maki BE. Effect of a perturbation-based balance training program on compensatory stepping and grasping reactions in older adults: a randomized controlled trial. Phys Ther. 2010;90:476–491 [DOI] [PubMed] [Google Scholar]
- 38. Hu MH, Woollacott MH. Multisensory training of standing balance in older adults, II: kinematic and electromyographic postural responses. J Gerontol. 1994;49:M62–M71 [DOI] [PubMed] [Google Scholar]
- 39. Silsupadol P, Shumway-Cook A, Lugade V, et al. Effects of Single-task versus dual-task training on balance performance in older adults: a double-blind, randomized controlled trial. Arch Phys Med Rehabil. 2009;90:381–387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Maki BE, McIlroy WE. Postural control in the older adult. Clin Geriatr Med. 1996;12:637–658 [PubMed] [Google Scholar]
- 41. McGinnis PQ, Hack LM, Nixon-Cave K, Michlovitz SL. Factors that influence the clinical decision making of physical therapists in choosing a balance assessment approach. Phys Ther. 2009;89:233–247 [DOI] [PubMed] [Google Scholar]
- 42. Kay TM, Myers AM, Huijbregts MPJ. How far have we come since 1992? A comparative survey of physiotherapists' use of outcome measures. Physiother Can. 2001;53:268–275, 281 [Google Scholar]
- 43. McGlynn M, Cott CA. Weighing the evidence: clinical decision making in neurological physical therapy. Physiother Can. 2007;59:241–254 [Google Scholar]
- 44. McGinnis PQ, Wainwright SE, Hack LM, et al. Use of a Delphi panel to establish consensus for recommended uses of selected balance assessment approaches. Physiother Theory Pract. 2010;26:358–373 [DOI] [PubMed] [Google Scholar]
- 45. Davis DA, Mazmanian PE, Fordis M, et al. Accuracy of physician self-assessment compared with observed measures of competence. JAMA. 2006;296:1094–1102 [DOI] [PubMed] [Google Scholar]